Abstract
The pathogenesis of preeclampsia (PE) involves a number of biological processes that may be directly or indirectly affected by glucocorticoid (GC) and vitamin D. GC exposure increases the risk of PE, and 1,25-dihydroxyvitamin D3 (1,25-(OH)2D3) deficiency may result in PE. The purpose of the present study was to confirm the involvement of GC/1,25-(OH)2D3 axis in the pathogenesis of PE. In the study, cortisol levels of PE patients were found to be higher than that of non-complicated pregnancies, while 1,25-(OH)2D3 were decreased in both PE women and GC-induced PE rats. Mechanically, GC reduced 1,25-(OH)2D3 levels via disturbing its biosynthetic and catabolic enzymes, including Cyp3a1,Cyp24a1 and Cyp27b1, especially enhancing the expressions of Cyp3a1, the dominant enzyme for vitamin D degeneration. Moreover, replenishing 1,25-(OH)2D3 ameliorated the symptoms and placental oxidative stress of GC-induced rat PE. The protective actions of 1,25-(OH)2D3 might be explained by its roles in antagonizing the effects of GC on trophoblast proliferation and apoptosis. Together, these findings suggest that GC exposure could lead to PE via dampening 1,25-(OH)2D3 biosynthesis, and GC/1,25-(OH)2D3 axis might represent a common pathway through which PE occurs.
Similar content being viewed by others
Introduction
Preeclampsia (PE), characterized by maternal hypertension, proteinuria and other systemic disorders occurring after 20 weeks of gestation, is a leading cause of maternal and fetal morbidity and mortality.1, 2, 3 Despite active research, the etiological mechanism of this disorder remains elusive. Increasing evidence indicates that stress or glucocorticoid (GC) exposure may result in PE.4, 5, 6, 7, 8 László et al.7 showed that stress in the first trimester of pregnancy might increase the risk of early-onset PE. Moreover, Takiuti et al.9 confirmed that stress in early pregnancy could induce PE in rat. We demonstrated previously that stress-mediated increase in GC activity is involved in spontaneous miscarriages10 and PE,5 and GC exposure in mid-late gestation could lead to rat intrauterine growth restriction.11 Interestingly, we confirmed recently that GC exposure in early placentation could induce PE in rats.6
The pathogenesis of PE involves a number of biological processes that may be directly or indirectly affected by vitamin D, including immune dysfunction, placental implantation, abnormal angiogenesis, excessive inflammation and hypertension.12, 13 In fact, PE has been demonstrated to be associated with low circulating levels of 25-hydroxyvitamin D (25(OH)D) and 1,25-dihydroxyvitamin D3 (1,25-(OH)2D3).14, 15 A case–control study showed a significant association between 25(OH)D concentrations in early pregnancy and subsequent PE.16 Moreover, expression and activity of 25-hydroxyvitamin D-1 alpha-hydroxylase (CYP27B1) are restricted in cultures of syncytiotrophoblast cells from preeclamptic pregnancies.17 Therefore, a deficiency of 1,25-(OH)2D3 may result in PE.
The balance between bioactivation and degradation of 1,25-(OH)2D3 is critical for ensuring its appropriate biological effects and is tightly controlled in vivo. Biosynthesis of vitamin D involves the action of CYP27B1, leading to the synthesis of hormonally active 1,25-(OH)2D3.18 1,25-(OH)2D3 is catabolized by CYP24A1, which is followed by sequential metabolism, yielding the terminal product calcitroic acid.19 It also undergoes CYP3A4-dependent 24- and 25-hydroxylations.20 CYP3A1 (the rodent ortholog of CYP3A4) represents a major component of CYP system in the rat placenta, highly expressed throughout pregnancy.21 Interestingly, previous findings indicated that CYP3A4, not CYP24, dominated the hydroxylation of 1,25-(OH)2D3 in human liver and intestine, and SXR/CYP3A4 has a key role in mediating vitamin D catabolism and drug-induced osteomalacia.19 Synthetic GC dexamethasone (Dex) could induce CYP3A1 expression in rat liver,22 and Dex could transactivate PXR and induce CYP3A1 expression in rat hepatocytes.23 Importantly, CYP3A4 induction could exert an important role in decreasing 1,25-(OH)2D3 levels.24 We showed that serum cortisol levels of PE women are higher than that of normal pregnancies.5 Moreover, we confirmed recently that GC exposure in early placentation could induce PE in rats,6 which may involve the loss of 1,25-(OH)2D3.
The present study, therefore, was undertaken to confirm the involvement of GC/1,25-(OH)2D3 axis in the pathogenesis of PE and to explore the underlying mechanisms. This study would provide a clue for better understanding of the pathogenesis of PE and contribute to develop potential therapeutic strategies in preventing PE.
Methods
Reagents and antibodies
Dex, Dex sodium phosphate, 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT), 1,25-(OH)2D3 and Hoechst 33258 were from Sigma Aldrich (Allentown, PA, USA). Anti-hypoxia-inducible factor 1-alpha (HIF1A, sc-10790) and Lamin B (sc-374015) antibodies were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA).
Patient samples
Blood samples were obtained from 26 women: 13 women with PE defined by hypertension (systolic and diastolic blood pressures higher than 140/90 mm Hg) and proteinuria (0.3 g per day)25 were recruited from the Puai Hospital, Tongji Medical College, Huazhong University of Science and Technology, China; as a comparative group, 13 pregnant women were originally selected with characteristics similar to those presented by the preeclamptic patients, including body mass index, gestational age, eliminated high blood pressure, kidney disease, diabetes and so on. Blood and placenta samplings were obtained from diagnosed patients after informed consent and approved by the Ethical Committee of the Medical Faculty of Tongji Medical College, Huazhong University of Science and Technology in accordance with the Declaration of Helsinki.
