Abstract
Eucommia ulmoides Oliver leaf extract (ELE) has been shown to have anti-hypertensive and anti-obesity effects in rats that are fed a high-fat diet (HFD). To explore the effects of chronic administration of ELE on body weight, blood pressure and aortic media thickness, 7-week-old male Wistar-Kyoto (WKY) rats were orally administered a normal diet, a 30% HFD, or a 5% ELE plus HFD ad libitum for 10 weeks. The HFD treatment caused mild obesity and hypertension in the normotensive rats, while rats receiving both ELE and the HFD had significantly lower body weights, less visceral and perirenal fat, lower blood pressure and thinner aortic media than the control rats receiving the HFD only. The plasma adiponectin/leptin ratio also improved in ELE-treated rats. Although plasma leptin levels were elevated in all HFD rats, adiponectin levels increased only in the ELE-treated rats. Anti-hypertensive and anti-obesity effects may be caused by the geniposidic acid (GEA) and/or asperuloside present in ELE. These findings suggest that chronic ELE administration prevents aortic media hypertrophy in early-stage obesity with hypertension. Long-term administration of ELE might inhibit the development of arteriosclerosis.
Similar content being viewed by others
Introduction
The World Health Organization has estimated that ~17.3 million people died from cardiovascular disease (CVD) in 2008;1 more than 80% of these individuals lived in low- and middle-income countries. More than 23 million people per year are predicted to die from CVD by 2030.1 Hypertension directly increases the risk of CVD and is responsible for at least 45% of CVD-related deaths.1 Of the components of metabolic syndrome (MS), hypertension is the most important determinant in the development of carotid intima-media thickness, which is a useful marker of early atherosclerosis development.2 A recent study shows that being overweight or obese has been a major risk factor for hypertension over the past 30 years in Japan.3 In obese individuals, the accumulated visceral fat tissues secrete adipocytokines, which cause metabolic abnormalities such as insulin resistance4 and hypertension.5 Both abdominal obesity and hypertension result in impaired cardiac function at the early asymptomatic stage of CVD.6, 7 Therefore, the early prevention and control of obesity and hypertension represent important approaches for reducing the risk of future CVD.
Eucommia ulmoides Oliver is a tree that is found in China and belongs to the Eucommiaceae family. Eucommia leaves (ELs) are used as a traditional Chinese anti-hypertensive medicine.8 In Japan, a bottled beverage made from ELs (Tochu-cha) is marketed as a government-approved food for specified health uses for people with elevated blood pressure. A hot water extract of ELs (ELE) has also demonstrated anti-hypertensive,9 anti-obesity,10 anti-hyperlipidemic,11 anti-oxidant,12 anti-hyperglycemic13 and insulin-sensitizing effects.14 The anti-hypertensive effects of ELE have been demonstrated in humans, where ELE intake reduced blood pressure in individuals with high-normal blood pressure and stage I hypertension, defined as the blood pressure range of 130–139 mm Hg/85–89 mm Hg, and 140–159 mm Hg/90–99 mm Hg, respectively.15 The anti-obesity effects of ELE have been evaluated in vivo using an MS-like rat model fed a high-fat diet (HFD) for 3 months; ELE intake decreased body weight, white adipose tissue (WAT) weight and plasma levels of triglyceride and total cholesterol in these animals.10 Recently, we studied a spontaneously hypertensive rat model fed a normal diet supplemented with 5% (w/w) ELE and found that long-term ELE administration suppressed systolic blood pressure (SBP), restored vascular function and prevented hypertrophy of the thoracic aorta.16 However, there is little information about the long-term effects of ELE on thoracic aorta morphology in early-stage obesity.
Based on the results of these previous in vivo studies of ELE, the present study was designed to examine the effects of chronic ELE administration on aortic media thickness in normotensive Wistar-Kyoto (WKY) rats fed a HFD containing 30% (w/w) lard. WKY rats are often used as controls in studies of spontaneously hypertensive rat (SHR), and they have been reported to develop aortic fat deposition more readily than other normotensive rat strains, such as Sprague-Dawley or Wistar rats.17 Therefore, WKY rats fed a HFD are a useful model of dietary-induced obesity and hypertension for studying early-stage arteriosclerosis. In this study, we investigated WKY rat body weight, WAT, SBP, thoracic aorta morphology and plasma adipocytokines such as adiponectin and leptin with and without ELE administration for 10 weeks.
