Abstract
Adverse changes in retinal microvasculature caliber are associated with incident hypertension, coronary heart disease and stroke. The absence of a nocturnal dipping in arterial pressure may induce changes throughout the vascular tree, including the retinal microvasculature, but the later link is not sufficiently studied. We explored the relationship between retinal vessel caliber and dipping status in a group of black and white teachers. The study included black (n=68) and white (n=81) men (24–66 years) from the SABPA study. We measured 24 h ambulatory blood pressure and the percentage mean arterial pressure dipping(%MAPdip) was calculated as (diurnal MAP−nocturnal MAP)/diurnal MAP × 100. Retinal images were captured and the central retinal artery equivalent (CRAE) and central retinal vein equivalent (CRVE) calculated. Black men demonstrated higher diurnal and nocturnal MAP (P⩽0.001) and a lesser %MAPdip compared with white men (P=0.047). When stratified by dipping status, black non-dippers (n=33) revealed an increased CRVE (P<0.001) compared with their dipper counterparts (n=35). In black men, CRVE was negatively (R2=0.38, β=−0.47, P<0.001) associated with %MAPdip independent of 24 h MAP or nocturnal MAP. CRVE also associated negatively with dipping status as a dichotomized variable (R2=0.29, β=−0.32, P=0.006), independent of 24 h MAP. These associations were absent in the white men. In conclusion, in this group of black men, a non-dipping blood pressure profile was associated with a larger CRVE, suggesting microvascular deterioration due to the absence of nocturnal dipping in blood pressure. This may add to our understanding of the stroke risk in black populations.
Similar content being viewed by others
Introduction
Hypertension is associated with structural and functional changes at both the micro- and macrovasculature level.1 The retina represents an unique site whereby direct visualization of hypertension-related microvasculature changes can be observed.2 The development of precise quantification techniques of vessel caliber measurement has demonstrated the clinical importance of early alterations occurring in retinal microvascular calibers. In this respect, it has become well established that changes in retinal microvascular caliber are strongly related to elevated blood pressure2 and arterial stiffness3 and predict incident hypertension,4 coronary heart disease5 and stroke.6 As various similarities exist between the anatomy and physiology of the retinal microvasculature and that of the coronary and cerebral circulation,7 it is thought that inferences can be made regarding the human microvasculature as a whole using information obtained from the retinal microcirculation.2
A non-dipping nocturnal blood pressure profile is a well-established cardiovascular risk factor8 as it is associated with pronounced hypertension-related target organ damage9 and may add to cardiovascular risk prediction irrespective of blood pressure status.10 Considering the known relationship between the retinal microvasculature and blood pressure, it seems feasible that a sustained elevated nocturnal blood pressure could induce independent changes in the retinal vessel caliber.
In response to elevated BP, retinal arteriolar narrowing is mostly observed2 with no change or widening of the retinal venular circulation.11, 12 Although a non-dipping blood pressure is associated with hypertensive retinopathy,13 previous studies have failed to observe a relationship with mild hypertensive retinopathy (grade I/II)14 or retinal microvascular calibers.15, 16
In the context of South Africa, investigating the relationship between retinal vessel calibers and dipping status is of added importance due to the high prevalence of hypertension17 and the lack of data regarding retinal vessel calibers, and consequently the microvasculature. This is further emphasized by a recent small South African study where endothelium-independent microvascular function in forearm skin microvessels was attenuated in black compared with white men.18 We therefore investigated the relationship of retinal arteriolar and venular calibers with nocturnal blood pressure dipping in black and white participants.
Methods
Design and recruitment of participants
The Sympathetic activity and Ambulatory Blood Pressure in Africans (SABPA) study is a prospective cohort study that collected data from urban-dwelling black and white South African teachers between the ages of 20 and 65 years. The inclusion/exclusion criteria and other study information have been published elsewhere.19 All participants taking part in the baseline phase were re-invited to take part in the 3-year follow-up performed between February and June of 2011 and 2012. As retinal images were only captured at follow-up, the data were explored cross-sectionally.
