Abstract
An association between hypertension and diabetes has been reported; however, the temporal relationship of blood pressure changes and incident diabetes has not been fully investigated in the general population. We examined whether increasing blood pressure is associated with the risk of developing diabetes among community-dwelling Korean adults. This study included 2225 participants (859 men and 1366 women) aged 27–87 years from the Korean Genome Epidemiology Study. The participants were free of diabetes and cardiovascular disease at baseline. Incident diabetes was defined as fasting blood glucose⩾126 mg dl−1 or hemoglobin a1c ⩾6.5% (48 mmol mol−1) at follow-up examination and/or a physician’s diagnosis of diabetes during the follow-up period. The effects of the baseline level and change in blood pressure on the risk of incident diabetes were assessed by multivariate logistic regression analysis. During the mean follow-up of 2.6 years, new-onset diabetes was observed in 5.0% (43/859) of the men and 3.4% (47/1366) of the women. In the multivariate model, the baseline systolic blood pressure was not significantly associated with incident diabetes (adjusted odds ratio 0.93 per 10 mmHg, P=0.747). However, an increase in systolic blood pressure during the follow-up period was independently associated with incident diabetes (adjusted odds ratio 5.53 per 5 mmHg per year, P=0.002) after adjusting for the baseline blood pressure and other potential confounders. Increasing blood pressure, but not a high baseline blood pressure, was independently associated with the risk of diabetes in Korean adults.
Similar content being viewed by others
Introduction
Hypertension is the most important modifiable risk factor for cardiovascular disease1, 2, 3 and is also associated with metabolic abnormalities such as diabetes and dyslipidemia.4 Both hypertension and diabetes mellitus are well-known common morbidities that affect the general population and often coincide because there is substantial overlap between hypertension and diabetes in terms of etiology. Hypertension and diabetes mellitus interact with each other and share common pathways that include obesity, inflammation, oxidative stress and insulin resistance.5
A relationship between hypertension and diabetes has been reported in several studies, primarily those regarding whether fasting glucose or insulin level are independent risk factors for hypertension.4, 6, 7 The Multi-Ethnic Study of Atherosclerosis cohort study reported that higher levels of glucose and insulin may contribute to the development of hypertension, partially by damaging the kidney and arterial walls.4 The effects of insulin and glucose on incident hypertension have also been studied in French, Japanese and Iranian populations.6, 7, 8 These studies reported that the insulin and glucose levels may be independent risk factors for the development of hypertension. However, the effects of blood pressure changes on incident diabetes have not been fully investigated in the general population. Thus, we examined whether increasing blood pressure is associated with the risk of developing diabetes among rural community-dwelling adults in Korea.
Methods
Study participants
This study analyzed data from the Korean Genome Epidemiology Study (KoGES)-Kangwha Study, which is a rural community-based prospective cohort. A total of 4899 people over 40 years of age were enrolled between 2006 and 2011. The participants were all independently living on Kangwha Island, Incheon, South Korea. Detailed methods for the KoGES-Kangwha study have been reported elsewhere.9, 10
For this study, according to the baseline characteristics, we excluded people who had histories of stroke, angina pectoris or myocardial infarction (n=202), had fasting blood glucose⩾126 mg dl−1, hemoglobin a1c (HbA1c)⩾6.5%, those who were using oral antidiabetic drugs or insulin (n=687), those who were using antihypertensive or lipid-lowering drugs (n=133) and those missing the key variables (n=9). Among the remaining 3868 participants, a total of 2225 participants (859 men and 1366 women) completed follow-up health examinations and were enrolled in the current study. The participants were followed up for 1–7 years (mean 2.6 years). All participants provided written informed consent, and the study protocol was approved by the Institutional Review Board of the Yonsei University Health System (4-2004-0105, 4-2006-0101, 4-2008-0135, 4-2009-0270 and 4-2010-0272) and was monitored by the Human Research Protection Center of Severance Hospital, Yonsei University Health System.
