Abstract
Mean platelet volume (MPV) is increased in various cardiovascular diseases. We sought to determine the prognostic value of MPV for hypertension. We performed a retrospective cohort study. Baseline characteristics were measured in 9168 individuals without hypertension, and the follow-up period was 9 years. Hypertension was confirmed in 2881 participants during the follow-up period. When the participants were grouped according to MPV quartiles, the hazard ratio of future hypertension gradually increased across the MPV quartiles. The hazard ratios of hypertension for the II, III and IV (high) vs. I (low) quartiles of MPV were 1.13 (95% confidence interval (CI) 1.01–1.25, P=0.027), 1.25 (95% CI 1.12–1.39, P<0.001) and 1.40 (95% CI 1.26–1.55, P<0.001), respectively. In multivariate Cox regression analysis, MPV predicted hypertension independently of age, sex, platelet count, waist circumference, drinking, systolic blood pressure and creatinine levels. The present study indicated that elevated MPV is associated with increased incidence of hypertension independent of other risk factors, which suggests that platelet activity may play a role in hypertension incidence.
Similar content being viewed by others
Introduction
Platelet activity plays an essential role in atherothrombosis, the principal risk of most cardiovascular diseases.1 The pathogenesis of occlusive arterial disease involves platelet activation at thrombus lesion sites, pathological exaggeration and dysregulation through the mechanisms involved in the protection of hemostasis.1 Anti-platelet drugs have been widely used in the clinical treatment of cardiovascular and cerebrovascular diseases and have been demonstrated to be very effective at reducing adverse outcomes such as myocardial infarction, stroke and death.1 Mean platelet volume (MPV) is a marker of platelet size in complete blood counts and reflects platelet activity.2 In past decades, the association between elevated MPV and increased cardiovascular events has been demonstrated by a number of studies.3
Hypertension affects more than one-quarter of Chinese individuals and is the one of the leading causes of stroke and death.4 The incidence of hypertension has dramatically risen in recent years, especially in the middle-aged and elderly populations, posing an enormous economic and medical care burden on both society and the national medical insurance system. The main risk factors for hypertension have been identified as genetics, the environment, endocrine,5 mental stress, obesity, poor diet, drinking habits, sex, ethnicity and age. However, the role of platelet activation in cardiovascular events has led us to speculate that it may be associated with hypertension. In fact, previous studies have found elevated MPV values in resistant hypertension6 and non-dipper hypertension.7 However, whether an elevated MPV can independently predict future risk for hypertension has not been noted in the literature. In the present study, we evaluated whether elevated MPV could independently predict future risk for hypertension.
Methods
Study participants
The investigation is an ongoing cohort study. This investigation was approved by Zhenhai Lianhua Hospital Medical Science Research Ethics Committee. Written informed consent was received from all participants. The study participants include community residents. The individuals were consecutively referred to our hospital for annual routine medical checkups from January 2006 to December 2015. Between January 2006 and December 2006, a total of 12 707 individuals, including 8425 men and women 4282 aged 19–87 years (median of 44 years), self-reported their personal health information, including medical history, family history, smoking status and alcohol consumption. Then, their height, weight and blood pressure were measured, and blood specimens were provided for hematological and biochemical testing. A family history of hypertension was defined as having a father or mother with hypertension.
Of the 12 707 candidate participants, a total of 3539 were excluded due to one or more of the following conditions: (1) self-reported hypertension, use of antihypertensive medication or hypertension diagnosed by routine medical check-up at baseline (n=1874); (2) platelet count <100 × 109 l−1 or >350 × 109 l−1 (n=231); (3) serious illness (n=35); (4) loss during follow-up (n=751); and (5) missing values for any covariates of interest (n=742). After exclusion, the study cohort consisted of 9168 individuals, including 5980 men and 3188 women aged 20–87 years (median of 42 years).