The patients had not taken any medications before specimen collection. Blood extracted from the pregnant women stood for 20 min at room temperature. After centrifugation, serum was collected and stored at −80 °C until use.
Animals and experimental protocol
Female Sprague–Dawley rats (10–12 weeks old, weighing 220–250 g) were purchased from the Experimental Animal Center of Tongji Medical College, Huazhong University of Science and Technology. Animals were housed individually in plastic cages with wood chips as bedding under pathogen-free conditions, in a controlled environment of temperature at 20–25 °C and 12 h cycles of light and dark. Rats were fed a standard laboratory diet and water ad libitum. Pregnancy was obtained by mating female rats with fertile male rats at a ratio of 2:1 overnight. Daily vaginal smears were observed, and appearance of spermatozoa in vaginal smear was defined as gestational day (GD) 1. All animal work was conducted according to the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health. All studies involving rats were approved by Animal Care and Use Committee of Huazhong University of Science and Technology.
Experimental protocol 1
Pregnant rats were randomly divided into control and treatment groups. Treatment rats were injected s.c. with Dex sodium phosphate (2.5 mg kg−1 per day) from GD7 to 13, while controls were injected s.c. with equal saline. On GD21 (pregnancy time=22 days), rats were fully anesthetized with chloral hydrate and placental specimens were rapidly extracted. Blood samples were drawn by heart puncture and centrifuged at 3000 r.p.m. for 20 min at 4 °C to obtain the serum.
Experimental protocol 2
Pregnant rats were injected s.c. with different doses of Dex sodium phosphate (1, 2.5, 5 and 10 mg kg−1) on GD13, while controls were injected s.c. with equal saline. At 24 h post Dex or saline injection, the rats were fully anesthetized with chloral hydrate, and the placenta, kidney and liver specimens were rapidly collected.
Experimental protocol 3
Pregnant rats were randomly divided into three groups: control; Dex; and Dex plus 1,25-(OH)2D3. From GD7 to 13, controls were injected s.c. with equal saline, rats in Dex group were injected s.c. with Dex sodium phosphate (2.5 mg kg−1 per day) and rats in Dex plus 1,25-(OH)2D3 group were injected with Dex sodium phosphate (2.5 mg kg−1 per day) s.c. as well as 1,25-(OH)2D3 (1.2 μg kg−1 per day) i.p. On GD21, rats were fully anesthetized with chloral hydrate and the uterus was removed and placed in a chilled dish. Placenta and pup were rapidly extracted. All of the pups and placentas were weighed, and litter size noted. Kidney was also removed. All samples were analyzed individually.
Here 2.5 mg kg−1 of Dex is selected because we referenced a previous report indicating that this dose could result in circulating GC levels in rats over time that reproduce the circulating levels of GC in rats observed during and after exposure to acute stress.26 Our previous work has also reported that this dose of Dex could induce PE development in pregnant rats.6 Moreover, 2.5 mg kg−1 of Dex was administered as we observed in the initial experiments that 1 mg kg−1 or lower doses of Dex was insufficient to significantly induce typical manifestations of PE in pregnant rats, while 5 mg kg−1 Dex contributed to fetal loss or death rather than PE development. A unit of 1.2 μg kg−1 of 1,25-(OH)2D3 per day is selected because we referenced a previous report indicating that 5 μg kg−1 every other day was safe and tolerated by the mice, having no major side effects while maintaining its activity.27 Importantly, the most advantage of 1,25-(OH)2D3 is its fast metabolic clearance in vivo.
Measurement of systolic blood pressure
At indicated time (initial non-pregnant status, GD3-5, GD14 and GD20), the systolic blood pressure was determined in conscious, restrained pregnant rats. An automated system with a photoelectric sensor linked to a dual channel recorder (BP-98A, Softron, Tokyo, Japan), tail cuff and sphygmomanometer was used to obtain indirect blood pressure measurements, which have been previously demonstrated to be closely correlated with direct arterial measurements.28 The measurements were repeated three times for each rat, with the mean value recorded.
Determination of urinary albumin excretion
For 24 h urine collection, on GD5 and GD20, the pregnant rats were placed in metabolic cages. To avoid contaminating the collected urine, rats were restricted from food; however, they were allowed free access to water. To avoid the adverse effects of fasting, rats were fed in other cages for 30 min every 6 h. Urine samples were centrifuged at 3000 r.p.m. for 20 min at room temperature, and the supernatant was collected for urinary albumin analysis. Urine protein concentrations were determined by using pyrogallol red in an automatic biochemical analyzer (ADVIA 2400 Chemistry System, Siemens Medical Solutions Diagnostics, Tarrytown, NY, USA).
Hematoxylin and eosin staining
For histological evaluation, placenta and kidney were fixed in neutral-buffered formalin. Hematoxylin and eosin staining was performed on 4 μm paraffin sections of placenta and kidney specimens for conventional morphological evaluation under light microscope (Olympus BX60, Tokyo, Japan).
Measurement of thiobarbituric acid reactive substances
Placental thiobarbituric acid reactive substances (TBARS) was measured by using a commercially available kit (QuantiChrom TBARS Assay Kit, DTBA-100) according to the manufacturer’s instruction (BioAssay Systems, Hayward, CA, USA). Briefly, placentas (~20 mg) were placed into 200 μl ice-cold phosphate-buffered saline with protease inhibitors. The tissues were first homogenized thoroughly and then sonicated for 20 s on ice. Samples were then centrifuged at 3000 r.p.m. for 10 min at 4 °C. A 20 μl aliquot was removed for protein analysis. The resultant absorbances were read at 535 nm. TBARS levels were expressed as nmol mg−1 protein.