Owing to the influence of menopausal status on the degree of nocturnal dipping, women were excluded from the analysis.20 A total of 180 men, representing 89% of the baseline male participants, took part in the SABPA follow-up study. We excluded men with missing data for static retinal vessel analysis (n=20), and thereafter participants with a 24 h or nocturnal inflation rate <70% (n=10). A total of 68 black and 82 white men were therefore included in this substudy. All objectives and procedures were explained to the participants prior to their involvement in the study, and signed informed consent was obtained by all participants. The study complied with the Declaration of Helsinki (2008) and was approved by the Health Research Ethics Committee of the North-West University, Potchefstroom Campus (Approval number 0003607S6).
Organizational procedures
On day 1, an ambulatory blood pressure monitoring (ABPM) and 2-lead electrocardiogram device (CE120 CardioTens; Meditech, Budapest, Hungary) was fitted to the non-dominant arm of teachers while at their school between 0700 and 0800 hours. Appropriate cuff sizes were used. Thereafter teachers resumed their normal working routines. Participants were provided with a 24 h diet. At 1500 hours participants arrived at the North-West University and retinal images were captured between 1500 and 1700. At 1700 hours participants were transported to a metabolic unit and received supper. The last food and drink was consumed at 2030 hours. Participants were requested to go to bed by 2200, and to remain fasting overnight.
From 0705 hours of day 2, anthropometric measurements were taken. Thereafter participants rested in a semirecumbent position for 2 h. The ABPM devices were removed at 0730 and the Actiheart physical activity monitor (GB0/67703, CamNtech, Cambridgeshire, UK) was fitted and worn for 7 days. At the end of the 2-h resting period, blood sampling commenced. Blood samples were processed using standardized methods to obtain serum and plasma fractions that were stored at −80 °C until required for further analysis.
Anthropometric measurements
Measurements were performed in triplicate using standardized procedures.21 Body height was measured to the nearest 0.1 cm using a stadiometer (Invicta Stadiometer, IP 1465, London, UK), body mass to the nearest 0.1 kg using a Precision Health Scale (A & D Company,Tokyo, Japan) and waist circumference to the nearest 0.1 cm using an non-stretchable flexible 7 mm wide metal tape (Holtain, Crosswell, Wales). Body mass index was subsequently calculated (kg m−2).
Ambulatory blood pressure measurements
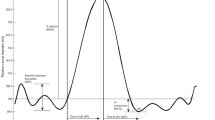
ABPM devices were fitted between 0700 and 0800 of day 1 and removed at 0730 on day 2. During the day (0700–2200 hours) measurements were taken at 30 min intervals whereas nighttime blood pressure (2200–0600) was taken hourly. Once the ABPM devices were removed, the BP data were downloaded into a database using CardioVisions 1.20 Personal Edition software (Meditech). Over the 24- h period that the ABPM devices were worn, we achieved a successful inflation rate of 87.5±7.3% for the black men and 91.4±7.0% for the white men. Participants were classified as hypertensive by either being on antihypertensive medication or having a 24 h systolic blood pressure (SBP) ⩾130 mm Hg and/or a diastolic blood pressure (DBP) ⩾80 mm Hg.22 MAP was calculated as ((SBP−DBP)/3)+DBP. We investigated nocturnal blood pressure dipping either as a categorical variable determined from the CardioVisions software (classified as non-dipper when the diurnal index was below 10%) or as a continuous variable by calculating the percentage mean arterial pressure (MAP) dipping (%MAPdip): (diurnal MAP−nocturnal MAP)/diurnal MAP × 100. Similar calculations were used to determine the percentage SBP dipping (%SBPdip) and percentage DBP dipping (%DBPdip).
