Abstract
Preeclampsia (PE), one of the most common disorders of pregnancy, is characterized by hypertension and albuminuria. In severe cases, PE results in eclampsia-like seizures. Studies have suggested that severe PE is related to an exaggerated systemic inflammatory response, which may increase sensitivity to seizures. In the current study, we investigated whether the seizure activity of neurons was enhanced under excessive systemic inflammation. We also sought to determine whether MgSO4 could reduce the effects of systemic inflammation on seizure activity after electrical stimulation in a lipopolysaccharide (LPS)-induced model of PE. In addition to pregnancy outcomes, we analyzed biochemical parameters to ascertain whether our PE model was successful. Enzyme-linked immunosorbent assay analysis revealed that the levels of inflammatory cytokines (tumor necrosis factor (TNF)-α and interleukin (IL)-1β) were significantly higher in the LPS-treated rats than in the untreated rats. After electrical stimulation, behavioral assessments showed that the LPS-treated rats that were not treated with MgSO4 had the shortest latency period to develop a seizure and the longest seizure duration. The electroencephalographic (EEG) recordings in the hippocampus demonstrated that this group also had the highest EEG amplitude. MgSO4 treatment significantly decreased both TNF-α and IL-1β concentrations, increased the latency to develop a seizure, decreased the seizure duration and shortened the EEG amplitude. These results suggest that neuronal seizure activity and systemic inflammation are increased in severe PE. In addition, MgSO4 treatment reduced systemic inflammation and seizure severity. We conclude that excessive systemic inflammation in PE promotes eclampsia seizures, which can be attenuated by MgSO4 treatment.
Similar content being viewed by others
Introduction
Preeclampsia (PE) is a serious complication of pregnancy. Its clinical manifestations are maternal hypertension, albuminuria, liver and kidney dysfunction, fetal growth restriction and maternal and infant death in late pregnancy.1 According to the World Health Organization’s estimates of global incidence, >4 million live births are affected by PE each year, resulting in maternal deaths between 40 000 and 72 000.2 Eclampsia is defined as the development of grand mal seizures in patients with gestational hypertension or PE.3 The risk of maternal death caused by eclampsia is 0–1.8% in developed countries and as high as 15% in the developing countries.4, 5, 6, 7 PE and eclampsia continue to be a major cause of maternal and fetal morbidity and mortality, but their pathogenesis remains unclear.
Clinical data suggest that excessive systemic inflammatory is associated with PE.1, 8 PE has been found to involve the activation of a large number of white blood cells,9 and inflammatory markers, such as tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6) and C-reactive protein, were increased at least twofold in PE patients compared with non-pregnant patients.8, 9, 10, 11, 12 (TNF)-α infusion and low-dose lipopolysaccharide (LPS) infusion have been used to establish animal models of PE by inducing systemic inflammation in pregnant rats.10 Eclampsia is associated with the development of tonic–clonic seizures in PE patients.11 Seizures are caused by synchronized aberrant electrical activity of neuronal populations owing to underlying hyperexcitability.12, 13 Vezzani et al.14 showed that proinflammatory cytokines such as IL-1β and TNF-α can enhance neuronal excitability and initiate spontaneous seizures. Key inflammatory mediators are also correlated with seizure frequency15; therefore, it is possible that a systemic inflammatory response is involved in the pathogenesis of PE and eclampsia.
Magnesium sulfate (MgSO4) has been shown to have therapeutic effects in PE and reduces the release of acetylcholine in the neuromuscular junction, which causes the muscles to relax,16 increases the synthesis of prostacyclins, increases vasodilation by inhibiting angiotensin-converting enzyme17 and improves sedation of the nervous system.18 In addition, Dowling et al.19 found that administration of MgSO4 inhibited LPS-induced excessive inflammation at the maternal–fetal interface. Other studies have also highlighted the anti-inflammatory effects of MgSO4. Nuan-Yen’s study20 suggested that MgSO4 could prevent the endotoxin-induced upregulation of inflammatory mediators in vitro21 and mitigate the inflammatory response in rats with endotoxemia.22 Because PE and eclampsia are often associated with abnormal maternal inflammation, parenteral MgSO4 has been an important drug for treating severe PE.23
In the present study, to investigate whether systemic inflammation correlates with seizure activity, we established a new eclampsia-like model using electrical stimulation. We measured systolic blood pressure (SBP), proteinuria, creatinine (Cr), blood urea nitrogen (BUN), alanine transaminase (ALT) and aspartate transaminase (AST) to determine whether the model was successful. The seizure activity of neurons in the eclampsia-like model was recorded and analyzed using behavioral methods and electroencephalography (EEG). Furthermore, we detected inflammatory markers to investigate the relationship of systemic inflammation with seizure activity. In addition, we explored the effects of MgSO4 treatment on seizure activity and inflammatory responses.
Materials and methods
Animals
Experimental protocols were approved by the Committee on the Ethics of Animal Experiments of Guangzhou Medical University (Permit Number: 2012–50) and were in strict accordance with the recommendations of the NIH Guidelines (NIH Publications No. 8023, revised 1978) for the Care and Use of Laboratory Animals. All efforts were made to minimize the number of animals used and their suffering. A total of 45 female Sprague Dawley rats (weight, 210–250 g; 10–12 weeks old) were obtained from the Medical Experimental Animal Center of Guangdong, China. The rats were acclimatized to the laboratory conditions for 1 week prior to the start of the experiments. Each rat used in all the pregnancy groups was separately mated overnight. Day 0 of pregnancy was defined as the day when spermatozoa were found in a vaginal smear.24 There were five experimental groups: the non-pregnant group (NP group, n=12), the non-pregnant group treated with LPS (NP+LPS group, n=12), the pregnant group (P group, n=6), the pregnant group treated with LPS (P+LPS group, n=7), and the pregnant group treated with LPS and MgSO4 (P+LPS+Mg group, n=8).