Cell culture and treatment
Human first-trimester trophoblast cell line HPT-8 was kindly provided by Fourth Military Medical University (Xi’an, China). Cells were cultured at 37 °C in a humidified atmosphere with 5% CO2 in Dulbecco’s modified Eagle’s medium/F-12 medium supplemented with 10% heat-inactivated fetal bovine serum, 25 mm HEPES, 100 U ml−1 penicillin G and 100 U ml−1 streptomycin. Cells were treated with Dex (10−7 mol l−1), 1,25-(OH)2D3 (10−9 mol l−1) or Dex (10−7 mol l−1) plus 1,25-(OH)2D3 (10−9 mol l−1) for MTT cell proliferation assay, and Dex (10−6 mol l−1), 1,25-(OH)2D3 (10−9 mol l−1) or Dex (10−6 mol l−1) plus 1,25-(OH)2D3 (10−9 mol l−1) for Hoechst cell apoptosis assay.
Cell proliferation and apoptosis assay
Cell proliferation was determined by a colorimetric method based upon metabolic reduction of the soluble yellow tetrazolium dye MTT to its insoluble purple formazan. Approximately, 5000 cells per well were grown in 96-well plates and incubated overnight in 200 μl of culture medium. After cells were treated with indicated conditions for 24 h, each well was added with 20 μl MTT (0.5 mg ml−1) and incubated for 4 h before supernatant was removed. After plate was placed at 37 °C for 15 min in 150 μl dimethlysulfoxide, the absorbency was measured with a micro ELISA reader (Amersham Biosciences, Pittsburgh, PA, USA) at a wavelength of 492 nm.
Cell apoptosis was examined by Hoechst staining. Cells were incubated with the Hoechst dye for 15 min before examination under fluorescence microscope. Apoptotic cells were characterized by characteristic nuclear fragmentation; only those nuclei showing evidence of DNA fragmentation without plasma membrane damage were taken to be apoptotic cells.
RNA isolation and real-time PCR
Total RNA was isolated from placenta, kidney or liver using Trizol reagent (Life Technologies, Grand Island, NY, USA) according to the manufacturer’s protocol. The concentration and purity of RNA was determined by the ultraviolet spectrophotometer (Eppendorf, Hamburg, Germany). cDNA synthesis was performed using ReverTra Ace cDNA Synthesis kit (FSQ-101, TOYOBO, Osaka, Japan) according to the manufacturer’s instruction. Quantitative PCR analysis was carried out on a Bio-Rad CFX Connect Real-Time PCR Detection System using iTaq Universal SYBR Green Supermix (Bio-Rad Laboratories, Richmond, CA, USA). Each sample was quantified in triplicate (n=3). PCR conditions were 30 s at 95 °C, followed by 40 cycles of 10 s at 95 °C and 20 s at 60 °C. Data were analyzed using the Bio-Rad CFX Manager 2.1 software, and normalized to GAPDH. The sequences of primers were as follows: rat Cyp24a1, forward 5′-CCGCTGATGACAGACGGTGA-3′ and reverse 5′-TACTCTGCCAGCGTGTCGTG-3′; rat Cyp27b1, forward 5′-GCTAACGGCGGATGGTGAAG-3′ and reverse 5′-CCTTAGTCGTCGCACGAGGT-3′; rat Cyp3a1, forward 5′-TGGAGAAAGCCAAGAAGCTCTT-3′ and reverse 5′-TCATATACTGGCGTGAGGAATGG-3′; rat Pxr, forward 5′-GACGGCAGCATCTGGAACTAC-3′ and reverse 5′-TGATGACGCCCTTGAACATG-3′; rat Gapdh, forward 5′-GGCACAGTCAAGGCTGAGAATG-3′ and reverse 5′-ATGGTGGTGAAGACGCCAGTA-3′.
Western blotting
Nuclear protein of placental tissue was extracted using Nuclear and Cytoplasmic Protein Extraction Kit (Beyotime Institute of Biotechnology, Shanghai, China) for assessing HIF1A expression. Protein concentrations were determined using BCA protein assay kit (Pierce, Rockford, IL, USA). Then, regular western blotting assay was performed. Briefly, equal amounts of protein (40 μg) were subjected to 12% SDS-polyacrylamide gel electrophoresis electrophoresis and transferred to polyvinylidene fluoride membranes (Millipore, Billerica, MA, USA). The membranes were blocked with 5% (w/v) non-fat dried milk and incubated with primary antibodies overnight at 4 °C, followed by incubation with a secondary horseradish peroxidase-conjugated antibody. The bound antibody was detected by an enhanced chemiluminescence kit (Millipore) on X-ray film. Lamin B served as internal control.
Measurement of cortisol, 25(OH)D and 1,25-(OH)2D3
The levels of cortisol were detected by enzyme chemiluminescence immunoassay in chemiluminescence analyzer (ADVIA Centaur XP Immunoassay System, Siemens Healthcare Diagnostics Inc., Tarrytown, NY, USA). The concentrations of total 25(OH)D were measured by electrochemical luminescence immunoassay in chemiluminescence analyzer (Roche cobas e 601, Roche Diagnostics GmbH, Mannheim, Germany). 1,25-(OH)2D3 was determined using 1,25-(OH)2D3 ELISA kit (Uscn Life Science Inc., Wuhan, China) according to the manufacturer’s instructions.