Retinal vessel caliber measurements
Retinal photography was performed using the Dynamic Retinal Vessel Analyzer (Imedos, Jena, Germany) fitted with a Zeiss Fundus camera FF-450plus. No intake of food or fluid was permitted 1 h prior to the measurement. Participants also refrained from smoking and exercise during this time. Fifteen minutes prior to the measurement a drop of Tropicamide (1% Alcon) was administered in the right eye to induce mydriatic conditions. Monochrome and color retinal images were captured (using Visualis 2.81 software) at a 50° camera angle. The monochrome image underwent vessel analysis using VesselMap2 software. Briefly all vessels located between 0.5 and 1.0 optic disc diameters from the outer margin of the optic disc were marked as either arteriole or venule. The color image assisted with the identification of vessel type. The central retinal artery equivalent (CRAE) and central retinal vein equivalent (CRVE) were subsequently calculated using revised formulas proposed by Knudtson et al.,23 where only the six largest arteriole and six largest venular segments were included in the calculation. The arteriolar-to-venular ratio (AVR) was calculated as CRAE/CRVE. The presence of arteriolar–venular nicking was determined by an ophthalmologist. Both CRAE and CRVE were measured in measuring units (MU). These units correspond to micrometer (1:1) if the dimensions of the eye are similar to the normal Gullstrand eye. The reproducibility of our analysis has previously been described.24
Biochemical measurements
Plasma glucose (sodium fluoride) and serum total and high-density lipoprotein cholesterol (HDL-C), triglycerides, γ-glutamyltransferase, high sensitivity and C-reactive protein (CRP) were analyzed using a sequential multiple analyzer (Cobus Integra 400 Plus; Roche, Basel, Switzerland). Cotinine was determined using a homogeneous immunoassay (modular automated analyzer; Roche). Because of the large proportion of participants with a cotinine value of <50 ng ml−1, we used self-reported smoking to identify current smokers. In the event that a participant indicated that they were a non-smoker, but had a cotinine value ⩾50 ng ml−1, they were reclassified as a smoker.
Statistical analysis
Data analysis was performed using Statistica v 12.0 (Statsoft, Tulsa, OK, USA). Variables that did not follow a Gaussian distribution (body mass index, total energy expenditure, HDL-C, total cholesterol:HDL-C, triglycerides, glucose, CRP, cGGT) were logarithmically transformed. Comparisons between groups were performed with independent t-tests where data were presented as arithmetic mean with the standard deviation and logarithmically transformed data presented as the geometric mean with 5th and 95th percentiles. Chi square tests were used to compare proportions between groups. Single (presented with scatterplots), partial and multiple regression analyses were performed to test the association between retinal vessel calibers and %MAPdip or dipping status (dichotomous variable). When performing partial correlations, associations with CRAE were adjusted for CRVE and vice versa.25 To test for independent associations between retinal vessel calibers and indices of dipping status, we performed multiple regression analysis. In particular, a forward stepwise approach was used in order to only highlight the most significant contributors to the variance in the particular retinal vessel caliber. For the forward stepwise multiple regression analysis, the following variables were considered for entry into the model: age, body mass index, waist circumference, smoking, antihypertensive medication, total cholesterol, HDL-C, total cholesterol:HDL-C, triglycerides, total energy expenditure, glucose and CRP. We chose our covariates by identifying which of these variables were significantly related to CRAE, CRVE or %MAPdip in single regression analysis. The final model included age, log glucose, log CRP, total cholesterol and 24 h MAP, which were included as covariates along with either %MAPdip or dipping status serving as the main independent variable. Indeed, glucose, lipid parameters, inflammation and blood pressure have previously been shown to be related to retinal vessel calibers,26 and their inclusion in the model is to help establish whether the relationship between retinal vessel calibers and %MAPdip is independent of these possible mediating factors. When CRAE or CRVE was selected as the dependent variable, CRVE or CRAE was, respectively, included as covariates.25 In sensitivity analysis, one analysis involved patients with diabetes being excluded. In this case diabetes was defined as previously diagnosed with diabetes, on medication to treat diabetes, or a fasting blood glucose level >7 mmol l−1.
Results
Comparisons between groups
The general characteristics of the black and white participants are presented in Table 1. Despite black men being younger than the white men, they presented with higher glucose and CRP, a worse diurnal and nocturnal BP profile, and lesser SBP and MAP nocturnal dipping. The CRVE was also significantly larger in the black group (P<0.0001).
