Abstract
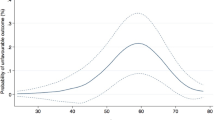
There is an established association between ED and pelvic fracture urethral injuries (PFUIs). However, ED can occur after the injury and/or the urethral repair. To our knowledge, only one study of erectile function (EF) after urethroplasty for PFUIs used a validated questionnaire. This study was carried out to determine the impact of anastomotic posterior urethroplasty for PFUIs on EF. We retrospectively reviewed the computerized surgical records to identify patients who underwent anastomotic urethroplasty for PFUIs from 1998 to 2014. Those patients were contacted by phone or mail and were re-evaluated in the outpatient clinic by International Index of Erectile Function questionnaire; in unmarried men, the single-question self-report of ED was used for evaluation of EF, clinical examination and penile color Doppler ultrasonography (CDU) for men with ED. Overall, 58 patients were included in the study among whom 36 (62%) men were sexually active and the remaining 22 (38%) were single. The incidence of ED among our group is 72%. All patients developed ED after initial pelvic trauma and none of our patients had impaired EF after urethroplasty. The incidence of ED increased proportionally with severity of pelvic trauma. All patients with type-C pelvic fracture, associated symphysis pubis diastasis, sacroiliac joints diastasis and bilateral pubic ramus fractures had ED. Men with PFUIs had worse EF than men in other series with pelvic fractures without urethral injury. The majority (88%) of men with ED showed veno-occlusive dysfunction on penile CDU. So we concluded that men with PFUIs had a high incidence of ED up to 72%. Anastomotic posterior urethroplasty had no negative impact on EF and the development of ED after PFUIs was related to the severity of the original pelvic trauma. Veno-occlusive dysfunction is the commonest etiology of ED on penile CDU.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Gomez RG, Mundy T, Dubey D, El-Kassaby AW, Firdaoessaleh, Kodama R et al. SIU/ICUD consultation on urethral strictures: pelvic fracture urethral injuries. Urology 2014; 83 (3 Suppl): S48–S58.
Anger JT, Sherman ND, Dielubanza E, Webster GD, Hegarty PK . Erectile function after posterior urethroplasty for pelvic fracture-urethral distraction defect injuries. BJU Int 2009; 104: 1126–1129.
Asci R, Sarikaya S, Buyukalpelli R, Saylik A, Yilmaz AF, Yildiz S . Voiding and sexual dysfunctions after pelvic fracture urethral injuries treated with either initial cystostomy and delayed urethroplasty or immediate primary urethral realignment. Scand J Urol Nephrol 1999; 33: 228–233.
Corriere JN, Rudy DC, Benson GS . Voiding and erectile function after delayed one-stage repair of posterior urethral disruptions in 50 men with a fractured pelvis. J Trauma 1994; 37: 587–589.
Dhabuwala CB, Hamid S, Katsikas DM, Pierce JM . Impotence following delayed repair of prostatomembranous urethral disruption. J Urol 1990; 144: 677–678.
Koraitim MM . Predictors of erectile dysfunction post pelvic fracture urethral injuries: a multivariate analysis. Urology 2013; 81: 1081–1085.
Malavaud B, Mouzin M, Tricoire JL, Game X, Rischmann P, Sarramon JP et al. Evaluation of male sexual function after pelvic trauma by the International Index of Erectile Function. Urology 2000; 55: 842–846.
Mark SD, Keane TE, Vandemark RM, Webster GD . Impotence following pelvic fracture urethral injury: incidence, aetiology and management. Br J Urol 1995; 75: 62–64.
Ozumba D, Starr AJ, Benedetti GE, Whitlock SN, Frawley WH . Male sexual function after pelvic fracture. Orthopedics 2004; 27: 313–318.
Shenfeld OZ, Kiselgorf D, Gofrit ON, Verstandig AG, Landau EH, Pode D et al. The incidence and causes of erectile dysfunction after pelvic fractures associated with posterior urethral disruption. J Urol 2003; 169: 2173–2176.
Harwood PJ, Grotz M, Eardley I, Giannoudis PV . Erectile dysfunction after fracture of the pelvis. J Bone Joint Surg (Br) 2005; 87: 281–290.
Lue TF, Zeineh SJ, Schmidt RA, Tanagho EA . Neuroanatomy of penile erection: its relevance to iatrogenic impotence. J Urol 1984; 131: 273–280.
Coursey JW, Morey AF, McAninch JW, Summerton DJ, Secrest C, White P et al. Erectile function after anterior urethroplasty. J Urol 2001; 166: 2273–2276.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A . The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997; 49: 822–830.
Tile M . Acute pelvic fractures: I. Causation and classification. J Am Acad Orthop Surg 1996; 4: 143–151.
O'Donnell AB, Araujo AB, Goldstein I, McKinlay JB . The validity of a single-question self-report of erectile dysfunction. Results from the Massachusetts Male Aging Study. J Gen Int Med 2005; 20: 515–519.
Metze M, Tiemann AH, Josten C . Male sexual dysfunction after pelvic fracture. J Trauma 2007; 63: 394–401.
O'Leary MP, Fowler FJ, Lenderking WR, Barber B, Sagnier PP, Guess HA et al. A brief male sexual function inventory for urology. Urology 1995; 46: 697–706.
Moreland RB . Is there a role of hypoxemia in penile fibrosis: a viewpoint presented to the Society for the Study of Impotence. Int J Impot Res 1998; 10: 113–120.
Mullerad M, Donohue JF, Li PS, Scardino PT, Mulhall JP . Functional sequelae of cavernous nerve injury in the rat: is there model dependency. J Sex Med 2006; 3: 77–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
El-Assmy, A., Harraz, A., Benhassan, M. et al. Erectile function after anastomotic urethroplasty for pelvic fracture urethral injuries. Int J Impot Res 28, 139–142 (2016). https://doi.org/10.1038/ijir.2016.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2016.18
This article is cited by
-
Epidemiology and aetiology of male and female sexual dysfunctions related to pelvic ring injuries: a systematic review
International Orthopaedics (2021)
-
Low-intensity shock wave therapy ameliorates erectile dysfunction in men with pelvic fractures associated with urethral injury
International Journal of Impotence Research (2019)