Over the next 9 years, the participants who were diagnosed with hypertension by their attending physician at their annual routine medical checkups had their diagnoses confirmed. According to Chinese guidelines for the management of hypertension, hypertension was defined as systolic blood pressure (SBP) of 140 mm Hg or higher and diastolic blood pressure of 90 mm Hg or higher. Participants who had an SBP of 140 mm Hg or higher or diastolic blood pressure of 90 mm Hg or higher but denied having hypertension were scheduled for a repeat measurement.
The hospital record room and the Department of Chronic Non-communicable Diseases were contacted for the available supporting documentation. Some participants were confirmed as having prevalent hypertension or initiated antihypertensive medication, and participants who were confirmed to have secondary hypertension were excluded.
Laboratory procedures
The laboratory procedures and methods have previously been described elsewhere.8, 9 Hematological testing was performed on the Advia 120 (Bayer Diagnostics, Newbury, UK), an automated hematology analyzer. Biochemical parameters (glucose, total cholesterol, triglycerides, high-density lipoprotein cholesterol, uric acid and creatinine) were evaluated by enzymatic techniques in an AU640 Olympus Auto Analyzer (Olympus, Tokyo, Japan).
Height, weight and waist circumference were measured at the screening center by two trained nurses, and body mass index was equal to weight divided by squared height (kg m−2). An Omron HEM-1000 (OMRON, Dalian, China) was used to measure blood pressure after the subjects rested for 5 min in a sitting position in a quiet room.
Statistical analysis
Data were expressed as the median (25th–75th) or counts. For normality tests, skewed variables (triglycerides) were logarithmically transformed to improve normality prior to analysis. Normally distributed continuous variables were compared by one-way ANOVA (followed by the least significant difference test for multiple comparisons between groups). For categorical variables, the differences between groups were examined using the χ2 test. Cox proportional hazards regression was used to determine the incidence of hypertension. Potential confounding factors such as sex, age, waist circumference, drinking status, platelet count, SBP and creatinine levels were used as covariates in the Cox model. Potential interactions between exposure variables were tested by interaction terms in the Cox models. Statistical analyses were performed using the statistical package SPSS version 19.0 (SPSS, Chicago, IL, USA). The level of statistical significance was set at P<0.05.
Results
Based on the MPV values, the participants were categorized into quartiles, and the baseline characteristics of this investigation are presented in Table 1. Age and the percentage of women increased as MPV increased. Accordingly, the percentage of smoking and drinking as well as creatinine concentrations decreased as MPV increased. Individuals in the highest MPV quartile had higher mean SBP, diastolic blood pressure, and glucose and total cholesterol concentrations than individuals in the lowest MPV quartile; they also had the highest percentage of hyperlipidemia and diabetes. Body mass index, waist circumference and triglyceride levels were not significantly different among the MPV quartiles.
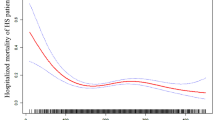
A total of 2881 subjects were identified as new hypertensive patients during follow-up. As expected, those who developed hypertension had higher MPV (10.7 (10.0–11.7) vs. 10.5 (9.8–11.5) fl), SBP (126 (119–132) vs. 114 (107–122) mm Hg) and diastolic blood pressure (80 (75–85) vs. 73 (68–78) mm Hg) at baseline; all P-values <0.001.
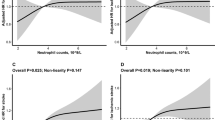
The incidence of hypertension was significantly higher in subjects with high MPV at baseline (Figure 1). Similar results were found when the participants were stratified by age (<60 and ⩾60 years; Figure 2).
The hazard ratio (HR) for future hypertension steadily increased across the MPV quartiles. The HRs for hypertension in quartiles II, III and IV vs. quartile I of MPV were 1.13 (95% confidence interval (CI) 1.01–1.25, P=0.027), 1.25 (95% CI 1.12–1.39, P<0.001) and 1.40 (95% CI 1.26–1.55, P<0.001), respectively. Data are shown in Table 2. The HR between MPV and the incidence of hypertension remained significant after adjustments for age, sex, waist circumference, drinking status, platelet count, and SBP and creatinine levels (HR=1.30, 95% CI 1.13–1.48, P<0.001).