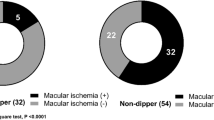
We compared dippers and non-dippers in Supplementary Table S1. The various biochemical, anthropometric and cardiovascular parameters did not differ between black or white dippers and non-dippers. In black participants, the exception was nocturnal BP (MAP: 101±13 vs. 87±10 mm Hg; P<0.001) and the CRVE (259±18 vs. 243±17 MU, P<0.001) which were elevated, whereas the AVR was lower (0.58±0.05 vs. 0.61±0.06; P=0.036) in the non-dipper group. White non-dippers were less physically active compared with the dipper group. In contrast to the retinal profile observed in black non-dippers, the CRVE and AVR did not differ between white dippers and non-dippers. There was however a tendency for CRAE to be narrower in the non-dipper white group (P=0.054).
Single and partial regression analysis
Scatter-plots depicting the relationship between retinal vessel calibers and the %MAPdip are shown in Figure 1. In the black men, AVR associated positively, whereas CRVE associated negatively with the %MAPdip. These results remained robust when substituting %MAPdip with dipping status (AVR: r=0.25; P=0.036; CRVE: r=0.43; P<0.001). The associations between CRVE with %MAPdip (r=−0.55; P<0.001) or dipping status (r=−0.42; P<0.001) remained significant when adjusting for CRAE. However, when adjusting for CRVE, the relationship between CRAE and %MAPdip became significant (r=0.26; P=0.033).
In the white group, CRAE was positively associated with %MAPdip (r=0.24; P=0.032), but not dipping status. This association became nonsignificant when adjusting for CRVE.
Multiple linear regression analysis
Following multiple adjustments, CRVE negatively associated with both %MAPdip and dipping status, whereas AVR was positively associated with %MAPdip in black men only (Table 2 and Supplementary Table S2). Similar results were obtained when entering %DBPdip or %SBPdip in place of %MAPdip (with a subsequent swop of 24 hMAP with either 24 h DBP or 24 h SBP as an independent variable where appropriate) into the model.
In the white men, retinal vessel calibers were not associated with either %MAPdip or dipping status. We further substituted %MAPdip with %DBPdip or %SBPdip (with a subsequent swop of 24 h MAP with either 24 h DBP or 24 h SBP as an independent variable where appropriate), but the result remained unchanged.
Because 78% of black and 58% of white men were hypertensive, we repeated the analysis between retinal vessel caliber and %MAPdip or dipping status in hypertensives alone. In both black and white hypertensive men the results remained similar, with the exception of an association with CRAE. In the black men, a positive association emerged between CRAE and %MAPdip (R2=0.27; β=0.32 (0.02; 0.62); P=0.043).
Sensitivity analysis
After excluding either HIV-infected individuals (n=14) or participants with diabetes (n=13), or by removing 24 h MAPfrom the model, the result between %MAPdip and CRVE in black men remained largely unchanged. We also additionally adjusted for the presence of AV nicking, which was more prominent among the black participants. Lastly we substituted glucose with body mass index in the model. All of these analyses did not influence the aforementioned relationship between %MAPdip and CRVE in the black men.
Discussion
In this study, we demonstrated that retinal venular widening is independently associated with nocturnal non-dipping in a group of black South African male teachers. These associations were absent in the white teachers. These results suggest that a non-dipping nocturnal BP profile, especially in black men, may adversely affect the retinal microvasculature with possible implications for the microvasculature of other organ systems.
Because of the relationship between retinal vascular caliber and BP, we hypothesized that a sustained increase in nocturnal BP (i.e. a non-dipping BP profile) would elicit adverse retinal microvascular caliber changes. In particular we expected to see that retinal arteriolar narrowing would be strongly related to nocturnal non-dipping. Previous studies14, 15, 16 failed to observe an independent relationship between mild hypertensive retinopathy or retinal vascular calibers with nocturnal BP dipping status. However, these findings could possibly have been influenced by the methodology used. Noteworthy, in these previously mentioned studies, mild hypertensive retinopathy was selected as a categorical variable,14 or the central retinal vessel equivalents were calculated16 using formulas, which could increase vessel caliber variability based on the number of vessels included in the equation.23 In the latter example, it was demonstrated that this variability impacted on the vessel caliber blood pressure relationship. Using the revised formulas proposed by Knudtson et al.23 to determine our vessel equivalents, we initially observed arteriolar narrowing with reduced nocturnal dipping in the white men following single regression analysis. This relationship however became nonsignificant following multiple adjustments and therefore is in agreement with the available data.14, 15, 16 The result between %MAPdip and CRAE in black hypertensive men, although plausible needs to be further explored as CRAE did not differ between black hypertensive dippers and non-dippers (143 vs. 147 MU, P=0.28).