Implantation of electrodes for electrical stimulation and EEG recording
For all surgeries, the rats were anesthetized with 10% chloral hydrate (3.5 ml kg−1, i.p.). EEG electrodes were made using a section of insulated Nichrome wire (0.2 mm in diameter with uninsulated tips) that was soldered to a 080-1/8 inch stainless steel screw (RWD Life Science, Shenzhen, China), which was implanted and fixed to the skull using dental acrylic.25 The free end of the wire was soldered to a SM-3P wiring terminal coupled to a stimulating electrode and the EEG recording equipment. A stereotaxic frame (RWD Life Science) was used to guide the electrodes to the correct location in the hippocampus. The electrode was implanted in the right dorsal hippocampus (3.8 mm behind the bregma, 3.9 mm right of the midline and 3.7 mm below the skull bone). After the scalps were sutured, the rats were individually housed in cages and allowed to recover for 7–10 days.
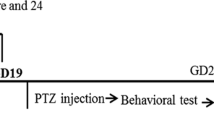
Rat model of PE
On gestational day (GD) 14, the rats in the P+LPS and NP+LPS groups were anesthetized and received 2 ml of LPS (1.0 μg kg−1) infused through the tail vein with a pump at a rate of 2 ml h−1 according to method described by Fass et al.26 On the same day, the rats in the NP and P groups were infused with 0.9% saline using a similar protocol.
Electrical stimulation and EEG recordings in the PE model
On GD 18, all rats received electrical stimulation. The rats were individually placed in a 20 × 35 × 25 cm3 box and allowed to freely explore for at least 10 min before the start of electrical stimulation. After 10 min, the rats received the electrical stimulations (0.2 mA, 20 Hz, 100 ms intervals, rectangular pulses). The behavioral characteristics of the seizures were classified and recorded according to Racine’s staging: stage 1, mouth and facial movements; stage 2, head nodding; stage 3, forelimb clonus; stage 4, rearing; and stage 5, rearing and falling. A grand mal seizure was referred to as a stage 5 motor seizure.27 The latency to develop a stage 5 seizure was defined as the time from the start of the electrical stimulation to the occurrence of an evoked stage 5 seizure. The stimulation duration was defined as the time to develop a tonic–clonic seizure (to a maximum of 30 min). EEG data were continuously recorded during the procedure using a BL-420S Biological Functional System (Chengdu Taimeng Technologies, Chengdu, China).
MgSO4 treatment
On GD 14, after LPS infusion, osmotic mini-pumps (Model 2ML1; Alzet Corporation, Palo Alto, CA, USA), which were loaded to continuously deliver MgSO4 (60 mg kg−1 day−1),28 were s.c. inserted into the mid-scapular region of each rat in the P+LPS+Mg group.
Measurement of biochemical parameters and cytokine analysis
On GDs 7, 13, 15, 17 and 19, SBP was measured between 0900 and 1200 hours using a non-invasive blood pressure system (Chengdu Taimeng Technologies). SBP measurements were performed three times in 1 day for each rat, and the mean values were recorded. On GD 16, the rats were placed into metabolic cages and urine samples were collected. Twenty-four-hour urine protein excretion was measured using an auto-analyzer (HITACHI automatic analyzer, 7600-020, HITACHI, Tokyo, Japan). On GD 18, prior to electrical stimulation, 2 ml of blood was collected from the intraorbital sinus of each rat, and the serum was separated for biochemical parameters and cytokine analysis. On GD 20, we repeated the cytokine analysis. On GD 21, the rats were anesthetized with a non-lethal dose of chloral hydrate and blood samples were collected. After the blood collection, the rats were killed. The pups and the placentas were removed through cesarean section and were counted, weighed and examined for resorption and malformation. Measurements of liver enzymes (ALT, AST), BUN and Cr were performed using an automatic analyzer (HITACHI 7600-020). The serum levels of cytokines (TNF-α and IL-1β) were determined using a highly sensitive enzyme-linked immunosorbent assay (eBioscience, San Diego, CA, USA). For each assay, the standards and samples were tested in duplicate.
Drugs and solutions
LPS (E. coli, 0.55:B5; Sigma Aldrich, St Louis, MO, USA) was dissolved in 0.9% saline, and a stock solution of 1 mg ml−1 of LPS was prepared and stored at −20 °C. A 10% MgSO4 solution was prepared and stored at 4 °C.
Statistical analysis
The normally distributed continuous data are expressed as the mean±s.e.m. A one-way analysis of variance was used to compare the average values between the different groups, which was followed by the least significant difference post-hoc test. The rats were compared using chi-squared test or Fisher’s exact test. All the statistical analyses were performed using the SPSS 13.0 software package (SPSS, Chicago, IL, USA). A P-value <0.05 was considered statistically significant.
Results
SBP was increased in the P+LPS group
To confirm that the rats in the P+LPS group developed PE-like symptoms, we analyzed the SBP of each rat. Before LPS administration, quantitative analysis (Figure 1) revealed that there were no significant differences between the groups on GDs 7 and 13 (P>0.05). After LPS administration, SBP significantly increased in the P+LPS group at GDs 17 (129±3 mm Hg) and 19 (135±4 mm Hg), compared with GDs 7 (112±3 mm Hg), 13 (113±4 mm Hg) and 15 (119±2 mm Hg) (P<0.05). In addition, SBP at GD 17 was significantly higher in the P+LPS group than in the NP (111±2 mm Hg), NP+LPS (110±3 mm Hg) and P (113±2 mm Hg) groups (P<0.05). SBP at GD 19 was also higher in the P+LPS group than in the NP (111±2 mm Hg), NP+LPS (110±3 mm Hg) and P (113±2 mm Hg) groups (P<0.05).
Changes in the mean systolic blood pressure (SBP) in all the five groups at 7, 13, 15 and 19 days after gestation. The values are presented as the mean±s.e.m. SBP was significantly increased in the P+LPS group compared with the NP, NP+LPS and P groups on gestation days (GDs) 17 and 19 (*P<0.05). Following LPS administration, SBP was also increased in the P+LPS group on GDs 17 and 19 compared with GDs 7 and 13. SBP in the P+LPS+Mg group exhibited a similar pattern as the P+LPS group (#,*P<0.05). NP=non-pregnant, NP+LPS=non-pregnant+LPS, P=pregnant, P+LPS=pregnant+LPS, P+LPS+Mg=pregnant+LPS +MgSO4.
