Abstract
Home blood pressure (HBP) measurements are known to be lower than conventional office blood pressure (OBP) measurements. However, this difference might not be consistent across the entire age range and has not been adequately investigated. We assessed the relationship between OBP and HBP with increasing age using the International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO). OBP, HBP and their difference were assessed across different decades of age. A total of 5689 untreated subjects aged 18–97 years, who had at least two OBP and HBP measurements, were included. Systolic OBP and HBP increased across older age categories (from 112 to 142 mm Hg and from 109 to 136 mm Hg, respectively), with OBP being higher than HBP by ∼7 mm Hg in subjects aged >30 years and lesser in younger subjects (P=0.001). Both diastolic OBP and HBP increased until the age of ∼50 years (from 71 to 79 mm Hg and from 66 to 76 mm Hg, respectively), with OBP being consistently higher than HBP and a trend toward a decreased OBP–HBP difference with aging (P<0.001). Determinants of a larger OBP–HBP difference were younger age, sustained hypertension, nonsmoking and negative cardiovascular disease history. These data suggest that in the general adult population, HBP is consistently lower than OBP across all the decades, but their difference might vary between age groups. Further research is needed to confirm these findings in younger and older subjects and in hypertensive individuals.
Similar content being viewed by others
Introduction
Several studies have shown that home blood pressure (HBP) measurements give lower values than conventional office blood pressure (OBP) measurements.1 Therefore, the current guidelines recommend higher blood pressure (BP) thresholds for defining hypertension based on office compared with home measurements.1, 2, 3
The current evidence on the difference between OBP and HBP measurements is based on studies that analyzed average BP values of samples including subjects of different ages.4, 5, 6 Whether the OBP–HBP difference is consistent across the entire age range is unclear. Some evidence suggests that the relationship of office with home or daytime ambulatory BP (dABP) differs with increasing age.4, 5, 6 This information has important implications for clinical practice where physicians classify patients into white-coat, masked and sustained hypertensives on the basis of office and out-of-office BP measurements.
This study assessed the relationship between OBP and HBP measurements in adults from the general population across each decade of age.
Methods
Population
The International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) has been constructed using population cohorts with individual subjects’ data, including OBP and HBP measurements and information on subsequent fatal and nonfatal cardiovascular outcomes. The protocols have been approved by scientific ethics committees, and participants provided written informed consent. The results have been published in peer-reviewed journals.7
At the time of writing this report, the IDHOCO data set included 7 prospective studies (n=8912) performed in Ohasama, Japan (n=2777),8 Finland (Finn-Home; n=2075),9 Tsurugaya, Japan (n=836),10 Didima, Greece (n=665),11 Montevideo, Uruguay (n=400),12 Buenos Aires, Argentina (n=426)13 and Dijon, France (n=1733).14 The Buenos Aires cohort13 (n=426) was excluded because it included referred patients rather than a population cohort. Moreover, 2516 subjects were excluded because they were on antihypertensive drugs (irrespective of the indication), 10 because of unknown antihypertensive treatment status, 270 because of inadequate OBP or HBP measurements and 1 because of unknown cardiovascular disease history (Figure 1).
BP measurements
Office
At least two baseline OBP measurements were required for inclusion. OBP was measured in a sitting8, 9, 11, 12, 14 or supine10 position, after 2 or 5 min of rest, using a standard mercury sphygmomanometer (2 studies)9, 11 or a validated automated arm device (4 studies)8, 10, 12, 14 with appropriate cuff size, and in a single visit (5 studies)8, 9, 10, 12, 14 or 2 visits (1 study).11 The averages of the first two readings of the first visit were analyzed.
Home
At least two baseline HBP measurements were required. HBP was measured after a 2–5-min sitting rest using validated electronic arm devices with appropriate cuff size, in the morning and evening (5 studies),8, 9, 11, 12, 14 or only in the morning (1 study).10 The median number of HBP readings ranged from 2 (Montevideo) to 51 (Ohasama). Five studies (93.7% of the participants) obtained a median of ⩾12 readings.8, 9, 10, 11, 14 All available HBP readings were averaged.
