Abstract
To evaluate the biomarkers of sexual function, we investigated the relationship between questionnaire responses and biological hormones such as testosterone (T) and cortisol (F) in serum and saliva. The study population included 105 men aged 30–72 years (mean: 49±4.5, median: 49). Levels of all serum hormones (Total-T, Free-T, Bioavailable-T, Total-F and Bioavailable-F) and salivary hormones (Saliva-T and Saliva-F) were measured directly by liquid chromatography/tandem mass spectrometry. The International Index of Erectile Function (IIEF) was used as a questionnaire to evaluate sexual dysfunction. Free-T and Bioavailable-T showed significant inverse correlations with age (P<0.01). In the group not taking antidepressants, the levels of Bioavailable-F and Saliva-F showed significant inverse correlations with a portion of the IIEF score (P<0.05). However, reductions in Bioavailable-T and Saliva-T showed no association with the IIEF score. In the group taking antidepressants, these hormone levels showed no correlation with IIEF.
Similar content being viewed by others
Introduction
Male sexual hormones such as androgens are generally considered to be associated with sexual function. Among the androgens, testosterone (T) is a useful marker that is frequently used to evaluate male hypogonadism. Androgen production decreases with aging, and decreased testosterone is thought to induce late-onset hypogonadism, one of the most common symptoms of which is erectile dysfunction (ED).1 Late-onset hypogonadism is defined as a biochemical syndrome associated with advancing age and characterized by a deficiency in serum androgen levels with or without decreased genomic sensitivity to androgens. It may result in significant alterations in the quality of life and adversely affect the function of multiple organ systems.2 In Japan, measurement of free testosterone is recommended to diagnose late-onset hypogonadism.
Serum total testosterone (Total-T) consists of testosterone that binds strongly to sex hormone-binding globulin (SHBG), the testosterone that loosely binds to albumin and free testosterone (Free-T). The latter two are designated collectively as bioavailable-T (Bio-T), and its measurement is considered to be an index of androgen activity.3 In addition, the T of saliva (Sa-T) is regarded as free testosterone, and its measurement is thought to reflect blood Free-T and Bio-T.4 It has been reported that Total-T does not vary, but Free-T decreases gradually with aging.5
Cortisol (F), which is an adrenal cortical hormone, does not show changes in level with aging, but is increased by stress.6 Cortisol remains constant after increasing during the period of sexual maturation at the same time as T. Cortisol is known to raise blood pressure and blood sugar levels as well as cause sterility and immune dysfunction. When we feel stress, fear or tension, sympathetic nervous activity is increased relative to parasympathetic nervous activity, and the penis is contracted. Blood cortisol levels are known to increase in the hypothalamic–pituitary–adrenocortical system at the same time as that in which blood norepinephrine levels increase in the sympathetic nervous–adrenal medullary system when sympathetic nervous activity is dominant. Thus, ED may occur when cortisol levels are high. Although the cortisol level may reflect sexual function, there have been no earlier investigations of the relationships between these two parameters. Similar to Bio-T, bioavailable cortisol (Bio-F) is an active form that does not bind to globulin, and saliva cortisol (Sa-F) is secreted in the saliva as the free type.7 Here, we developed methods to measure testosterone and cortisol levels in the blood and saliva by liquid chromatography/tandem mass spectrometry (LC/MS-MS).8 We measured various hormones directly using this method and investigated the correlations of these hormone levels and sexual function on the basis of questionnaire responses from 105 patients.
Materials and methods
Patients
The study population included 103 men aged 32–72 years (mean: 49±4.5, median: 49). All patients visited our hospital for treatment of urological symptoms, including late-onset hypogonadism, with or without ED. Thirteen patients were taking antihypertensive agents and two patients were taking antidiabetic drugs. None of the patients were taking hormone medication (supplementation or deprivation) or phosphodiesterase type 5 (PDE5) inhibitors. All patients gave full informed consent to participate in this study. Saliva and serum samples were collected in the morning (between 0900 and 1100 hours). In addition, we investigated their sexual function and examined whether the patients had taken any psychotropic drugs. Each patient also completed validated questionnaires exploring anxiety and depression (Hospital Anxiety and Depression Scale [HAD scale]). This study was approved by the Internal Review Board of Kanazawa University, and was supported by a medical research fund from Kanazawa University Hospital (Kanazawa, Japan).
