Abstract
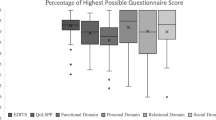
Peyronie’s disease (PD) is caused by progressive fibrotic scarring of the tunica albuginea resulting in curvature or other deformities of the erect penis. The severity of penile curvature or other deformity may contribute to a man’s inability to have intercourse (sexual disability), due to difficulty with penetration, partner pain or emotional stress. To determine whether the degree of curvature or type of penile deformity predicts sexual disability among men with PD. This cross-sectional analysis of consecutive men evaluated for PD at a single tertiary referral center used a PD-specific questionnaire to evaluate risk factors for sexual disability in men with PD, who did not have erectile dysfunction (ED). Multivariate logistic regression was used to determine the clinical predictors of sexual disability. Sexual disability as defined by the inability to have penetrative intercourse. A total of 202 men were evaluated and 88 men with ED were excluded. Sexual disability was associated with relationship problems, penile curvature and penile length loss in bivariate, but not multivariate analysis. We found that although many of the demographic, medical and sexual function domains were significant predictors of inability to have sex, the only significant predictor of sexual disability in multivariate analysis was curvature>60° (odds ratio 3.23 95%CI 1.08–9.67). PD can be sexually disabling in many men without ED. Severe penile curvature is a robust independent predictor of the ability to have intercourse. Other penile deformities fail to predict sexual disability. This is important for counseling patients with newly diagnosed PD and those who are considering medical or surgical intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pryor J, Akkus E, Alter G, Jordan G, Lebret T, Levine L et al. Peyronie’s disease. J Sex Med 2004; 1: 110–115.
La Pera G, Pescatori ES, Calabrese M, Boffini A, Colombo F, Andriani E et al. Peyronie’s disease: prevalence and association with cigarette smoking. A multicenter population-based study in men aged 50-69 years. Eur Urol 2001; 40: 525–530.
Jarow JP, Lowe FC . Penile trauma: an etiologic factor in Peyronie’s disease and erectile dysfunction. J Urol 1997; 158: 1388–1390.
Mulhall JP, Creech SD, Boorjian SA, Ghaly S, Kim ED, Moty A et al. Subjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screening. J Urol 2004; 171: 2350–2353.
Mulhall JP . Expanding the paradigm for plaque development in Peyronie’s disease. Int J Impot Res 2003; 15: S93–102.
Kadioglu A, Oktar T, Kandirali E, Kendirci M, Sanli O, Ozsoy C . Incidentally diagnosed Peyronie’s disease in men presenting with erectile dysfunction. Int J Impot Res 2004; 16: 540–543.
Tunuguntla HS . Management of Peyronie’s disease—a review. World J Urol 2001; 19: 244–250.
Kendirci M, Trost L, Sikka SC, Hellstrom WJ . Diabetes mellitus is associated with severe Peyronie’s disease. BJU Int 2007; 99: 383–386.
Deveci S, Hopps CV, O'Brien K, Parker M, Guhring P, Mulhall JP . Defining the clinical characteristics of Peyronie’s disease in young men. J Sex Med 2007; 4: 485–490.
Smith JF, Walsh TJ, Conti SL, Turek P, Lue T . Risk factors for emotional and relationship problems in Peyronie’s disease. J Sex Med 2008; 5: 2179–2184.
Smith JF, Walsh TJ, Lue TF . Peyronie’s disease: a critical appraisal of current diagnosis and treatment. Int J Impot Res 2008; 20: 445–459.
Muller A, Mulhall JP . Peyronie’s disease intervention trials: methodological challenges and issues. J Sex Med 2009; 6: 848–861.
Nelson CJ, Diblasio C, Kendirci M, Hellstrom W, Guhring P, Mulhall JP . The chronology of depression and distress in men with Peyronie’s disease. J Sex Med 2008; 5: 1985–1990.
Kelami A . Classification of congenital and acquired penile deviation. Urol Int 1983; 38: 229–233.
Perimenis P, Athanasopoulos A, Gyftopoulos K, Katsenis G, Barbalias G . Peyronie’s disease: epidemiology and clinical presentation of 134 cases. Int Urol Nephrol 2001; 32: 691–694.
Tefekli A, Kandirali E, Erol B, Tunc M, Kadioglu A . Peyronie’s disease: a silent consequence of diabetes mellitus. Asian J Androl 2006; 8: 75–79.
Kendirci M, Nowfar S, Gur S, Jabren GW, Sikka SC, Hellstrom WJ . The relationship between the type of penile abnormality and penile vascular status in patients with peyronie's disease. J Urol 2005; 174: 632–635, discussion 35.
Kadioglu A, Tefekli A, Erol B, Oktar T, Tunc M, Tellaloglu S . A retrospective review of 307 men with Peyronie’s disease. J Urol 2002; 168: 1075–1079.
Saigal CS, Wessells H, Pace J, Schonlau M, Wilt TJ . Predictors and prevalence of erectile dysfunction in a racially diverse population. Arch Intern Med 2006; 166: 207–212.
Hellstrom WJ, Bivalacqua TJ . Peyronie’s disease: etiology, medical, and surgical therapy. J Androl 2000; 21: 347–354.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Walsh, T., Hotaling, J., Lue, T. et al. How curved is too curved? The severity of penile deformity may predict sexual disability among men with Peyronie’s disease. Int J Impot Res 25, 109–112 (2013). https://doi.org/10.1038/ijir.2012.48
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2012.48
Keywords
This article is cited by
-
Are finasteride-related penile curvature/Peyronie’s disease Adverse Event Reports worthy of further clinical investigation? Disproportionality analysis based on both the Food and Drug Administration (FDA) and the European Medicines Agency (EMA) pharmacovigilance databases
International Journal of Impotence Research (2023)
-
Clinical characteristics and surgical outcomes in men undergoing tunica albuginea plication for congenital penile curvature who present with worsening penile deformity
World Journal of Urology (2020)
-
Patient perspectives on Peyronie’s disease: results of poststudy interviews from a phase 2 trial of collagenase clostridium histolyticum
International Journal of Impotence Research (2019)
-
Introducing the ventral sealing technique using collagen fleece for surgical therapy of patients with ventral Peyronie’s curvature: initial experience
International Journal of Impotence Research (2018)
-
Advances in the Surgical Treatment of Peyronie’s Disease
Current Sexual Health Reports (2016)