Abstract
Proprotein convertase subtilisin/kexin type 9 (PCSK9), a novel target for low-density lipoprotein cholesterol (LDL-C)-lowering therapy, has been found to possess multiple off-target effects in humans. The aim of the present study was to investigate the association of blood pressure (BP) with plasma PCSK9 levels in a large Chinese cohort and the relation of PCSK9 level to carotid intima–media thickness (cIMT) in hypertensive patients. A total of 805 patients without lipid-lowering drug therapy were consecutively enrolled. First, the relationship between BP and PCSK9 was evaluated in hypertensives and normotensives. Furthermore, we examined the relation of PCSK9 to cIMT in 256 enrolled patients who had received a carotid ultrasound test. Plasma PCSK9 levels were measured by enzyme-linked immunosorbent assay, and cITM of left and right carotid arteries was assessed by B-mode ultrasound. There was no significant difference in PCSK9 levels between hypertensives and normotensives. PCSK9 level was not associated with systolic and diastolic BP and pulse pressure in hypertensives and normotensives regardless of sex. A positive correlation between PCSK9 and maximum-IMT and mean-MIT in hypertensives was found in univariate analyses, whereas such an association was absent in normotensives. In addition, the positive association of PCSK9 with cIMT disappeared in hypertensives in multivariate analyses. PCSK9 level is not associated with systolic or diastolic BP in hypertensives or normotensives, but it positively correlates with cIMT in hypertensives in univariate but not multivariate analyses, and further researches are needed.
Similar content being viewed by others
Introduction
Dyslipidemia and hypertension are not only the manifestations of metabolic syndrome,1 but also the well-established risk factors for coronary artery disease.2, 3, 4 During the past decade, increasing evidence from epidemiological observations and prospective clinical studies has indicated that elevated serum total cholesterol and low-density lipoprotein cholesterol (LDL-C) levels are associated with an increased risk of new onset of arterial hypertension.5, 6, 7, 8, 9, 10 On the other hand, it has been demonstrated that the reduction of serum cholesterol levels decreases blood pressure (BP).11
Proprotein convertase subtilisin/kexin type 9 (PCSK9), a secretory protease produced by the liver, is a major regulator of LDL-C by binding to hepatic LDL receptor and promoting their degradation, thereby leading to increased LDL-C concentrations.12, 13, 14 Recently, several large clinical trials have demonstrated that PCSK9 monoclonal antibody can significantly reduce LDL-C levels.15, 16, 17 In view of the association between LDL-C and the risk of new onset of hypertension or BP values, it seems reasonable to speculate that PCSK9 may affect the development of hypertension or BP control. Furthermore, it is important to address the issue because it may predict whether the promising PCSK9 inhibitors bring a potential effect on hypertension or BP control.
Actually, the association between PCSK9 and hypertension or BP remains controversial. In the Dallas Heart Study, a positive correlation was found between PCSK9 level and both systolic blood pressure (SBP) and diastolic blood pressure (DBP) in women but not in men.18 Cui et al.19 reported that PCSK9 was positively associated with SBP and DBP in both men and women. On the contrary, Berger et al.20 found that PCSK9 deficiency did not alter BP in mouse models of hypertension. Similarly, in a recent nested case–control study with healthy American women, Ridker et al.21 showed no association between PCSK9 and SBP and DBP. However, in most of previous studies, the enrolled participants were under lipid-lowering drugs including statins or the researchers did not declare whether lipid-lowering drugs were taken. The relationship between PCSK9 and BP could be influenced because lipid-lowering drugs including statins were demonstrated to play a role in BP and PCSK9 levels.22, 23 Furthermore, little information is currently available for the relationship between PCSK9 and BP in patients with hypertension to date. In addition, hypertension is considered as the major determinant of carotid artery intima–media thickness (cIMT) as an index of carotid atherosclerosis as well as artery stiffness,24, 25, 26, 27, 28 whereas the level of cIMT is higher in normotensive offspring of hypertensive parents compared with those of normotensive parents.29 Previous study showed a positive association of PCSK9 levels with cIMT in hypertensive patients, but in the study statins were taken.30
Hence, in the present study we aimed to detect the association between PCSK9 level and BP and IMT in patients without or with hypertension without lipid-lowering drug therapy.
