Abstract
The current study investigated physicians’ awareness and use of the Japanese Society of Hypertension Guidelines for the Management of Hypertension 2014 (JSH2014) and is based on the results of a survey performed by the Publicity and Advertisement Committee of JSH. A questionnaire was used to survey physicians’ awareness of the JSH2014, their recommended target blood pressure for hypertensive patients with complications and their use of antihypertensive drugs. Physicians who downloaded a PDF version of JSH2014 during the 6 months after its publication (April–September 2014) were asked to complete an online questionnaire. Of the 7872 respondents, 91% were aware of the JSH and complied partially, mostly or completely with it in their practice. With reference to hypertensive patients, ∼70% of physicians who completed the questionnaire recommended a target blood pressure (BP) of 140/90 mm Hg for an office BP value, and 40% recommended 135/85 mm Hg for a home BP value. Physicians recommended target BP levels of 130/80 mm Hg for patients with diabetes or chronic kidney disease (50–63% of physician surveyed) and for elderly patients with diabetes or kidney disease (45–55% of respondents), whereas they recommended 140/90 mm Hg for elderly patients with low cardiovascular disease risk (56–60% of physician surveyed) and for patients with chronic-phase stroke (40–47% of respondents). The most commonly prescribed combination of antihypertensive drugs was angiotensin receptor blocker (ARB) with calcium channel blocker. In addition, physicians’ first choice of drug for patients with diabetes or chronic kidney disease was most often ARB. Overall, the survey results showed that the new recommendations from the JSH2014 accurately reflect daily clinical practices for hypertension management used by Japanese physicians.
Similar content being viewed by others
Introduction
The Japanese Society of Hypertension (JSH) published their guidelines on the management of hypertension in April 2014.1 The objective of the current study was to investigate physicians’ awareness and use of these guidelines, their evaluation of the modifications in the JSH2014, the target blood pressure (BP) they use for hypertensive patients with or without complications and the antihypertensive agents they commonly use in their practice. For this purpose, we administered a questionnaire to survey Japanese physicians.
Methods
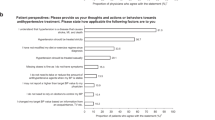
A questionnaire was used to survey the practices of physicians and to determine their awareness and evaluation of modifications in the JSH2014, their target blood pressure for hypertensive patients with or without complications and the antihypertensive drugs they commonly use. Physicians who downloaded a PDF version of the JSH2014 during the 6 months after its publication (April–September 2014) were asked to participate in an online questionnaire. An online survey system was created using the Google Form software in Google Drive (Google, Mountain View, CA, USA). The questionnaire was developed by members of the JSH. The survey was requested before physicians downloaded the JSH2014. The results were analyzed using the response spreadsheet. The survey questions were designed to examine the traits of the physicians, whether they were aware of the JSH-recommended hypertensive management guidelines and their use of these guidelines in their practice. The survey also compared the recommended values used by physicians for hypertensive patients’ office and home BPs, the optimal levels recommended for office BPs and the target BP levels for patients with diabetes or chronic kidney disease, elderly patients with diabetes or kidney disease, patients with low cardiovascular disease risk and patients with chronic-phase stroke with the values recommended in the JSH2014. The survey also contained questions about the physicians’ most commonly prescribed combination of antihypertensive drug treatments and most commonly used antihypertensive drug for hypertensive patients with chronic kidney disease or diabetes.
Results
The traits of the 7872 physicians who completed the questionnaire are shown in Table 1. Men comprised 79% of respondents. With regard to age of the respondents, 90% were 20 to 59 years old and they were evenly distributed within that range. Physicians specializing in internal medicine comprised 79% of respondents, and 71% responded that they practice in hospitals. There were similar proportions of generalists and specialists (Table 1).
The values that physicians recommended for office BP measurements were most often >140 mm Hg for the systolic BP and >90 mm Hg for the diastolic BP (Table 2). However, target values for home BP measurements were slightly more variable; recommended levels were often >135 mm Hg for the systolic BP and >85 mm Hg for the diastolic BP (Table 3), but ∼20% of physicians recommended levels of >130 or 140 mm Hg for the systolic BP and >80 or 90 mm Hg for the diastolic BP.