Statistical analysis
All statistical analyses were done using the SPSS 19.0 software (IBM, Armonk, NY, USA). The results were expressed as means±s.e.m. of multiple independent experiments. The means of the different groups were compared by using either Student’s t-test or one-way analysis of variance1 followed by S–N–K post hoc test. A value of P<0.05 was considered significant.
Results
Upregulation of cortisol and downregulation of 1,25-(OH)2D3 in human PE
To determine whether GC and 1,25-(OH)2D3 are correlated with PE, we measured the levels of cortisol and 1,25-(OH)2D3 in serum and placenta of both normal pregnancy and PE women. As shown in Figure 1a, the levels of serum cortisol had no significant difference between PE and normal women, while the levels of placental cortisol in PE women showed significant increase compared to normal pregnancies (Figure 1b). As expected, serum 1,25-(OH)2D3 levels of PE women decreased significantly compared to normal pregnancies (Figure 1c). In line with this, placental 1,25-(OH)2D3 levels of PE women were significantly lower than those of normal pregnancies (Figure 1d). Furthermore, serum total 25-(OH)D levels of PE women decreased significantly compared to controls (Supplementary Figure 1). These clinical data suggest that cortisol activity is upregulated while 1,25-(OH)2D3 level is downregulated in human PE.
Expressions of cortisol and 1,25-(OH)2D3 in human preeclampsia (PE). (a) Serum cortisol levels in PE women; (b) placental cortisol levels in PE women; (c) serum 1,25-(OH)2D3 levels in PE women; (d) and placental 1,25-(OH)2D3 levels in PE women. The levels of cortisol were detected by enzyme chemiluminescence immunoassay. 1,25-(OH)2D3 was determined by enzyme-linked immunosorbent assay. Results are expressed as means±s.e.m. (n=13 in control and PE group). *P<0.05 and **P<0.01 vs. control group, two-tailed Student’s t-test.
GC downregulates 1,25-(OH)2D3 in experimental PE rats
To confirm the involvement of GC/1,25-(OH)2D3 axis in the pathogenesis of PE, we detected the 1,25-(OH)2D3 levels of both serum and placenta in GC-mediated rat PE. As shown in Figures 2a and b, 1,25-(OH)2D3 of both serum and placenta were strikingly downregulated by Dex in experimental PE rats. Furthermore, Dex significantly decreased serum total 25-(OH)D levels of experimental PE rats compared to controls (Supplementary Figure 2). These results suggest that GC exposure may result in PE via inhibiting 1,25-(OH)2D3 expression.
Glucocorticoid downregulates 1,25-(OH)2D3 levels in experimental preeclampsia rats. Rats were treated with Dex according to Experimental protocol 1. (a) Effect of dexamethasone (Dex) on serum 1,25-(OH)2D3 levels in pregnant rats; and (b) effect of Dex on placental 1,25-(OH)2D3 levels in pregnant rats. 1,25-(OH)2D3 levels were determined by enzyme-linked immunosorbent assay. Results are expressed as means±s.e.m. (n=7 rats in each group). *P<0.05 and **P<0.01 vs. control group, two-tailed Student’s t-test.
GC disturbs 1,25-(OH)2D3 synthesis and catabolism in pregnant rats
To explore related molecular mechanisms underlying the effects of GC on 1,25-(OH)2D3 levels, we detected the expressions of Cyp24a1, Cyp27b1, Pxr and Cyp3a1 in liver, kidney and placenta of pregnant rats after GC treatment. As shown by real-time PCR in Figure 3a, the mRNA expressions of liver Cyp24a1 and Pxr were strikingly downregulated by Dex, while liver Cyp27b1 and Cyp3a1 expressions were strikingly upregulated by Dex in pregnant rats. Downregulation of Cyp24a1 and upregulation of Cyp27b1 and Cyp3a1 were observed in kidney of Dex-treated pregnant rats (Figure 3b). The mRNA expressions of placental Cyp24a1, Pxr and Cyp3a1 were enhanced by Dex in pregnant rats (Figure 3c). Therefore, GC-mediated disturbance of 1,25-(OH)2D3-synthesizing and -catabolizing enzymes may be the reason for lower levels of 1,25-(OH)2D3 in PE.
Glucocorticoid disturbs 1,25-(OH)2D3-synthesizing and -catabolizing enzymes in pregnant rats. Rats were treated with dexamethasone (Dex) according to Experimental protocol 2. (a) Effect of Dex on Cyp24a1, Cyp27b1, Pxr and Cyp3a1 gene expression in liver of pregnant rats; (b) effect of Dex on Cyp24a1, Cyp27b1, Pxr and Cyp3a1 gene expression in kidney of pregnant rats; and (c) effect of Dex on Cyp24a1, Cyp27b1, Pxr and Cyp3a1 gene expression in placenta of pregnant rats. Gene expression was detected by real-time PCR. Results are expressed as means±s.e.m. (n=7 rats in each group). *P<0.05, **P<0.01 and ***P<0.001, one-way analysis of variance with S–N–K post test.