Methods
Study population
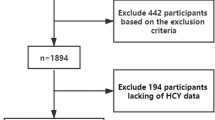
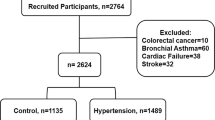
In the present study, consecutive patients hospitalized in our center were screened between October 2012 and October 2014 for the following inclusion criteria: not treated with lipid-lowering agents (statins, fibrates, nicotinic acid, ezitimibe and omega 3) for at least 3 months before the study and over the age of 18 years. Exclusion criteria were the existence of any infectious or systematic inflammatory diseases, significant hematologic disorders, thyroid dysfunction, severe liver and/or renal insufficiency and malignant tumors. According to the inclusion and exclusion criteria, a total of 805 patients were enrolled eligibly. Of these participants, 481 hypertensives and 324 normotensives were included, and the data of 256 patients for IMT were available. There were no significant differences in clinical characteristics between 256 participants who were enrolled in cIMT study and 549 participants who were not. The definition of hypertension was repeated SBP and/or DBP ⩾140 and/or ⩾90 mm Hg on at least two different occasions or currently using anti-hypertension drugs.31, 32 Coronary artery disease was diagnosed as the presence of coronary lesions ⩾50% at least one major epicardial artery segment assessed by at least two independent senior interventional cardiologists. Diabetes mellitus was defined as fasting glucose levels ⩾7.0 mmol l−1 in multiple determinations and/or was receiving at least one glucose-lowing treatment. The study was approved by the hospital ethical review board (Fuwai Hospital & National Center for Cardiovascular Diseases, Beijing, China), and all patients gave their written informed consent.
Biochemical determinations
Fasting blood samples were collected from all enrolled patients after hospitalization. The blood samples for the measurement of PCSK9 levels were stored at −80 °C until analysis. The concentrations of plasma triglyceride, total cholesterol, high-density lipoprotein cholesterol, LDL-C, apolipoprotein B, apolipoprotein A-I and fasting glucose were measured by automatic biochemistry analyzer (Hitachi 7150, Tokyo, Japan). Hemoglobin A1c was examined using Tosoh Automated Glycohemoglobin Analyzer (HLC-723G8, Tokyo, Japan). PCSK9 levels in plasma were assayed using a high-sensitivity, quantitative sandwich enzyme immunoassay (Quantikine ELISA, R&D Systems Europe Ltd, Sweden) as described in our previous studies.33, 34 The minimum detectable dose of PCSK9 was 0.096 ng ml−1.
Carotid ultrasonography assessment
Carotid ultrasound was evaluated as described previously.35, 36 Briefly, ultrasonic examinations of left and right carotid arteries were performed by two trained ultrasonographers who were blinded to participants’ clinical characteristics using 128 System (Acuson, Mountain View, CA, USA) with a high-resolution 7.5–10.0 MHz transducer. IMT was measured at the far wall of three 10-mm segments of bilateral carotid artery: the proximal common carotid artery, the distal common carotid artery and the bifurcation. The largest IMT value was determined as the maximum IMT (max-IMT) and the average value of measured IMT as the mean IMT (mean-IMT). The average of right and left values was recorded as the individual representative value. The mean difference of IMT between two ultrasonographers was 0.036 mm.
Statistical analysis
Continuous variables are expressed as mean±s.d. or median (interquartile range) and categorical variables as frequencies (percentage). Mann–Whitney test was applied for comparison of clinical parameters between the groups of patients with or without hypertension. The categorical variables were compared using the χ2 test. The associations of PCSK9 with SBP, DBP, pulse pressure (PP), mean-IMT, max-IMT and other parameters were analyzed using Spearman’s rank correlation and multiple linear regression. Two-sided P-values were considered statistically significant. Statistical analysis was performed with SPSS version 19.0 software (SPSS, Chicago, IL, USA).
Results
Clinical and biochemical characteristics of patients with or without hypertension
The baseline characteristics of the cohort of 805 participants are shown in Table 1. There were higher values for age and body mass index as well as higher percentages of coronary artery disease and diabetes in hypertensives than in normotensives (P<0.01). The levels of SBP, DBP and PP were higher in hypertensives than in normotensives, and higher levels of SBP and PP but lower levels of DBP in hypertensives were found in females than in males (P<0.01 or 0.05). Compared with men, women in hypertensives or normotensives had higher levels of total cholesterol, high-density lipoprotein, LDL-C and apolipoprotein A-I (P<0.01 or 0.05). In additionally, higher levels of total cholesterol, TG and LDL-C in women were found in normotensives than in hypertensives (P<0.01 or 0.05), and it was likely because of current smoking status, the percentages of diabetes and coronary artery disease, hormone level, the usage of β-receptor blockers or dietary habits.37, 38, 39, 40 PCSK9 level was found higher in women than in men in patients with or without hypertension, consistent with previous studies,18, 19 but no significant difference in PCSK9 level was found between hypertensives and normotensives. Of the 256 patients for the study of the association between PCSK9 and IMT, the baseline clinical and biochemical characteristics are summarized in Supplementary Table 1.