Questionnaire data
Detailed methods for the measurements used in the KoGES-Kangwha study have previously been reported elsewhere.9, 10 All participants underwent an individual interview using standardized questionnaires to obtain information about their demographics, medical histories and lifestyles. All interviewers were trained and performed the questionnaire surveys according to a prescribed procedure. The participants were categorized according to smoking status as the current smoking group and the current nonsmoking group (that is, ex-smokers and non-smokers). Alcohol intake was also classified into the following two groups: current alcohol drinkers and current nondrinkers (past alcohol drinkers and never drinkers). Physical activity was classified into two groups: regular exercise and non-regular exercise. Education level was categorized into the following two groups: high (high school graduation or above) and low (did not complete high school).
Physical examination
Standing height was measured with an accuracy of 0.1 cm using a stadiometer (SECA 225; SECA, Hamburg, Germany), and body weight, without shoes, was measured to within 0.1 kg accuracy using a digital scale (GL-60000-20; CAS Korea, Seoul, Korea). Body mass index (BMI) was calculated as an individual’s body weight in kilograms divided by their height in meters squared. Waist circumference was assessed within an accuracy of 0.1 cm at the intermediate spot between the lower borders of the rib cage and the iliac crest with an ergonomic circumference-measuring tape (SECA 201; SECA). The resting systolic and diastolic blood pressures (SBP and DBP) were measured twice with an interval of at least 5 min using an automatic sphygmomanometer (Dinamap 1846 SX/P; GE Healthcare, Waukesha, WI, USA). The average of the two measurements was used for the analysis. Considering variation in the follow-up period, the mean change in SBP per year was calculated.
Laboratory assays
After at least 8 h of fasting, blood samples were collected from the antecubital vein in the morning. Fasting blood glucose levels were determined by a colorimetry method (ADVIA 1800; Siemens Medical Solutions, Pleasanton, CA, USA), and fasting insulin levels were determined using an immunoradiometric assay (SR-300; Stratec, Birkenfeld, Germany). Enzymatic methods were used to measure the total cholesterol, high-density cholesterol (HDL) and triglyceride levels (ADVIA 1800; Siemens Medical Solutions, Pleasanton, CA, USA). Low-density lipoprotein cholesterol levels were calculated using the Friedewald formula.11 C-reactive protein (CRP) concentration was assessed with a turbidimetric immunoassay (ADVIA 1800, Wako, Japan). The homeostasis model assessment of insulin resistance (HOMA-IR) was used to evaluate insulin resistance: HOMA-IR=fasting glucose (mg dl−1) × fasting insulin (μIU ml−1)/405.12 Incident diabetes was defined by a fasting glucose level⩾126 mg dl−1 or an HbA1c⩾6.5% at the follow-up examination and/or a physician’s diagnosis of diabetes during the follow-up period.
Statistical analysis
The analyses were performed separately for the men and women and for all of the participants. Gender differences in the general characteristics were analyzed using the independent t-test and the Wilcoxon rank-sum test for continuous variables, and the X2-test was applied for categorical variables. Fasting insulin levels, triglycerides, HOMA-IR and CRP were log-transformed for parametric testing due to the right-skewed distributions of these variables.
We also evaluated the differences in the clinical and demographic characteristics between three groups that were distinguished based on baseline blood pressure, that is, normotensive, pre-hypertensive and hypertensive, to examine whether there were nonlinear associations of baseline SBP with the other variables. One-way analysis of variance was used for the continuous variables, and the X2-statistical test was used for the categorical variables to compare the baseline characteristics between the groups. We also evaluated the linear trends and present the P-values for the trends according to the category of baseline blood pressure. We used a contrast to test for linear trends to calculate the P-values for the continuous variables. We also used the Cochran-Armitage test and the Mantel–Haenszel test to examine the existence of linear trends in the categorical variables.
The correlations of the baseline characteristics with the baseline SBP and the increment in the SBP were evaluated using Pearson correlation analyses. Simple and multiple logistic regression models were used to estimate the odds ratios of incident diabetes and their 95% confidence intervals. A multiple regression model that included the covariates of age, BMI, SBP, DBP, fasting glucose, insulin, total cholesterol, HDL cholesterol, triglyceride, CRP, smoking and alcohol intake at baseline was performed. All analyses were performed using the SAS statistical software, version 9.4 (SAS Institute, Cary, NC, USA), and statistical significance was defined as by a two-sided P-value of <0.05.