In black men who displayed a worse 24 h BP profile and less %MAPdip compared with the whites, retinal venular widening correlated independently with a decline in the degree of nocturnal dipping. Venular widening has in the past been associated with adverse hemodynamic loading conditions,11 and itself been shown to be indicative of incident hypertension.4 The current result therefore extends our knowledge that nocturnal non-dipping not only contributes to hypertensive retinopathy,13 but possibly also to venular widening in black populations. Importantly the association between CRVE and %MAPdip was independent of AV nicking prevalence.
In this study, we were unable to determine the mechanism contributing to venular widening. Nevertheless venular widening may have occurred due to the sustained increase in arterial pressure associated with a non-dipping status. This is in line with the notion that venular widening may partly be attributed to retinal hypoxia27 or hypoperfusion28 as a consequence of hypertensive damage to the microcirculation.25 Alternatively, it is known that retinal venular widening may infer increased cardiovascular risk as it is related to incident stroke,6 diabetic retinopathy29 and markers associated with atherosclerosis such as inflammation and adverse lipid profiles.26 In response to the observation that retinal arteriolar and venular widening was associated with certain atherosclerotic risk factors, Ikram et al.30 speculated that vessel widening, or rather an increase in intraluminal diameter, may result from interference of the endothelial surface layer by these factors. Although glucose levels and the inflammatory marker, CRP, were elevated in the black group when compared with the white group, these variables did not differ between black dippers and non-dippers. It is therefore unlikely that these pro-atherogenic risk markers were the major driver of venular widening in non-dippers in this study.
Besides the sustained increase in arterial pressure (%MAPdip), a nocturnal non-dipping status may contribute to retinal microvascular changes via other mechanisms. Indeed, a blunted nocturnal BP dipping profile is associated with among others, autonomic dysfunction and salt sensitivity related to volume overload.31 Available data suggest that black South Africans could be more prone to salt-sensitive hypertension than whites.32 Additionally, data from our group propose that the black men of the SABPA study utilizing defensive coping mechanism may present with disturbed sympathovagal balance and depressed heart rate variability, indicative of autonomic dysfunction.33 This latter observation may have implications to the findings of the present study as increased levels of the autonomic nervous system activity marker, 24 h urinary epiniphrine:creatinine ratio, are independently associated with retinal venular widening and arteriolar narrowing.34 The propensity of black Africans to be more salt-sensitive and display signs of autonomic dysfunction,32, 33 coupled with the tendency for the prevalence of non-dippers to be higher among the black cohort (dipping status and %MAPdip), could also explain the associations found between retinal vessel caliber and %MAPdip in this study.
Because this is a cross-sectional study, the possible implications of our findings need to be interpreted with caution. It is important to note that retinal venular widening is not a precise marker for a specific condition as it is associated with among others, an adverse lipid profile, inflammation,26 and incident hypertension,4 coronary heart disease5 and stroke.6 Nevertheless, nocturnal non-dipping, the prevalence of which tended to be higher in this studies’ black group, is itself associated with various cardiovascular end points such as stroke.35 Hypertension prevalence may also be higher in the black population of South Africa.36 Since similarities exist between the retinal and cerebral circulation,7 hypertensive blacks who display a combination of retinal venular widening and a non-dipping nocturnal blood pressure may have an added increased cardiovascular (possibly stroke) risk. But this notion requires further study.