Changes in biochemical outcomes in groups without magnesium (Mg) treatment
To further ascertain whether the PE model was successful, we measured the levels of proteinuria, Cr, BUN, ALT and AST using an automatic analyzer (Table 1). The results showed that proteinuria was significantly higher in the P+LPS group (3.8±0.5 mg per 24 h) than in the NP (2.3±0.4 mg per 24 h), NP+LPS (2.4±0.4 mg per 24 h) and P (2.6±0.6 mg per 24 h) groups (P<0.05). Furthermore, ALT levels were significantly higher in the P+LPS group (91±11.3 U l−1) than in the NP (64±3.5 U l−1) and NP+LPS (78±6.7 U l−1) groups (P<0.05). Moreover, the AST level was higher in the P+LPS group (191±14.3 U l−1) than in the NP (117±6.9 U l−1), NP+LPS (121±8.7 U l−1) and P (131±11.2 U l−1) groups (P<0.05). However, BUN and Cr levels were not significantly different between the P+LPS, NP, NP+LPS and P groups.
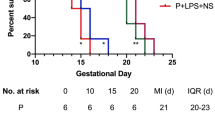
Poor pregnancy outcomes in the P+LPS group
PE is also characterized by poor pregnancy outcomes. Therefore, we measured the number of live fetuses, the percentage of resorbed fetuses, the fetal weight and the placental weight (Table 2). The results showed that the percentage of fetal resorption was increased by 79.2% in the P+LPS group (24%) compared with the P group (5%). Furthermore, the fetal weight was lower in the P+LPS group (3.97±0.04 g) than in the P group (4.31±0.12 g) (P<0.05). There were no significant differences in the number of live fetuses and the placental weight between the P+LPS and P groups.
Increased seizure activity in the P+LPS group after electrical stimulation as detected using behavioral methods
The electrical stimulation-induced seizure behavior was assessed according to Racine’s scale.27, 29 After electrical stimulation, all the pregnant rats that were infused with either 0.9% saline or LPS developed stage 5 seizures, whereas only 58.3% of non-pregnant rats developed a full motor seizure. The latency to develop tonic–clonic seizures was significantly shorter in the P+LPS group (3.3±0.7 min) than in the NP (10.6±2.1 min) and NP+LPS (11.3±1.8 min) groups (P<0.05, Figure 2a). Furthermore, the seizure duration was significantly longer in the P+LPS rats (21.5±2.1 s) than in the NP (13.4±1.2 s), NP+LPS (14.1±1.4 s) and P (16.7±1.7 s) groups (P<0.05, Figure 2b).
Changes in the latency to develop grade 5 seizures and the seizure duration in all the experimental groups. (a) Compared with the NP and NP+LPS groups, the latency to develop grade 5 seizures was significantly decreased in the P and P+LPS groups (*P<0.05). However, MgSO4 treatment increased the latency in the P+LPS+Mg group compared with the other four groups (#P<0.05). (b) Compared with NP and the NP+LPS groups, the seizure duration was significantly increased in the P and P+LPS groups (*P<0.05). In addition, the seizure duration was longer in the P+LPS group than in the P group. MgSO4 treatment significantly decreased the seizure duration in the P+LPS+Mg group compared with the P and the P+LPS groups (#P<0.05).
EEG neuronal seizure activity increased in the P+LPS group after electrical stimulation
Because an abnormal EEG can help to predict the risk of seizure recurrence, EEG has been proposed as part of the initial neurological diagnostic evaluation in pregnant patients.30 EEG recordings were used to show the seizure activity when the rats developed clinical tonic–clonic convulsions and revealed changes in seizure activity before and after electrical stimulation in the different groups. No trace of evoked seizures was found in the five groups before electrical stimulation (Figures 3a–e). After stimulation, dramatic seizures were observed in the EEG traces in the NP (Figure 3a-1), NP+LPS (Figure 3b-1), P (Figure 3c-1) and P+LPS groups (Figure 3d-1); all of the seizures lasted for 4–5 s. Furthermore, the amplitude of the seizure traces was twice as high as the traces before electrical stimulation.
EEG recordings before and after electrical stimulation in the different groups. Before electrical stimulation, EEG traces showed that there were no convulsive seizures in all the five groups (a–e). Electrical stimulation induced seizures in the NP, NP+LPS, P and P+LPS groups, and the amplitudes of the EEG traces were two to three times higher compared with the EEG traces before stimulation (a-1, b-1, c-1 and d-1). MgSO4 treatment significantly decreased the seizure amplitude (e-1). (f) Histogram of the EEG amplitude. The EEG amplitudes were significantly increased after electrical stimulation in the NP, NP+LPS, P and P+LPS groups (*P<0.01). A comparison of the EEG amplitudes between the groups after electrical stimulation showed that the amplitude was significantly decreased in the P+LPS+Mg group compared with the P+LPS group (▲*P<0.05).
Statistical analysis revealed that EEG amplitude increased significantly after electrical stimulation in each group compared with the prestimulation recordings (NP: 90.54±12.5 vs. 23.45±2.56 μV; NP+LPS: 89.68±13.38 vs. 25.17±2.12 μV; P: 92.27±11.17 vs. 27.93±2.78 μV; P+LPS: 107.74±14.29 vs. 26.07±2.89 μV; P<0.01). There were no significant differences in the EEG amplitude between the P+LPS group and the NP, NP+LPS and P groups after electrical stimulation (Figure 3f).