There was a significant interaction between MPV and age at baseline. We determined the HR for incident hypertension among participants with an age < or ⩾60 years. As shown in Figure 3, after adjustments for the above-mentioned risk factors, the HRs for hypertension in quartiles II, III and IV relative to the HR in quartile I in the under-60 year subgroup were 1.16 (95% CI 1.02–1.33, P=0.028), 1.16 (95% CI 1.01–1.33, P=0.036) and 1.24 (95% CI 1.07–1.44, P=0.004), respectively, and the HRs for hypertension in the ⩾60-year subgroup were 1.05 (95% CI 0.82–1.34, P=0.692), 1.30 (95% CI 1.02–1.65, P=0.033) and 1.35 (95% CI 1.07–1.70, P=0.014), respectively.
Since elevated MPV is associated with a decrease in platelet count, the association between platelet count and hypertension was evaluated. Sex, age, waist circumference, drinking status, and SBP and creatinine levels were used as covariates in the Cox model, after adjustment for the above-mentioned risk factors, the HRs for hypertension in quartiles II (164–193 × 109 l−1), III (194–227 × 109 l−1) and IV (228–350 × 109 l−1) relative to the HR in quartile I (100–164 × 109 l−1) of the platelet count were 1.04 (95% CI 0.92–1.17, P=0.515), 1.07 (95% CI 0.95–1.20, P=0.270) and 1.12 (95% CI 0.99–1.26, P=0.055), respectively. The association between MPV and hypertension was investigated within the quartiles of platelet count (Table 3). After adjustment for the above-mentioned risk factors, the highest MPV was significantly related to an increased incidence of hypertension, although this difference had only borderline significance in the highest platelet count subgroup.
Discussion
In the current investigation, individuals with elevated MPV values had a significantly higher risk of developing hypertension during the 9-year follow-up period. The difference remains significant even after adjusting for multivariate confounding factors.
Many indexes of platelet function have appeared as underlying prognostic markers of cardiovascular disease. However, most of the techniques used to analyze platelet activity are costly and time-consuming, and require specialized techniques.10 In contrast to these methods, an approach considering MPV could be easily and cheaply made available. Elevated MPV indicates the presence of larger, more reactive platelets.2 Larger and activated platelets secrete more prothrombotic material and express more substances than small platelets, which accelerate the formation of thrombus and increase the risk for several diseases. In fact, over the past decade, an accumulating body of evidence has demonstrated that MPV is a predictive marker for stroke11 and coronary artery disease.12
Platelet count and platelet parameters such as platelet distribution width are usually measured along with MPV, and significant differences have been observed in thrombosis and cardiovascular events as well as MPV.13, 14 However, no reports concerning these two indices have been found for hypertension. Compared with platelet count and platelet distribution width, MPV seems to be very stable and has more associated discoveries in recent studies. Martin et al.15 found that MPV remains unchanged in patients with acute myocardial infarction at 6 weeks after treatment, indicating that MPV is less susceptible to short-term health conditions and treatment. Furthermore, platelet inhibitors such as aspirin have not been found to affect MPV.16, 17 Hypoglycemic or hypolipidemic decreases the MPV as well as plasma glucose level18 or cholesterol levels.19 Hundreds of participants of this study are taking hypoglycemic agent or hypolipidemic agent, may decrease the association between MPV and hypertension incidence, because individuals with diabetes or dyslipidemia have higher hypertension incidence even on treat. Changes in MPV are chronic rather than abrupt, which is another indication that it correlates with chronic diseases such as hypertension.
To the best of our knowledge, this study is the first to examine the association between MPV and hypertension incidence in a large cohort. Several previous studies have reported that MPV seems to be correlated with hypertension. A small case–control study has reported higher MPV in individuals with hypertension compared with those with prehypertension, and individuals with prehypertension have higher MPV values than do normotensive individuals.20 Another recent, small case–control study investigated resistant hypertension and showed that MPV values in cases of resistant hypertension are higher than those in controlled-hypertensive cases or in normotensive cases.5 Similar results have likewise been found in gestational hypertension.21 These studies have shown that MPV is positively correlated with blood pressure. However, studies have not demonstrated that the MPV can independently predict hypertension. The results of our study of originally non-hypertensive individuals from a large population-based sample of community dwellers show that individuals with increased MPV had a noticeably greater risk of developing hypertension.