1,25-(OH)2D3 treatment improves symptoms of GC-mediated rat PE
To validate the involvement of GC/1,25-(OH)2D3 axis in the pathogenesis of PE, a GC-induced rat PE model was constructed as previously,8 and, meanwhile, the rat PE model was treated with 1,25-(OH)2D3. As shown in Figure 4a, systolic blood pressure was significantly elevated after Dex exposure, while blood pressure conditions were obviously improved relative to Dex group after 1,25-(OH)2D3 treatment, but they could not be dropped to the control levels. The urine protein level was significantly higher in Dex group on GD20, and 1,25-(OH)2D3 treatment significantly reduced the excretion of urine protein (Figure 4b). The fetal and placental weight of Dex group was significantly lower than that of control and 1,25-(OH)2D3 groups (Figure 4c). In addition, Dex-treated rats displayed significant structural abnormalities in placenta and kidney characterized by thickening of vessel walls in labyrinth and glomerular endotheliosis, while 1,25-(OH)2D3 treatment significantly ameliorated placental and renal impairment (Figure 4d). These data suggest that 1,25-(OH)2D3 is effective in relieving rat PE-related symptoms induced by GC.
1,25-(OH)2D3 ameliorates the symptoms of glucocorticoid-mediated rat preeclampsia. Rats were treated with dexamethasone (Dex) according to Experimental protocol 3. Systolic blood pressure (SBP), 24 h urinary protein excretion and fetal and placental weight are presented in a–c, respectively. Results are expressed as means±s.e.m. (n=7 rats in each group). **P<0.01 and ***P<0.001 vs. control group, †P<0.05 vs. Dex group, one-way analysis of variance with S–N–K post test. (d) Effect of 1,25-(OH)2D3 on Dex-mediated placental and renal impairment. Representative hematoxylin and eosin staining images of placenta and kidney are showed, the magnification is × 400, bar=50 μm. A full color version of this figure is available at the Hypertension Research journal online.
1,25-(OH)2D3 treatment ameliorates placental oxidative stress of GC-mediated rat PE
To further address the question of how 1,25-(OH)2D3 prevents GC-mediated PE, the focus was turned to placental oxidative impairment. Placenta oxidative impairment is the fundamental abnormality leading to PE.29 HIF1A, overexpressed in hypoxic placentas of preeclamptic women, is implicated in the pathogenesis of PE.1, 2, 30 On GD21, levels of placental oxidative impairment and HIF1A expression were detected by TBARS assay kit and western blotting respectively. As shown in Figure 5a, Dex administration resulted in increased placental TBARS levels, suggesting placental oxidative damage. HIF1A was overexpressed in placenta of Dex-treated rats vs. controls (Figure 5b). But after 1,25-(OH)2D3 treatment, both placental TBARS level and HIF1A expression were downregulated (Figures 5a and b).
1,25-(OH)2D3 improves placental oxidative stress of glucocorticoid-mediated rat preeclampsia. Rats were treated with dexamethasone (Dex) according to Experimental protocol 3. (a) Effect of 1,25-(OH)2D3 on Dex-mediated placental lipid peroxidation. Levels of lipid peroxidation were determined by using a commercially available thiobarbituric acid reactive substances (TBARS) kit. The measurements of lipid peroxidation represent the degree of placental oxidative stress. Results are expressed as means±s.e.m. (n=7 rats in each group). (b) Effect of 1,25-(OH)2D3 on Dex-mediated placental HIF1A expression. HIF1A was detected by western blotting. The histogram represents means±s.e.m. of the densitometric scans for protein bands (n=7 rats in each group), normalized by comparison with Lamin B and expressed as a percentage of control. ***P<0.001 vs. control group, ††P<0.01 and †††P<0.001 vs. Dex group, one-way analysis of variance with S–N–K post test.
1,25-(OH)2D3 antagonizes the effects of GC on trophoblast proliferation and apoptosis in vitro
Dex significantly decreased the proliferation of trophoblast cell line HPT-8, while Dex triggered HPT-8 apoptosis in vitro (Figures 6a and b). Importantly, 1,25-(OH)2D3 treatment antagonized the effects of Dex on HPT-8 proliferation and apoptosis (Figures 6a and b). These results suggest that 1,25-(OH)2D3 could antagonize the inhibitory effects of Dex on trophoblast development in vitro, supporting the protective actions of 1,25-(OH)2D3 on trophoblast against GC.
1,25-(OH)2D3 antagonizes the effects of glucocorticoid on trophoblast proliferation and apoptosis in vitro. HPT-8 cells were treated with dexamethasone (Dex; 10−7 mol l−1), 1,25-(OH)2D3 (10−9 mol l−1) or Dex (10−7 mol l−1) plus 1,25-(OH)2D3 (10−9 mol l−1) for 24 h in proliferation assay (a) and treated with Dex (10−6 mol l−1), 1,25-(OH)2D3 (10−9 mol l−1) or Dex (10−6 mol l−1) plus 1,25-(OH)2D3 (10−9 mol l−1) for 24 h in apoptosis assay (b). (a) 1,25-(OH)2D3 reverses the inhibitory effect of Dex on HPT-8 proliferation; and (b) 1,25-(OH)2D3 inhibits the promotion effect of Dex on HPT-8 apoptosis. Results are expressed as means±s.e.m. from six independent experiments. ***P<0.001 vs. control group, ††P<0.01 and †††P<0.001 vs. Dex group, one-way analysis of variance with S–N–K post test.
Discussion
To date, the molecular mechanisms underlying PE remain elusive. Our data support that GC/1,25-(OH)2D3 axis might be a common pathway through which PE occurs. The present study provides evidence that GC might result in PE via downregulating 1,25-(OH)2D3, an endogenous protective mediator during pregnancy. Our results also reveal the molecular mechanism underlying the effect of GC on 1,25-(OH)2D3.