Considering the cross-sectional design, causality cannot be inferred. Although we try to explain our findings by suggesting that a sustained increase in nocturnal blood pressure may contribute to increased CRVE, the relationship could work in the opposite direction. It is feasible that changes in vascular function also contributing to larger CRVE could be the cause of the attenuated nocturnal dipping. Another consideration could be the natural progression of vascular changes in our ethnic cohort. Adverse vascular changes could start occurring at a younger age in black South Africans,37 with probable implications even at the microvasculature level. This could translate into microvascular differences being observed at any given age between black and white South Africans. Indeed, healthy back South Africans were found to have attenuated endothelium-independent microvascular functional responses in the skin when compared with whites.18 Longitudinal studies are however currently underway to further investigate the previously mentioned issues. Lastly although we expected to observe associations between CRAE and %MAPdip, the findings of an independent association between CRVE and %MAPdip in black men are, while hypothesis generating, not completely unexpected.11 Nevertheless, these findings warrant confirmation in larger studies.
In conclusion, retinal venular widening is associated with an increase in the degree of nocturnal non-BP dipping but only in black men. This result demonstrates the retinal microvascular changes associated with a non-dipping BP status, which may add to our understanding of stroke risk in black populations.
Disclosure
Any opinion, findings and conclusions or recommendations expressed in this material are those of the author(s) and therefore the National Research Foundation does not accept any liability in regard thereto.
Change history
14 January 2016
This article has been corrected since Advance Online Publication, and a corrigendum is also printed in this issue.
References
Yannoutsos A, Levy BI, Safar ME, Slama G, Blacher J . Pathophysiology of hypertension: interactions between macro and microvascular alterations through endothelial dysfunction. J Hypertens 2014; 32: 216–224.
Cheung CY, Ikram MK, Sabanayagam C, Wong TY . Retinal microvasculature as a model to study the manifestations of hypertension. Hypertension 2012; 60: 1094–1103.
Lin F, Zhu P, Huang F, Li Q, Yuan Y, Gao Z, Yu P, Lin J, Chen F . Aortic stiffness is associated with the central retinal arteriolar equivalent and retinal vascular fractal dimension in a population along the southeastern coast of China. Hypertens Res 2015; 38: 342–348.
Ding J, Wai KL, McGeechan K, Ikram MK, Kawasaki R, Xie J, Klein R, Klein BB, Cotch MF, Wang JJ, Mitchell P, Shaw JE, Takamasa K, Sharrett AR, Wong TY . Retinal vascular caliber and the development of hypertension: a meta-analysis of individual participant data. J Hypertens 2014; 32: 207–215.
McGeechan K, Liew G, Macaskill P, Irwig L, Klein R, Klein BE, Wang JJ, Mitchell P, Vingerling JR, Dejong PT, Witteman JC, Breteler MM, Shaw J, Zimmet P, Wong TY . Meta-analysis: retinal vessel caliber and risk for coronary heart disease. Ann Intern Med 2009; 151: 404–413.
McGeechan K, Liew G, Macaskill P, Irwig L, Klein R, Klein BE, Wang JJ, Mitchell P, Vingerling JR, de Jong PT, Witteman JC, Breteler MM, Shaw J, Zimmet P, Wong TY . Prediction of incident stroke events based on retinal vessel caliber: a systematic review and individual-participant meta-analysis. Am J Epidemiol 2009; 170: 1323–1332.
Wong TY, Klein R, Klein BE, Tielsch JM, Hubbard L, Nieto FJ . Retinal microvascular abnormalities and their relationship with hypertension, cardiovascular disease, and mortality. Surv Ophthalmol 2001; 46: 59–80.
Birkenhager AM, van den Meiracker AH . Causes and consequences of a non-dipping blood pressure profile. Neth J Med 2007; 65: 127–131.
Mancia G, Parati G . The role of blood pressure variability in end-organ damage. J Hypertens Suppl 2003; 21: S17–S23.
Hermida RC, Ayala DE, Mojon A, Fernandez JR . Blunted sleep-time relative blood pressure decline increases cardiovascular risk independent of blood pressure level—the "normotensive non-dipper" paradox. Chronobiol Int 2013; 30: 87–98.
