Abstract
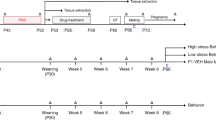
Dapoxetine, a selective serotonin reuptake inhibitor, is considered an antidepressant drug and has been developed for the treatment of premature ejaculation. Hence the objective was to assess whether dapoxetine administration to male rats adversely affect sexual behavior and pregnancy outcomes after mating with untreated female rats. Proven fertile male rats were gavaged with 0, 2.0, 4.0 and 8.0 mg dapoxetine per kg body weight (bw) per day (DC, DI, DII and DIII groups, respectively) for 70 days prior to mating with untreated female rats. Weight gain, organ weights and feed consumption were decreased significantly in the DII and DIII groups. A significant decline in the number of spermatozoa in the DII and DIII groups is attributed to a significant decrease in testosterone, luteinizing hormone and follicle-stimulating hormone. Levels of prolactin were significantly increased in the DII and DIII groups. Rats treated with a high dose of dapoxetine (8.0 mg kg−1) showed a significant inhibition in sperm motility and increment in sperm abnormalities. There was a pronounced decrease in fertility index in females mated with males treated chronically with 4.0 and 8.0 mg per kg bw dapoxetine. In addition, the treatment markedly increased the number of fetal resorptions in female rats impregnated by males in the DII and DIII groups reflecting their infertility. The number of implantation sites and the number of viable fetuses were also notably decreased in female rats impregnated by males given 4.0 or 8.0 mg kg−1 dapoxetine. These findings suggest that the long-term dapoxetine at high dosages causes failure of the fertilization or successful impregnation of the females mated with dapoxetine-treated male rats, which were clearly able to copulate. A detrimental effect of dapoxetine on fertility parameters was also revealed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Pattij T, Olivier B, Waldinger M . Animal models of ejaculatory behavior. Curr Pharm Des 2005; 11: 4069–4077.
Waldinger MD, Olivier B . Utility of selective serotonin reuptake inhibitors in premature ejaculation. Curr Opin Investig Drugs 2004; 5: 743.
McMahon CG, Lee G, Park JK, Adaikan PG . Premature ejaculation and erectile dysfunction prevalence and attitudes in the Asia-Pacific region. J Sex Med 2012; 9: 454–465.
Pryor JL, Althof SE, Steidle C, Miloslavsky M, Kell S . Efficacy and tolerability of dapoxetine in the treatment of premature ejaculation. J Urol 2005; 173 (Suppl): 201.
Stone KJ, Viera AJ, Parman CL . Off-label applications forSSRIs. Am Fam Physician 2003; 68: 498–504.
Jeong I, Kim S, Yoon S, Hahn S . Block of cloned Kv4.3 potassium channels by dapoxetine. Neuropharmacol 2012; 62: 2261–2266.
Ali MK, Lam RW . Comparative efficacy of escitalopram in the treatment of major depressive disorder. Neuropsychiatr Dis Treat 2011; 7: 39–49.
Hendrick V, Gitlin M, Altshuler L, Korenman S . Antidepressant medications, mood and male fertility. Psychoneuroendocrinol 2000; 25: 37–51.
Tanrikut C, Schlegel PN . Antidepressant-associated changes in semen parameters. Urology 2007; 69: 185.
Relwani R, Berger D, Santoro N, Hickmon C, Nihsen M, Zapantis A et al. Semen parameters are unrelated to BMI but vary with SSRI use and prior urological surgery. Reprod Sci 2011; 18: 391–397.
Tanrikut C, Feldman AS, Altemus M, Paduch DA, Schlegel PN . Adverse effect of paroxetine on sperm. Fertil Steril 2010; 94: 1021–1026.
Niederberger C . Adverse effect of paroxetine on sperm. J Urology 2011; 185: 638–639.
Koyuncu H, Serefoglu EC, Ozdemir AT, Hellstrom WJ . Deleterious effects of selective serotonin reuptake inhibitor treatment on semen parameters in patients with lifelong premature ejaculation. Intern J Imp Res 2012; 24: 171–173.
Wright C, Milne S, Leeson H . Sperm DNA damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod BioMed Online 2014; 28: 684–703.
Kumar VS, Sharma VL, Tiwari P, Singh D, Maikhuri JP, Gupta G et al. The spermicidal and antitrichomonas activities of SSRI antidepressants. Bioorg Med Chem Lett 2006; 16: 2509–2512.
OECD (Organization for Economic Co-operation and Development), 1995. Guideline for the Testing of Chemicals. Guideline 407: Repeated Dose 28-Day Oral Toxicity Study in Rodents (Adopted 27.07.1995).