Associations of plasma PCSK9 level with metabolism factors and BP
As shown in Table 2, a significant but weak positive correlation of PCSK9 level with age was found in hypertensives (r=0.099, P=0.029) but not in normotensives. PCSK9 level was not associated with TG and body mass index in both hypertensives and normotensives, consistent with previous studies41, 42, 43 but contrary to some studies.18, 44 On the other hand, PCSK9 level was positively associated with LDL-C, apolipoprotein B, apolipoprotein A-I and hemoglobin A1c in both groups but high-density lipoprotein cholesterol in normotensives. No correlation between PCSK9 and SBP and DBP was found in all enrolled population, hypertensives or normotensives, whereas the level of PCSK9 exhibited a negative association with PP in normotensives. Meanwhile, we assessed the association between PCSK9 and BP according to sex in hypertensives and normotensives. However, there was still a lack of a correlation between plasma PCSK9 level and SBP and DBP in both hypertensives and normotensives regardless of sex (Figures 1 and 2). In addition, there was a significant correlation of PCSK9 with PP only in female normotensives (Figure 2).
Correlation of PCSK9 levels with cIMT
In the cohort of 256 participants, PCSK9 levels were positively associated with mean-cIMT (r=0.206, P=0.020) and max-cIMT (r=0.186, P=0.036) in hypertensives but not in all enrolled population and normotensives (Figure 3). However, this positive association was not found after adjusting for age, sex and body mass index (Table 3). Similarly, PCSK9 level was found to be positively associated with mean-cIMT (r=0.297, P=0.011) and max-cIMT (r=0.288, P=0.013) in male hypertensives but not in female hypertensives, whereas such positive associations were absent after adjusting for age (P>0.05). In addition, we examined the link of PCSK9 with cIMT under different status of BP control in hypertensives. Under the status of controlled BP (SBP <140 mm Hg and DBP <90 mm Hg), PCSK9 levels showed a positive correlation with max-cIMT, whereas there was a tendency for a positive association between PCSK9 and mean-cIMT (Supplementary Table 2). Nevertheless, such a positive association disappeared after adjusting for age (β=0.034, P=0.152). Under the status of uncontrolled BP (SBP ⩾140 mm Hg or DBP⩾90 mm Hg), there was no relation of PCSK9 to mean- or max-cIMT (Supplementary Table 2).
Discussion
In the present study, we found that plasma PCSK9 levels were not associated with SBP, DBP and PP in patients with or without hypertension. Besides, we also found that PCSK9 level was not associated independently with cIMT in hypertensives. To our knowledge, this is the first study to investigate the relationship between PCSK9 level and BP and cIMT in hypertensive and normotensive patients who were not under lipid-lowering drugs.
Our results are inconsistent with previous epidemiological studies concerning the relationship between PCSK9 levels and BP. For instance, in Dallas Heart Study, Lakoski et al.18 reported that PCSK9 levels were positively associated with SBP and DBP in women but not in men in both African Americans and European Americans. In parallel, Cui et al.19 showed a positive association of PCSK9 with SBP and DBP in both men and women in Han Chinese population by univariate analysis, but in a multiple regression analysis the positive correlations of PCSK9 with SBP in women and DBP in men were not found. In those studies, healthy participants were enrolled, whereas in the present study we investigated the relationship between PCSK9 levels and BP in hypertensives. In our study we found no association of PCSK9 with SBP, DBP and PP in patients with or without hypertension. Furthermore, the similar results were found in sex subgroup except the negative association between PCSK9 and PP in normotensive women. Moreover, Cariou et al.45 reported that a positive correlation of PCSK9 concentrations with SBP but not DBP was found in diabetic patients by univariate analysis, but the correlation was absent in a multiple regression analysis.