Methods
Reagents
Ethanol was purchased from Kanto Chemical (Tokyo, Japan). Ethylenediaminetetraacetic acid (EDTA)-2 K, 10% buffered formalin and 30% H2O2 were purchased from Wako Pure Chemical Industries (Osaka, Japan). Citraconic anhydride solution (0.05%; ImmunoSaver) and 10% normal donkey serum were purchased from Nisshin EM (Tokyo, Japan) and Abcam (Cambridge, UK), respectively. Diaminobenzidine and hematoxylin were purchased from Dojindo Laboratories (Kumamoto, Japan) and Merck KGaA (Darmstadt, Germany), respectively.
Animals and experimental protocols
Six-week-old male WKY/Izm (n=24) rats were purchased from Japan SLC (Shizuoka, Japan) and were fed a normal diet (ND group, n=8), a HFD (HFD-control group, n=8), or a HFD with 5% (w/w) ELE (HFD-ELE group, n=8) for 10 weeks. They were given food and water ad libitum and housed in the experimental room at the Animal Research Center (Faculty of Agriculture, Shinshu University), which was maintained on a 12 h light/dark cycle. The ambient temperature of the room was 23±1.0 °C, with a relative humidity of 50±5%. All animal experiments were carried out in strict accordance with the Care and Management of Laboratory Animals and Relief of Pain (2006) published by the Japanese Ministry of the Environment and approved by the Animal Care Committee of the Faculty of Agriculture, Shinshu University (permit number: 260026). During the feeding period, food and water intake, body weight and SBP were measured. At the end of the experimental period, the animals were given diethyl ether anesthesia and then dissected. In each animal, the WAT weight, aortic media thickness, plasma adiponectin and leptin levels and leptin/adiponectin ratio were examined.
Preparation of ELE
ELs leaves were obtained from the Sichuan District of China, and ELE was prepared as described previously.18 Briefly, fresh ELs were pretreated with steam at 100–110 °C and then dried and roasted. The roasted leaves (2 tons) were soaked in 10 tons of water and heated for 1 h at 90 °C. After extraction, the slurry was filtered and concentrated. The concentrate was left to stand for 1 day before further filtration and vacuum drying; the yield of powdered extract was 18%. The content of GEA was 63.0 mg g−1 dry weight of ELE, as determined by high-performance liquid chromatography.19
Long-term dietary administration
A moderate-fat diet (Oriental Yeast Company, Tokyo, Japan) was fed to the ND group. This diet was composed of water (7.9%), protein (23.1%), lipid (5.1%), ash (5.8%), dietary fiber (2.8%) and nitrogen-free extract (55.3%); the total calorie content was 359 kcal per 100 g. The control HFD was prepared by adding 30% (w/w) lard and 5% (w/w) casein to this moderate-fat diet. The HFD was thus composed of 8.0% water, 18.8% protein, 32.5% lipid, 3.8% ash, 1.8% dietary fiber and 35.1% nitrogen-free extract; the total calorie content was 508 kcal per 100 g. The diet containing ELE was prepared by mixing 5% (w/w) ELE with this HFD; the total calorie content was 504 kcal per 100 g. After acclimation for 6 days, the animals were divided into three groups of eight animals that received the ND, the HFD, or the HFD plus 5% ELE for 10 weeks ad libitum. This dosing period was suitable for the evaluation of arteriosclerosis in early CVD caused by high fat-loading.20 During the experimental period, the rats’ body weights and food and water intake were measured twice a week, and the SBP was measured once a week using the tail cuff method (Softron BP98A; Softron, Tokyo, Japan).