WHO (World Health Organization). Handbook for Good Clinical Research Practice (GCP): Guidance for Implementation, 2002.
Vento PJ, Swartz ME, Martin LBE, Daniels D . Food intake in laboratory rats provided standard and fenbendazole-supplemented diets. J Am Assoc Lab Anim Sci 2008; 47: 46–50.
ElMazoudy RH, Attia AA, AbdElGawad HS . Evaluation of developmental toxicity induced by anti-cholinesterase insecticide, diazinon in female rats. Birth Defects Res B Dev Reprod Toxicol 2011; 92: 534–542.
Tietz NW . Clinical Guide to Laboratory Tests, 2nd edn. WB Saunders Company: Philadelphia, PA, USA, 1995; pp 1096.
Wheeler MJ . The determination of bio-available testosterone. Ann Clin Biochem 1995; 32: 345–357.
Smith CR, Norman MR . Prolactin and growth hormone: molecular heterogeneity and measurement in serum. Ann Clin Biochem 1990; 27: 542–550.
Roeschlau P, Bernt E, Gruber WJ . Enzymatic determination of total cholesterol in serum. J Clin Chem Clin Biochem 1974; 12: 226.
Mesbah S, Shokri S, Karbalay-Doust S, Mirkhani H . The effect of nandrolone decanoate on the body, testis and epididymis weight and semen parameters in adult male rats. Iran J Med Sci 2007; 32: 93–99.
Seed J, Chapin RE, Clegg ED, Dostal LA, Foote RH, Hurtt ME et al. Methods for assessing sperm motility, morphology, and counts in the rat, rabbit, and dog: a consensus report. ILSI Risk Science Institute Expert Working Group on Sperm Evaluation. Reprod Toxicol 1996; 10: 237–244.
Narayana K, D'Souza UJ, Rao KP . Ribavirin-induced sperm shape abnormalities in Wistar rat. Mutat Res 2002; 513: 193–196.
WHO (World Health Organization). Laboratory Manual for the Examination of Human Semen and Semen-Cervical Mucus Interaction, 4th (edn). Press syndicate of the University of Cambridge, 1999.
Cheng D, Zheng XM, Li SW, Yang ZW, Hu LQ . Effects of epidermal growth factor on sperm content and motility of rats with surgically induced varicoceles. Asian J Androl 2006; 8: 713–717.
Bjorndahl L, Soderlund I, Kvist U . Evaluation of the one-step eosin-nigrosin staining technique for human sperm vitality assessment. Hum Reprod 2003; 18: 813–816.
Cooper TG, Noonan E, von Eckardstein S, Auger J, Gordon Baker HW, Behre HM et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update 2010; 16: 231–245.
Faqi AS, Johnson WD, Morrissey RL, Mccormick DL . Reproductive toxicity assessment of chronic dietary exposure to soy isoflavones in male rats. Reprod Toxicol 2004; 18: 605–611.
Fernandes GSA, Arena AC, Fernandez CDB, Mercadante A, Barbisan LF, Kempinas WG . Reproductive effects in male rats exposed to diuron. Reprod Toxicol 2007; 23: 106–112.
Robb GW, Amann RP, Killian GJ . Daily sperm production and epididymal sperm reverses of pubertal and adult rats. J Reprod Fertil 1978; 54: 103–107.
Amann RP, Johnson L, Thompson DL, Pickett BW . Daily spermatozoal production. Biol Reprod 1976; 15: 586–592.
Tejada RI, Mitchell JC, Norman A, Marik JJ, Friedman S . A test for the practical evaluation of male fertility by acridine orange (AO) fluorescence. Fertil Steril 1984; 42: 87–91.
Manson JM, Kang YJ. Test methods for assessment of female reproductive and developmental toxicology. In: Hayes AW, (ed). Principles and Methods of Toxicology. Raven Press: New York, USA, 1989, pp 311–361.
Fox RP, Laird CW. Sexual cycles. In: Hafez ESE, (ed). Reproduction and Breeding Techniques for Laboratory Animals. Lea and Febiger: Philadelphia, PA, USA, 1970, pp 107–122.
Kanojia RK, Junaid M, Murthy RC . Chromium induced teratogenicity in female rat. Toxicol Lett 1996; 89: 207–213.
Salewski E . Staining method for a macroscopic test for implantation points in the uterus of the rat. Naunyn Schmiedebergs Arch Exp Pathol Pharmakol 1964; 247: 367.
