Abstract
The neutrophil to lymphocyte ratio (NLR) is increased in various cardiovascular diseases. The objective of this study is to determine whether the NLR is increased in persons suffering from hypertension with hyperhomocysteinemia (HTH). We retrospectively analyzed the results of a large cohort of individuals undergoing health examinations with respect to NLR values, homocysteine (HCY) concentration, total cholesterol, triglyceride (TG) concentration, glucose concentration, creatinine (Cr) concentration, smoking status, drinking status and blood pressure. When participants were grouped according to the NLR quartiles, there were strong, graded increases in HCY (P<0.001) and the numbers of patients suffering from HTH were up to two-fold higher in the fourth vs. the first quartile. The NLR of the participants suffering from HTH group was significantly higher than the participants suffering from hypertension in the non-HTH group and the normotension group. In an unconditional multiple logistic regression analysis, NLR predicted HTH independently of age, sex, body mass index, smoking, drinking, TG and Cr. The present study demonstrated that the NLR value increased in the HTH group and positively correlated with HCY but not with blood pressure.
Similar content being viewed by others
Introduction
Hypertension is estimated to affect over 200 million Chinese individuals and its incidence has dramatically increased in recent years, especially in the middle aged and elderly populations.1 Up to two-thirds of individuals with hypertension are undiagnosed or untreated.1 As many as one-third of individuals who live in the Chinese South region have plasma homocysteine (HCY) ⩾10 μmol l−1, and in the northern region the proportion is three-fifth. In individuals with hypertension, the prevalence of hyperhomocysteinemia was significantly higher than in healthy individuals.2 Persons suffering from hypertension with hyperhomocysteinemia (HTH) have a higher risk of developing ischemic stroke3 and cardiovascular events4 than persons suffering from hypertension alone.
Hyperhomocysteinemia and hypertension increase the risk of ischemic stroke and cardiovascular events are mutually reinforcing. Although definitive mechanisms have not been completely elucidated, an accumulating body of evidence suggests that chronic low-grade systemic inflammation might have a crucial intermediary role in pathogenesis. Previous studies suggest that HCY can induce the expression of monocyte chemoattractant protein-1 and interleukin-8 (IL-8) by impairing endothelial cells. This may then promote neutrophil recruitment and induce leukocyte activation, accelerating atherosclerotic lesion formation.5 Moreover, neutrophil infiltration was found to have a role in ischemic stroke.6
The neutrophil to lymphocyte ratio (NLR), a major inflammation biomarker, is calculated by dividing the absolute neutrophil counts by the absolute lymphocyte count. Recent evidence documented a strong association between an elevation in NLR and the occurrence of stroke,7, 8 cardiac events,9 acute coronary syndrome,10 heart failure,11 as well as fatal and nonfatal events.
Despite these findings, to the best of our knowledge, an association between the NLR and HTH has not been reported in the literature. HCY has been reported to be associated with inflammatory biomarkers. Therefore, we evaluated whether the NLR is increased in HTH.
Materials and methods
Study participants
The study involved participants from a large company, including current and retired employees. According to the company’s policy, all current and retired employees are provided with an annual health examination. Between January 2014 and December 2014, a total of 6788 participants (4238 men and women 2550, aged 26–92 years, mean 58 years) self-reported personal health information including medical history, family history, smoking status, alcohol consumption and measured height, weight and blood pressure, and provided blood specimens for hematological and biochemical testing. Hypertensive patients were registered and received medical services at the department of chronic non-communicable diseases of our hospital. According to the Chinese guidelines for the management of hypertension, hypertension was defined as systolic blood pressure of 140 mm Hg or higher, or diastolic blood pressure of 90 mm Hg or higher. HTH was defined as plasma HCY ⩾10 μmol l−1 with essential hypertension. Non-HTH was defined as plasma HCY <10 μmol l−1 with essential hypertension.
Laboratory procedures
Blood specimens were collected in the morning from 0730–0900 h when the subjects were still fasting from the previous evening. Fasting was defined as not having consumed a meal for more than 10 h. Whole blood samples were collected in EDTA-K2 and were used for hematological analysis; serum specimens were collected in dried vacuum tubes, centrifuged within 1 h and used for biochemical analyses, including total cholesterol (TC), triglyceride (TG), glucose (Glu), creatinine (Cr) and HCY assays.