Results
The general characteristics of the study population according to sex are depicted in Table 1. This study included 859 men with a mean age of 56.8 years and 1366 women with a mean age of 54.3 years. The SBP and DBP values were significantly higher in the men than in the women. Age, fasting blood glucose, triglyceride level, CRP, smoking, alcohol intake and education level were also higher in the men than in the women. In contrast, BMI, fasting blood insulin, total cholesterol, HDL cholesterol, HOMA-IR and the frequency of regular exercise were higher in the women than in the men. During the follow-up period, 43 men (5.0%) and 47 women (3.4%) developed diabetes.
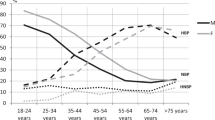
Table 2 provides the baseline characteristics and incident diabetes in the study population according to the categories of baseline blood pressure level. Among the men, 18.2% were hypertensive and 36.1% were pre-hypertensive. Among the men, higher blood pressure levels were associated with higher BMI and waist circumference. The men with higher blood pressures had significantly higher levels of fasting blood glucose, insulin, triglycerides and HOMA-IR. The men with higher blood pressure were also more likely to be current drinkers. There were 14 cases (3.6%) of incident diabetes in normotensive men during the follow-up period. In contrast, 22 (7.1%) pre-hypertensive and 7 (4.5%) hypertensive persons developed incident diabetes. Among the women, 14.2% were hypertensive and 27.9% were pre-hypertensive. Women with higher blood pressures were significantly older and had higher BMIs, waist circumferences, fasting blood glucose levels, insulin levels, HbA1c levels, total cholesterol levels, triglyceride levels, HOMA-IR values and CRP values. Women with higher blood pressure were also more likely to be in the high education group.
Table 3 provides the correlations of the baseline characteristics with the baseline SBPs and the increments of the SBPs during the follow-up. Baseline SBP was significantly and positively associated with BMI, waist circumference, DBP, fasting glucose, insulin, HOMA-IR and triglyceride before and after adjusting for sex and age. The increment in SBP was significantly and positively associated with the total cholesterol, triglyceride, baseline SBP and baseline DBP values. The significance of the association between the increment in SBP and the fasting glucose level was borderline.
The baseline characteristics of the study population according to the development of diabetes during the follow-up period are illustrated in Supplementary Table S1. Among the men, the total cholesterol and smoking status were higher among those who developed diabetes than those who did not. Among the women, the age and CRP were higher among those who developed diabetes than those who did not develop diabetes. In contrast, among the women, the DBP and HDL cholesterol were lower among those who developed diabetes than those who did not. In both the men and women, the BMI, waist circumference, fasting blood glucose, insulin, HbA1c, triglyceride and HOMA-IR values were higher in those who developed diabetes than those who did not.
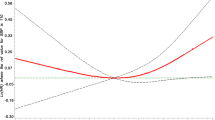
Table 4 presents the risks of incident diabetes based on the baseline characteristics and annual changes in SBP during the follow-up period. The crude odds ratios for developing diabetes among all participants were 1.09 per 10 mmHg baseline SBP (P=0.142) and 2.30 per 5 mmHg SBP change within a year (P=0.040). In the multivariate logistic analysis, after adjusting for the risk factors for diabetes, including age, BMI, DBP, weight change, fasting blood glucose, insulin, total cholesterol, HDL cholesterol, triglycerides, smoking, alcohol intake, education and exercise, the annual change in SBP was positively associated with incident diabetes (P=0.002), but baseline SBP was not associated with incident diabetes (P=0.160). Stratified according to sex, increasing SBP in the follow-up period was independently associated with the risk of diabetes, and this risk was more prominent in women (P=0.001) than in men (P=0.286; Figure 1).
Discussion
In our prospective study of a rural population, the baseline SBP was not associated with incident diabetes, but increasing SBP was significantly associated with the risk of incident diabetes. People with higher blood pressure at baseline had significantly higher BMI, waist circumference, fasting blood glucose, insulin, triglyceride and HOMA-IR values than normotensive people. Although we could not fully elucidate the causal relationships between these variables and high blood pressure, they seemed to be closely connected.