Biochemical analyses
Biochemical analyses were performed at the end of the experimental period. Blood was drawn from the abdominal vena cava into an EDTA-2 K-coated tube, and the plasma was obtained by centrifuging the blood at 1200 g for 20 min at 4 °C. Plasma adiponectin and insulin levels were evaluated using a mouse/rat adiponectin enzyme-linked immunosorbent assay kit (Otsuka Pharmaceutical, Tokyo, Japan) and an ultra-high-sensitivity rat insulin assay kit (Morinaga Milk Industry, Tokyo, Japan), respectively. Plasma leptin, glucose, hemoglobin A1c (HbA1c), non-esterified fatty acid (NEFA), triglyceride, and total cholesterol levels were measured using an automated analyzer (Hitachi 7180; Hitachi, Tokyo, Japan).
Immunohistochemical analysis
This analysis was performed using an avidin-biotin-peroxidase complex technique, as described previously.16 The thoracic aorta of each rat (n=8/group) was isolated, as described in the ‘Animals and experimental protocols’ section. Briefly, the aortic tissue was fixed in 10% buffered formalin, embedded in paraffin, and sliced into 4 μm sections at the Research Center for Human and Environmental Science, Shinshu University. After deparaffinization of the sections, the antigen retrieval was performed by incubating the sections in ImmunoSaver for 50 min at 98 °C. Endogenous peroxidase and non-specific binding were blocked using 3% H2O2 for 30 min and 10% normal donkey serum for 30 min, respectively. The blocked sections were reacted with a polyclonal rabbit anti-alpha smooth muscle actin primary antibody (1:1000; Abcam) overnight at 4 °C. The treated sections were then incubated with a horseradish peroxidase-conjugated secondary antibody (1:500; Abcam) for 30 min at room temperature. Immunoreactivity was visualized using diaminobenzidine, and sections were counterstained with hematoxylin. Finally, the sections were washed in tap water, dehydrated using ethanol, coverslipped and observed using an Axio Imager A1 microscope (Carl Zeiss AG, Oberkochen, Germany) equipped with AxioVision software (Carl Zeiss AG) to measure the medial thickness.
Statistical analysis
All experimental data were presented as the mean±s.e.m. A P-value of <0.05 was taken to indicate a statistically significant difference between two groups using Student’s t-test.
Results
WKY rats were fed a normal diet (ND group, n=8), a HFD (HFD-control group, n=8), or a HFD with 5% (w/w) ELE (HFD-ELE group, n=8) for 10 weeks. During the feeding period, food and water intake, body weight and SBP were measured. After the study period, the WAT weight, aortic media thickness, plasma adiponectin and leptin levels and leptin/adiponectin ratio were examined.
Dietary intake, body weight and WAT weight
Table 1 shows the dietary intake and tissue weights in the study groups. During the 10-week treatment period, the average daily food intake of the HFD-control and HFD-ELE groups was significantly lower than that of the ND group (each P<0.01), but there was no significant difference between the food intake of the HFD-control and HFD-ELE groups. The differences in the average daily water intake of the three groups showed the same pattern of significance as the food intake. Caloric intake in the three groups was calculated based on their food intake. The average daily caloric intake of the ND group was significantly lower than that of the HFD-control group (P<0.05), but there was no significant difference between the caloric intake of the HFD-control and HFD-ELE groups. There were no significant differences among the initial average body weights of the ND, HFD-control and HFD-ELE groups (196.4±2.3, 202.4±3.2 and 204.6±3.0 g, respectively). The final body weight and body weight gain values of the HFD-control group were significantly higher than those of the ND group and HFD-ELE group (P<0.01). The mesenteric vascular bed and perirenal WAT weights in the HFD-control group increased significantly compared with the ND group (each P<0.01); however, these changes were significantly ameliorated in the HFD-ELE group (Table 1).
SBP
As shown in Figure 1, the SBP of WKY rats in the ND, HFD-control and HFD-ELE groups did not differ significantly at the beginning of the experiment. In the HFD-control group, the average SBP began to increase after 2 weeks of dietary intervention and differed significantly from that of the ND group from week 3 onward, when the rats were 9–17 weeks old (P<0.01, Figure 1). The SBP of the HFD-ELE group was significantly lower than that of the HFD-control group at 10–17 weeks old and did not differ significantly from that of the ND group throughout the experiment. The HFD treatment induced mild hypertension in WKY rats that were originally normotension.
