Abstract
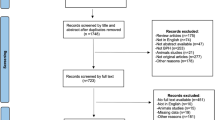
Tamsulosin has been used for the off-label treatment of lower urinary tract symptoms (LUTS) in women. Over the past few years, several randomized controlled trials (RCTs) have reported the clinical effectiveness and safety of tamsulosin for LUTS in women. Therefore, the aim of the present study was to perform a meta-analysis to evaluate the safety and efficacy of tamsulosin in treating LUTS in women, which may resolve some of the current controversies over use of the drug and provide more reliable evidence for the use of tamsulosin. A literature review was performed to identify all published RCTs of tamsulosin for the treatment of LUTS in women. The search included the following databases: PUBMED, EMBASE, the Cochrane Controlled Trail Register of Controlled Trials, Chinese Biomedical Literature Database, China National Knowledge Infrastructure, Chinese Science and Technique Journals Database (VIP) and Wanfang Database. A systematic review and meta-analysis were conducted. Six RCTs studies involving 764 female participants were included in the analysis. Four out of the six RCTs compared tamsulosin with placebo, one RCT compared tamsulosin with prazosin and the other study compared tamsulosin with tamsulosin combined with tolterodine. Two RCTs evaluated total International Prostate Symptom Score (IPSS) and improved total IPSS compared with the placebo (standardized mean difference=−4.08, 95% confidence interval=−5.93 to −2.23, P<0.00001). IPSS (storage symptom score), IPSS (voiding symptom score) and quality-of-life score also showed the similar effects. In addition, tamsulosin improved the Overactive Bladder Questionnaire score when compared with placebo in only one RCT. For urodynamic parameters, tamsulosin improved the average flow rate and the post-void residual volume when compared with prazosin and tolterodine combined with tamsulosin, respectively. Beyond that, the other parameters showed no significant difference between the treatment and control groups. On the basis of the present evidence, tamsulosin is an effective treatment for the relief of LUTS in women when compared with placebo. However, the safety of the tamsulosin remains unknown. Further, well-conducted trials that examine long-term outcomes are required.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout











Similar content being viewed by others
References
Moller LA, Lose G, Jorgensen T . The prevalence and bothersomeness of lower urinary tract symptoms in women 40-60 years of age. Acta Obstet Gynecol Scand 2000; 79: 298–305.
Jones C, Hill J, Chapple C Guideline Development Group. Management of lower urinary tract symptoms in men: summary of NICE guidance. BMJ 2010; 340: c2354.
Robinson D, Giarenis I, Cardozo L . New developments in the medical management of overactive bladder. Maturitas 2013; 76: 225–229.
Kim KH . Ischemic tolerance induced by cerebral preconditioning: new urologic research area. Int Neurourol J 2010; 14: 201–202.
Robinson D, Cardozo L . Pharmacotherapy of overactive bladder syndrome. Expert Rev Clin Pharmacol 2008; 1: 163–175.
Boyd K, Hilas O . alpha-adrenergic blockers for the treatment of lower-urinary-tract symptoms and dysfunction in women. Ann Pharmacother 2014; 48: 711–722.
Schwinn D . Novel role for α1‐adrenergic receptor subtypes in lower urinary tract symptoms. BJU Int 2000; 86: 11–22.
Groutz A, Blaivas JG . Non-neurogenic female voiding dysfunction. Curr Opin Urol 2002; 12: 311–316.
Barry MJ, Fowler FJ Jr., O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992; 148: 1549–1557, discussion 1564.
Okamura K, Nojiri Y, Osuga Y, Tange C . Psychometric analysis of international prostate symptom score for female lower urinary tract symptoms. Urology 2009; 73: 1199–1202.
Chai TC, Belville WD, McGuire EJ, Nyquist L . Specificity of the American Urological Association voiding symptom index: comparison of unselected and selected samples of both sexes. J Urol 1993; 150 (5 Pt 2): 1710–1713.
Chancellor MB, Rivas DA . American Urological Association symptom index for women with voiding symptoms: lack of index specificity for benign prostate hyperplasia. J Urol 1993; 150 (5 Pt 2): 1706–1708, discussion 1708-1709.
Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs FD, Fourcade R et al. The prevalence of lower urinary tract symptoms in men and women in four centres. The UrEpik study. BJU Int 2003; 92: 409–414.
Terai A, Matsui Y, Ichioka K, Ohara H, Terada N, Yoshimura K . Comparative analysis of lower urinary tract symptoms and bother in both sexes. Urology 2004; 63: 487–491.