A previous prospective cohort study of 38 172 women reported that baseline blood pressure and increasing blood pressure were strong and independent predictors of incident type 2 diabetes.13 This previous study had a longer follow-up duration (10.2 years) and a larger sample size. In the previous study, some participants had received interventions of low-dose aspirin and vitamin E, and the uses of antihypertensive and lipid-lowering drugs were not considered in the analysis. However, in our study, people who were using antihypertensive and lipid-lowering drugs were excluded. In contrast, another study reported that SBP was not a significant predictor of incident diabetes in men, but SBP was a significant predictor of coronary heart disease events.14 In a previous Korean study with 14 064 individuals, the hypertensive group was found to have a higher risk of incident diabetes than the normotensive group. However, the significance of this difference disappeared after adjusting for the baseline BMI and fasting glucose level.15 Recently, another Korean study reported that prehypertension and hypertension are significantly associated with the development of diabetes, independent of sex, BMI and glucose status at baseline.16 A previous study in Turkish people reported that prehypertension may be a predictor of incident diabetes in women independent of obesity.17 Another cross-sectional study also found a significant association between prehypertension and insulin resistance.18
Several potential mechanisms that may explain that these associations have been suggested.
First, one of the possible pathophysiological pathways that underlies the significant association between increasing SBP and incident diabetes is endothelial dysfunction. Previous studies have reported that endothelial cells are dysfunctional in hypertensive patients, which suggests that progression with blood pressure is significantly associated with endothelial dysfunction.19, 20, 21, 22 In a previous study in normotensive people, blood pressure was found to be raised to hypertensive levels by an intravenous infusion of norepinephrine, and endothelium-dependent vasodilation was subsequently rapidly attenuated.23 Another previous study of primary aldosteronism found that endothelium-dependent vasodilation returned to normal when the blood pressure had returned to a normal level.24 In contrast, biomarkers related to endothelial dysfunction have exhibited a significant association with new-onset diabetes in previous studies.25, 26 In the Framingham Offspring Study, plasma markers of endothelial dysfunction, such as elevated levels of plasminogen activator inhibitor-1 antigen and von Willebrand factor antigen, were found to be associated with an increased risk of incident diabetes independent of obesity, insulin resistance and inflammation.25 In a nested case–case–control study within the Nurses’ Health Study, plasma markers of endothelial dysfunction, such as elevated levels of cellular adhesion molecules including E-selectin, intercellular adhesion molecule-1 and vascular cell adhesion molecule-1, predicted diabetes in women independent of obesity and subclinical inflammation.26
Inflammation could be another potential mechanism that explains the relationship between increasing blood pressure and incident diabetes.13, 27, 28, 29 A prospective study with 14 719 healthy women suggested that CRP is a predictor of metabolic syndrome including the component of hypertension.28 In contrast, a previous cross-sectional study with 508 apparently healthy men suggested that increased blood pressure may be a stimulus for inflammation.27 This previous study found that blood pressure was significantly associated with markers, such as intercellular adhesion molecule-1 and interleukin-6, using multivariate linear regression models that controlled for age and other cardiac risk factors.27 Inflammatory markers were also associated with the development of diabetes. In a cohort study with 12 330 middle-aged adults, markers of inflammation, such as white-cell count, orosomucoid and sialic acid, were found to be significantly associated with the development of diabetes.30 In our study, the odds ratio for incident diabetes per 5 mmHg increase in SBP was 5.72 (95% confidence interval 1.90–17.18), with adjustments for other covariates but not the CRP level. When we additionally adjusted for the CRP level, the corresponding odds ratio was 4.03 (95% confidence interval 1.45–11.23), although CRP was significantly associated with incident diabetes (P=0.045). Considering these results because there was no significant difference between the odds ratios before and after adjusting for CRP, the association between SBP changes and incident diabetes is unlikely to be mainly due to insulin resistance.