Hematological testing was performed on the Sysmex XE-2100 (Sysmex Corporation, Kakogawa, Hyogo, Japan) automated hematology analyzer. Biochemical parameters (Glu, TC, TGs, Cr and HCY) were evaluated by enzymatic techniques in an AU2700 Olympus Autoanalyzer (Olympus Corporation, Tokyo, Japan). TC was measured via colorimetric analysis. The fasting plasma Glu was measured using a hexokinase assay. TG was measured using a glycerol phosphate oxidase assay. Cr was measured using an enzymatic assay. An enzymatic cycling assay was used for HCY analysis. Throughout the study, routine internal quality-control procedures and an external quality assessment scheme were used to validate the reliability of the results. As severe lipidemia and hemolysis could interfere with the assessments, samples with a concentration of TGs >5 mmol l−1 or a free hemoglobin value higher than 5 g l−1 were scheduled for re-acquisition.
An Omron HEM-6000 (OMRON Corporation, Dalian, China) was used to measure blood pressure after the subjects rested for 5 min in a sitting position in a quiet room. Height and weight were measured at the screening center by two trained nurses and body mass index was calculated as the weight divided by the squared height (kg m−2).
Statistical analysis
The data were expressed as the median (5th–95th) or counts. For normality tests, skewed variables (HCY and NLR) were logarithmically transformed to improve normality before analysis. Normally distributed continuous variables were compared by one-way analysis of variance (followed by a least significant difference test for multiple comparisons between groups). As the distributions of TG were skewed, differences in the distributions of these variables between groups were determined using the non-parametric Kruskal–Wallis test. For categorical variables, differences between groups were examined using the χ2-test. The χ2-test was also used to calculate the odds ratio (by the Bonferroni test for multiple comparisons). An unconditional logistic regression was used to identify factors that were independently associated with HTH. A receiver operating characteristic curve was used to determine the cutoff value of NLR to predict HTH vs. non-HTH. The statistical analyses were performed using the statistical package SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). The level of statistical significance was set at P<0.05.
Results
NLR results were categorized into quartiles and the main findings from this investigation are shown in Table 1. As predicted, individuals in the highest NLR quartile were, on average, older and had higher TC, Glu and Cr levels than individuals in the lowest NLR quartile. There were strong, graded increases in HCY and HTH prevalence across the NLR quartiles, and the number of HTH patients was up to two-fold higher in the fourth quartile vs. the first quartile of NLR. The systolic blood pressure and diastolic blood pressure were not significantly increased in the highest NLR quartile compared with the lowest NLR quartile, although the difference was statistically significant.
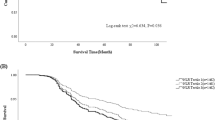
We evaluated the odds ratio of HTH according to the NLR quartiles. As shown in Figure 1, the risks of HTH in quartiles II, III and IV relative to the odds ratio of I were 1.426 (95% confidence interval, 1.091–1.863, P=0.009), 1.671 (95% confidence interval, 1.270–2.148, P<0.001) and 2.117 (95% confidence interval, 1.645–2.725, P<0.001), respectively. The odds ratios of HTH steadily increased across the NLR quartiles.
Next, we compared the NLR values of HTH group with the non-HTH group and whether there were other differences between the groups. These results are shown in Table 2. The individuals in the HTH group were, on average, older and had a higher smoking ratio, drinking ratio and had higher Cr levels than individuals in the non-HTH group. The NLR values of the HTH group were significantly higher than the non-HTH group. Similar results were found when the participants were stratified by age (<49, 49–65 and >65 years; Table 3). In addition, the NLR values were not statistically significantly different when comparing the non-HTH group with the normotension group. The systolic blood pressure and diastolic blood pressure values of the HTH group were not significantly greater than the non-HTH group.
In the unconditional multiple logistic regression analysis performed on the entire population, the following risk factors were evaluated: gender, age, body mass index, smoking, drinking, Glu, TC, TG, Cr and NLR. HTH was significantly associated with all variables, except for Glu and TC. These results are shown in Table 4. The NLR was a positive predictor of HTH independently of sex, age, body mass index, smoking, drinking, TG and Cr.