Adilaxmamma K, Janardha A, Reddy KS . Monocrotophos: reproductive toxicity in rats. Ind J Pharmacol 1994; 26: 126–129.
Amin KMY, Khan MN, Rahman SZ, Khan NA . Sexual function improving effect of Mucuna pruriens in sexually normal male rats. Fitoterapia 1996; 67: 53–58.
OECD. Guidance or genetic document histological evaluation of endocrine and reproductive tests in rodents. Preparation, reading and reporting of vaginal smears, 2009.
Zanoli P, Benelli A, Rivasi M, Baraldi C, Vezzalini F, Baraldi M . Opposite effect of acute and subchronic treatments with Ferula hermonis on copulatory behavior of male rats. Int J Impot Res 2003; 15: 450–455.
Zanoli P, Benelli A, Zavatti M, Rivasi M, Baraldi C, Baraldi M . Improved sexual behavior in male rats treated with a Chinese herbal extract: hormonal and neuronal implications. Asian J Androl 2008; 10: 937–945.
Agmo A . Male rat sexual behavior. Brain Res Protoc 1997; 1: 203–209.
Pratap C, Tancer M, Yeragani VK . Metabolic syndrome: relevance to antidepressant treatment. J Psychiat Neurosci 2006; 31: 414.
Deiro TCBJ, Castro RM, Filho JEC, Souza SL, Freitas S, Ferreira LMP et al. Neonatal administration of citalopram delays somatic maturation in rats. Braz J Med Bio Res 2004; 37: 1503–1509.
Ballus C, Quiros G, De Flores T, de la Torre J, Palao D, Rojo L et al. The efficacy and tolerability of venlafaxine and paroxetine in outpatients with depressive disorder or dysthymia. Int Clin Psychopharmacol 2000; 15: 43–48.
Westenberg GM, Sandner C . Tolerability and safety of fluvoxamine and other antidepressants. Int J Clin Pract 2006; 60: 482–491.
Inkielewicz I . Impact of fluoxetine on liver damage in rats. Pharmacol Rep 2011; 63: 441–447.
Fava M . Weight gain and antidepressants. J Clin Psychiatry 2000; 61 (Suppl): 37–41.
Maina MB, Garba SH, Jacks TW . Histological evaluation of the rats testis following administration of a herbal tea mixture. J Pharmacol Toxicol 2008; 3: 464–470.
Althof S, Abdo C, Dean J, Hackett G, McCabe M, McMahon C et al. International Society for Sexual Medicine’s guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med 2010; 7: 2947–2969.
Porst H, McMahon C, Althof S, Sharlip I, Bull S, Aquilina J et al. Baseline characteristics and treatment outcome for men with acquired or lifelong premature ejaculation with mild or no erectile dysfunction: integrated analyses of three phase 3 dapoxetine trials. J Sex Med 2010; 7: 2231–2242.
Lima FB, Szawka RE, Anselmo-Franci JA, Franci CR . Pargyline effect on luteinizing hormone secretion throughout the rat estrous cycle: correlation with serotonin, catecholamines and nitric oxide in the medial preoptic area. Brain Res 2007; 1142: 37–45.
Mennigen JA, Martyniuk CJ, Crump K, Xiong H, Zhao E, Popesku J et al. Effects of fluoxetine on the reproductive axis of female goldfish (Carassius auratus. Physiol Genomics 2008; 35: 273–282.
Xin-Min Z, Traore SI, Wei-bin Z, Lu Q . Internal spermatic and peripheral vein plasma 5-hydroxytryptamine concentration levels in patients ith varicocele. Urotoday Int J 2010; 4: 1944–1957.
Safarinejad MR . Sperm DNA damage and semen quality impairment after treatment with selective serotonin reuptake inhibitors detected using semen analysis and sperm chromatin structure assay. J Urol 2008; 180: 2124–2128.
Freeman ME, Kanyicska B, Lerant A, Nagy G . Prolactin: structure, function, and regulation of secretion. Physiol Rev 2000; 80: 1523–1631.
Lee BH, Kim YK, Park SH . Using aripiprazole to resolve antipsychotic induced symptomatic hyperprolactinemia: a pilot study. Prog Neuropsychopharmacol Biol Psychiatry 2006; 30: 714–717.
Lafuente A, Gonzalez-Carracedo A, Romero A, Cano P, Esquifino AI . Effect of nitric oxide on prolactin secretion and hypothalamic biogenic amine contents. Life Sci 2004; 74: 1681–1690.