The present investigation found a causal relationship of MPV with the development of hypertension and may provide insight to enhance our comprehension of the pathophysiology of hypertension. Larger and activated platelets have been found to possess greater aggregability in response to adenosine diphosphate,22 which may accelerate the formation of thrombus through mechanical blockage; combined with hypoxia, it may cause arterial contractions, leading to increased resistance in circulation. Platelet clumps are also a possible stimulator for capillary vessels to contract. However, these presumptions will need to be demonstrated in future studies, and extending this investigation to find the determinants of MPV in individuals with hypertension will be beneficial.
Although the potential mechanism of elevated MPV in hypertensive individuals is not fully clear, many risk factors for hypertension have been found to be positively correlated with MPV. Obese individuals have elevated MPV values.23 Elevated MPV values have also been reported to correlate with a higher prevalence of metabolic syndrome.24 In the present investigation, positive correlations were found between MPV and the prevalence of hyperlipidemia. Furthermore, inflammation may induce platelet activation, which increases MPV.25 Cytokines such as interleukin-6 are a possible regulator of the increases in MPV caused by megakaryocyte ploidy.26 Inflammatory markers such as C-reactive protein and interleukin-6 have been reported to be independently predictive of hypertension.27, 28 Long-term poor sleep quality may increase both MPV values and hypertension incidence.29, 30 These factors may contribute to the association between MPV and hypertension.
When participants were stratified by platelet count, the highest MPV was significantly associated with an increased incidence of hypertension. However, borderline statistical significance was present in the highest platelet-count subgroup. There are markedly negative correlations between platelet count and MPV. The MPV value in the subgroup in the highest quartile of platelet counts is significantly lower than that in the subgroups in the low or medium quartile of platelet counts and is associated with a lower incidence of hypertension. Another finding of the present study was the significant and positive relationship between MPV and age. However, after adjustment for multivariate confounding factors, a significant association between increased MPV and an increased risk of developing hypertension was found in the analysis that was stratified by age.
To decrease the risk of confounding effects, we adjusted for multivariate confounding factors that are known to influence the risk of hypertension. Other factors such as glucose, total cholesterol, high-density lipoprotein cholesterol,31 uric acid,32 smoking, body mass index and triglycerides33 were also selected for inclusion in the fully adjusted model that considered these factors correlated with blood pressure levels in former studies but that were not included in the list of covariates. These factors were included into the fully adjusted model but did not distinctly alter the association of elevated MPV and the increased risk of hypertension. The adjustment for multivariate confounding factors allowed us to ensure that these associations are substantial and compelling. However, it should be acknowledged that because of the limitations of epidemiological studies, we cannot establish whether MPV is a marker or a mediator of hypertension.
Several limitations of this study should be noted. First, it is possible that a small group of individuals whose hypertension was undetected at enrollment and a small group of secondary-hypertensive subjects included in the cohort might have introduced bias into our results. However, our hospital is responsible for the health care of the inhabitants of this community and contains the health records of almost all inhabitants. Hypertensive patients were registered and received medical services at the Department of Chronic Non-communicable Diseases of our hospital. Therefore, this possibility is infinitesimal. Second, some lifestyle factors, such as salt intake and frequency of exercise, were not adjusted for. However, no published reports have indicated that these factors are correlated with MPV. Third, no information regarding hypoglycemic or hypolipidemic was available to evaluate the impact on the association between MPV and hypertension incidence. Finally, because this cohort was composed of southern Chinese individuals, our results may not be generalized to other ethnic groups.
Despite these limitations, this study has its strengths. First, this cohort includes almost all the inhabitants of an entire community, and the study followed up with patients for more than a mean time of 9 years, which is potentially representative of the adult residents in the region of southern China. Second, MPV has been observed to increase in a time-dependent manner.34 In our clinical laboratory, all whole-blood samples were processed and analyzed by uniform methods for all assays, and the testing was completed within 1 h.