A receiver operating characteristic analysis was used to determine the cutoff value of NLR to predict HTH vs. non HTH. A NLR value of 1.88 or higher predicted HTH with a sensitivity of 45.2% and specificity of 67.2% (Figure 2).
Discussion
The findings of the present study are as follows: (1) the NLR values of the HTH group were significantly greater than the non-HTH group, followed by the normotension group; (2) elevated NLR values were positively correlated with increased HCY; and (3) elevated NLR values have higher odds ratios for HTH. To the best of our knowledge, this is the first report on the clinical significance of the NLR in HTH.
Individuals with HTH have a higher predicted risk for developing coronary atherosclerosis and vascular thrombosis later in life. A case–control study reported that the risk of cardiovascular events for individuals with HTH nearly quintupled compared with individuals with hypertension alone and was 25-fold higher than healthy normotensive people.12 A prospective cohort study of Chinese individuals during a 12-year follow-up period demonstrated that individuals with HCY >9.47 μmol l−1 had a 2.3-fold increased risk for stroke and myocardial infarction, and there was a 2.4-fold increased risk of death in individuals with HCY >11.84 μmol l−1.13 An accumulating body of evidence has shown that in healthy people, a 5 μmol l−1 increase in HCY is associated with a 60% increase in men and 80% increase in women in the risk of acute coronary syndrome and a 50% increase in the risk of stroke.14 The risks are not only associated with cardiovascular and cerebrovascular conditions; similar results were also found in peripheral vascular conditions.15
NLR is an inflammatory index in complete blood counts and could be easily and inexpensively measured clinically. Over the past few years, the association between an elevated NLR and cardiovascular and cerebrovascular diseases has become increasingly clear. Recent prospective studies have found that an elevated NLR is a prognostic marker of stroke8, 16 and is strongly associated with the risk of a cardiovascular event.9 Moreover, an accumulating body of evidence suggests that NLR is a useful parameter for predicting mortality in patients with coronary artery disease17, 18 or myocardial infarction.19 As HTH is a typical cardiovascular and cerebrovascular disease, we hypothesized that the NLR value might be increased in HTH. This hypothesis has been supported by the present study.
Some inflammatory markers have been reported to be correlated with hypertension. A study of African Americans reported that increased neutrophil levels or decreased lymphocyte levels could predict the development of hypertension.20. A greater NLR value has also been observed in some subtypes of hypertension. For instance, a recent small case–control study in Turkey investigated resistant hypertension21, showing that the NLR value in cases of resistant hypertension was 3.15 vs. 2.11 in controlled hypertension cases or 1.87 in normotension cases. Another case–control study of non-dipper hypertension22 reported that individuals with non-dipper hypertension had a greater NLR value compared with dipper hypertension. Other inflammatory markers such as C-reactive protein have been found to be positively correlated with blood pressure23 and independently predict hypertension.24 Similar to C-reactive protein, IL-6 has also been found to be positively correlated with blood pressure. Furthermore, animal experiments showed that neutrophil gelatinase-associated lipocalin increased in young spontaneously hypertensive rats.25 However, studies have not considered the effect of HTH. The results of our investigation demonstrate that the NLR did not increase with increasing blood pressure and was not significantly different between the non-HTH group and the normotension group. However, the NLR is linked to HCY and in the HTH group the NLR was significantly greater than in the non-HTH group and the normotension group. Therefore, perhaps the relationship between the NLR and HTH is mainly attributable to the influence of HTH.
Several in vitro and in vivo studies have shown that HCY can cause inflammation by a variety of mechanisms. HCY was found to enhance the endothelial cell production of superoxide anions26 and superoxide anions decrease the availability of endothelial nitric oxides.27 Decreased endothelial nitric bioavailability can increase the expression of monocyte chemoattractant protein-1,28 an inflammatory cell chemoattractant oxide. The expression of other inflammatory cell chemoattractant oxides, such as IL-8, has also been increased, owing to the effects of HTH. Therefore, the association between NLR and HTH, possibly due to HCY, could induce the expression of monocyte chemoattractant protein-1 and IL-8 by impairing endothelial cells, and monocyte chemoattractant protein-1 and IL-8 could then promote neutrophil recruitment and induce leukocyte activation to accelerate atherosclerotic lesion formation. As individuals with HTH have a higher risk of cardiovascular events and stroke, and elevated NLR values are linked to an increased risk of cardiovascular events and stroke, we hypothesized that the increased risk in part caused by HCY could indirectly attract inflammatory cells. In addition, if HCY is found to directly attract inflammatory cells to infiltrate the cardiac vasculum and cerebral vasculum in future in vitro or in vivo studies, this may confirm the results of this study and provide a possible mechanism to explain why HTH is associated with a higher risk of stroke and cardiovascular events, and provide possible targets for future therapies.