Kaushik S, Kifley A, Mitchell P, Wang JJ . Age, blood pressure, and retinal vessel diameter: separate effects and interaction of blood pressure and age. Invest Ophthalmol Vis Sci 2007; 48: 557–561.
Sun C, Liew G, Wang JJ, Mitchell P, Saw SM, Aung T, Tai ES, Wong TY . Retinal vascular caliber, blood pressure, and cardiovascular risk factors in an Asian population: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 2008; 49: 1784–1790.
Torun D, Sezer S, Arat Z, Pelit A, Yigit F, Ozdemir FN . The frequency of combined target organ damage and the beneficial effect of ambulatory blood pressure monitoring in never treated mild-to-moderate hypertensive patients. Int Heart J 2005; 46: 1073–1082.
Cuspidi C, Michev I, Meani S, Severgnini B, Fusi V, Corti C, Salerno M, Valerio C, Magrini F, Zanchetti A . Reduced nocturnal fall in blood pressure, assessed by two ambulatory blood pressure monitorings and cardiac alterations in early phases of untreated essential hypertension. J Hum Hypertens 2003; 17: 245–251.
Pose-Reino A, Rodriguez-Fernandez M, Hayik B, Gomez-Ulla F, Carrera-Nouche MJ, Gude-Sampedro F, Estevez-Nunez JC, Mendez-Naya I . Regression of alterations in retinal microcirculation following treatment for arterial hypertension. J Clin Hypertens (Greenwich) 2006; 8: 590–595.
Triantafyllou A, Doumas M, Anyfanti P, Gkaliagkousi E, Zabulis X, Petidis K, Gavriilaki E, Karamaounas P, Gkolias V, Pyrpasopoulou A, Haidich AB, Zamboulis C, Douma S . Divergent retinal vascular abnormalities in normotensive persons and patients with never-treated, masked, white coat hypertension. Am J Hypertens 2013; 26: 318–325.
Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S . Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol 2014; 43: 116–128.
Pienaar PR, Micklesfield LK, Gill JM, Shore AC, Gooding KM, Levitt NS, Lambert EV . Ethnic differences in microvascular function in apparently healthy South African men and women. Exp Physiol 2014; 99: 985–994.
Malan L, Hamer M, Frasure-Smith N, Steyn HS, Malan NT . Cohort Profile: Sympathetic Activity and Ambulatory Blood Pressure in Africans (SABPA) prospective cohort study. Int J Epidemiol 2015; 44: 1814–1822.
Sherwood A, Thurston R, Steffen P, Blumenthal JA, Waugh RA, Hinderliter AL . Blunted nighttime blood pressure dipping in postmenopausal women. Am J Hypertens 2001; 14: 749–754.
Marfell-Jones M, Olds T, Stewart AD, Carter L . International Society for the International Standards for Anthropometric Assessment. International Society for the Advancement of Kinanthropometry (ISAK): Potchefstroom, South Africa. 2006, pp 61–75.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F . 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
Knudtson MD, Lee KE, Hubbard LD, Wong TY, Klein R, Klein BE . Revised formulas for summarizing retinal vessel diameters. Curr Eye Res 2003; 27: 143–149.
Malan NT, Smith W, von Kanel R, Hamer M, Schutte AE, Malan L . Low serum testosterone and increased diastolic ocular perfusion pressure: a risk for retinal microvasculature. Vasa 2015; 44: 435–443.
Liew G, Sharrett AR, Kronmal R, Klein R, Wong TY, Mitchell P, Kifley A, Wang JJ . Measurement of retinal vascular caliber: issues and alternatives to using the arteriole to venule ratio. Invest Ophthalmol Vis Sci 2007; 48: 52–57.
Wong TY, Islam FM, Klein R, Klein BE, Cotch MF, Castro C, Sharrett AR, Shahar E . Retinal vascular caliber, cardiovascular risk factors, and inflammation: the multi-ethnic study of atherosclerosis (MESA). Invest Ophthalmol Vis Sci 2006; 47: 2341–2350.
Saldivar E, Cabrales P, Tsai AG, Intaglietta M . Microcirculatory changes during chronic adaptation to hypoxia. Am J Physiol Heart Circ Physiol 2003; 285: H2064–H2071.