In summary, elevated MPV is associated with a higher incidence of hypertension in this population-based cohort study. This finding suggests that platelet activity may play a role in the development of hypertension. Further studies are needed to seek the determinants of MPV in individuals with hypertension and to evaluate whether remedial revision of this indicator can improve care for hypertensive patients.
References
Davì G, Patrono C . Platelet activation and atherothrombosis. N Engl J Med 2008; 357: 2482–2494.
Park Y, Schoene N, Harris W . Mean platelet volume as an indicator of platelet activation: methodological issues. Platelets 2003; 14: 335–336.
Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, Konkle B, Mohler ER, Reilly MP, Berger JS . Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta‐analysis. J Thromb Haemost 2010; 8: 148–156.
Gao Y, Chen G, Tian H, Lin L, Lu J, Weng J, Jia W, Ji L, Xiao J, Zhou Z . Prevalence of hypertension in China: a cross-sectional study. PLoS ONE 2013; 8: e65938.
Leow MK . Environmental origins of hypertension: phylogeny, ontogeny and epigenetics. Hypertens Res 2015; 38: 299–307.
Surgit O, Pusuroglu H, Erturk M, Akgul O, Buturak A, Akkaya E, Gul M, Uygur B, Yazan S, Eksik A . Assessment of mean platelet volume in patients with resistant hypertension, controlled hypertension and normotensives. Eurasian J Med 2015; 47: 79–84.
Inanc T, Kaya MG, Yarlioglues M, Ardic I, Ozdogru I, Dogan A, Kalay N, Gunturk E, Gunebakmaz O, Gul I . The mean platelet volume in patients with non-dipper hypertension compared to dippers and normotensives. Blood Pressure 2010; 19: 81–85.
Gang L, Lifang W . Association of the elevated red blood cell distribution width with the risk of developing diabetes mellitus. Intern Med 2016; 55: 1959–1965.
Gang L, Yanyan Z . Increased neutrophil to lymphocyte ratio in persons suffering from hypertension with hyperhomocysteinemia. Hypertens Res 2016; 39: 606–611.
Michelson AD . Methods for the measurement of platelet function. Am J Cardiol 2009; 103: 20A–26A.
Bath P, Algert C, Chapman N, Neal B . Association of mean platelet volume with risk of stroke among 3134 individuals with history of cerebrovascular disease. Stroke 2004; 35: 622–626.
De Luca G, Santagostino M, Secco GG . Mean platelet volume and the extent of coronary artery disease: results from a large prospective study. Atherosclerosis 2009; 206: 292–297.
Vinholt PJ, Hvas AM, Frederiksen H, Bathum L, Jorgensen MK, Nybo M . Platelet count is associated with cardiovascular disease, cancer and mortality: a population-based cohort study. Thromb Res 2016; 148: 136–142.
Cetin M, Bakirci EM, Baysal E, Tasolar H, Balli M, Cakici M, Abus S, Akturk E, Ozgul S . Increased platelet distribution width is associated with ST-segment elevation myocardial infarction and thrombolysis failure. Angiology 2014; 65: 737–743.
Martin JF, Kishk YT . Changes in volume and density of platelets in myocardial infarction. Br Med J 1983; 287: 456–459.
Jagroop IA, Tsiara S, Mikhailidis DP . Mean platelet volume as an indicator of platelet activation: methodological issues. Platelets 2003; 14: 335–336.
Sharpe PC, Desai ZR, Morris TC . Increase in mean platelet volume in patients with chronic renal failure treated with erythropoietin. J Clin Pathol 1994; 47: 159–161.
Akinsegun A, Akinola OD, Sarah JO, Olajumoke O, Adewumi A, Majeed O, Anthonia O, Ebele U, Olaitan O, Olanrewaju A, Kingsley A . Mean platelet volume and platelet counts in type 2 diabetes: mellitus on treatment and non-diabetic mellitus controls in Lagos, Nigeria. Pan Afr Med J 2014; 18: 42.