On the other hand, our finding is in agreement with some studies. A recent study with a large cohort of >28 000 initially healthy American women did not exhibit an association between PCSK9 levels and SBP and DBP.21 Previous in vitro study showed that PCSK9 downregulated epithelial Na+ absorption by reducing the epithelial Na+ channel expression, and the researchers speculated that PCSK9 could contribute to BP control and a decrease in PCSK9 level would raise the risk of hypertension.46 However, Berger et al.20 found that PCSK9 deficiency did not alter BP and sodium homeostasis in mouse models of hypertension, supporting our finding. Furthermore, several clinical trials concerning anti-PCSK9 monoclonal antibodies have not shown available date on BP and no adverse events linked to hypertension have been reported.47, 48, 49 Our previous studies also indicated no association of PCSK9 level with BP in patients with coronary artery disease.50, 51, 52. In addition, clinical rare patients with undetectable PCSK9 level did not exhibit an influence on BP.53, 54, 55
Previous gene studies of PCSK9 revealed that hypertension was less common in the carriers of PCSK9 (Y142X, C679X) compared with noncarriers.56 Moreover, the interaction of PCSK9 AG genotype and cigarette smoking decreased SBP, whereas the interaction of PCSK9 AA genotypes and cigarette smoking increased DBP levels in Chinese Minority of Zhuang.57 In our study, we found no difference in the association of PCSK9 with SBP and DBP under different smoking status (data not shown), in accordance with previous study.21 We speculated that the difference could have resulted from different gene styles of PCSK9 from different study populations.58
Hypertension is demonstrated as the key determinant of cIMT.24 Hence, in our study we also investigated the association between PCSK9 level and cIMT. We found that PCSK9 levels were positively associated with both mean-cIMT and max-cIMT in hypertensives but not in normotensives, in accordance with previous study by Lee et al. Nevertheless, to be inconsistent with the results of Lee et al.,30 we found that these positive associations were absent after adjusting some risk factors of cardiovascular disease such as age and sex, which is supported by the recent study from Zhu et al.59 Zhu et al. reported that PCSK9 level was related to cIMT (β=0.073, P=0.005) but it was not an independent predictor of cIMT in backward multiple regression models in the cohort consisting of 1527 middle-aged men who were free of vascular diseases. Nevertheless, in the cohort from Zhu et al.,59 26% of the participants were patients with hypertension and 8% were on statin therapy. In the present study, we found that PCSK9 level was positively associated with cIMT in hypertensives but such a positive association was absent after adjusting for age. To be different from the study by Lee et al.,30 the participants in our study were not treated by lipid-lowering drugs that can increase PCSK9 level22. Moreover, the hypertensives were younger in our study compared with those in the study by Lee et al.,30 whereas cIMT is associated with age.60 All these could account for the difference in results. Furthermore, the significantly positive association between PCSK9 and cIMT was found in male hypertensives, whereas in female hypertensives there was a positive tendency for the association of PCSK9 with IMT that may result from the smaller sample of females. Interestingly, the positive association between PCSK9 and cIMT in male hypertensives was absent after adjusting for age. Similarly, the positive association between PCSK9 and cIMT in hypertensive patients with controlled BP disappeared after adjusting for age. In addition, previous study showed that mean-IMT was reduced in PCSK9 loss-of-function variant carriers when compared with noncarriers,56 supporting our finding. In view of the positive association of PCSK9 with cIMT, we speculate that PCSK9 inhibitor could reduce carotid artery atherosclerosis. Thus, our finding is partly inconsistent with the study by Lee et al.30 but is supported by Zhu et al.59 However, further study is required to clarify this issue, and whether PCSK9 inhibitors reduce cIMT also needs further research.
Despite negative results concerning the relationship between PCSK9 levels and BP, our finding deserves interest. As serum LDL-C levels are demonstrated to be associated with hypertension and BP values, the promising lipid-lowering drug PCSK9 inhibitor could play some role in BP or onset of hypertension. Thus, it is vital to address the issue. Although some studies have been performed, the relationship between PCSK9 and BP is not well established. Our finding supports the viewpoint that PCSK9 could not affect BP. Of course, the possibility could not be excluded that the PCSK9 activity may be more relevant than its level in determining the BP values as well as LDL-C level, and it requires further study. However, the ongoing large-scale studies about PCSK9 inhibitors will help to clarify this issue.