Increased inflammatory cytokines in the PE model
The concentrations of TNF-α and IL-1β were measured before and after electrical stimulation (Table 3). TNF-α was not detected in the NP and the NP+LPS groups before and after stimulation. However, the level of TNF-α was approximately 30% higher in the P+LPS group (23.6±4.01 pg ml−1) than in the P group (16.99±2.81 pg ml−1). After stimulation, the TNF-α levels were 25% higher in the P+LPS group (24.02±4.72 pg ml−1) than in the P group (18.42±2.45 pg ml−1); however, these differences were not statistically significant. The IL-1β levels were significantly higher in the P+LPS group (82.56±8.19 pg ml−1) before stimulation than in the NP (40.92±4.64 pg ml−1), NP+LPS (43.35±5.49 pg ml−1) and P groups (57.91±6.21 pg ml−1) (P<0.05). After stimulation, the IL-1β levels were also higher in the P+LPS group (88.94±7.91 pg ml−1) than in the NP (44.84±5.49 pg ml−1), NP+LPS (41.18±4.35 pg ml−1) and P (60.08±7.16 pg ml−1) groups (P<0.05). However, there were no differences in TNF-α and IL-1β levels within each group after electrical stimulation.
The effect of MgSO4 on the PE and seizure models
The serum magnesium concentration was significantly higher in the P+LPS+Mg group (0.86±0.24 mmol l−1) than in the groups that did not receive MgSO4 treatment (the P group, 0.63±0.09 mmol l−1; and the P+LPS group, 0.61±0.12 mmol l−1; P<0.05). There was no significant difference in SBP between the P+LPS+Mg and P+LPS groups (Figure 1). Furthermore, there were no differences in the levels of proteinuria, Cr, BUN, ALT and AST in the P+LPS+Mg group compared with the PE group (proteinuria: 3.5±0.5 vs. 3.8±0.5 mg per 24 h; Cr: 31.4±1.8 vs. 32.9±2.7 μmol l−1; BUN: 7.1±0.7 vs. 7.5±1.0 mmol l−1; ALT: 89±7.6 vs. 91±11.3 U l−1; and AST: 176±12.9 vs. 191±143 U l−1; Table 1). In addition, the number of live fetuses (9.3±0.6), fetal weight (4.12±0.06 g) and placental weight (0.52±0.02 g) were not significantly different after MgSO4 treatment compared with the values in the P+LPS group. However, the percentage of resorbed fetuses decreased by approximately 50% in the P+LPS+Mg group (11.9%) compared with the PE group (24%) (Table 2).
After stimulation, the rats in the P+LPS group developed seizures. MgSO4 administration decreased the degree of the seizures. The latency to develop stage 5 seizures was significantly longer in the P+LPS+Mg group (18.6±2.9 min) than in the P+LPS group (3.3±0.7 min) (P<0.01, Figure 2a). In addition, seizure duration was significantly shorter in the P+LPS+Mg group (13.1±1.2 s) than in the P+LPS group (21.5±2.1 s) (P<0.01, Figure 2b). Furthermore, EEG was used to record the neuronal seizure activity. After stimulation, the spikes in the trace, which indicates a lower EEG amplitude, was shorter in the P+LPS+Mg group (78.25±11.57 μV) than in the P+LPS group (107.74±14.29 μV, P<0.05). The total seizure duration was slightly shorter after MgSO4 treatment (Figure 3e-1). However, there were no significant differences between the two groups before the electrical stimulation. In the P+LPS+Mg group, EEG amplitude was also significantly increased after stimulation (78.25±11.57 μV) compared with the unstimulated conditions (22.48±2.91 μV, P<0.01, Figure 3f).
Inflammatory cytokines were also reduced by MgSO4 treatment. Before stimulation, the TNF-α levels were lower in the P+LPS group (23.36±4.01 pg ml−1) than in the P+LPS+Mg group (17.25±3.84 pg ml−1). After stimulation, the TNF-α levels were decreased in the P+LPS group (24.02±4.72 pg ml−1) compared with the P+LPS+Mg group (18.96±3.15 pg ml−1). However, these changes were not statistically significant. Before stimulation, the IL-1β levels were lower in the P+LPS+Mg group (63.19±7.24 pg ml−1) than in the PE group (82.56±8.19 pg ml−1, P<0.05). After stimulation, the IL-1β level was also significantly lower in the P+LPS+Mg group (72.24±6.25 pg ml−1) than in the PE group (88.94.±7.91 pg ml−1, P<0.05, Table 3).
Discussion
PE and eclampsia models
PE is a common disease during pregnancy; however, the mechanisms underlying its pathogenesis remain unclear. Therefore, animal models of PE are necessary to study the etiology of PE and explore therapeutic treatment interventions. Several key events have been shown to be involved in the early development of PE, including insufficient spiral artery remodeling and higher plasma levels of soluble fms-like tyrosine kinase-1. Higher plasma levels of soluble fms-like tyrosine kinase-1 has been shown to antagonize vascular endothelial growth factor, which causes abnormal spiral artery remodeling31, 32, 33; therefore, vascular endothelial growth factor inhibitors have been used as a model of PE.34, 35 In addition, based on two predominant theories of PE (the locally chronic uterine placenta ischemia and hypoxia theory and the excessive activation of the maternal immune system theory), additional animal models of PE have been developed. These include uteroplacental ischemia models,36 nitric oxide synthase inhibition models,37, 38 inflammation-related models (such as LPS infusion)39 and TNF-α infusion models.40 Unfortunately, only a few of the PE models lead to the development of eclampsia-like seizures. We have previously used pentylenetetrazol treatment to induce eclampsia-like seizures in pregnant rats treated with low-dose LPS.41 Johnson et al.42 combined reduced uteroplacental perfusion pressure with a high-cholesterol diet to develop an eclampsia model. In the present study, we successfully induced eclampsia-like seizures using electrical stimulation in the hippocampus of PE rats. This model excludes the effects of external chemical agents and directly reflects the neuronal firing activity observed in PE.