LC-MS/MS
Levels of all serum hormones (Total-T, Free-T, Bio-T, Total-F and Bio-F) and salivary hormones (Sa-T and Sa-F) were measured directly by LC/MS-MS. LC/MS-MS is effective for determining fixed quantities of very small amounts of material in biological samples.9 The LC/MS-MS apparatus used was an API4000 (Applied Biosystems, Kanazawa, Ishikawa, Japan) mass spectrometer and an HP1100 (Hewlett-Packard, Kanazawa, Ishikawa, Japan) liquid chromatograph. Bioavailable T (Bio-T) and F (Bio-F) were determined after separation of the SHBG-bound steroid.
Conventionally, Bio-T was calculated on the basis of albumin, SHBG and Total-T, using the method proposed by the International Society for the Study of the Aging Male. However, Bio-T and Bio-F were measured directly as levels of non-SHBG-bound T and F using LC/MS-MS in our study.
Definition of erectile function
To evaluate sexual dysfunction, the International Index of Erectile Function (IIEF) was used as a questionnaire study.10 IIEF is divided into five domains (erectile function, orgasmic function, sexual desire, intercourse satisfaction and overall satisfaction) and IIEF5 was evaluated simultaneously.11 Men who did not complete the questionnaire were excluded from statistical analysis.
Statistical analysis
Data from completed questionnaires were input into a Microsoft Excel spreadsheet. All analyses were performed with a SAS package (version 8.1) and differences were considered significant at P<0.05. The hormonal values were subjected to logarithmic transformation and controlled for age. Thereafter, we examined correlations between IIEF responses and hormonal levels. Spearman's rank test was used to test the correlations between age and hormonal profile, IIEF score and hormonal profile.
Results
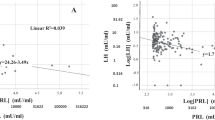
The relationships of testosterone and cortisol to age are shown in Table 1. Free-T and Bio-T showed significant inverse correlations with age (P<0.01). Sa-T showed a tendency toward a negative correlation, but the relation was not significant. Cortisol did not have a meaningful correlation with age (Figure 1). In addition, the levels of each type of testosterone (Total-T, Free-T, Bio-T and Sa-T) showed very strong correlations to the other forms of testosterone and there were also correlations among cortisol levels (Total-F, Bio-F and Sa-F).
Table 2 shows the baseline characteristics and the levels of each hormone in men who did and did not take psychotropic drugs. Sixty-four of the 103 patients included in the investigation (62%) took psychotropic drugs. The HAD scale was significantly high in the group taking psychotropic drugs. It was suggested that populations of men who took psychotropic drugs suffered from anxiety and depression. With regard to different types of psychotropic drugs, 15 patients took only selective serotonin reuptake inhibitors (SSRI), 14 took serotonin and norepinephrine reuptake inhibitors (SNRI), 9 took tricyclic antidepressants, 10 took minor tranquilizers and 16 patients took antidepressants and minor tranquilizers. Men who did not take psychotropic drugs showed significantly lower Total-T levels. There were no significant differences in levels of hormones other than those of Total-T.
When we examined the correlation between hormonal level and IIEF response, the hormonal levels were controlled for age, as it is well known that testosterone shows a significant inverse correlation with age. Table 3 shows the correlation coefficients for each domain of IIEF (erectile function, orgasmic function, sexual desire, intercourse satisfaction and overall satisfaction), IIEF5 and total score of IIEF, with various hormones in men who did not take psychotropic drugs. Bio-F showed negative correlations with erectile function, sexual desire, IIEF5 and total IIEF score (P<0.05). In addition, Sa-F showed negative correlations with intercourse satisfaction and total IIEF score (P<0.05). However, testosterone did not show a meaningful correlation with any of the IIEF domains (Figure 2).