This study first revealed novel findings regarding the GC levels and 1,25-(OH)2D3 concentrations in serum and placenta of PE women. The serum cortisol levels of PE women had an increase (not significant), while the placental cortisol levels showed significant increase compared to normal pregnancies. In contrary, 1,25-(OH)2D3 levels of both serum and placenta decreased significantly in PE women compared to controls. These clinical data suggest the increase of GC activity and decrease of 1,25-(OH)2D3 levels in PE. Hence, this study reports the clinical data of involvement of GC/1,25-(OH)2D3 in PE.
Accumulating evidence suggest the adverse effects of stress and GC exposure on pregnancy.7, 10, 11, 31 Previous works reported that stress could induce PE in pregnant rats and women.7, 9 We demonstrated recently that GC exposure in early placentation could lead to PE-related manifestations in pregnant rats,6 supporting that GC exposure is a potential stimulus for PE development. Here GC-treated pregnant rats were characterized by reduced 1,25-(OH)2D3 expression, suggesting these symptoms may have occurred, at least in part, in response to 1,25-(OH)2D3 downregulation caused by GC as 1,25-(OH)2D3 is an endogenous protective mediator during pregnancy. In fact, 1,25-(OH)2D3 concentrations of both serum and placenta were strikingly downregulated by GC in experimental PE rats.
The biosynthesis and degradation of 1,25-(OH)2D3 is controlled by several enzymes. CYP24A1 is important in the catabolism of 1,25-(OH)2D3, while CYP27B1 is involved in its biosynthesis. PXR/CYP3A1 also has the dominant role in hydroxylation of 1,25-(OH)2D3. To clarify the effects of GC on 1,25-(OH)2D3-synthesizing and -catabolizing enzymes, we studied the expressions of Cyp24a1, Cyp27b1, Pxr and Cyp3a1 in liver, kidney and placenta of GC-treated pregnant rats systematically. The results showed that GC downregulated the expressions of Cyp24a1 and Pxr, while enhanced Cyp27b1 and Cyp3a1 expressions in liver of pregnant rats. Moreover, downregulation of Cyp24a1 and upregulation of Cyp27b1 and Cyp3a1 were observed in kidney of GC-treated pregnant rats. Furthermore, the expressions of placental Cyp24a1, Pxr and Cyp3a1 were enhanced by GC. Therefore, GC-mediated enhancement of liver and renal Cyp3a1 expression, not Cyp24a1, may be the dominant reason for lower serum 1,25-(OH)2D3 levels in PE, which is supported by previous findings.19 Here both liver and renal Cyp27b1 expressions were upregulated by GC, the reason of which may be the remove of 1,25-(OH)2D3-mediated inhibition on Cyp27b1 promoter. It is also possible that secondary to the 1,25-(OH)2D3 degeneration, Cyp27b1 upregulation observed here may occur as a compensatory response against 1,25-(OH)2D3 reduction. Further studies are planned to investigate the detailed reasons. Indeed, a previous report demonstrated that Dex induces the rat hepatic CYP27 gene expression.32 However, GC-mediated enhancement of placental Cyp24a1 and Pxr/Cyp3a1 expression may represent the main reason for local decrease of 1,25-(OH)2D3 levels in PE placenta. Plasma concentrations of 1,25-(OH)2D3 are tightly controlled via feedback regulation of renal CYP27B1 and CYP24A1, while placenta-specific methylation of the CYP24A1 gene occurs in pregnancy.33 Our findings may suggest that epigenetic regulation of CYP24A1 by GC has an important role in disturbing 1,25-(OH)2D3 bioavailability at the fetomaternal interface. Taken together, GC decrease 1,25-(OH)2D3 via modulating the expressions of Cyp24a1, Cyp27b1, Pxr and Cyp3a1 in liver, kidney and placenta differentially.
In this study, Dex exposure contributed to hypertension, proteinuria, restricted placenta and fetus, placental abnormalities and renal impairment, all classic hallmarks of PE. Interestingly, 1,25-(OH)2D3 supplementation significantly improved PE-related manifestations in Dex-induced PE rats, suggesting the effectiveness of 1,25-(OH)2D3 in relieving symptoms of GC-mediated PE. Furthermore, 1,25-(OH)2D3 treatment ameliorated placental oxidative stress in GC-mediated rat PE. Placenta oxidative stress is the fundamental abnormality leading to PE.29 We demonstrated here decreased placental oxidative stress after 1,25-(OH)2D3 treatment in Dex-mediated rat PE model that may support the protective effects of 1,25-(OH)2D3 against adverse actions of GC on placental function. HIF1A, overexpressed in hypoxic placentas of preeclamptic women, is implicated in the pathogenesis of PE.1, 2, 30 Importantly, we reported that 1,25-(OH)2D3 treatment could inhibit HIF1A overexpression in Dex-treated placenta. Here 1,25-(OH)2D3-mediated inhibition of HIF1A in Dex-treated placenta provides an important mechanistic explanation for the antagonism of 1,25-(OH)2D3 on GC in PE.
We demonstrated that Dex could inhibit trophoblast proliferation while promote trophoblast apoptosis in vitro. However, 1,25-(OH)2D3 antagonized the effects of Dex on trophoblast proliferation and apoptosis. These results demonstrate that 1,25-(OH)2D3 could antagonize the inhibitory effects of Dex on trophoblast development, supporting the protective actions of 1,25-(OH)2D3 against GC in placentation, providing another important mechanistic explanation for the counterregulation of 1,25-(OH)2D3 on GC in PE placenta.