Inflammatory mechanisms might participate in seizure occurrence in PE after electrical stimulation
The outcomes of PE have been found to be associated with systemic inflammation,43, 44, 45, 46 which includes increases in serum levels of circulating proinflammatory cytokines, such as TNF-α, IL-1 and IL-6.47, 48 Systemic inflammation can be rapidly activated by LPS administration in experimental models, which subsequently increases the levels of inflammatory cytokines (TNF-α or IL-1β) and oxygen-free radicals.8, 49 In the present study, we administered LPS to pregnant rats to promote the development of PE and found that the serum levels of IL-1β significantly increased in the PE group compared with the NP, NP+LPS and P groups. Furthermore, TNF-α levels also increased by 30% compared with the P group. These results are consistent with previous findings on cytokines in PE41, 50, 51, 52 which have shown that direct or indirect endothelial dysfunction may result in the excessive production of cytokines, reduction in angiogenic processes and renal dysfunction.48, 53 More importantly, we investigated whether seizure susceptibility increased significantly in the PE group, corresponding to the increased inflammation after electrical stimulation. First, behavioral assessments revealed that seizure activity was the strongest in the PE group after electrical stimulation. Second, EEG recordings demonstrated that the EEG amplitude was the longest in the PE group after electrical stimulation; however, there was no significant difference between the PE group and the NP, NP+LPS and P groups. These results indicated that the PE group was more inclined to develop seizures. In addition, we observed increased signs of inflammation in the PE group, which suggests that excessive inflammation decreased seizure sensitivity. It is worth noting that the serum levels of IL-1β and TNF-α were significantly higher in the pregnancy groups than in the NP and NP+LPS groups. The latency to develop stage 5 seizures was also decreased in the pregnancy groups compared with the NP and NP+LPS groups. Seizure duration and EEG amplitudes were also increased in the P group, although there were no significant differences between the P group and the NP and NP+LPS groups. These results suggest that during normal pregnancy, cytokines are also elevated and promote seizure activity. The findings are consistent with the findings by Cipolla et al.,54 who found that increased serum levels of cytokines during pregnancy could induce neuroinflammation and seizure activity. In fact, during normal pregnancy, the immune system changes to meet the demands of the growing fetus. As a result, high levels of cytokines are released into the circulation and may have an important role in the development of seizures later in gestation.55, 56 These studies further suggest that increased systemic inflammation is related to seizure sensitivity.57, 58 Systemic inflammation has been suggested to have transient or long-term effects on seizure susceptibility by inducing a mirror inflammatory response in the brain through microglial activation.59, 60 Studies have demonstrated that neuronal excitability is enhanced by central nervous system immune responses, which are promoted by systemic inflammation.60 The increased neuronal excitability is induced by abnormal hyper-synchronous electrical activity of the neuronal networks in the central nervous system61, 62 and results in increased seizure susceptibility. Therefore, although we did not examine neuroinflammation in the current study, the higher levels of inflammatory cytokines in the PE group may result in higher seizure activity in the brain by inducing neuroinflammation. Using quantification and morphological assessment of microglia, Johnson et al.42 demonstrated that neuroinflammation was increased in severe PE. Riazi et al.60 also observed increased microglial activation and number in the hippocampus of animals with peripheral inflammation. Communication between systemic inflammation and neuroinflammation involves the transport of cytokines into the central nervous system through the blood–brain barrier,63 which employs neural and humoral pathways to mediate the brain response to systemic inflammation.64, 65 Then the cytokines activate the microglia, which causes additional cytokines to be released throughout the whole brain.66, 67
MgSO4 treatment decreases seizure activity and systemic inflammation in severe PE
It is well known that MgSO4 can prevent PE from developing into eclampsia, and MgSO4 is the drug of choice in the treatment of eclamptic seizures.68, 69, 70, 71 Ohno et al.72 demonstrated that MgSO4 decreased the risk of convulsion in eclampsia patients. In our study, we found that there was no significant difference in SBP, the levels of proteinuria, Cr, BUN, ALT and AST, the number of live fetuses and the placental weight between the P+LPS and the P+LPS+Mg groups. These results demonstrate that MgSO4 should not be recommended to control high blood pressure during pregnancy, which is in agreement with the finding by Duley et al.73 In addition, biomedical parameters and pregnancy outcomes have not been therapeutic targets of MgSO4. However, MgSO4 treatment significantly reduced both IL-1β and TNF-α levels in the P+LPS group before and after electrical stimulation. These results indicate that MgSO4 had anti-inflammatory effects in our PE model (P+LPS before stimulation) and eclampsia (P+LPS after stimulation). These effects were also reported by Dowling et al.,19 who revealed that MgSO4 could inhibit LPS-induced inflammation and that enhanced activity of the phosphoinositide-3 kinase/Akt pathway was a crucial mechanism underlying the anti-inflammation effects of MgSO4. Furthermore, MgSO4 treatment increased the latency to develop stage 5 seizures, decreased the seizure duration and shortened the EEG amplitude after electrical stimulation. These results suggest that eclampsia-like seizure activity may be reduced by MgSO4 and confirms the anticonvulsant effects of MgSO4, which have been observed in animal studies.74
In conclusion, LPS increases systemic inflammation in PE rats after electrical stimulation in conjunction with increases in neuronal seizure activity. The anticonvulsant, MgSO4, decreased inflammation and seizure susceptibility. These results support the idea that increased seizure activity correlates with excessive systemic inflammation in severe PE.
Limitations of the study
First, we did not include a ‘P+MgSO4’ control group in our study. However, Amash et al.75 found that MgSO4 does not affect maternal circulating levels of IL-1β in the placenta during normal pregnancy but decreases circulating IL-1β levels in the placenta during PE. These results both support and supplement our present investigation.75 Second, our results showed that excessive systemic inflammation might have an important role in eclampsia by increasing the susceptibility to neuronal seizure activity. However, future studies are needed to clarify our present results.
References
Podjarny E, Losonczy G, Baylis C . Animal models of preeclampsia. Semin Nephrol 2004; 24: 596–606.
AbouZahr C . Global burden of maternal death and disability. Br Med Bull 2003; 67: 1–11.
Sibai BM . Diagnosis, prevention, and management of eclampsia. Obstet Gynecol 2005; 105: 402–410.