Additional information
Baseline information was recorded regarding the subjects’ age, gender, ethnicity, body mass index (BMI), smoking and drinking habits, diabetes mellitus (self-reported diagnosis, fasting or random blood glucose ⩾7.0 or ⩾11.1 mmol l−1, respectively, or antidiabetic drug use) and cardiovascular disease history (cardiac, cerebrovascular, peripheral arterial disease).
Hypertension phenotypes
Office hypertension was defined as systolic OBP ⩾140 and/or diastolic ⩾90 mm Hg and home hypertension as systolic HBP ⩾135 and/or diastolic ⩾85 mm Hg,2 normotension as low OBP and HBP (systolic and diastolic), white-coat hypertension as elevated OBP (systolic and/or diastolic) with low HBP (systolic and diastolic), masked hypertension as elevated HBP (systolic and/or diastolic) with low OBP (systolic and diastolic) and sustained hypertension as elevated OBP and HBP (systolic and/or diastolic).
Statistical analysis
The analysis was performed using baseline data only. Subjects were divided into 6 age subgroups (18–30, 30–40, 40–50, 50–60, 60–70 and ⩾70 years). Participants’ characteristics and BP values across different age subgroups were compared with one-way analysis of variance or Kruskal–Wallis test as appropriate and χ2 tests for categorical variables. OBP and HBP measurements of each age subgroup were compared using paired t-tests. An unpaired t-test was used to compare BP values and OBP–HBP differences per age subgroup between the sensitivity and main analyses. Linear multiple regression analysis was performed, with the center included as a random effect variable, to identify determinants of the OBP–HBP differences. Independent variables included gender, age, BMI, smoking, alcohol consumption, diabetes mellitus, cardiovascular disease history and sustained hypertension. The prevalence of white-coat, masked and sustained hypertension was compared among different age subgroups and separately by gender using χ2 tests. Multivariate logistic regression analyses were performed to identify independent determinants of white-coat, masked and sustained hypertension. Age, gender, BMI, smoking and alcohol use, diabetes and cardiovascular disease history were considered as independent variables, with the center included as a random effect variable. The results are presented as mean values±s.d., unless otherwise stated. The Statistical Package for Social Sciences software was used (IBM Corp. Released 2012, SPSS Statistics for Windows, Version 21.0. Armonk, NY, USA). A probability value P<0.05 was considered statistically significant.
Results
A total of 5689 untreated subjects were analyzed (2010 from Ohasama, Japan,8 1604 from Finland,9 476 from Tsurugaya, Japan,10 561 from Didima, Greece,11 356 from Montevideo, Uruguay12 and 682 from Dijon, France14) (Figure 1). The baseline characteristics differed across age groups (P⩽0.001), except for gender (Table 1). The age category of 18–30 years included only Caucasians. There was an increasing prevalence of diabetes mellitus and cardiovascular disease with increasing age. Current smoking, alcohol use and BMI showed a nonlinear relationship with age.
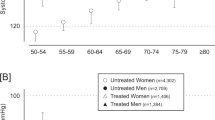
Systolic OBP and HBP progressively increased from the youngest to the oldest age category (from 112 to 142 mm Hg and from 109 to 136 mm Hg, respectively). Diastolic OBP and HBP also increased with age until 50–60 years (71–79 and 66–76 mm Hg, respectively; Figure 2 and Supplementary Table S1). The same analysis by gender showed a steeper systolic OBP and HBP increase in women (106–142 and 103–136 mm Hg, respectively) than in men (120–141 and 118–136 mm Hg, P<0.001). In both genders, diastolic OBP and HBP increased with age until 50–60 years and thereafter remained stable in women and slightly decreased in men (Supplementary Table S2 and Supplementary Figure S1).
Across all the age subgroups, OBP was consistently higher than HBP (P⩽0.001 for all systolic/diastolic comparisons within each subgroup). The age-dependent OBP–HBP differences are presented in Figure 2. The systolic OBP–HBP differences were similar in age subgroups >30 years (average 6.8±14.9 mm Hg) and smaller in younger subjects (2.9±11.5 mm Hg, P=0.001). The diastolic OBP–HBP difference was reduced from the youngest (5.2±8.3 mm Hg) to the oldest subgroup (1.2±9.5 mm Hg, P<0.001 for trend). Analyses by gender showed larger (P<0.001) systolic OBP–HBP differences in middle-aged (40–60 years) women (8.6±13.7 mm Hg) than men (6.5±13.4 mm Hg). The diastolic OBP–HBP differences showed a similar pattern with aging in both genders (Supplementary Table S2 and Supplementary Figure S2).