There were no significant correlations between the various hormones and IIEF in this group who took psychotropic drugs.
Discussion
It has been suggested that androgen insufficiency disrupts cellular signaling pathways and produces pathological alterations in penile tissues, leading to ED.12 Although there is evidence suggesting that testosterone plays an important role in erectile function, testosterone levels below the normal lower limit may still be sufficient to retain a normal erectile function in most men.13, 14 The weak relationship between low T and ED is well known and supported by the results of both human and animal studies.15 A lack of association between T and IIEF-5 has been documented in a large consecutive series of almost 1000 elderly individuals with or without ED.16 In ED patients, hypogonadism is often associated with reduced sexual desire and nocturnal penile erections, whereas association with sex-induced erection is less evident. This is because T regulates not only cyclic guanosine monophosphate formation through nitric oxide synthase stimulation but also its catabolism through PDE5 activity. Androgens positively regulate PDE5, thus providing a possible explanation for the highest levels of this enzyme in the male genital tract.17 The androgen-dependent PDE5 expression could explain the reduced effectiveness of PDE5 inhibitors in the treatment of ED in hypogonadal patients. As T positively regulates both the initiation (nitric oxide synthase) and the end (PDE5) of the erectile process, its net effect on erection is modest. Hence, erections are still possible under hypogonadal conditions in which decreased cyclic guanosine monophosphate formation because of impaired NO production is most likely counterbalanced by regulated PDE5 activity and cyclic guanosine monophosphate hydrolysis. The main physiological action of T is therefore to ensure the timely adjustment of the erectile process as a function of sexual desire, therefore finalizing erection associated with sex. A trophic effect of T on the penile architecture has also been shown in different animal species.18 For all of the above reasons, treating hypogonadism restores impaired penile erections in experimental animal models, as well as in a clinical setting. Conversely, T administration to otherwise eugonadal individuals is rather ineffective. There have been many reports that sexual function is improved by androgen replacement therapy.19, 20, 21 All the above considerations explain the well-known weak correlation between ED and T. In this study, there was no correlation between testosterone and IIEF responses. That is, testosterone is not an appropriate biomarker for an evaluation of sexual function.
Bio-F and Sa-F showed significant negative correlations with some domains of IIEF in this study. In a rat model of adrenal insufficiency, it was shown earlier that the rat adrenal gland contributes to the maintenance of the erectile mechanism and may affect the neuronal nitric oxide synthase content in the penis.22 In a human study, on the other hand, there were no differences in cortisol levels between individuals with and without ED.23 These studies did not include detailed differential counts of cortisol. However, in our study, Bio-F and Sa-F (not Total-F) showed negative correlations with the IIEF score. This suggested that Bio-F and Sa-F, which are active forms of cortisol, likely decrease sexual function. One reason why ED occurred in patients with high levels of cortisol is because cortisol is increased by stress. It is known that the blood cortisol level increases at the same time as the blood norepinephrine level when sympathetic nervous activity is dominant. Sympathetic nervous activity has a restraining effect on erection, and sexual function is thought to be reduced under stress.24, 25 Our results indicate that increases in plasma and salivary cortisol may play causative roles in ED induced by social stress.
In studies of stress, cortisol and norepinephrine have been overused as standard stress markers. Cortisol level is an index of the endocrine response to stress and shows comparatively high normal values in blood (100–150 ng ml−1). We can analyze cortisol from saliva if we use a high sensitivity analytical procedure such as ELISA or LC-MS/MS.26 Measuring cortisol in saliva may become a useful index for evaluating the sexual function non-invasively. In addition, saliva-based measurement methods have attracted attention for measuring amylase in saliva as a marker of the sympathetic nervous system response to stress.27 Further studies in this field are needed.