Akyuz A, Akkoyun DC, Degirmenci H, Oran M . Rosuvastatin decreases mean platelet volume in patients with diabetes mellitus. Angiology 2016; 67: 116–120.
Varol E, Akcay S, Icli A, Yucel H, Ozkan E, Erdogan D, Ozaydin M . Mean platelet volume in patients with prehypertension and hypertension. Clin Hemorheol Microcirc 2010; 45: 67–72.
Akhila NR, Jayalakshmi L, Komala DSD . Study of mean platelet volume in gestational hypertension and normal pregnancy. Horizon Rep Higher Educ 2015; 6: 366–369.
Karpatkin S, Khan Q, Freedman M . Heterogeneity of platelet function. Correlation with platelet volume. Am J Med 1978; 64: 542–546.
Coban E, Ozdogan M, Yazicioglu G, Akcit F . The mean platelet volume in patients with obesity. Int J Clin Pract 2005; 59: 981–982.
Tavil Y, Sen N, Yazıcı HU, Hızal F, Abacı A, Cengel A . Mean platelet volume in patients with metabolic syndrome and its relationship with coronary artery disease. Thromb Res 2007; 120: 245–250.
Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD . Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des 2011; 17: 47–58.
Brown AS, Hong Y, de Belder A, Beacon H, Beeso J, Sherwood R, Edmonds M, Martin JF, Erusalimsky JD . Megakaryocyte ploidy and platelet changes in human diabetes and atherosclerosis. Arterioscler Thromb Vasc Biol 1997; 17: 802–807.
Sung KC, Suh JY, Kim BS, Kang JH, Kim H, Lee MH, Park JR, Kim SW . High sensitivity c-reactive protein as an independent risk factor for essential hypertension. Am J Hypertens 2003; 16: 429.
Fujii M, Ohnishi H, Saitoh S, Akasaka H, Miura T, Mori M . The combination of abdominal obesity and high-sensitivity C-reactive protein predicts new-onset hypertension in the general Japanese population: the Tanno-Sobetsu study. Hypertens Res 2015; 38:426–432.
Liu RQ, Qian Z, Trevathan E, Chang JJ, Zelicoff A, Hao YT, Lin S, Dong GH . Poor sleep quality associated with high risk of hypertension and elevated blood pressure in China: results from a large population-based study. Hypertens Res 2016; 39: 54–59.
Kanbay A, Tutar N, Kaya E, Buyukoglan H, Ozdogan N, Oymak FS, Gulmez I, Demir R . Mean platelet volume in patients with obstructive sleep apnea syndrome and its relationship with cardiovascular diseases. Blood Coagul Fibrinolysis 2013; 24: 532–536.
Shah B, Sha D, Xie D, Mohler ER, Berger JS . The relationship between diabetes, metabolic syndrome, and platelet activity as measured by mean platelet volume: The National Health and Nutrition Examination Survey, 1999–2004. Diabetes Care 2012; 35: 1074–1078.
Nagahama K, Inoue T, Kohagura K, Kinjo K, Ohya Y . Associations between serum uric acid levels and the incidence of hypertension and metabolic syndrome: a 4-year follow-up study of a large screened cohort in Okinawa, Japan. Hypertens Res 2015; 38: 213–218.
Otsuka T, Kachi Y, Takada H, Kato K, Kodani E, Ibuki C, Kusama Y, Kawada T . Development of a risk prediction model for incident hypertension in a working-age Japanese male population. Hypertens Res 2014; 38:419–425.
Bath PM, Butterworth RJ . Platelet size: measurement, physiology and vascular disease. Blood Coagul Fibrinolysis 1996; 7: 157–161.
Acknowledgements
We thank the staff of the Zhenhai Lianhua Hospital for their cooperation and study participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Gang, L., Yanyan, Z., Zhongwei, Z. et al. Association between mean platelet volume and hypertension incidence. Hypertens Res 40, 779–784 (2017). https://doi.org/10.1038/hr.2017.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.30