An additional analysis including only subjects with ⩾12 HBP readings (Supplementary Table S3) revealed similar OBP–HBP differences across the age subgroups in comparison with the main analysis (Supplementary Table S1), apart from a borderline 2 mm Hg higher systolic BP difference in the subgroup of participants aged 30–40 years (8.7±12.1 vs. 6.7±12.4 mm Hg, respectively; P=0.04). In addition, by repeating the analysis using mean HBP of the first 3 days only15 or morning HBP only, no remarkable differences from the main analysis were found (Supplementary Figures S3 and S4).
To evaluate the potential impact of supine vs. seated OBP measurements on the results, an additional analysis was conducted after excluding the Tsurugaya study that obtained supine measurements (n=476; all aged ⩾69 years; 8.4% of the sample size).10 The average OBP–HBP differences per age subgroup did not differ significantly from the corresponding BP differences of the main analysis (Supplementary Table S1), with the exception of a smaller diastolic OBP–HBP difference in the oldest subgroup (1.8±8.7 vs. 3.1±9.0 mm Hg, respectively; P<0.01).
The prevalence of white-coat hypertension increased until the fifth decade (from 4 to 15%, P<0.001) and thereafter remained relatively stable (Figure 3). Masked and sustained hypertension, although scarce in younger participants (0.6%), consistently increased with aging, with sustained hypertension displaying a steeper increase and being more common than masked hypertension in the older participants (36.4% vs. 13% in subjects ⩾70 years, respectively, P<0.001; Figure 3). Similar trends in hypertension phenotype prevalence across age categories were observed in both genders. However, in most age categories, masked and sustained hypertension were more common in men than in women (11.2% vs. 7.1%, P<0.0001 and 24.1% vs. 18.9%, P<0.0001, respectively; Supplementary Table S4 and Supplementary Figure S5). With regard to the prevalence of white-coat hypertension, there was a significant interaction between gender and age category (P=0.04). In subjects <50 years old, the prevalence of white-coat hypertension was higher in men than women (15.1% vs. 8.5%, P<0.001), with no such difference in older subjects.
Multivariable linear regression analyses adjusted for center were performed to identify determinants of the OBP–HBP difference (Table 2). Sustained hypertension appeared to increase the OBP–HBP difference (systolic/diastolic), whereas age, smoking and cardiovascular disease history diminished this difference. BMI was a significant negative predictor of the systolic OBP–HBP difference. All the covariates combined explained only 3% and 6% of the between-subject variability in the systolic and diastolic OBP–HBP difference, respectively.
In the multivariate logistic regression analyses exploring the determinants of hypertension phenotypes and adjusting for center, older age (odds ratio (OR) 1.04, 95% confidence interval (CI) 1.03–1.05; P<0.001) and higher BMI (OR 1.08, 95% CI 1.05–1.10; P<0.001) were found to increase the odds of white-coat hypertension (vs. normotensives), whereas female gender decreased these odds (0.70, 95% CI 0.58–0.86; P=0.001). For masked hypertension, older age (OR 1.07, 95% CI 1.06–1.09; P<0.001), higher BMI (1.18, 95% CI 1.15–1.22; P<0.001), smoking (1.75, 95% CI 1.31–2.32; P<0.001) and diabetes (1.57, 95% CI 1.07–2.31; P=0.022) were positive, but female gender was a negative (0.59, 95% CI 0.47–0.75; P<0.001) determinant (vs. normotensives). For sustained hypertension, older age (OR 1.09, 95% CI 1.08–1.10; P<0.001), higher BMI (1.21, 95% CI 1.18–1.24; P<0.001) and smoking (1.33, 95% CI 1.05–1.68; P=0.016) were found to increase, whereas the female gender was found to diminish (0.65, 95% CI 0.54–0.78; P<0.001), the probability of this phenotype (vs. normotensives).