In the men who took antidepressants in this study, there were no significant correlations between hormone values and IIEF. Neither testosterone nor cortisol values played an important role in erectile function in the group taking antidepressants. This was thought to be because ED and ejaculation disorder are induced by the actions of antidepressant medication. Furthermore, psychiatric disorder in itself may be a cause of ED.28 Patients with depression may have elevated cortisol levels.29 In addition, this type of drug could result in an increase in the prolactin level determining the reduction of T.30 Therefore, we could not obtain meaningful data from the patients taking psychotropic drugs.
Conclusions
The active forms of cortisol (Bio-F and Sa-F) showed negative correlations with sexual function in men who did not take psychotropic drugs, although there was no such correlation for testosterone. ED is thought to occur in patients with high levels of cortisol because of the relations between cortisol and stress. Cortisol may thus become a useful index for the evaluation of sexual function.
Conflict of interest
The authors declare no conflict of interest.
References
Hwang TIS, Lo HC, Tsai TF, Chiou HY . Association among hypogonadism, quality of life and erectile dysfunction in middle-aged and aged male in Taiwan. Int J Impot Res 2007; 19: 69–75.
Morales A, Lunenfeld B . Standards, guidelines and recommendations of the international society for the study of the aging male (ISSAM). Investigation, treatment and monitoring of late-onset hypogonadism in males. Official recommendations of ISSAM. Aging Male 2002; 5: 74–86.
Morley JE . The diagnosis of late life hypogonadism. Aging Male 2007; 10: 217–220.
Shirtcliff EA, Granger DA, Likos A . Gender differences in the validity of testosterone measured in saliva by immunoassay. Horm Behav 2002; 42: 62–69.
Ellison PT, Bribiescas RG, Bentley GR, Campbell BC, Lipson SF, Panter-Brick C et al. Population variation in age-related decline in male salivary testosterone. Hum Reprod 2002; 17: 3251–3253.
Kumsta R, Entringer S, Hellhammer DH, Wust S . Cortisol and ACTH responses to psychosocial stress are modulated by corticosteroid binding globulin levels. Psychoneuroendocrinology 2007; 32: 1153–1157.
Becker JB, Arnold AP, Berkley KJ, Blaustein JB, Eckel LA, Hampson E et al. Strategies and methods for research on sex differences in brain and behavior. Endocrinology 2005; 146: 1650–1673.
Honma S, Okuyama M, Kumagai Y . The estimation of bioavailable testosterone in serum using concanavalin A. Med Sci Digest 2005; 31: 99–103.
Higashi T . Trace determination of steroids causing age-related diseases using LC/MS combined with detection-oriented derivatization. Chem Pharm Bull 2006; 54: 1479–1485.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A . The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology 1997; 49: 822–830.
Rosen RC, Cappellori JC, Smith MD, Lipsky J, Pena BM . Development and evaluation of an abridged, 5-item version of the international index of erectile function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res 1999; 11: 319–326.
Traish AM, Goldstein I, Kim NN . Testosterone and erectile function: from basic research to a new clinical paradigm for managing men with androgen insufficiency and erectile dysfunction. Euro Urol 2007; 52: 54–70.
Martinez-Jabaloyas JM, Quepo-Zaragoza A, Hernandez-pastor F, Gil-salom M, Chuan-Nuez P . Testosterone levels in men with erectile dysfunction. BJU Int 2006; 97: 1278–1283.
Mikhail N . Does testosterone have a role in erectile function? Am J Med 2006; 119: 373–382.
Morelli A, Corona G, Filippi S, Ambrosini S, Forti G, Vignozzi L et al. Which patients with sexual dysfunction are suitable for testosterone replacement therapy? J Endocrinol Invest 2007; 30: 880–888.
Rhoden EL, Teloken C, Sogari PR, Souto CAV . The relationship of serum testosterone to erectile function in normal aging man. J Urol 2002; 167: 1745–1748.