Systolic blood pressure (SBP) in rats receiving a normal diet (ND), a high-fat diet (HFD) (HFD-control) or a HFD containing 5% Eucommia leaf extract (HFD-ELE) over the 10-week study period, when the animals were 7–17 weeks old (n=8 for each test group). All values represent the means±s.e.m. *P<0.05, **P<0.01, compared with the HFD-control group; #P<0.05, ##P<0.01, compared with the ND group.
Aortic media thickness
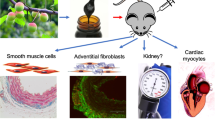
Figure 2 shows typical histology images of the aortic media from rats in the ND, HFD-control, and HFD-ELE groups. The vascular smooth muscle cells (VSMCs) were aligned in the ND and HFD-ELE groups. In contrast, the aortic media showed hypertrophy, and the VSMCs appeared disordered in the HFD-control group. Figure 3 shows thoracic aortic ring medial thickness in the ND, HFD-control, and HFD-ELE groups. The aortic media thickness in the HFD-control group was significantly greater than that observed in the HFD-ELE and ND groups (114.4±4.0, 82.6±3.3, and 98.8±4.6 μm, respectively). Moreover, the medial thickness in the HFD-ELE group was significantly smaller than that of the ND group (P<0.05).
Thoracic aortic ring medial thickness in rats that received a normal diet (ND), a high-fat diet (HFD) (HFD-control) or a HFD with Eucommia leaf extract (HFD-ELE) (n=8 for each test group). All values represent the means±s.e.m. *P<0.05, **P<0.01, compared with the HFD-control group; #P<0.05 compared with the ND group.
Blood components
The results of the biochemical analyses in blood plasma from the test animals are listed in Table 2. The glucose metabolism markers (plasma glucose, insulin and HbA1c) did not differ significantly among the three study groups. The plasma levels of lipids, including NEFA, triglycerides and total cholesterol, were also not significantly different among the three groups. The results of the evaluations of plasma adipocytokines from the test animals are shown in Figure 4. In the HFD-ELE group, the plasma adiponectin level was significantly higher than those in the ND and HFD-control groups (4.8±0.3, 3.5±0.4 and 3.8±0.2 μg ml−1, respectively; each P<0.01). Significantly higher plasma leptin levels were observed in the HFD-ELE and HFD-control groups than in the ND group (2.4±0.4, 2.7±0.6 and 1.9±0.4 ng ml−1, respectively; P<0.01 or P<0.05). The adiponectin/leptin ratio of the HFD-control group was significantly lower than that of the ND group (1.5±0.1 and 1.9±0.2, respectively; P<0.05). In the HFD-ELE group (2.1±0.2), a significantly elevated adiponectin/leptin ratio was observed compared with the HFD-control group (P<0.01).
Plasma adiponectin and leptin levels, and leptin/adiponectin ratio in rats that received a normal diet (ND), a high-fat diet (HFD) (HFD-control), or a HFD with Eucommia leaf extract (HFD-ELE) (n=8 for each test group). All values represent the means±s.e.m. **P<0.01, compared with the HFD-control group; #P<0.05, ##P<0.01, compared with the ND group.
Discussion
In the present study, we demonstrated that long-term administration of ELE decreased blood pressure and aortic media thickness in WKY rats fed a HFD. Long-term ELE administration in these animals also increased plasma adiponectin levels and the leptin/adiponectin ratio, and decreased body weight and visceral and peripheral fat. To our knowledge, this is the first report showing that administration of ELE may have beneficial effects on blood pressure, aortic hypertrophy, and obesity in a model of early-stage MS.
The present study showed that administration of the HFD for 10 weeks caused a significant increase in the final body weight, WAT weight and SBP in the HFD-control group compared with the ND group. Therefore, it was confirmed that feeding WKY rats on a HFD provided an appropriate rat model of diet-induced early-stage obesity with hypertension with which to investigate the effects of chronic ELE administration on the structural changes to the aorta. In addition, our results also indicated that WKY rats might exhibit MS-like conditions such as obesity with hypertension as a result of a HFD intake.