Klijn CJ, Kappelle LJ, van Schooneveld MJ, Hoppenreijs VP, Algra A, Tulleken CA, van Gijn J . Venous stasis retinopathy in symptomatic carotid artery occlusion: prevalence, cause, and outcome. Stroke 2002; 33: 695–701.
Klein R, Myers CE, Lee KE, Gangnon R, Klein BE . Changes in retinal vessel diameter and incidence and progression of diabetic retinopathy. Arch Ophthalmol 2012; 130: 749–755.
Ikram MK, de Jong FJ, Vingerling JR, Witteman JC, Hofman A, Breteler MM, de Jong PT . Are retinal arteriolar or venular diameters associated with markers for cardiovascular disorders? The Rotterdam Study. Invest Ophthalmol Vis Sci 2004; 45: 2129–2134.
Yano Y, Kario K . Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertens Res 2012; 35: 695–701.
Rayner BL, Myers JE, Opie LH, Trinder YA, Davidson JS . Screening for primary aldosteronism—normal ranges for aldosterone and renin in three South African population groups. S Afr Med J 2001; 91: 594–599.
Malan L, Hamer M, Schlaich MP, Lambert G, Ziemssen T, Reimann M, Frasure-Smith N, Amirkhan JH, Schutte R, van Rooyen JM, Mels CM, Fourie CM, Uys AS, Malan NT . Defensive coping facilitates higher blood pressure and early sub-clinical structural vascular disease via alterations in heart rate variability: the SABPA study. Atherosclerosis 2013; 227: 391–397.
Malan NT, von Känel R, Smith W, Lambert GW, Vilser W, Eikelis N, Reimann M, Malan L . Retinal vessel calibre associated with sympathetic activity and depression symptoms in a bi-ethnic cohort of South African men: the SABPA study. In: H Lenasi (ed), Microcirculation in Health and Disease. InTech: Rijeka, Croatia. 2016.
Tsivgoulis G, Vemmos KN, Zakopoulos N, Spengos K, Manios E, Sofia V, Zis V, Mavrikakis M . Association of blunted nocturnal blood pressure dip with intracerebral hemorrhage. Blood Press Monit 2005; 10: 189–195.
Connor M, Rheeder P, Bryer A, Meredith M, Beukes M, Dubb A, Fritz V . The South African stroke risk in general practice study. S Afr Med J 2005; 95: 334–339.
Schutte AE, Huisman HW, Schutte R, Van Rooyen JM, Malan L, Malan NT, Reimann M . Arterial stiffness profiles: investigating various sections of the arterial tree of African and Caucasian people. Clin Exp Hypertens 2011; 33: 511–517.
Acknowledgements
We gratefully acknowledge the voluntary participation of all participants and the contribution of co-investigators and support staff. The present work was partially supported by the North West Department of Education, South African Medical Research Council, National Research Foundation, North-West University, ROCHE Diagnostics South Africa and the Metabolic Syndrome Institute, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
WV is the managing director of IMEDOS Systems UG.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Smith, W., Malan, N., Schutte, A. et al. Retinal vessel caliber and its relationship with nocturnal blood pressure dipping status: the SABPA study. Hypertens Res 39, 730–736 (2016). https://doi.org/10.1038/hr.2016.48
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.48
Keywords
This article is cited by
-
Non-dipping pattern of nocturnal blood pressure as a risk factor for macular ischemia in branch retinal vein occlusion
Scientific Reports (2021)
-
Association Between Caliber of Retinal Vessels and Cardiovascular Disease: a Systematic Review and Meta-Analysis
Current Atherosclerosis Reports (2020)
-
Diminished circadian blood pressure variability in elderly individuals with nuclear cataracts: cross-sectional analysis in the HEIJO-KYO cohort
Hypertension Research (2019)
-
Seasonal variation in nocturnal home blood pressure fall: the Nagahama study
Hypertension Research (2018)
-
Early detection of microvascular dysfunction in hypertension: the holy grail of cardiovascular prevention and risk assessment?
Hypertension Research (2018)