Morelli A, Filippi S, Mancina R, Luconi M, Vignozzi L, Marini M et al. Androgens regulate phosphodiesterase type 5expression and functional activity in corpora cavernosa. Endocrinology 2004; 145: 2253–2263.
Traish AM, Park K, Dhir V, Kim NN, Moreland RB, Goldstein I . Effect of castration and androgen replacement on erectile function in a rabbit model. Endocrinology 1999; 140: 1861–1868.
Greco EA, Spera G, Aversa A . Combining testosterone and PDE5 inhibitors in erectile dysfunction: basic rationale and clinical evidence. Euro Urol 2006; 50: 940–947.
Shabsigh R . Testosterone therapy in erectile dysfunction and hypogonadism. J Sex Med 2005; 2: 785–792.
Shabsigh R, Rajfer J, Aversa A, Traish AM, Yassin A, Kalinchenko SY et al. The evolving role of testosterone in the treatment of erectile dysfunction. Int J Clin Pract 2006; 60: 1087–1092.
Penson DF, NG C, Rajfer J, Gonzalez-Cadavid NF . Adrenal control of erectile function and nitric oxide synthase in rat penis. Endocrinology 1997; 138: 3925–3932.
Derouet H, Lehmann J, Stamm B, Luhl C, Romer D, Georg T et al. Age dependent secretion of LH and ACTH in healthy men and patients with erectile dysfunction. Euro Urol 2002; 41: 144–154.
Mizuno T, Yotsuyanagi S, Kondo Y, Komatsu K, Ishiura Y, Nakamura Y et al. Dehydroepiandrosterone alleviates copulatory disorder induced by social stress in male rats. J Sex Med 2006; 3: 612–618.
Niikura O, Yokoyama O, Komatsu K, Yotsuyanagi S, Mizuno T, Namiki M . A causative factor of copulatory disorder in rats following social stress. J Urol 2002; 168: 803–809.
Vining RF, Mcginley RA, Maksvytis JJ, Ho KY . Salivary cortisol: a better measure of adrenal cortical function than serum cortisol. Ann Clin Biochem 1983; 20: 329–335.
Yamaguchi M, Deguchi M, Wakasugi J, Ono S, Takai N, Higashi T et al. Hand-held monitor of sympathetic nervous system using salivary amylase activity and its validation by driver fatigue assessment. Biosens Bioelectron 2005; 21: 1007–1014.
Araujo AB, Durante R, Feldman HA, Goldstein I, McKinlay JB . The relationship between depressive symptoms and male erectile dysfunction: cross-sectional results from the Massachusetts Male Aging Study. Psychosom Med 1998; 60: 458–465.
Belmaker RH, Agam G . Major depressive disorder. New Eng J Med 2008; 358: 55–68.
Corona G, Mannucci E, Fisher AD, Lotti F, Ricca V, Balecia G et al. Effect of Hyperprolactinemia in male patients consulting for sexual dysfunction. J Sex Med 2007; 4: 1485–1493.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kobori, Y., Koh, E., Sugimoto, K. et al. The relationship of serum and salivary cortisol levels to male sexual dysfunction as measured by the International Index of Erectile Function. Int J Impot Res 21, 207–212 (2009). https://doi.org/10.1038/ijir.2009.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijir.2009.14
Keywords
This article is cited by
-
Diabetes as a potential compounding factor in COVID-19-mediated male subfertility
Cell & Bioscience (2022)
-
The Role of Hormones in Male Sexual Function
Current Sexual Health Reports (2020)
-
Physical activity as an adjunct treatment for erectile dysfunction
Nature Reviews Urology (2019)
-
Individual prolactin reactivity modulates response of nucleus accumbens to erotic stimuli during acute cannabis intoxication: an fMRI pilot study
Psychopharmacology (2017)
-
Irritable bowel syndrome is associated not only with organic but also psychogenic erectile dysfunction
International Journal of Impotence Research (2015)