Discussion
This analysis explored the relationship between OBP and HBP measurements with aging in 5689 untreated adults from population cohorts of the IDHOCO database. The main findings are as follows: (1) systolic OBP and HBP progressively increase with aging, with OBP being consistently higher than HBP by ∼7 mm Hg in subjects aged >30 years and lesser in younger subjects; (2) diastolic OBP and HBP also increased with aging until the fifth decade, with OBP being consistently higher than HBP and with a trend for this difference to decrease with aging; (3) women have lower OBP and HBP values than men until the fifth decade but display a steeper systolic OBP and HBP increase with age and larger systolic OBP–HBP differences in middle age than men; and (4) age, sustained hypertension, smoking and cardiovascular disease history are the main determinants of the OBP–HBP difference.
The age-dependent difference between office and out-of-office BP is an intriguing yet obscure issue in adults4, 5, 6 and children.16, 17 In line with the present findings, a meta-analysis of 7 population-based studies and 1 school-based study (n=4916) reported that OBP was consistently higher than HBP across all age groups.4 However, the systolic OBP–HBP difference increased with increasing age, whereas the diastolic difference remained unchanged.4 This observation contrasts with the present findings showing that the systolic OBP–HBP difference is similar among subjects aged >30 years but lower in younger adults, and the diastolic difference is reduced with aging. This disagreement might be attributed to methodological differences in the analysis that was based on individual subject data in the present work, compared with aggregated data in the meta-analysis by Ishikawa et al.4, 18
Stergiou et al.5 investigated the relationship between office and out-of-office BP in 642 adults and children who were referred to a hypertension clinic. The analysis of adults (n=465) confirms the consistently higher OBP than HBP in all age subgroups but with different patterns of change than in the present study.5 Although both systolic OBP and HBP increased with aging, there was a ‘plateau’ period in middle age. In addition, both diastolic OBP and HBP displayed an inverse U-shaped relationship with aging.5 These partially contradictory results might be attributed to different BP evaluation protocols and participant characteristics. The considerably higher BP levels and hypertension prevalence in the study by Stergiou et al.5 are because that study included subjects who were referred to a hypertension clinic.18 The large population sample of the present analysis (n=5689 vs. 642 in the study by Stergiou et al.5) allowed a thorough analysis of the OBP–HBP difference determinants by considering additional factors, including ethnicity, smoking, alcohol consumption, diabetes and cardiovascular disease.
Conen et al.6 investigated the age-specific differences between OBP and dABP based on the International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO) constructed from general population studies (n=9550). It should be noted that the IDACO and the IDHOCO projects, in addition to investigating different BP measurement methodologies (ambulatory and home BP, respectively), were based on different databases, as they included very dissimilar studies and populations (13 cohorts in the IDACO compared with 6 in the IDHOCO). Eleven of 13 cohorts included in the IDACO analysis by Conen et al.6 were not included in the present work, and 4 of 6 cohorts included in the present work were not included in that by Conen et al.6 Despite these differences, Conen et al.,6 in line with the present study, reported that systolic OBP displayed a progressive increase with aging from 117 to 149 mm Hg. Thus, there was an increase from the youngest to the oldest subgroup of 32 compared with 30 mm Hg in the present study.6 However, the systolic dABP increase with age was only 13 mm Hg (from 123 to 136 mm Hg), which was approximately half of the respective HBP increase in the present study (27 mm Hg, from 109 to 136 mm Hg).6 The comparison of the present work with that by Conen et al.6 suggests that systolic dABP is higher than HBP in younger individuals in the general population, and this difference is eliminated with increasing age. These findings are supported by the abovementioned study by Stergiou et al.5 in subjects who were referred to a hypertension clinic and assessed by dABP and HBP monitoring. This result might be explained by the higher activity levels of the younger subjects during the day, whereas HBP is measured in a sitting position.