Many potential confounding factors could affect the NLR value, HCY concentrations and blood pressure. In Chinese individuals, men consume more tobacco and alcohol,29 and have higher HCY concentrations.30 Smoking is associated with elevated NLR values31 and has a strong positive correlation with HCY concentrations.32 Alcohol consumption is associated with an augmented risk for hypertension. HCY concentrations have been reported to increase with age.30 Hypercholesterolemia accelerates angiosclerosis. Impaired renal function is not conducive to the metabolism of HCY and consequently increases HCY concentrations.33 Obesity, even without metabolic syndrome, is also associated with elevated NLR values.34 However, in the unconditional multiple logistic regression analysis after adjustment for multivariate confounding factors, the relationships between NLR and HTH were still observable in our investigation, indicating that these associations are strong and convincing.
The NLR is a sensitive but nonspecific indicator, which is easily influenced by the above-described factors and appears to present complicated information in clinical applications. As hypertensive patients with these risk factors are also linked to a worse prognosis, an elevated NLR value may be a predictor of morbidity and mortality in hypertensive patients, and may also be able to be exploited in the risk stratification of hypertension as has been done with other cardiovascular diseases.16, 17, 18, 19 Relevant studies of poor clinical outcome subtypes of hypertension, such as resistant hypertension21 and non-dipper hypertension,22 have observed greater NLR values compared with the standard subtype of hypertension; these results appear to support the opinion that the NLR could be used for risk stratification. High-risk hypertensive patients benefited from diminishing oxidative stress in a recent clinical trial,35 proving the relationship between inflammation and risk from a clinical application point of view. NLR values may be applied to the risk stratification of hypertension if the results of the present study are confirmed in future follow-up studies, and their further application may offer a chance to improve our understanding of pathophysiology and improve treatment for high risk hypertension.
This study has several limitations. First, it is possible that a minority of undiagnosed hypertension subjects at study entry might have biased our results. Nevertheless, the cohort underwent a medical examination by our hospital every year and this possibility is infinitesimal. Second, no information regarding vitamin B6 was available to evaluate whether the NLR link to HCY was independent or mediated by vitamin B6.
Regardless of these limitations, several strengths should be noted. First, we included a very large cluster sample, which is perhaps representative of the adult inhabitants living in the area of southern China. Second, uniform methods were used to collect data for all assays in our clinical laboratory. Third, the adjustment for potential confounding factors including gender, age, body mass index, smoking, drinking, Glu, TC, TG and Cr permitted us to ensure that we provided an impartial estimate for the correlation between NLR and HTH.
In summary, this cross-sectional study demonstrated that the NLR value increased in the hypertension with the HTH group and was positively correlated with HCY and not related to blood pressure This suggests that that the hypertension with HTH group had a higher risk of cardiovascular events and stroke, perhaps partially because HCY could indirectly attract inflammatory cells. The NLR could be used for risk stratification of hypertension and risk determination.
Change history
05 August 2016
This article has been corrected since Advance Online Publication, and an erratum is also printed in this issue.
References
Gao Y, Chen G, Tian H, Lin L, Lu J, Weng J, Jia W, Ji L, Xiao J, Zhou Z . Prevalence of hypertension in China: a cross-sectional study. PLoS ONE 2013; 8: e65938.
Hao L, Ma J, Zhu J, Stampfer MJ, Tian Y, Willett WC, Li Z . High prevalence of hyperhomocysteinemia in Chinese adults is associated with low folate, vitamin B-12, and vitamin B-6 status. J Nutr 2007; 137: 407–413.
Ma Y, Zhao X, Zhang W, Liu L, Wang Y, Fang R, Wang Y . Homocysteine and ischemic stroke subtype: a relationship study in Chinese patients. Neurol Res 2010; 32: 636–641.