Our study has several limitations. First, the association between PCSK9 level and one-time levels of SBP or DBP was investigated, but BP values are easy to fluctuate and we did not show the relationship between mean BP values over a period of time and PCSK9 level because of the lack of concerning data. Second, although our data did not show an association between PCSK9 levels and BP values, we did not exclude a possibility that PCSK9 activity may be more relevant than its level in determining the BP values. Finally, our study sample is relatively small.
Conclusion
Our data showed that PCSK9 levels are not associated with BP in hypertensives or normotensives, suggesting that the ongoing development of PCSK9 inhibitors could have no effect on BP. In addition, our results exhibited a positive association between PCSK9 and cIMT in univariate but not multivariate analyses. Thus, whether a decrease in PCSK9 level or PCSK9 inhibitors could reduce carotid atherosclerosis in patients with hypertension requires further researches.
References
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Costa F, American Heart Association National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735–2752.
Wilson PW . Established risk factors and coronary artery disease: the Framingham Study. Am J Hypertens 1994; 7 (7 Pt 2): 7s–12s.
Kannel WB . Cardioprotection and antihypertensive therapy: the key importance of addressing the associated coronary risk factors (the Framingham experience). Am J Cardiol 1996; 77: 6b–11b.
Austin MA, Hokanson JE, Edwards KL . Hypertriglyceridemia as a cardiovascular risk factor. Am J Cardiol 1998; 81: 7b–12b.
Sesso HD, Buring JE, Chown MJ, Ridker PM, Gaziano JM . A prospective study of plasma lipid levels and hypertension in women. Arch Intern Med 2005; 165: 2420–2427.
Cicero AF, Rosticci M, Baronio C, Morbini M, Parini A, Grandi E, D'Addato S, Borghi C, Brisighella Heart Study Group. Serum LDL cholesterol levels and new onset of arterial hypertension: an 8-year follow-up. Eur J Clin Invest 2014; 44: 926–932.
Borghi C, Cicero AF, Saragoni S, Buda S, Cristofori C, Lilli P, Degli Esposti L . Rate of control of LDL cholesterol and incident hypertension requiring antihypertensive treatment in hypercholesterolemic subjects in daily clinical practice. Ann Med 2014; 46: 97–102.
Laaksonen DE, Niskanen L, Nyyssonen K, Lakka TA, Laukkanen JA, Salonen JT . Dyslipidaemia as a predictor of hypertension in middle-aged men. Eur Heart J 2008; 29: 2561–2568.
Halperin RO, Sesso HD, Ma J, Buring JE, Stampfer MJ, Gaziano JM . Dyslipidemia and the risk of incident hypertension in men. Hypertension 2006; 47: 45–50.
Paynter NP, Sesso HD, Conen D, Otvos JD, Mora S . Lipoprotein subclass abnormalities and incident hypertension in initially healthy women. Clin Chem 2011; 57: 1178–1187.
Strazzullo P, Kerry SM, Barbato A, Versiero M, D'Elia L, Cappuccio FP . Do statins reduce blood pressure?: a meta-analysis of randomized, controlled trials. Hypertension 2007; 49: 792–798.
Urban D, Poss J, Bohm M, Laufs U . Targeting the proprotein convertase subtilisin/kexin type 9 for the treatment of dyslipidemia and atherosclerosis. J Am Coll Cardiol 2013; 62: 1401–1408.
Lagace TA . PCSK9 and LDLR degradation: regulatory mechanisms in circulation and in cells. Curr Opin Lipidol 2014; 25: 387–393.
Seidah NG, Awan Z, Chretien M, Mbikay M . PCSK9: a key modulator of cardiovascular health. Circ Res 2014; 114: 1022–1036.
Cunningham D, Danley DE, Geoghegan KF, Griffor MC, Hawkins JL, Subashi TA, Varghese AH, Ammirati MJ, Culp JS, Hoth LR, Mansour MN, McGrath KM, Seddon AP, Shenolikar S, Stutzman-Engwall KJ, Warren LC, Xia D, Qiu X . Structural and biophysical studies of PCSK9 and its mutants linked to familial hypercholesterolemia. Nat Struct Mol Biol 2007; 14: 413–419.
Cariou B, Le May C, Costet P . Clinical aspects of PCSK9. Atherosclerosis 2011; 216: 258–265.
Alborn WE, Cao G, Careskey HE, Qian YW, Subramaniam DR, Davies J, Conner EM, Konrad RJ . Serum proprotein convertase subtilisin kexin type 9 is correlated directly with serum LDL cholesterol. Clin Chem 2007; 53: 1814–1819.