Physicians’ target BP values were a systolic BP of <130 mm Hg and a diastolic BP of <80 mm Hg for patients with diabetes or chronic kidney disease with proteinuria (Table 4A), and 140 mm Hg for the systolic BP and <90 mm Hg for the diastolic BP for patients with chronic-phase stroke (Table 4B). However, many physicians also used target BP values of 130 mm Hg for the systolic BP and <80 mm Hg for the diastolic BP for patients with chronic-phase stroke. In elderly patients (⩾65 years old), target BP values included a systolic BP of <130 mm Hg and a diastolic BP of <80 mm Hg for patients with diabetes or chronic kidney disease with proteinuria and a systolic BP of <140 mm Hg and a diastolic BP of <90 mm Hg for patients with low cardiovascular disease risk (Table 4C). More than half the physicians surveyed recommended higher target BP values of ∼140/90 mm Hg for older patients with diabetes or chronic kidney disease with proteinuria than for younger patients with these conditions.
Finally, the most common combination of antihypertensive drugs prescribed was ‘angiotensin receptor blocker (ARB) and calcium channel blocker (CCB)’, comprising ∼72% of answers to this question, with the next most common answers being ‘angiotensin converting enzyme (ACE) inhibitor and CCB’, and ‘ARB and diuretic’ (Table 5). The most commonly prescribed antihypertensive drug for hypertensive patients with chronic kidney disease or diabetes was ARB, followed by CCB or ARB (Table 6).
Discussion
This survey demonstrated that most of the physicians who downloaded the JSH2014 managed hypertensive patients in a manner similar to the recommendations from the JSH guidelines. The Japanese physicians surveyed mostly recommended relying on the home BP when there is a discrepancy between the clinic blood pressure and the home blood pressure. The importance of the home BP has long been suggested2 and is now widely recognized by Japanese physicians. In addition, because a meta-analysis demonstrated that the use of β-blockers is less than optimum because of an increased risk of stroke with these drugs compared with other antihypertensive drugs,3 there has been much dispute about the recommendation of β-blockers as first-line drugs in the hypertension guidelines. In general, Japanese physicians agree that β-blockers are not appropriate as first-line drugs. Furthermore, Japanese physicians also recognize the need to establish guidelines to manage hypertension in elderly patients (those who are >75 years old) that are independent from the guidelines used for younger hypertensive patients. The JSH2014 recommends that the target BP in individuals >75 years old should be <150/90 mm Hg, and, if treatment is well tolerated, more aggressive BP control (<140/90 mm Hg) is suggested because of the high incidence of stroke in the Japanese population. This survey result indicates that Japanese physicians modify target BP levels for elderly hypertensive patients. Overall, these survey results showed that the new recommendations from the JSH2014 are reflective of the daily clinical practice for hypertension management used by Japanese physicians.
The target BP values given were near the recommended values in the JSH2014. The recommended home BP values given were ∼5 mm Hg lower for 40% of the respondents and 10 mm Hg lower for 20% of the respondents compared with the recommended office BP values. On the other hand, ∼20% of the respondents recommended similar values to those given in the JSH2014 (140/90 mm Hg) as their suggested home BP values. A previous paper by Obara et al.4 presenting a survey of the awareness of the JSH guidelines showed that >40% of respondents suggested 135/85 mm Hg and another 40% recommended a value of <135/85 mm Hg, but ∼15% suggested a value of >135/85 mm Hg, for their recommended home BP values. The survey respondents of this paper were physicians who had attended educational seminars on hypertension that were presented throughout Japan during the months after the publication of the JSH2009. Considering this, there may be biases related to the differences in respondents who participated in these surveys.
Despite there being no benefit of intensive BP decrease on cardiovascular outcomes in diabetic subjects, according to clinical studies like the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial and so on,5, 6 Japanese physicians still select the low target BP for patients with diabetes or kidney disease of 130/80 mm Hg, even in elderly patients. This practice is performed in order to avoid stroke events7 that are more frequent in Asians compared with Caucasians. Previous survey results by Obara et al.4 had similar findings. The reason why more physicians select a systolic BP of <130 mm Hg (40% of respondents) and a diastolic BP of <80 mm Hg (36% of respondents) for patients with chronic-phase stroke can be explained by this concern.
The target BP for patients with chronic-phase stroke was 140/90 mm Hg for ∼45% of respondents, and <140/90 for another ∼45% of respondents. Based on stroke subtypes, the target BP may vary. According to survey respondents, BP should be reduced in patients with lacunar infarcts or antithrombotic therapy, and should not be reduced as much in patients with stenotic lesions of major cerebral arteries. BP levels should be managed based on the patient’s background.
The most common combination of antihypertensive drugs that physicians stated they prescribed was ‘a RAS blocker and a CCB’, especially ‘an ARB and a CCB’. ‘A RAS blocker and diuretic’ was stated with about one-fourth the frequency as ‘a RAS blocker and a CCB’. Physicians are more familiar with using a CCB compared with a diuretic. This result also confirms that ARBs are more commonly used and more popular renin–angiotensin system (RAS) blockade drugs than ACE inhibitors. Furthermore, β-blockers are rarely used as a second drug for hypertensive patients.