Dasari P, Habeebullah S . Maternal mortality due to hypertensive disorders of pregnancy in a tertiary care center in Southern India. Int J Gynaecol Obstet 2010; 110: 271–273.
Urassa DP, Carlstedt A, Nystrom L, Massawe SN, Lindmark G . Eclampsia in dar es salaam, Tanzania -- incidence, outcome, and the role of antenatal care. Acta Obstet Gynecol Scand 2006; 85: 571–578.
Zwart JJ, Richters JM, Ory F, de Vries JI, Bloemenkamp KW, van Roosmalen J . Severe maternal morbidity during pregnancy, delivery and puerperium in the Netherlands: a nationwide population-based study of 371,000 pregnancies. BJOG Int J Obstet Gynaecol 2008; 115: 842–850.
Walker JJ . Pre-eclampsia. Lancet 2000; 356: 1260–1265.
Mihu D, Razvan C, Malutan A, Mihaela C . Evaluation of maternal systemic inflammatory response in preeclampsia. Taiwan J Obstet Gynecol 2015; 54: 160–166.
Leng CH, Chen HW, Chang LS, Liu HH, Liu HY, Sher YP, Chang YW, Lien SP, Huang TY, Chen MY, Chou AH, Chong P, Liu SJ . A recombinant lipoprotein containing an unsaturated fatty acid activates NF-kappaB through the TLR2 signaling pathway and induces a differential gene profile from a synthetic lipopeptide. Mol Immunol 2010; 47: 2015–2021.
Cotechini T, Graham CH . Aberrant maternal inflammation as a cause of pregnancy complications: a potential therapeutic target? Placenta 2015; 36: 960–966.
Livingston JC, Livingston LW, Ramsey R, Mabie BC, Sibai BM . Magnesium sulfate in women with mild preeclampsia: a randomized controlled trial. Obstet Gynecol 2003; 101: 217–220.
Vezzani A, Maroso M, Balosso S, Sanchez MA, Bartfai T . IL-1 receptor/Toll-like receptor signaling in infection, inflammation, stress and neurodegeneration couples hyperexcitability and seizures. Brain Behav Immun 2011; 25: 1281–1289.
Hart LA, Sibai BM . Seizures in pregnancy: epilepsy, eclampsia, and stroke. Semin Perinatol 2013; 37: 207–224.
Vezzani A, Ravizza T, Balosso S, Aronica E . Glia as a source of cytokines: implications for neuronal excitability and survival. Epilepsia 2008; 49 ((Suppl 2)): 24–32.
Pernhorst K, Herms S, Hoffmann P, Cichon S, Schulz H, Sander T, Schoch S, Becker AJ, Grote A . TLR4, ATF-3 and IL8 inflammation mediator expression correlates with seizure frequency in human epileptic brain tissue. Seizure 2013; 22: 675–678.
Ganem EM, Castiglia YM . [Anesthesia in pre-eclampsia.]. Rev Bras Anestesiol 2002; 52: 481–497.
Elsharnouby NM, Elsharnouby MM . Magnesium sulphate as a technique of hypotensive anaesthesia. Br J Anaesth 2006; 96: 727–731.
Alday Munoz E, Una Orejon R, Redondo Calvo FJ, Criado Jimenez A . [Magnesium in anesthesia and postoperative recovery care]. Rev Esp Anestesiol Reanim 2005; 52: 222–234.
Dowling O, Chatterjee PK, Gupta M, Tam Tam HB, Xue X, Lewis D, Rochelson B, Metz CN . Magnesium sulfate reduces bacterial LPS-induced inflammation at the maternal-fetal interface. Placenta 2012; 33: 392–398.
Su NY, Peng TC, Tsai PS, Huang CJ . Phosphoinositide 3-kinase/Akt pathway is involved in mediating the anti-inflammation effects of magnesium sulfate. J Surg Res 2013; 185: 726–732.
Rochelson B, Dowling O, Schwartz N, Metz CN . Magnesium sulfate suppresses inflammatory responses by human umbilical vein endothelial cells (HuVECs) through the NFkappaB pathway. J Reprod Immunol 2007; 73: 101–107.
Lee CY, Jan WC, Tsai PS, Huang CJ . Magnesium sulfate mitigates acute lung injury in endotoxemia rats. J Trauma 2011; 70: 1177–1185 (discussion 1185).
Bar J, Ben-Haroush A, Feldberg D, Hod M . The pharmacologic approach to the prevention of preeclampsia: from antiplatelet, antithrombosis and antioxidant therapy to anticonvulsants. Curr Med Chem Cardiovasc Hematol Agents 2005; 3: 181–185.
McCarthy FP, Kingdom JC, Kenny LC, Walsh SK . Animal models of preeclampsia; uses and limitations. Placenta 2011; 32: 413–419.
Tortella FC, Rose J, Robles L, Moreton JE, Hughes J, Hunter JC . EEG spectral analysis of the neuroprotective kappa opioids enadoline and PD117302. J Pharmacol Exp Ther 1997; 282: 286–293.
Faas MM, Schuiling GA, Baller JF, Visscher CA, Bakker WW . A new animal model for human preeclampsia: ultra-low-dose endotoxin infusion in pregnant rats. Am J Obstet Gynecol 1994; 171: 158–164.
Racine RJ . Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol 1972; 32: 281–294.
Coates BJ, Broderick TL, Batia LM, Standley CA . MgSO4 prevents left ventricular dysfunction in an animal model of preeclampsia. Am J Obstet Gynecol 2006; 195: 1398–1403.
Proposal for revised clinical and electroencephalographic classification of epileptic seizures. From the Commission on Classification and Terminology of the International League Against Epilepsy. Epilepsia 1981; 22: 489–501.
Krumholz A, Wiebe S, Gronseth G, Shinnar S, Levisohn P, Ting T, Hopp J, Shafer P, Morris H, Seiden L, Barkley G, French J, Quality Standards Subcommittee of the American Academy of Neurology, American Epilepsy Society. Practice Parameter: evaluating an apparent unprovoked first seizure in adults (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Neurology 2007; 69: 1996–2007.