Lakoski SG, Lagace TA, Cohen JC, Horton JD, Hobbs HH . Genetic and metabolic determinants of plasma PCSK9 levels. J Clin Endocrinol Metab 2009; 94: 2537–2543.
Cui Q, Ju X, Yang T, Zhang M, Tang W, Chen Q, Hu Y, Haas JV, Troutt JS, Pickard RT, Darling R, Konrad RJ, Zhou H, Cao G . Serum PCSK9 is associated with multiple metabolic factors in a large Han Chinese population. Atherosclerosis 2010; 213: 632–636.
Berger JM, Vaillant N, Le May C, Calderon C, Bregeon J, Prieur X, Hadchouel J, Loirand G, Cariou B . PCSK9-deficiency does not alter blood pressure and sodium balance in mouse models of hypertension. Atherosclerosis 2015; 239: 252–259.
Ridker PM, Rifai N, Bradwin G, Rose L . Plasma proprotein convertase subtilisin/kexin type 9 levels and the risk of first cardiovascular events. Eur Heart J 2016; 37: 554–560.
Sahebkar A, Simental-Mendia LE, Guerrero-Romero F, Golledge J, Watts GF . Effect of statin therapy on plasma proprotein convertase subtilisin kexin 9 (PCSK9) concentrations: a systematic review and meta-analysis of clinical trials. Diabetes Obes Metab 2015; 17: 1042–1055.
Lambert G, Ancellin N, Charlton F, Comas D, Pilot J, Keech A, Patel S, Sullivan DR, Cohn JS, Rye KA, Barter PJ . Plasma PCSK9 concentrations correlate with LDL and total cholesterol in diabetic patients and are decreased by fenofibrate treatment. Clin Chem 2008; 54: 1038–1045.
Su TC, Jeng JS, Chien KL, Sung FC, Hsu HC, Lee YT . Hypertension status is the major determinant of carotid atherosclerosis: a community-based study in Taiwan. Stroke 2001; 32: 2265–2271.
Xie W, Liu J, Wang W, Wang M, Li Y, Sun J, Liu J, Qi Y, Zhao F, Zhao D . Five-year change in systolic blood pressure is independently associated with carotid atherosclerosis progression: a population-based cohort study. Hypertens Res 2014; 37: 960–965.
Ring M, Eriksson MJ, Zierath JR, Caidahl K . Arterial stiffness estimation in healthy subjects: a validation of oscillometric (Arteriograph) and tonometric (SphygmoCor) techniques. Hypertens Res 2014; 37: 999–1007.
Seidlerova J, Filipovsky J, Mayer O, Wohlfahrt P, Cifkova R . Positive effects of antihypertensive treatment on aortic stiffness in the general population. Hypertens Res 2014; 37: 64–68.
Otsuka K, Fukuda S, Shimada K, Suzuki K, Nakanishi K, Yoshiyama M, Yoshikawa J . Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res 2014; 37: 1014–1020.
Yildirim A, Kosger P, Ozdemir G, Sahin FM, Ucar B, Kilic Z . Carotid intima-media thickness and elastic properties of aortas in normotensive children of hypertensive parents. Hypertens Res 2015; 38: 621–626.
Lee CJ, Lee YH, Park SW, Kim KJ, Park S, Youn JC, Lee SH, Kang SM, Jang Y . Association of serum proprotein convertase subtilisin/kexin type 9 with carotid intima media thickness in hypertensive subjects. Metabolism 2013; 62: 845–850.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Liu LS . [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011; 39: 579–615.
Zhang Y, Zhu C-G, Xu R-X, Li S, Guo Y-L, Sun J, Li J-J . Relation of circulating PCSK9 concentration to fibrinogen in patients with stable coronary artery disease. J Clin Lipidol 2014; 8: 494–500.
Li S, Zhang Y, Xu R-X, Guo Y-L, Zhu C-G, Wu N-Q, Qing P, Liu G, Dong Q, Li J-J . Proprotein convertase subtilisin-kexin type 9 as a biomarker for the severity of coronary artery disease. Ann Med 2015; 47: 386–393.
Liang L-R, Wong ND, Shi P, Zhao L-C, Wu L-X, Xie G-Q, Wu Y-F . Cross-sectional and longitudinal association of cigarette smoking with carotid atherosclerosis in Chinese adults. Prev Med 2009; 49: 62–67.