The increase in OBP and HBP with aging is consistent with the higher prevalence of hypertension with aging, together with a higher awareness and concern about cardiovascular risks in the elderly.19 The higher OBP than HBP across all age subgroups is probably because of the alert reaction in the office (white-coat effect). Moreover, HBP may often detect additional aspects of BP behavior, such as postprandial hypotension, a frequent phenomenon especially in elderly hypertensives.20 Regarding the factors affecting the OBP–HBP difference, the present analysis confirms previous reports showing that older age and smoking decrease this difference.21, 22 Furthermore, cardiovascular disease history was found to diminish whereas sustained hypertension aggravated the BP discrepancies.
This study confirmed the increasing prevalence of all hypertension phenotypes (and particularly sustained hypertension) with aging that was probably underestimated because of the exclusion of treated hypertensives. In most age subgroups, white-coat hypertension was more prevalent than masked hypertension, with this difference tending to be eliminated in the youngest and oldest individuals and more common than sustained hypertension until the fifth decade of age. These findings contrast with the data by Conen et al.6 based on dABP, in which masked hypertension reached the highest rates in individuals aged 30–50 years, whereas in those aged <50–60 years, white-coat hypertension was less common than in the present study. Although it has been suggested that dABP and HBP are similar and potentially interchangeable methods for diagnosing hypertension,23, 24 the aforementioned disparity indicates that the measurement method used to define hypertension phenotypes is crucial and that the BP thresholds recommended by the current guidelines may not be appropriate in all subjects irrespective of their age. Moreover, this study confirmed the known impact of aging and obesity in increasing the prevalence of all hypertension phenotypes25, 26, 27, 28 and that male gender is a determinant for masked and sustained hypertension.25, 29 The known association of masked hypertension with smoking and diabetes mellitus26, 27 was also observed but not the aggravating role of alcohol.27
From a clinical viewpoint, the present finding that the OBP–HBP difference changes with increasing age raises concerns about the applicability of the established reference values in adults of the entire age spectrum. Current guidelines based on distributional analyses of cross-sectional studies established the diagnostic HBP threshold at 135/85 mm Hg for all adults. However, Niiranen et al.,30 analyzing the IDHOCO database, introduced population-based outcome-driven HBP thresholds at slightly lower values (130/85 mm Hg). In addition, Nomura et al.31 showed that when these thresholds were stratified by gender and age, there was no significant difference between genders, but there was a trend for a higher threshold (∼4/1 mm Hg, systolic/diastolic) in subjects aged ⩾60 years compared with younger adults. However, the present analysis did not examine BP thresholds but rather the relationship of OBP with HBP across the age spectrum. Moreover, in contrast to other IDHOCO papers,30, 31, 32 it was based on a cross-sectional analysis and a different data set that did not include outcome data.
The main advantages of the present study are the large sample size derived from population cohorts and the analysis of individual subjects. The limitations include (1) different methodologies for evaluating the participants’ characteristics in different cohorts, (2) uneven age subgroup sizes with limited precision in the youngest subgroup and (3) the youngest group including only Caucasians. The heterogeneity in the implementation of HBP monitoring schedules in terms of the number or the timing of readings could also be considered as a limitation; however, the results were robust when additional analyses were performed. Interestingly, when only subjects with at least 12 available HBP readings were included (based on the minimum acceptable HBP monitoring schedule according to the European Society of Hypertension guidelines), only minor differences were observed compared with the main analysis.
References
Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, Kario K, Lurbe E, Manolis A, Mengden T, O'Brien E, Ohkubo T, Padfield P, Palatini P, Pickering T, Redon J, Revera M, Ruilope LM, Shennan A, Staessen JA, Tisler A, Waeber B, Zanchetti A, Mancia G ; ESH Working Group on Blood Pressure Monitoring. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens 2008; 26: 1505–1526.
ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2013; 31: 1925–1938.
Pickering TG, Miller NH, Ogedegbe G, Krakoff LR, Artinian NT, Goff D ; American Heart Association American Society of Hypertension Preventive Cardiovascular Nurses Association. Call to action on use and reimbursement for home blood pressure monitoring: executive summary: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension 2008; 52: 1–9.
Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE . Age and the difference between awake ambulatory blood pressure and office blood pressure: a metaanalysis. Blood Press Monit 2011; 16: 159–167.