Genetic variants in the genes encoding angiotensinogen, adrenomedullin and apolipoprotein have been reported to be associated with common features such as diabetes, hypertension, dysglycemia and metabolic syndrome.31, 32 In a previous study in Chinese people, single-nucleotide polymorphisms that were associated with the development of diabetes were also found to be associated with the occurrence of hypertension.33, 34 Similarly, in genome-wide scan study, the region relevant to the development of diabetes was also associated with metabolic syndrome, including the component of hypertension.35 Obesity, insulin resistance and birth weight may be other potential links between blood pressure and the incidence diabetes, and may partially explain our results.36, 37, 38
The current study has some limitations. First, it may not be appropriate to generalize the present results to other ethnic groups because this study was conducted among Korean adults from a single rural community. This issue may limit the generalizability of our study findings. However, the annual incidence of diabetes in our study population was comparable to those reported in a previous Korean study. In a previous Korean study with people aged over 40 years at baseline, the crude annual incidence of diabetes was 1.4%.39 In our study, the crude annual incidences of diabetes were 1.9% in men and 1.3% in women. Moreover, because only a portion (57.5%) of the total KoGES-Kangwha Study participants participated in the follow-up health examination after applying the exclusion criteria based on the baseline characteristics, we compared the people who completed the follow-up health examinations with those who did not. In this comparison, no significant differences were found in the health behaviors or the prevalence of hypertension. However, the ages and fasting glucose, HbA1c, HDL cholesterol, triglyceride and HOMA-IR levels were significantly higher among the people who did not participate in the follow-up health examination (data not shown). Second, oral glucose tolerance tests were not performed in our study, which may have resulted in an underestimation of incident diabetes. Such a non-differential misclassification of outcomes would tend to attenuate the strength of the association. Nonetheless, we observed a significant association between increasing SBP and incident diabetes. Third, we were unable to account for the day-to-day variation in blood pressure because the blood pressure levels were recorded in a single visit, although we conducted the blood pressure measurements multiple times. These issues may have led to misclassifications regarding the blood pressure groups. However, the effects of non-differential misclassification would have resulted in a bias toward the null. Fourth, because we measured resting blood pressure after the blood pressure level was stable, we could not measure and access the hemodynamic fluctuation of the blood pressure or the cumulative exposure to elevated blood pressure. Fifth, because we did not consider medications for the treatment of hypertension during the follow-up period as covariates, the participants who began antihypertensive medications during the follow-up period were included in the current analysis. This fact may have resulted in the underestimation of changes in blood pressure during the follow-up period and might have reduced the association between SBP change and incident diabetes toward the null. Further studies are needed to clarify whether the control of blood pressure with medication is associated with the risk of incident diabetes because changes in blood pressure can be influenced by these medications. Sixth, the periods of observation of the participants varied widely in our study. However, we did not perform analyses that considered the differences in the follow-up periods of the participants, for example, a proportional hazard model, because the exact dates of the occurrence of incident diabetes were not known. Alternatively, considering the variation in the follow-up period among the study population, the mean change in SBP per year was used in the current analysis. Seventh, we assumed that increasing SBP affected incident diabetes. However, in other studies, fasting blood glucose has been found to be independently associated with increases in blood pressure.6, 40 This finding can partially be explained by reverse causation because this study could not establish a temporal relationship between blood pressure progression and incident diabetes. Further studies are needed to elucidate the causal association between blood pressure and incident diabetes.
In conclusion, we found that increasing SBP is independently associated with incident diabetes in Korean adults. However, baseline SBP is not significantly associated with incident diabetes. Our data suggest that the maintenance of blood pressure is important for the prevention of diabetes in normotensive people as well as in hypertensive or pre-hypertensive people.
References
Levy D, Larson MG, Vasan RS, Kannel WB, Ho KKL . The progression from hypertension to congestive heart failure. JAMA 1996; 275: 1557–1562.
He J, Whelton PK . Epidemiology and prevention of hypertension. Med Clin N Am 1997; 81: 1077–1097.
Lee SW, Kim HC, Lee HS, Suh I . Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J 2015; 45: 202–209.
Levin G, Kestenbaum B, Chen YDI, Jacobs DR, Psaty BM, Rotter JI, Siscovick DS, de Boer IH . Glucose, insulin, and incident hypertension in the multi-ethnic study of atherosclerosis. Am J Epidemiol 2010; 172: 1144–1154.
Cheung BMY, Li C . Diabetes and hypertension: is there a common metabolic pathway? Curr Atheroscler Rep 2012; 14: 160–166.
Morio M, Inoue M, Inoue K, Akimoto K . Impaired fasting glucose as an independent risk factor for hypertension among healthy middle-aged Japanese subjects with optimal blood pressure: the Yuport Medical Checkup Centre retrospective cohort study. Diabetol Metab Syndrome 2013; 5: 81.
FagotCampagna A, Balkau B, Simon D, Ducimetiere P, Eschwege E . Is insulin an independent risk factor for hypertension? The Paris prospective study. Int J Epidemiol 1997; 26: 542–550.