Ni M, Zhang XH, Jiang SL, Zhang Y . Homocysteinemia as an independent risk factor in the Chinese population at a high risk of coronary artery disease. Am J Cardiol 2007; 100: 455–458.
Poddar R, Sivasubramanian N, DiBello PM, Robinson K, Jacobsen DW . Homocysteine induces expression and secretion of monocyte chemoattractant protein-1 and interleukin-8 in human aortic endothelial cells implications for vascular disease. Circulation 2001; 103: 2717–2723.
Weston RM, Jones NM, Jarrott B, Callaway JK . Inflammatory cell infiltration after endothelin-1-induced cerebral ischemia: histochemical and myeloperoxidase correlation with temporal changes in brain injury. J Cereb Blood Flow Metab 2007; 27: 100–114.
Gökhan S, Ozhasenekler A, Mansur Durgun H, Akil E, Ustündag M, Orak M . Neutrophil lymphocyte ratios in stroke subtypes and transient ischemic attack. Eur RevMed Pharmacol Sci 2013; 17: 653–657.
Tokgoz S, Kayrak M, Akpinar Z, Seyithano lu A, Güney F, Yürüten B . Neutrophil Lymphocyte Ratio as a Predictor of Stroke. J Stroke Cereb Dis 2013; 22: 1169–1174.
Azab B, Chainani V, Shah N, Mcginn JT . Neutrophil-lymphocyte ratio as a predictor of major adverse cardiac events among diabetic population: a 4-year follow-up study. Angiology 2013; 64: 456–465.
Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS . Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol 2008; 102: 653–657.
Rudiger A, Burckhardt OA, Harpes P, Müller SA, Follath F . The relative lymphocyte count on hospital admission is a risk factor for long-term mortality in patients with acute heart failure. Am J Emerg Med 2006; 24: 451–454.
Graham IM, Daly LE, Refsum HM, Robinson K, Brattstr m LE, Ueland PM, Palma-Reis RJ, Boers GH, Sheahan RG, Israelsson B . Plasma homocysteine as a risk factor for vascular disease: The European Concerted Action Project. JAMA 1997; 277: 1775–1781.
Sun Y, Kuo-Liong C, Hsiu-Ching H, Ta-Chen SU, Chen MF, Yuan-Teh L . Use of serum homocysteine to predict stroke, coronary heart disease and death in ethnic Chinese. 12-year prospective cohort study. Circ J 2009; 73: 1423–1430.
Collaboration HS. Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA 2002; 288: 2015–2022.
Khandanpour N, Loke YK, Meyer FJ, Jennings B, Armon MP . Homocysteine and peripheral arterial disease: systematic review and meta-analysis. Eur J Vasc Endovasc Surg 2009; 38: 316–322.
Saliba W, Barnett Griness O, Elias M, Rennert G . Neutrophil to lymphocyte ratio (NLR) and risk of first episode stroke in patients with atrial fibrillation: a cohort study. J Thromb Haemost 2015; 13: 1971–1979.
Papa A, Emdin M, Passino C, Michelassi C, Battaglia D, Cocci F . Predictive value of elevated neutrophil-lymphocyte ratio on cardiac mortality in patients with stable coronary artery disease. Clin Chim Acta 2008; 395: 27–31.
Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS . Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol 2008; 102: 653–657.
Núñez J, Núñez E, Bodí V, Sanchis J, Miñana G, Mainar L, Santas E, Merlos P, Rumiz E, Darmofal H, Heatta AM, Llàcer A . Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarction. Am J Cardiol 2008; 101: 747–752.
Tian N, Penman AD, Mawson AR, Manning RD, Flessner MF . Association between circulating specific leukocyte types and blood pressure: the atherosclerosis risk in communities (ARIC) study. J Am Soc Hypertens 2010; 4: 272–283.
Belen E, Sungur A, Sungur MA, Erdoğan G . Increased neutrophil to lymphocyte ratio in patients with resistant hypertension. J Clin Hypertens 2015; 17: 532–537.
Sunbul M, Gerin F, Durmus E, Kivrak T, Sari I, Tigen K, Cincin A . Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper vs. non-dipper hypertension. Clin Exp Hypertens 2014; 36: 217–221.