Sahay AS, Patil VV, Sundrani DP, Joshi AA, Wagh GN, Gupte SA, Joshi SR . A longitudinal study of circulating angiogenic and antiangiogenic factors and AT1-AA levels in preeclampsia. Hypertens Res 2014; 37: 753–758.
Kulmala L, Phupong V . Combination of plasma-soluble fms-like tyrosine kinase 1 and uterine artery Doppler for the prediction of preeclampsia in cases of elderly gravida. Hypertens Res 2014; 37: 538–542.
Hirashima C, Ohkuchi A, Takahashi K, Suzuki H, Matsubara S, Suzuki M . A novel three-step approach for predicting the imminent onset of preeclampsia within 4 weeks after blood sampling at 19-31 weeks of gestation. Hypertens Res 2014; 37: 519–525.
Costantine MM, Tamayo E, Lu F, Bytautiene E, Longo M, Hankins GD, Saade GR . Using pravastatin to improve the vascular reactivity in a mouse model of soluble fms-like tyrosine kinase-1-induced preeclampsia. Obstet Gynecol 2010; 116: 114–120.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, Libermann TA, Morgan JP, Sellke FW, Stillman IE, Epstein FH, Sukhatme VP, Karumanchi SA . Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest 2003; 111: 649–658.
Walsh SK, English FA, Johns EJ, Kenny LC . Plasma-mediated vascular dysfunction in the reduced uterine perfusion pressure model of preeclampsia: a microvascular characterization. Hypertension 2009; 54: 345–351.
Salas-Ramirez M, Ariza Andraca R, Frati Munari A, Munoz H, Altamirano P . Effect of plasma volume expansion on auricular natriuretic peptide in non-dependent insulin diabetic patients with autonomic neuropathy. Arch Med Res 1995; 26: 35–40.
Molnar M, Suto T, Toth T, Hertelendy F . Prolonged blockade of nitric oxide synthesis in gravid rats produces sustained hypertension, proteinuria, thrombocytopenia, and intrauterine growth retardation. Am J Obstet Gynecol 1994; 170: 1458–1466.
Lin F, Zeng P, Xu Z, Ye D, Yu X, Wang N, Tang J, Zhou Y, Huang Y . Treatment of Lipoxin A(4) and its analogue on low-dose endotoxin induced preeclampsia in rat and possible mechanisms. Reprod Toxicol 2012; 34: 677–685.
LaMarca BB, Bennett WA, Alexander BT, Cockrell K, Granger JP . Hypertension produced by reductions in uterine perfusion in the pregnant rat: role of tumor necrosis factor-alpha. Hypertension 2005; 46: 1022–1025.
Huang Q, Liu L, Hu B, Di X, Brennecke SP, Liu H . Decreased seizure threshold in an eclampsia-like model induced in pregnant rats with lipopolysaccharide and pentylenetetrazol treatments. PLoS ONE 2014; 9: e89333.
Johnson AC, Tremble SM, Chan SL, Moseley J, LaMarca B, Nagle KJ, Cipolla MJ . Magnesium sulfate treatment reverses seizure susceptibility and decreases neuroinflammation in a rat model of severe preeclampsia. PLoS ONE 2014; 9: e113670.
Coussons-Read ME, Okun ML, Nettles CD . Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain Behav Immun 2007; 21: 343–350.
Anim-Nyame N, Gamble J, Sooranna SR, Johnson MR, Steer PJ . Microvascular permeability is related to circulating levels of tumour necrosis factor-alpha in pre-eclampsia. Cardiovasc Res 2003; 58: 162–169.
Borekci B, Aksoy H, Al RA, Demircan B, Kadanali S . Maternal serum interleukin-10, interleukin-2 and interleukin-6 in pre-eclampsia and eclampsia. Am J Reprod Immunol 2007; 58: 56–64.
Sharma A, Satyam A, Sharma JB . Leptin, IL-10 and inflammatory markers (TNF-alpha, IL-6 and IL-8) in pre-eclamptic, normotensive pregnant and healthy non-pregnant women. Am J Reprod Immunol 2007; 58: 21–30.
Sibai B, Romero R, Klebanoff MA, Rice MM, Caritis S, Lindheimer MD, Van Dorsten JP, Landon M, Miodovnik M, Dombrowski M, Meis P, Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Maternal plasma concentrations of the soluble tumor necrosis factor receptor 2 are increased prior to the diagnosis of preeclampsia. Am J Obstet Gynecol 2009; 200 ((630)): e631–e638.
Guven MA, Coskun A, Ertas IE, Aral M, Zencirci B, Oksuz H . Association of maternal serum CRP, IL-6, TNF-alpha, homocysteine, folic acid and vitamin B12 levels with the severity of preeclampsia and fetal birth weight. Hypertens Pregnancy 2009; 28: 190–200.
Schneiders J, Fuchs F, Damm J, Herden C, Gerstberger R, Soares DM, Roth J, Rummel C . The transcription factor nuclear factor interleukin 6 mediates pro- and anti-inflammatory responses during LPS-induced systemic inflammation in mice. Brain Behav Immun 2015; 48: 147–164.
Kumar A, Begum N, Prasad S, Agarwal S, Sharma S . IL-10, TNF-alpha & IFN-gamma: potential early biomarkers for preeclampsia. Cell Immunol 2013; 283: 70–74.
Siljee JE, Wortelboer EJ, Koster MP, Imholz S, Rodenburg W, Visser GH, de Vries A, Schielen PC, Pennings JL . Identification of interleukin-1 beta, but no other inflammatory proteins, as an early onset pre-eclampsia biomarker in first trimester serum by bead-based multiplexed immunoassays. Prenat Diagn 2013; 33: 1183–1188.
Kalinderis M, Papanikolaou A, Kalinderi K, Ioannidou E, Giannoulis C, Karagiannis V, Tarlatzis BC . Elevated serum levels of interleukin-6, interleukin-1beta and human chorionic gonadotropin in pre-eclampsia. Am J Reprod Immunol 2011; 66: 468–475.