Stergiou GS, Ntineri A, Kollias A, Destounis A, Nasothimiou E, Roussias L . Changing relationship among clinic, home and ambulatory blood pressure with increasing age. J Am Soc Hypertens 2015; 9: 544–552.
Conen D, Aeschbacher S, Thijs L, Li Y, Boggia J, Asayama K, Hansen TW, Kikuya M, Björklund-Bodegård K, Ohkubo T, Jeppesen J, Gu YM, Torp-Pedersen C, Dolan E, Kuznetsova T, Stolarz-Skrzypek K, Tikhonoff V, Schoen T, Malyutina S, Casiglia E, Nikitin Y, Lind L, Sandoya E, Kawecka-Jaszcz K, Mena L, Maestre GE, Filipovský J, Imai Y, O'Brien E, Wang JG, Risch L, Staessen JA . Age-specific differences between conventional and ambulatory daytime blood pressure values. Hypertension 2014; 64: 1073–1079.
Niiranen TJ, Thijs L, Asayama K, Johansson JK, Ohkubo T, Kikuya M, Boggia J, Hozawa A, Sandoya E, Stergiou GS, Tsuji I, Jula AM, Imai Y, Staessen JA ; IDHOCO Investigators. The International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO): moving from baseline characteristics to research perspectives. Hypertens Res 2012; 35: 1072–1079.
Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S . Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16: 971–975.
Niiranen TJ, Hänninen MR, Johansson J, Reunanen A, Jula AM . Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure. Hypertension 2010; 55: 1346–1351.
Niu K, Hozawa A, Awata S, Guo H, Kuriyama S, Seki T, Ohmori-Matsuda K, Nakaya N, Ebihara S, Wang Y, Tsuji I, Nagatomi R . Home blood pressure is associated with depressive symptoms in an elderly population aged 70 years and over: a population-based, cross-sectional analysis. Hypertens Res 2008; 31: 409–416.
Stergiou GS, Baibas NM, Kalogeropoulos PG . Cardiovascular risk prediction based on home blood pressure measurement: the Didima study. J Hypertens 2007; 25: 1590–1596.
Schettini C, Bianchi M, Nieto F, Sandoya E, Senra H . Ambulatory blood pressure: normality and comparison with other measurements. Hypertension Working Group. Hypertension 1999; 34: 818–825.
Barochiner J, Cuffaro PE, Aparicio LS, Elizondo CM, Giunta DH, Rada MA, Morales MS, Alfie J, Galarza CR, Waisman GD . [Reproducibility and reliability of a 4-day HBPM protocol with and without first day measurements]. Rev Fac Cien Med Univ Nac Cordoba 2011; 68: 149–153.
Cacciolati C, Tzourio C, Dufouil C, Alpérovitch A, Hanon O . Feasibility of home blood pressure measurement in elderly individuals: cross-sectional analysis of a population-based sample. Am J Hypertens 2012; 25: 1279–1285.
Niiranen TJ, Asayama K, Thijs L, Johansson JK, Hara A, Hozawa A, Tsuji I, Ohkubo T, Jula AM, Imai Y, Staessen JA ; IDHOCO Investigators. Optimal number of days for home blood pressure measurement. Am J Hypertens 2015; 28: 595–603.
Stergiou GS, Rarra VC, Yiannes NG . Changing relationship between home and office blood pressure with increasing age in children: the Arsakeion School study. Am J Hypertens 2008; 21: 41–46.
Stergiou GS, Karpettas N, Panagiotakos DB, Vazeou A . Comparison of office, ambulatory and home blood pressure in children and adolescents on the basis of normalcy tables. J Hum Hypertens 2011; 25: 218–223.
Stergiou GS, Ntineri A, Kollias A . Changing relationship between office, ambulatory and home blood pressure with increasing age: a neglected issue. Hypertension 2014; 64: 931–932.
Spruill TM, Pickering TG, Schwartz JE, Mostofsky E, Ogedegbe G, Clemow L, Gerin W . The impact of perceived hypertension status on anxiety and the white coat effect. Ann Behav Med 2007; 34: 1–9.