Xie W, Liang L, Zhao L, Shi P, Yang Y, Xie G, Huo Y, Wu Y . Combination of carotid intima-media thickness and plaque for better predicting risk of ischaemic cardiovascular events. Heart 2011; 97: 1326–1331.
Wu L, Parhofer KG . Diabetic dyslipidemia. Metabolism 2014; 63: 1469–1479.
Fonseca VA . Effects of β-blockers on glucose and lipid metabolism. Curr Med Res Opin 2010; 26: 615–629.
Van Horn L, McCoin M, Kris-Etherton PM, Burke F, Carson JA, Champagne CM, Karmally W, Sikand G . The evidence for dietary prevention and treatment of cardiovascular disease. J Am Diet Assoc 2008; 108: 287–331.
Wegge JK, Roberts CK, Ngo TH, Barnard RJ . Effect of diet and exercise intervention on inflammatory and adhesion molecules in postmenopausal women on hormone replacement therapy and at risk for coronary artery disease. Metabolism 2004; 53: 377–381.
Mayne J, Raymond A, Chaplin A, Cousins M, Kaefer N, Gyamera-Acheampong C, Seidah NG, Mbikay M, Chretien M, Ooi TC . Plasma PCSK9 levels correlate with cholesterol in men but not in women. Biochem Biophys Res Commun 2007; 361: 451–456.
Cariou B, Langhi C, Le Bras M, Bortolotti M, Le KA, Theytaz F, Le May C, Guyomarc'h-Delasalle B, Zair Y, Kreis R, Boesch C, Krempf M, Tappy L, Costet P . Plasma PCSK9 concentrations during an oral fat load and after short term high-fat, high-fat high-protein and high-fructose diets. Nutr Metab (Lond) 2013; 10: 4.
Cariou B, Le Bras M, Langhi C, Le May C, Guyomarc’h-Delasalle B, Krempf M, Costet P . Association between plasma PCSK9 and gamma-glutamyl transferase levels in diabetic patients. Atherosclerosis 2010; 211: 700–702.
Brouwers MCGJ, Troutt JS, van Greevenbroek MMJ, Ferreira I, Feskens EJ, van der Kallen CJH, Schaper NC, Schalkwijk CG, Konrad RJ, Stehouwer CDA . Plasma proprotein convertase subtilisin kexin type 9 is not altered in subjects with impaired glucose metabolism and type 2 diabetes mellitus, but its relationship with non-HDL cholesterol and apolipoprotein B may be modified by type 2 diabetes mellitus: The CODAM study. Atherosclerosis 2011; 217: 263–267.
Cariou B, Le Bras M, Langhi C, Le May C, Guyomarc'h-Delasalle B, Krempf M, Costet P . Association between plasma PCSK9 and gamma-glutamyl transferase levels in diabetic patients. Atherosclerosis 2010; 211: 700–702.
Sharotri V, Collier DM, Olson DR, Zhou R, Snyder PM . Regulation of epithelial sodium channel trafficking by proprotein convertase subtilisin/kexin type 9 (PCSK9). J Biol Chem 2012; 287: 19266–19274.
Blom DJ, Hala T, Bolognese M, Lillestol MJ, Toth PD, Burgess L, Ceska R, Roth E, Koren MJ, Ballantyne CM, Monsalvo ML, Tsirtsonis K, Kim JB, Scott R, Wasserman SM, Stein EA, DESCARTES Investigators. A 52-week placebo-controlled trial of evolocumab in hyperlipidemia. N Engl J Med 2014; 370: 1809–1819.
Desai NR, Kohli P, Giugliano RP, O'Donoghue ML, Somaratne R, Zhou J, Hoffman EB, Huang F, Rogers WJ, Wasserman SM, Scott R, Sabatine MS . AMG145, a monoclonal antibody against proprotein convertase subtilisin kexin type 9, significantly reduces lipoprotein(a) in hypercholesterolemic patients receiving statin therapy: an analysis from the LDL-C Assessment with Proprotein Convertase Subtilisin Kexin Type 9 Monoclonal Antibody Inhibition Combined with Statin Therapy (LAPLACE)-Thrombolysis in Myocardial Infarction (TIMI) 57 Trial. Circulation 2013; 128: 962–969.