Janghorbani M, Bonnet F, Amini M . Glucose and the risk of hypertension in first-degree relatives of patients with type 2 diabetes. Hypertens Res 2015; 38: 349–354.
Lee JY, Ahn SV, Choi DP, Suh M, Kim HC, Kim YS, Suh I . Association between hypertension and pulmonary function in rural adults in Korea. J Prev Med Public Health 2009; 42: 21–28.
Song B, Kim H, Lee J, Lee JM, Kim D, Lee YH, Suh I . Performance of HbA1c for the prediction of diabetes in a rural community in Korea. Diabetic Med 2015; 32: 1602–1610.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D, Turner R . Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Conen D, Ridker PM, Mora S, Buring JE, Glynn RJ . Blood pressure and risk of developing type 2 diabetes mellitus: the Women's Health Study. Eur Heart J 2007; 28: 2937–2943.
Sattar N, Gaw A, Scherbakova O, Ford I, O’Reilly DSJ, Haffner SM, Isles C, Macfarlane PW, Packard CJ, Cobbe SM . Metabolic syndrome with and without C-reactive protein as a predictor of coronary heart disease and diabetes in the West of Scotland Coronary Prevention Study. Circulation 2003; 108: 414–419.
Lee WY, Kwon CH, Rhee EJ, Park JB, Kim YK, Woo SY, Kim S, Sung KC . The effect of body mass index and fasting glucose on the relationship between blood pressure and incident diabetes mellitus: a 5-year follow-up study. Hypertens Res 2011; 34: 1093–1097.
Kim M-J, Lim N-K, Choi S-J, Park H-Y . Hypertension is an independent risk factor for type 2 diabetes: the Korean genome and epidemiology study. Hypertens Res 2015; 38: 783–789.
Onat A, Yazici M, Can G, Kaya Z, Bulur S, Hergenç G . Predictive value of prehypertension for metabolic syndrome, diabetes, and coronary heart disease among Turks. Am J Hypertens 2008; 21: 890–895.
Hwu C-M, Liou T-L, Hsiao L-C, Lin M-W . Prehypertension is associated with insulin resistance. QJM 2009; 102: 705–711.
Panza JA, Quyyumi AA, Brush JE Jr, Epstein SE . Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension. N Engl J Med 1990; 323: 22–27.
Taddei S, Virdis A, Mattei P, Ghiadoni L, Gennari A, Fasolo CB, Sudano I, Salvetti A . Aging and endothelial function in normotensive subjects and patients with essential hypertension. Circulation 1995; 91: 1981–1987.
Higashi Y, Sasaki S, Nakagawa K, Matsuura H, Chayama K, Oshima T . Effect of obesity on endothelium-dependent, nitric oxide–mediated vasodilation in normotensive individuals and patients with essential hypertension. Am J Hypertens 2001; 14: 1038–1045.
Gokce N, Holbrook M, Duffy SJ, Demissie S, Cupples LA, Biegelsen E, Keaney JF, Loscalzo J, Vita JA . Effects of race and hypertension on flow-mediated and nitroglycerin-mediated dilation of the brachial artery. Hypertension 2001; 38: 1349–1354.
Millgård J, Lind L . Acute hypertension impairs endothelium-dependent vasodilatation. Clin Sci 1998; 94: 601–608.
Kiowski W, Linder L, Nuesch R, Martina B . Effects of angiotensin converting enzyme inhibition on endothelial vasodilator function in primary human hypertension. Eur Heart J 1993; 14: 5–9.
Meigs JB, O’Donnell CJ, Tofler GH, Benjamin EJ, Fox CS, Lipinska I, Nathan DM, Sullivan LM, D’Agostino RB, Wilson PW . Hemostatic markers of endothelial dysfunction and risk of incident type 2 diabetes the Framingham Offspring Study. Diabetes 2006; 55: 530–537.
Meigs JB, Hu FB, Rifai N, Manson JE . Biomarkers of endothelial dysfunction and risk of type 2 diabetes mellitus. JAMA 2004; 291: 1978–1986.
Chae CU, Lee RT, Rifai N, Ridker PM . Blood pressure and inflammation in apparently healthy men. Hypertension 2001; 38: 399–403.