Higgins JP, Green S . Cochrane handbook for systematic reviews of interventions version 5.1.0. Available at (http://handbook.cochrane.org/, 2011.
Cui Y, Zong H, Zhang Y . The efficacy and safety of silodosin in treating BPH: a systematic review and meta-analysis. Int Urol Nephrol 2012; 44: 1601–1609.
Yang CS, Huang H, Zhang LL, Zhu CR, Guo Q . Aripiprazole for the treatment of tic disorders in children: a systematic review and meta-analysis. BMC Psychiatry 2015; 15: 179.
Pummangura N, Kochakarn W . Efficacy of tamsulosin in the treatment of lower urinary tract symptoms (LUTS) in women. Asian J Surg 2007; 30: 131–137.
Robinson D, Cardozo L, Terpstra G, Bolodeoku J Tamsulosin Study Group.. A randomized double-blind placebo-controlled multicentre study to explore the efficacy and safety of tamsulosin and tolterodine in women with overactive bladder syndrome. BJU Int 2007; 100: 840–845.
Wang CJ, Huang SW, Chang CH . Effects of tamsulosin on lower urinary tract symptoms due to double-J stent: a prospective study. Urol Int 2009; 83: 66–69.
Hajebrahimi S, Asrbadr YA, Azaripour A, Sadeghi-Bazargani H . Effect of tamsulosin versus prazosin on clinical and urodynamic parameters in women with voiding difficulty: a randomized clinical trial. Int J Gen Med 2011; 4: 35–39.
Shalaby E, Ahmed AF, Maarouf A, Yahia I, Ali M, Ghobish A . Randomized controlled trial to compare the safety and efficacy of tamsulosin, solifenacin, and combination of both in treatment of double-j stent-related lower urinary symptoms. Adv Urol 2013; 2013: 752382.
Kim SO, Hwang EC, Oh KJ, Kwon D, Park K, Ryu SB . Efficacy and safety of combined therapy with tamsulosin and tolterodine in female patients with a maximal flow rate less than 12ml/s. Int Urogynecol J 2011; 22: 1287–1291.
Coyne K, Revicki D, Hunt T, Corey R, Stewart W, Bentkover J et al. Psychometric validation of an overactive bladder symptom and health-related quality of life questionnaire: the OAB-q. Qual Life Res 2002; 11: 563–574.
Oh SJ, Son H, Kim SW, Lee KS, Choo MS, Kim SO et al. Psychometric Properties of the Korean Version of the Overactive Bladder Questionnaire (OAB-q) in a Korean Population. Int Neurourol J 2012; 16: 77–85.
Cipullo LM, Cosimato C, Filippelli A, Conti V, Izzo V, Zullo F et al. Pharmacological approach to overactive bladder and urge urinary incontinence in women: an overview. Eur J Obst Gynecol Reprod Biol 2014; 174: 27–34.
Lo T-S . Alpha blockers in the clinical treatment of female lower urinary tract dysfunction. Incont Pelvic Floor Dysfunct 2010; 4: 69–71.
Wei J, Song Y, Sun L, Lv C . Comparison of artificial total disc replacement versus fusion for lumbar degenerative disc disease: a meta-analysis of randomized controlled trials. Int Orthop 2013; 37: 1315–1325.
Acknowledgements
This project was financially supported by the National Natural Science Foundation of China (no. 81460569) and the Guangxi Zhuang Autonomous Region Health Department of Traditional Chinese Medicine Science and Technology projects, Guangxi Province, China (nos GZZJ13-17 and gzzc1233).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, H., Huang, Z., Qiu, Y. et al. Tamsulosin for treatment of lower urinary tract symptoms in women: a systematic review and meta-analysis. Int J Impot Res 29, 148–156 (2017). https://doi.org/10.1038/ijir.2017.12
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2017.12
This article is cited by
-
Outcomes of bladder neck botulinum toxin injection for female primary bladder neck obstruction—does subjective improvement correlate with an objective assessment?
International Urogynecology Journal (2023)
-
The effect of tamsulosin in postoperative urinary retention: a meta-analysis of randomized controlled trials
Naunyn-Schmiedeberg's Archives of Pharmacology (2023)
-
The resonance® metallic ureteral stent in the treatment of malignant ureteral obstruction: a prospective observational study
BMC Urology (2019)
-
Effects of urine alkalinization with sodium bicarbonate orally on lower urinary tract symptoms in female patients: a pilot study
International Urogynecology Journal (2018)