Urban D, Pöss J, Böhm M, Laufs U . Targeting the proprotein convertase subtilisin/kexin type 9 for the treatment of dyslipidemia and atherosclerosis. J Am Coll Cardiol 2013; 62: 1401–1408.
Zhang Y, Zhu CG, Xu RX, Li S, Guo YL, Sun J, Li JJ . Relation of circulating PCSK9 concentration to fibrinogen in patients with stable coronary artery disease. J Clin Lipidol 2014; 8: 494–500.
Xu RX, Li S, Zhang Y, Li XL, Guo YL, Zhu CG, Li JJ . Relation of plasma PCSK9 levels to lipoprotein subfractions in patients with stable coronary artery disease. Lipids Health Dis 2014; 13: 188.
Li S, Guo Y-L, Xu R-X, Zhang Y, Zhu C-G, Sun J, Qing P, Wu N-Q, Jiang L-X, Li J-J . Association of plasma PCSK9 levels with white blood cell count and its subsets in patients with stable coronary artery disease. Atherosclerosis 2014; 234: 441–445.
Zhao Z, Tuakli-Wosornu Y, Lagace TA, Kinch L, Grishin NV, Horton JD, Cohen JC, Hobbs HH . Molecular characterization of loss-of-function mutations in PCSK9 and identification of a compound heterozygote. Am J Hum Genet 2006; 79: 514–523.
Hooper AJ, Marais AD, Tanyanyiwa DM, Burnett JR . The C679X mutation in PCSK9 is present and lowers blood cholesterol in a Southern African population. Atherosclerosis 2007; 193: 445–448.
Cariou B, Ouguerram K, Zair Y, Guerois R, Langhi C, Kourimate S, Benoit I, Le May C, Gayet C, Belabbas K, Dufernez F, Chetiveaux M, Tarugi P, Krempf M, Benlian P, Costet P . PCSK9 dominant negative mutant results in increased LDL catabolic rate and familial hypobetalipoproteinemia. Arterioscler Thromb Vasc Biol 2009; 29: 2191–2197.
Cohen JC, Boerwinkle E, Mosley TH Jr, Hobbs HH . Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N Engl J Med 2006; 354: 1264–1272.
Yin RX, Wu DF, Wu JZ, Cao XL, Aung LH, Miao L, Long XJ, Liu WY, Zhang L, Li M . Interactions of several lipid-related gene polymorphisms and cigarette smoking on blood pressure levels. Int J Biol Sci 2012; 8: 685–696.
Tran NT, Aslibekyan S, Tiwari HK, Zhi D, Sung YJ, Hunt SC, Rao DC, Broeckel U, Judd SE, Muntner P, Kent ST, Arnett DK, Irvin MR . PCSK9 variation and association with blood pressure in African Americans: preliminary findings from the HyperGEN and REGARDS studies. Front Genet 2015; 6: 136.
Zhu YM, Anderson TJ, Sikdar K, Fung M, McQueen MJ, Lonn EM, Verma S . Association of proprotein convertase subtilisin/kexin type 9 (PCSK9) with cardiovascular risk in primary prevention. Arterioscler Thromb Vasc Biol 2015; 35: 2254–2259.
Zureik M, Ducimetiere P, Touboul PJ, Courbon D, Bonithon-Kopp C, Berr C, Magne C . Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: longitudinal results from the Aging Vascular Study (EVA) study. Arterioscler Thromb Vasc Biol 2000; 20: 1622–1629.
Acknowledgements
This work was partially supported by the National Natural Science Foundation of China (81070171, 81241121), the Specialized Research Fund for the Doctoral Program of Higher Education of China (20111106110013), the Capital Special Foundation of Clinical Application Research (Z121107001012015), the Capital Health Development Fund (2011400302), and the Beijing Natural Science Foundation (7131014) awarded to Dr Jian-Jun Li.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Yang, SH., Du, Y., Li, S. et al. Plasma PCSK9 level is unrelated to blood pressure and not associated independently with carotid intima–media thickness in hypertensives. Hypertens Res 39, 598–605 (2016). https://doi.org/10.1038/hr.2016.38
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.38
Keywords
This article is cited by
-
From Endothelium to Lipids, Through microRNAs and PCSK9: A Fascinating Travel Across Atherosclerosis
High Blood Pressure & Cardiovascular Prevention (2020)
-
Plasma PCSK9 levels are unrelated to arterial stiffness in a community-based, 4.8-year prospective study
Journal of Human Hypertension (2017)