Barochiner J, Alfie J, Aparicio LS, Cuffaro PE, Rada MA, Morales MS, Galarza CR, Marín MJ, Waisman GD . Postprandial hypotension detected through home blood pressure monitoring: a frequent phenomenon in elderly hypertensive patients. Hypertens Res 2014; 37: 438–443.
Hozawa A, Ohkubo T, Nagai K, Kikuya M, Matsubara M, Tsuji I, Ito S, Satoh H, Hisamichi S, Imai Y . Factors affecting the difference between screening and home blood pressure measurements: the Ohasama Study. J Hypertens 2001; 19: 13–19.
Imai Y, Ohkubo T, Tsuji I, Hozawa A, Nagai K, Kikuya M, Aihara A, Sekino M, Michimata M, Matsubara M, Ito S, Satoh H, Hisamichi S . Relationships among blood pressures obtained using different measurement methods in the general population of Ohasama, Japan. Hypertens Res 1999; 22: 261–272.
Stergiou GS, Salgami EV, Tzamouranis DG, Roussias LG . Masked hypertension assessed by ambulatory blood pressure versus home blood pressure monitoring: is it the same phenomenon? Am J Hypertens 2005; 18: 772–778.
Stergiou GS, Skeva II, Baibas NM, Kalkana CB, Roussias LG, Mountokalakis TD . Diagnosis of hypertension using home or ambulatory blood pressure monitoring: comparison with the conventional strategy based on repeated clinic blood pressure measurements. J Hypertens 2000; 18: 1745–1751.
Alwan H, Pruijm M, Ponte B, Ackermann D, Guessous I, Ehret G, Staessen JA, Asayama K, Vuistiner P, Younes SE, Paccaud F, Wuerzner G, Pechere-Bertschi A, Mohaupt M, Vogt B, Martin PY, Burnier M, Bochud M . Epidemiology of masked and white-coat hypertension: the family-based SKIPOGH study. PLoS ONE 2014; 9: e92522.
Cacciolati C, Hanon O, Alpérovitch A, Dufouil C, Tzourio C . Masked hypertension in the elderly: cross-sectional analysis of a population-based sample. Am J Hypertens 2011; 24: 674–680.
Hänninen MR, Niiranen TJ, Puukka PJ, Mattila AK, Jula AM . Determinants of masked hypertension in the general population: the Finn-Home study. J Hypertens 2011; 29: 1880–1888.
Hänninen MR, Niiranen TJ, Puukka PJ, Jula AM . Comparison of home and ambulatory blood pressure measurement in the diagnosis of masked hypertension. J Hypertens 2010; 28: 709–714.
Schoenthaler AM, Schwartz J, Cassells A, Tobin JN, Brondolo E . Daily interpersonal conflict predicts masked hypertension in an urban sample. Am J Hypertens 2010; 23: 1082–1088.
Niiranen TJ, Asayama K, Thijs L, Johansson JK, Ohkubo T, Kikuya M, Boggia J, Hozawa A, Sandoya E, Stergiou GS, Tsuji I, Jula AM, Imai Y, Staessen JA ; International Database of Home blood pressure in relation to Cardiovascular Outcome Investigators. Outcome-driven thresholds for home blood pressure measurement: international database of home blood pressure in relation to cardiovascular outcome. Hypertension 2013; 61: 27–34.
Nomura K, Asayama K, Thijs L, Niiranen TJ, Lujambio I, Boggia J, Hozawa A, Ohkubo T, Hara A, Johansson JK, Sandoya E, Kollias A, Stergiou GS, Tsuji I, Jula AM, Imai Y, Staessen JA ; International Database of Home Blood Pressure in Relation to Cardiovascular Outcome Investigators. Thresholds for conventional and home blood pressure by sex and age in 5018 participants from 5 populations. Hypertension 2014; 64: 695–701.
Aparicio LS, Thijs L, Asayama K, Barochiner J, Boggia J, Gu YM, Cuffaro PE, Liu YP, Niiranen TJ, Ohkubo T, Johansson JK, Kikuya M, Hozawa A, Tsuji I, Imai Y, Sandoya E, Stergiou GS, Waisman GD, Staessen JA ; International Database on HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO) Investigators. Reference frame for home pulse pressure based on cardiovascular risk in 6470 subjects from 5 populations. Hypertens Res 2014; 37: 672–678.