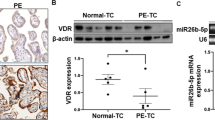
By using clinical data, the present study first showed the involvement of GC/1,25-(OH)2D3 in human PE. Furthermore, relying on the results gathered by using rat model and trophoblast model, the study provides evidence that GC/1,25-(OH)2D3 axis is involved in the pathogenesis of PE. However, PE is thought to be a multifactorial disorder, involving complicated mechanisms in its pathogenesis. A common pathophysiology of PE is endothelial dysfunction and angiogenic/angiostatic imbalance, involving sFlt-1, PIGF and sEng.34 In addition, a recent report showed that PE onset is associated with visfatin polymorphisms and levels.35 Interestingly, 1,25-(OH)2D3 receptor VDR has been demonstrated to be linked to the development of PE.36 Therefore, this study just proposes one of the important mechanisms underlying the occurrence of PE. It is also noteworthy that there may be other causative factors in addition to dysregulated 1,25-(OH)2D3 that are responsible for Dex-induced PE, and may act in concert to stimulate placental oxidative stress, HIF1A overexpression and PE development reported in the present study. In the study, rat was selected as the animal model to study whether Dex could induce PE-related symptoms. It is reasonable for us to conclude that GC exposure is a potential cause for PE development in rat. However, further studies are needed to study other potential molecular pathways, and, meanwhile, confirm whether GC-induced PE is rodent specific or not. Clinically, Dex is used to improve hellp syndrome in PE women, but increasing evidence indicates that Dex has several side effects and even aggravates clinical conditions after withdrawal. In fact, our previous work confirmed that prior exposure to Dex could induce PE development in rats.6 Here we further found that Dex exposure induces PE via dampening 1,25-(OH)2D3 by using this model.
In conclusion, relying on the results gathered by using GC-mediated rat PE model and in vitro trophoblast model, the present study provides further evidence that GC/1,25-(OH)2D3 axis is involved in the pathogenesis of PE. This study proposes a common mechanism underlying the occurrence of PE, providing new insights into the understanding of PE. Our data suggest that the avoidance of stress/GC exposure and administration of 1,25-(OH)2D3 might be potential strategies to prevent PE, and also contribute to develop other potential therapeutic strategies in preventing PE.
References
Young BC, Levine RJ, Karumanchi SA . Pathogenesis of preeclampsia. Annu Rev Pathol 2010; 5: 173–192.
Noris M, Perico N, Remuzzi G . Mechanisms of disease: pre-eclampsia. Nat Clin Pract Nephrol 2005; 1: 98–114.
Redman CW, Sargent IL . Latest advances in understanding preeclampsia. Science 2005; 308: 1592–1594.
Klonoff-Cohen HS, Cross JL, Pieper CF . Job stress and preeclampsia. Epidemiology 1996; 7: 245–249.
Xu Z, Zhao F, Lin F, Xiang H, Wang N, Ye D, Huang Y . Preeclampsia is associated with a deficiency of lipoxin A4, an endogenous anti-inflammatory mediator. Fertil Steril 2014; 102: 282–290.
Zhang D, Liu H, Zeng J, Miao X, Huang W, Chen H, Huang Y, Li Y, Ye D . Glucocorticoid exposure in early placentation induces preeclampsia in rats via interfering trophoblast development. Gen Comp Endocrinol 2016; 225: 61–70.
László KD, Liu XQ, Svensson T, Wikström AK, Li J, Olsen J, Obel C, Vestergaard M, Cnattingius S . Psychosocial stress related to the loss of a close relative the year before or during pregnancy and risk of preeclampsia. Hypertension 2013; 62: 183–189.
Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O . Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol 2000; 95: 487–490.
Takiuti NH, Kahhale S, Zugaib M . Stress in pregnancy: a new Wistar rat model for human preeclampsia. Am J Obstet Gynecol 2002; 186: 544–550.
Xu Z, Zhao J, Zhang H, Ke T, Xu P, Cai W, Katirai F, Ye D, Huang Y, Huang B . Spontaneous miscarriages are explained by the stress/glucocorticoid/lipoxin A4 axis. J Immunol 2013; 190: 6051–6058.
Lin F, Yu X, Zhang X, Guo Y, Huang Y, Zhou J, Zeng P, Ye D, Huang Y . A synthetic analog of lipoxin A4 partially alleviates dexamethasone-induced fetal growth restriction in rats. Placenta 2013; 34: 941–948.
Liu NQ, Hewison M . Vitamin D, the placenta and pregnancy. Arch Biochem Biophys 2012; 523: 37–47.
Lapillonne A . Vitamin D deficiency during pregnancy may impair maternal and fetal outcomes. Med Hypotheses 2010; 74: 71–75.
Robinson CJ, Alanis MC, Wagner CL, Hollis BW, Johnson DD . Plasma 25-hydroxyvitamin D levels in early-onset severe preeclampsia. Am J Obstet Gynecol 2010; 203: e361–e366.
Halhali A, Tovar AR, Torres N, Bourges H, Garabedian M, Larrea F . Preeclampsia is associated with low circulating levels of insulin-like growth factor I and 1,25-dihydroxyvitamin D in maternal and umbilical cord compartments. J Clin Endocrinol Metab 2000; 85: 1828–1833.
Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM . Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab 2007; 92: 3517–3522.
Díaz L, Arranz C, Avila E, Halhali A, Vilchis F, Larrea F . Expression and activity of 25-hydroxyvitamin D-1 alpha-hydroxylase are restricted in cultures of human syncytiotrophoblast cells from preeclamptic pregnancies. J Clin Endocrinol Metab 2002; 87: 3876–3882.
Barry EL, Rees JR, Peacock JL, Mott LA, Amos CI, Bostick RM, Figueiredo JC, Ahnen DJ, Bresalier RS, Burke CA, Baron JA . Genetic variants in CYP2R1, CYP24A1, and VDR modify the efficacy of vitamin D3 supplementation for increasing serum 25-hydroxyvitamin D levels in a randomized controlled trial. J Clin Endocrinol Metab 2014; 99: E2133–E2137.