Yamada S, Gotoh T, Nakashima Y, Kayaba K, Ishikawa S, Nago N, Nakamura Y, Itoh Y, Kajii E . Distribution of serum C-reactive protein and its association with atherosclerotic risk factors in a Japanese population Jichi Medical School Cohort Study. Am J Epidemiol 2001; 153: 1183–1190.
Sung KC, Suh JY, Kim BS, Kang JH, Kim H, Lee MH, Park JR, Kim SW . High sensitivity c-reactive protein as an independent risk factor for essential hypertension. Am J Hypertens 2003; 16: 429.
Heijnen BF, Van Essen H, Schalkwijk CG, Janssen BJ, Struijker-Boudier HA . Renal inflammatory markers during the onset of hypertension in spontaneously hypertensive rats. Hypertens Res 2014; 37: 100–109.
Jr GU, Welch GN, Fabian AJ . Stimulation of endothelial nitric oxide production by homocyst(e)ine. Atherosclerosis 1997; 132: 177–185.
Gryglewski RJ, Palmer RMJ, Moncada S . Superoxide anion is involved in the breakdown of endothelium-derived vascular relaxing factor. Nature 1986; 320: 454–456.
Tsao PS, Wang B, Buitrago R, Shyy JY, Cooke JP . Nitric oxide regulates monocyte chemotactic protein-1. Circulation 1997; 96: 934–940.
Hao L, Ma J, Stampfer MJ, Ren A, Tian Y, Tang Y, Willett WC, Li Z . Geographical seasonal and gender differences in folate status among Chinese adults. J Nutr 2003; 133: 3630–3635.
Hao L, Ma J, Zhu J, Stampfer MJ, Tian Y, Willett WC, Li Z . High prevalence of hyperhomocysteinemia in Chinese adults is associated with low folate, vitamin B-12, and vitamin B-6 status. J Nutr 2007; 137: 407–413.
Ishizaka N, Ishizaka Y, Toda E, Nagai R, Koike K, Hashimoto H, Yamakado M . Relationship between smoking, white blood cell count and metabolic syndrome in Japanese women. Diabetes Res Clin Pract 2007; 78: 72–76.
Jacques PF, Bostom AG, Wilson PW, Rich S, Rosenberg IH, Selhub J . Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr 2001; 73: 613–621.
Elshorbagy AK, Oulhaj A, Konstantinova S, Nurk E, Ueland PM, Tell GS, Nygård O, Vollset SE, Refsum H . Plasma creatinine as a determinant of plasma total homocysteine concentrations in the Hordaland Homocysteine Study: use of statistical modeling to determine reference limits. Clin Biochem 2007; 40: 1209–1218.
Ryder E, Diez-Ewald M, Mosquera J, Fernández E, Pedreañez A, Vargas R, Peña C, Fernández N . Association of obesity with leukocyte count in obese individuals without metabolic syndrome. Diabetes Metab Syndrome Clin Res Rev 2014; 8: 197–204.
Chida R, Hisauchi I, Toyoda S, Kikuchi M, Komatsu T, Hori Y, Nakahara S, Sakai Y, Inoue T, Taguchi I . Impact of irbesartan, an angiotensin receptor blocker, on uric acid level and oxidative stress in high-risk hypertension patients. Hypertens Res 2015; 38: 765–769.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gang, L., Yanyan, Z. Increased neutrophil to lymphocyte ratio in persons suffering from hypertension with hyperhomocysteinemia. Hypertens Res 39, 606–611 (2016). https://doi.org/10.1038/hr.2016.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.30
Keywords
This article is cited by
-
Neutrophil-lymphocyte ratio and its relation to microvascular complication in geriatric patients with diabetes: a case-controlled study
The Egyptian Journal of Internal Medicine (2022)
-
The neutrophil-to-lymphocyte ratio on admission is a good predictor for all-cause mortality in hypertensive patients over 80 years of age
BMC Cardiovascular Disorders (2017)
-
Association between mean platelet volume and hypertension incidence
Hypertension Research (2017)
-
The ratio of monocyte frequency to HDL cholesterol level as a predictor of asymptomatic organ damage in patients with primary hypertension
Hypertension Research (2017)
-
WBC count predicts the risk of new-onset peripheral arterial disease in a Chinese community-based population
Hypertension Research (2017)