Acknowledgements
The authors acknowledge the expert clerical assistance of Mrs Annick De Soete and Mrs Renilde Wolfs. The European Union (HEALTH-2011.2.4.2-2-EU-MASCARA, HEALTH-F7-305507 HOMAGE and the European Research Council Advanced Researcher Grant-2011-294713-EPLORE), the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0881.13 and G.088013), currently support the Studies Coordinating Centre in Leuven. The Ohasama study was supported by Grants for Scientific Research (23249036, 23390171, 24390084, 24591060, 24790654, 25253059, 25461083, 25461205, 25860156, 26282200 and 26860093) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; a Grant-in-Aid from the Japan Society for the Promotion of Science (JSPS) fellows (25.7756, 25.9328, 26.857 and 27.656); the Japan Arteriosclerosis Prevention Fund; Intramural Research Fund (22-4-5) for Cardiovascular Diseases of National Cerebral and Cardiovascular Center; and a Health Labour Sciences Research Grant (H26-Junkankitou [Seisaku]-Ippan-001) from the Ministry of Health, Labour, and Welfare; and A Scheme to Revitalize Agriculture and Fisheries in Disaster Area through Deploying Highly Advanced Technology (NouEi 2-02) from the Ministry of Agriculture, Forestry and Fisheries, Japan. The Finn-Home Project Organisation involved the Finnish Centre for Pensions, Social Insurance Institution, National Public Health Institute, Local Government Pensions Institution, National Research and Development Centre for Welfare and Health, Finnish Dental Society and the Finnish Dental Association, Statistics Finland, Finnish Work Ënvironment Fund, Finnish Institute for Occupational Health, UKK Institute for Health Promotion, State Pensions Office and State Work Environment Fund. The Tsurugaya study was supported by a Health Sciences Research Grant for Health Service (H21-Choju-lppan-O01) from the Ministry of Health, Labour and Welfare, Japan, and the Japan Arteriosclerosis Prevention Fund. The Asociacion Espaniola Primera de Socorros Mutuos and the Agencia Nacional de Innovacion e Investigacion and Gramon-Bago supported the Montevideo study. The Three-City Study is conducted under a partnership agreement between the Institut National de la Santé et de la Recherche Médicale (INSERM), the Victor Segalen- Bordeaux II University, and Sanofi-Aventis. The Fondation pour la Recherche Médicale funded the preparation and initiation of the study. The Fondation Plan Alzheimer partly funded the follow-up of the study. The 3C Study is also supported by the Caisse Nationale Maladie des Travailleurs Salariés, Direction Générale de la Santé, MGEN, Institut de la Longévité, Conseils Régionaux of Aquitaine and Bourgogne, Fondation de France and Ministry of Research-INSERM Programme ‘Cohortes et collections de données biologiques’. The funding organizations played no role in the design and conduct of the study; in the collection, management, analysis and interpretation of the data; or in the preparation, review or approval of the manuscript.
IDHOCO Investigators Japan (Ohasama): K Asayama, T Ohkubo, M Kikuya, R Inoue, M Satoh, M Hosaka, MT Utsugi, T Hirose, A Hara, N Fukushima, Obara, H Metoki and Y Imai; Finland (Finn-Home): T Niiranen, J Johansson, S Sivén and A Jula; Japan (Tsurugaya): K Ohmori-Matsuda, S Kuriyama, M Kakizaki, A Hozawa and I Tsuji; Greece (Didima): A Ntineri, A Kollias, N Boubouchairopoulou, G Thomopoulou, T Mountokalakis and G Stergiou; Uruguay (Montevideo): J Boggia and E Sandoya; France (Bordeaux): C Tzourio.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Ntineri, A., Stergiou, G., Thijs, L. et al. Relationship between office and home blood pressure with increasing age: The International Database of HOme blood pressure in relation to Cardiovascular Outcome (IDHOCO). Hypertens Res 39, 612–617 (2016). https://doi.org/10.1038/hr.2016.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.32
Keywords
This article is cited by
-
Home sphygmomanometers can help in the control of blood pressure: a nationwide field survey
Hypertension Research (2018)