Robinson SE, Hambrecht KL . Effects of intrastriatal injections of soman on acetylcholine, dopamine and 5-hydroxytryptamine metabolism. Life Sci 1988; 42: 2331–2339.
Brook CGD, Marshall NJ . Endocrinology, 4th (edn). Blackwell Science: Oxford, UK, 2001.
Selvage DJ, Rivier C . Importance of the paraventricular nucleus of the hypothalamus as a component of a neural pathway between the brain and the testes that modulates testosterone secretion independently of the pituitary. Endocrinol 2003; 144: 594–598.
Gill-Sharma MK . Prolactin and male fertility: the long and short feedback regulation. Intern J Endocrinol 2009; 2009: 1–13.
Svechnikov K, Izzo G, Landreh L, Weisser J, Soder O . Endocrine disruptors and Leydig cell function. J Biomed Biotechnol 2010; 2010: 1–10.
Wolf WA, Kuhn DM . Role of essential sulfhdryl groups in drug interactions at the neuronal 5-HT transporter. Differences between amphetamines and 5-HT uptake inhibitors. J Biol Chem 1992; 267: 20820–20825.
De Lamirande E, Gagnon C . Redox control of changes in protein sulfhydryl levels during human sperm capacitation. Free Radic Biol Med 2003; 35: 1271–1285.
Quijada M, Illner P, Krulich L, McCann SM . The effect of catecholamines on hormone release from anterior pituitaries and ventral hypothalami incubated in vitro. Neuroendocrinol 1974; 13: 151–163.
Silva JVA, Lins AMJAA, Amorim JAA, Pinto CF, Deir TBJ, Oliveira JRM et al. Neonatal administration of fluoxetine decreased final sertoli cell number in Wistar rats. Int J Morphol 2008; 26: 51–62.
Irvine DS, Twigg JP, Gordon EL, Fulton N, Milne PA, Aitken RJ . DNA integrity in human spermatozoa: relationships with semen quality. J Androl 2000; 21: 33–44.
Jana K, Jana S, Samanta PK . Effects of chronic exposure to sodium arsenite on hypothalamo-pituitary-testicular activities in adult rats: possible an estrogenic mode of action. Reprod Biol Endocrinol 2006; 4: 9–12.
Carballada R, Esponda P . Structure of the vaginal plugs generated by normal rats and by rats with partially removed seminal vesicles. J Exp Zoo 1993; 265: 61–68.
Wolters JP, Hellstrom WJ . Current concepts in ejaculatory dysfunction. Rev Urol 2006; 8: S18–S25.
Hull EM, Du J, Lorrain DS, Matuszewich L . Extracellular dopamine in the medial preoptic area: implications for sexual motivation and hormonal control of copulation. J Neurosci 1995; 15: 7465–7471.
Almeida SA, Kempinas WG, Lamano Carvalho TL . Sexual behavior and fertility of male rats submitted to prolonged immobilization-induced stress. Braz J Med Biol Res 2000; 33: 1105–1109.
Koyuncu HH, Serefoglu EC, Yencilek E, Atalay H, Akbas N, Sarica K . Escitalopram treatment for premature ejaculation has a negative effect on semen parameters. Int J Impot Res 2011; 23: 257–261.
Prabhakar D, Richard B . How do SSRIs cause sexual dysfunction? Curr Psychiatry 2010; 9: 30–34.
ElMazoudy RH, Attia AA . Endocrine-disrupting and cytotoxic potential of anticholinesterase insecticide, diazinon in reproductive toxicity of male mice. J Haz Mat 2012; 209–210: 111–120.
Yakubu MT, Akanji MA . Effect of aqueous extract of Massularia acuminata stem on sexual behaviour of male Wistar rats. Evid Compl Altern Med 2011; 2011: 738103.
Acknowledgements
We thank Dr Azza Attia, Professor of Cell Biology, Department of Zoology, Faulty of Science, Alexandria University for her helpful suggestions and her revision, which improved the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
ElMazoudy, R., AbdelHameed, N. & ElMasry, A. Paternal dapoxetine administration induced deterioration in reproductive performance, fetal outcome, sexual behavior and biochemistry of male rats. Int J Impot Res 27, 206–214 (2015). https://doi.org/10.1038/ijir.2015.16
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2015.16
This article is cited by
-
Disruption of brain conductivity and permittivity and neurotransmitters induced by citrate-coated silver nanoparticles in male rats
Environmental Science and Pollution Research (2021)
-
Redox metabolism modulation as a mechanism in SSRI toxicity and pharmacological effects
Archives of Toxicology (2020)