Vitoratos N, Economou E, Iavazzo C, Panoulis K, Creatsas G . Maternal serum levels of TNF-alpha and IL-6 long after delivery in preeclamptic and normotensive pregnant women. Mediators Inflamm 2010; 2010: 908649.
Cipolla MJ, Pusic AD, Grinberg YY, Chapman AC, Poynter ME, Kraig RP . Pregnant serum induces neuroinflammation and seizure activity via TNFalpha. Exp Neurol 2012; 234: 398–404.
Aagaard-Tillery KM, Silver R, Dalton J . Immunology of normal pregnancy. Semin Fetal Neonatal Med 2006; 11: 279–295.
Rusterholz C, Hahn S, Holzgreve W . Role of placentally produced inflammatory and regulatory cytokines in pregnancy and the etiology of preeclampsia. Semin Immunopathol 2007; 29: 151–162.
van den Broek NR, Letsky EA . Etiology of anemia in pregnancy in south Malawi. Am J Clin Nutr 2000; 72: 247S–256S.
Katz VL, Farmer R, Kuller JA . Preeclampsia into eclampsia: toward a new paradigm. Am J Obstet Gynecol 2000; 182: 1389–1396.
Riazi K, Galic MA, Pittman QJ . Contributions of peripheral inflammation to seizure susceptibility: cytokines and brain excitability. Epilepsy Res 2010; 89: 34–42.
Riazi K, Galic MA, Kuzmiski JB, Ho W, Sharkey KA, Pittman QJ . Microglial activation and TNFalpha production mediate altered CNS excitability following peripheral inflammation. Proc Natl Acad Sci USA 2008; 105: 17151–17156.
Lonsdale D, Burnham WM . The anticonvulsant effects of allopregnanolone against amygdala-kindled seizures in female rats. Neurosci Lett 2007; 411: 147–151.
Tchekalarova J, Kubova H, Mares P . Biphasic effect of chronic postnatal caffeine treatment on cortical epileptic afterdischarges during ontogeny in rats. Brain Res 2006; 1082: 43–49.
Banks WA . Blood-brain barrier transport of cytokines: a mechanism for neuropathology. Curr Pharmaceut Des 2005; 11: 973–984.
Goehler LE, Gaykema RP, Nguyen KT, Lee JE, Tilders FJ, Maier SF, Watkins LR . Interleukin-1beta in immune cells of the abdominal vagus nerve: a link between the immune and nervous systems? J Neurosci 1999; 19: 2799–2806.
Laflamme N, Rivest S . Toll-like receptor 4: the missing link of the cerebral innate immune response triggered by circulating gram-negative bacterial cell wall components. FASEB J 2001; 15: 155–163.
Block ML, Zecca L, Hong JS . Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci 2007; 8: 57–69.
Gonzalez-Scarano F, Baltuch G . Microglia as mediators of inflammatory and degenerative diseases. Annu Rev Neurosci 1999; 22: 219–240.
Altman D, Carroli G, Duley L, Farrell B, Moodley J, Neilson J, Smith D, Magpie Trial Collaboration Group. Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo-controlled trial. Lancet 2002; 359: 1877–1890.
Sibai BM . Magnesium sulfate is the ideal anticonvulsant in preeclampsia-eclampsia. Am J Obstet Gynecol 1990; 162: 1141–1145.
Mittendorf R, Pryde PG . Magnesium sulfate for the prevention of cerebral palsy. N Engl J Med 2009; 360: 189–190 (author reply 190).
Pryde PG, Mittendorf R . Contemporary usage of obstetric magnesium sulfate: indication, contraindication, and relevance of dose. Obstet Gynecol 2009; 114: 669–673.
Ohno Y, Kawai M, Morikawa S, Sakakibara K, Tanaka K, Ishikawa K, Kikkawa F . Management of eclampsia and stroke during pregnancy. Neurol Med Chir (Tokyo) 2013; 53: 513–519.
Duley L, Meher S, Jones L . Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database Syst Rev 2013; 7: CD001449.
Cotton DB, Hallak M, Janusz C, Irtenkauf SM, Berman RF . Central anticonvulsant effects of magnesium sulfate on N-methyl-D-aspartate-induced seizures. Am J Obstet Gynecol 1993; 168: 974–978.
Amash A, Holcberg G, Sapir O, Huleihel M . Placental secretion of interleukin-1 and interleukin-1 receptor antagonist in preeclampsia: effect of magnesium sulfate. J Interferon Cytokine Res 2012; 32: 432–441.
Acknowledgements
We thank Lijun Dai, Chengjie Liang, Jia Chen and Bihui Hu of Guangzhou Medical University for their help with the animal experiments. We also thank Dr Gendie Lash for her contribution in reviewing the manuscript. This study was supported by the National Natural Sciences Foundation of China (81170594, 30471828 and 30973206).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, L., Han, X., Huang, Q. et al. Increased neuronal seizure activity correlates with excessive systemic inflammation in a rat model of severe preeclampsia. Hypertens Res 39, 701–708 (2016). https://doi.org/10.1038/hr.2016.53
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.53
Keywords
This article is cited by
-
MRI characteristics of brain edema in preeclampsia/eclampsia patients with posterior reversible encephalopathy syndrome
BMC Pregnancy and Childbirth (2021)
-
Cyclosporin A ameliorates eclampsia seizure through reducing systemic inflammation in an eclampsia-like rat model
Hypertension Research (2020)
-
Targeting inflammation to reduce seizure severity in an experimental model of eclampsia
Hypertension Research (2020)
-
Nicotine Alleviates Cortical Neuronal Injury by Suppressing Neuroinflammation and Upregulating Neuronal PI3K-AKT Signaling in an Eclampsia-Like Seizure Model
Neurotoxicity Research (2020)
-
Neuroimaging findings in women who develop neurologic symptoms in severe preeclampsia with or without eclampsia
Hypertension Research (2018)