Recently, the main results of the Systolic Blood Pressure Intervention Trial (SPRINT) have been published and have the major impact of presenting the merits of a target systolic blood pressure of <120 mm Hg in patients who are at a high risk for cardiovascular events but do not have diabetes.8 Although the idea of ‘the lower the better’ with regard to BP should continue to be discussed, awareness of BP management and the survey results may change this theory in the near future.
The survey has some limitations. First, the survey respondents were people who wanted to know the guidelines for hypertension management, rather than physicians in general. Moreover, most respondents, ∼80%, were men. Second, the methodology of this survey requires consideration. This was a web-based survey; therefore, respondents only included people who have access to the internet. In addition, respondents selected systolic BP and diastolic BP independently; therefore, we could not determine correlations between the systolic BP and diastolic BP values that one respondent selected as recommended values and BP targets. Furthermore, because simple software was used for the survey, we could not analyze each trait of the responding physicians, such as type of practice, specialty and age. In addition, the study period was limited to the first 6 months after the publication of the JSH2014. Many physicians already knew the new recommendations of and modifications to the JSH2014 from other reviews, conferences or advertisements. A follow-up survey may be necessary in the future.
In conclusion, this survey demonstrated that most Japanese physicians are aware of the JSH guidelines and treat hypertensive patients with an approach similar to the recommendations in the guidelines, modified based on their own clinical experience. Some physicians stated in the survey that they vary several target BP values according to their understanding of their patients; however, overall, most physicians try to achieve the recommendation values or lower for the target BPs in the JSH guidelines. Continuous assessment of the awareness and use of the hypertension guidelines should be performed.
References
Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ishimitsu T, Ito M, Ito S, Itoh H, Iwao H, Kai H, Kario K, Kashihara N, Kawano Y, Kim-Mitsuyama S, Kimura G, Kohara K, Komuro I, Kumagai H, Matsuura H, Miura K, Morishita R, Naruse M, Node K, Ohya Y, Rakugi H, Saito I, Saitoh S, Shimada K, Shimosawa T, Suzuki H, Tamura K, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Umemura S . The Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2014). Hypertens Res 2014; 37: 253–390.
Obara T, Ohkubo T, Fukunaga H, Kobayashi M, Satoh M, Metoki H, Asayama K, Inoue R, Kikuya M, Mano N, Miyakawa M, Imai Y . Practice and awareness of physicians regarding home blood pressure measurement in Japan. Hypertens Res 2010; 33: 428–434.
Lindholm LH, Carlberg B, Samuelsson O . Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet 2005; 366: 1545–1553.
Obara T, Ubeda SR, Ohkubo T, Matsuura H, Ishimitsu T, Takata M, Rakugi H, Imai Y . Awareness of the Japanese Society of Hypertension guidelines for the management of hypertension and their use in clinical practices: 2009 survey results. Hypertens Res 2015; 38: 400–404.
Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F . Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010; 362: 1575–1585.
Bangalore S, Kumar S, Lobach I, Messerli FH . Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation 2011; 123: 2799–2810.
McBrien K, Rabi DM, Campbell N, Barnieh L, Clement F, Hemmelgarn BR, Tonelli M, Leiter LA, Klarenbach SW, Manns BJ . Intensive and standard blood pressure targets in patients with type 2 diabetes mellitus: systematic review and meta-analysis. Arch Intern Med 2012; 172: 1296–1303.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015; 373: 2103–2116.
Acknowledgements
This work was supported by directors, councilors and members of the Japanese Society of Hypertension.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mogi, M., Hasebe, N., Horiuchi, M. et al. The results of a survey of physicians about the Japanese Society of Hypertension Guidelines for the Management of Hypertension 2014 and its clinical use. Hypertens Res 39, 660–663 (2016). https://doi.org/10.1038/hr.2016.42
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.42
Keywords
This article is cited by
-
Management of Hypertension in the Asia-Pacific Region: A Structured Review
American Journal of Cardiovascular Drugs (2024)
-
Achievement rate of target blood pressure in patients with hypertension treated by hypertension specialists and non-specialists in a real-world setting
Hypertension Research (2023)
-
Strategies for improving the treatment and control of hypertension in Japan
Journal of Human Hypertension (2022)
-
Daily self-monitoring of blood pressure decreases systolic and diastolic blood pressure in hypertensive participants
Heart and Vessels (2022)
-
Prescription status of diuretics for essential hypertension in a Japanese population
Hypertension Research (2021)