Ridker PM, Buring JE, Cook NR, Rifai N . C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events an 8-year follow-up of 14 719 initially healthy American women. Circulation 2003; 107: 391–397.
Bautista L . Inflammation, endothelial dysfunction, and the risk of high blood pressure: epidemiologic and biological evidence. J Hum Hypertens 2003; 17: 223–230.
Schmidt MI, Duncan BB, Sharrett AR, Lindberg G, Savage PJ, Offenbacher S, Azambuja MI, Tracy RP, Heiss G,, investigators A. Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet 1999; 353: 1649–1652.
Ong KL, Li M, Tso AW, Xu A, Cherny SS, Sham PC, Tse HF, Lam TH, Cheung BM, Lam KS . Association of genetic variants in the adiponectin gene with adiponectin level and hypertension in Hong Kong Chinese. Eur J Endocrinol 2010; 163: 251–257.
Cheung CY, Tso AW, Cheung BM, Xu A, Ong KL, Law LS, Wat NM, Janus ED, Sham PC, Lam KS . Genetic variants associated with persistent central obesity and the metabolic syndrome in a 12-year longitudinal study. Eur J Endocrinol 2011; 164: 381–388.
Ong K, Leung RY, Wong LY, Cherny SS, Sham P, Lam T, Lam KS, Cheung BM . Association of a polymorphism in the lipin 1 gene with systolic blood pressure in men. Am J Hypertens 2008; 21: 539–545.
Chow W-S, Cheung BM, Tso AW, Xu A, Wat NM, Fong CH, Ong LH, Tam S, Tan KC, Janus ED . Hypoadiponectinemia as a predictor for the development of hypertension a 5-year prospective study. Hypertension 2007; 49: 1455–1461.
Ng MC, So W-Y, Lam VK, Cockram CS, Bell GI, Cox NJ, Chan JC . Genome-wide scan for metabolic syndrome and related quantitative traits in Hong Kong Chinese and confirmation of a susceptibility locus on chromosome 1q21-q25. Diabetes 2004; 53: 2676–2683.
Mancia G . The association of hypertension and diabetes: prevalence, cardiovascular risk and protection by blood pressure reduction. Acta Diabetol 2005; 42: s17–s25.
Sowers JR . Insulin resistance and hypertension. Am J Physiol Heart Circ Physiol 2004; 286: H1597–H1602.
Byberg L, McKeigue P, Zethelius B, Lithell H . Birth weight and the insulin resistance syndrome: association of low birth weight with truncal obesity and raised plasminogen activator inhibitor-1 but not with abdominal obesity or plasma lipid disturbances. Diabetologia 2000; 43: 54–60.
Oh JY, Lee HJ, Hong ES, Hong YS, Sung YA, Lee SH . The prevalence and incidence of diabetes in Mokdong, Seoul. J Korean Diabetes Assoc 2003; 27: 73–83.
Bjørnholt JV, Erikssen G, Kjeldsen SE, Bodegård J, Thaulow E, Erikssen J . Fasting blood glucose is independently associated with resting and exercise blood pressures and development of elevated blood pressure. J Hypertens 2003; 21: 1383–1389.
Acknowledgements
This study was supported by grants from the Korea Centers for Disease Control and Prevention (2006-347-2400-2440-215, 2008-E71004-00, 2009-E71006-00, 2010-E71003-00, 2011-E71002-00, 2012-E71007-00 and 2013-E71008-00) and the Korean Health Technology R&D Project, Ministry of Health & Welfare (HI13C0715).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website .
Supplementary information
Rights and permissions
About this article
Cite this article
Lee, S., Kim, H., Lee, Jm. et al. Association between changes in systolic blood pressure and incident diabetes in a community-based cohort study in Korea. Hypertens Res 40, 710–716 (2017). https://doi.org/10.1038/hr.2017.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2017.21
Keywords
This article is cited by
-
Predictive value of machine learning algorithm of coronary artery calcium score and clinical factors for obstructive coronary artery disease in hypertensive patients
BMC Medical Informatics and Decision Making (2023)
-
Associations of CKIP-1 and LOX-1 polymorphisms with the risk of type 2 diabetes mellitus with hypertension among Chinese adults
Acta Diabetologica (2023)
-
Hypertension with diabetes mellitus: physiology and pathology
Hypertension Research (2018)