Zhou C, Assem M, Tay JC, Watkins PB, Blumberg B, Schuetz EG, Thummel KE . Steroid and xenobiotic receptor and vitamin D receptor crosstalk mediates CYP24 expression and drug-induced osteomalacia. J Clin Invest 2006; 116: 1703–1712.
Gupta RP, He YA, Patrick KS, Halpert JR, Bell NH . CYP3A4 is a vitamin D-24- and 25-hydroxylase: analysis of structure function by site-directed mutagenesis. J Clin Endocrinol Metab 2005; 90: 1210–1219.
Ejiri N, Katayama KI, Nakayama H, Doi K . Expression of cytochrome P450 (CYP) isozymes in rat placenta through pregnancy. Exp Toxicol Pathol 2001; 53: 387–391.
Khan AA, Chow EC, van Loenen-Weemaes AM, Porte RJ, Pang KS, Groothuis GM . Comparison of effects of VDR versus PXR, FXR and GR ligands on the regulation of CYP3A isozymes in rat and human intestine and liver. Eur J Pharm Sci 2009; 37: 115–125.
Shi D, Yang D, Yan B . Dexamethasone transcriptionally increases the expression of the pregnane X receptor and synergistically enhances pyrethroid esfenvalerate in the induction of cytochrome P450 3A23. Biochem Pharmacol 2010; 80: 1274–1283.
Wang Z, Lin YS, Dickmann LJ, Poulton EJ, Eaton DL, Lampe JW, Shen DD, Davis CL, Shuhart MC, Thummel KE . Enhancement of hepatic 4-hydroxylation of 25-hydroxyvitamin D3 through CYP3A4 induction in vitro and in vivo: implications for drug-induced osteomalacia. J Bone Miner Res 2013; 28: 1101–1116.
Higgins JR, de Swiet M . Blood-pressure measurement and classification in pregnancy. Lancet 2001; 357: 131–135.
Frank MG, Miguel ZD, Watkins LR, Maier SF . Prior exposure to glucocorticoids sensitizes the neuroinflammatory and peripheral inflammatory responses to E. coli lipopolysaccharide. Brain Behav Immun 2010; 24: 19–30.
Mathieu C, Laureys J, Sobis H, Vandeputte M, Waer M, Bouillon R . 1,25-Dihydroxyvitamin D3 prevents insulitis in NOD mice. Diabetes 1992; 41: 1491–1495.
Mulvany MJ, Halpern W . Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 1977; 41: 19–26.
Redman CW, Sargent IL . Placental debris, oxidative stress and pre-eclampsia. Placenta 2000; 21: 597–602.
Tal R . The role of hypoxia and hypoxia-inducible factor-1alpha in preeclampsia pathogenesis. Biol Reprod 2012; 87: 134.
Michael AE, Papageorghiou AT . Potential significance of physiological and pharmacological glucocorticoids in early pregnancy. Hum Reprod Update 2008; 14: 497–517.
Mullick J, Anandatheerthavarada HK, Amuthan G, Bhagwat SV, Biswas G, Camasamudram V, Bhat NK, Reddy SE, Rao V, Avadhani NG . Physical interaction and functional synergy between glucocorticoid receptor and Ets2 proteins for transcription activation of the rat cytochrome P-450c27 promoter. J Biol Chem 2001; 276: 18007–18017.
Novakovic B, Sibson M, Ng HK, Manuelpillai U, Rakyan V, Down T, Beck S, Fournier T, Evain-Brion D, Dimitriadis E, Craig JM, Morley R, Saffery R . Placenta-specific methylation of the vitamin D 24-hydroxylase gene: implications for feedback autoregulation of active vitamin D levels at the fetomaternal interface. J Biol Chem 2009; 284: 14838–14848.
Ohkuchi A, Hirashima C, Takahashi K, Suzuki H, Matsubara S . Prediction and prevention of hypertensive disorders of pregnancy. Hypertens Res 2017; 40: 5–14.
Luizon MR, Belo VA, Palei AC, Amaral LM, Lacchini R, Sandrim VC, Duarte G, Cavalli RC, Tanus-Santos JE . Effects of NAMPT polymorphisms and haplotypes on circulating visfatin/NAMPT levels in hypertensive disorders of pregnancy. Hypertens Res 2015; 38: 361–366.
Zhan Y, Liu M, You Y, Zhang Y, Wang J, Wang X, Liu S, Liu X . Genetic variations in the vitamin-D receptor (VDR) gene in preeclampsia patients in the Chinese Han population. Hypertens Res 2015; 38: 513–517.
Acknowledgements
We acknowledge Professor Yinping Huang (First Affiliated Hospital, Wenzhou Medical University) for expert assistance in manuscript preparation. This work was supported by the National Natural Science Foundation of China (Grant No. 81671480, 81701469), Natural Science Foundation of Hubei Province (Grant No. 2015CFB179) and Young and Mid-Aged Key Medical Personnel Training Project of Wuhan City (Grant No. 2016-59).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Zhang, D., Zeng, J., Miao, X. et al. Glucocorticoid exposure induces preeclampsia via dampening 1,25-dihydroxyvitamin D3. Hypertens Res 41, 104–111 (2018). https://doi.org/10.1038/hr.2017.98
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.98
Keywords
This article is cited by
-
Association of serum 25-hydroxyvitamin D levels with primary hypertension: a study from south India
Hypertension Research (2020)