In this study, ELE intake produced an anti-obesity effect in WKY rats. The HFD-ELE group exhibited significantly reduced body weight gain, a lower final body weight and lower WAT weights, compared with the corresponding values in the HFD-control group. This result was consistent with a previous report that administration of ELE produced an anti-obesity effect in MS rat models receiving a HFD.10 ELE-enhanced metabolic function in several organs, including diminishing ATP production in WAT, accelerating β-oxidation in liver and increasing the use of ketone bodies/glucose in skeletal muscle.18 These effects on lipid metabolism promoted loss of visceral fat and body weight in rats fed a HFD.
For glucose and lipid metabolism measurements, no differences in plasma levels of glucose, insulin and lipids were observed in the three groups. Therefore, the WKY rats fed a HFD showed diet-induced early-stage obesity with hypertension but without insulin resistance, supporting an investigation into the effects of chronic ELE administration on the structural changes in the aorta observed during early obesity stages.
The present study identified a suppressive effect of ELE on the SBP elevation induced by the HFD in WKY rats, consistent with the anti-hypertensive effect of ELE in previous animal and human studies.15, 16 In the HFD-ELE group, significant suppression of medial thickness was also observed in the thoracic aorta. This result reflected the suppression of SBP by ELE because elevated SBP causes increased medial thickness.21
The examination of plasma adipocytokines identified significantly elevated plasma leptin levels in the HFD-control and HFD-ELE groups compared with the ND group. Leptin stimulates the sympathetic nervous system and increases blood pressure.22, 23 Therefore, hyperleptinemia might have contributed to the elevation of SBP observed in the HFD-control group. Moreover, leptin promotes VSMC proliferation, vascular remodeling and hypertrophy,24 and these effects may have contributed to the significant increase in medial thickness in the HFD-control group. However, despite the elevated blood leptin levels in the HFD-ELE group, these rats showed significantly lower SBP and aortic media thickness. In addition, the significant increase in plasma adiponectin levels was observed only in the HFD-ELE group. Adiponectin is an abundant circulating protein secreted by adipose tissue, and has been reported to promote fatty acid metabolism, induce nitric oxide-dependent vasodilation and inhibit smooth muscle cell proliferation.25, 26 Elevation of the adiponectin level in the HFD-ELE group could thus ameliorate the increases in SBP and medial thickness induced by the HFD. In addition, the media was significantly thinner in the HFD-ELE group than in the ND group, suggesting that the higher adiponectin level might also inhibit aging-related increases in medial thickness.
Adiponectin can be used as a marker of subclinical arteriosclerosis,27 and lower serum adiponectin levels have been reported to increase the risk of arteriosclerosis.28 Leptin has also been associated with systemic atherosclerosis,29 where increased serum leptin levels increase the risk of this condition. Therefore, the ratio of leptin to adiponectin has been reported to act as an atherogenic index in obese patients with type 2 diabetes.30 Recently, the adiponectin/leptin ratio has been reported to be a predictive marker of CVD-related events.31 The significantly higher adiponectin/leptin ratio observed in the HFD-ELE group compared with the HFD-control group may indicate a preventive effect of ELE on arteriosclerosis. Early-stage obesity contributes to the development of CVD, including arteriosclerosis.32 Our findings indicate the importance of the improved adiponectin/leptin ratio observed in the HFD-ELE group during early-stage obesity.
ELs contain compounds that include the iridoid glucosides, GEA, asperuloside (ASP) and the caffeic acid derivative chlorogenic acid (CHA).33, 34 It has been reported that the phytochemical components of ELs consisted of 5.47% GEA, 1.75% ASP and 0.35% CHA.35 The anti-hypertensive effect of ELE might be attributed to GEA,36 which is a major active component of EL.33 The observed increase in adiponectin levels and the anti-obesity effect of ELE may be attributed to ASP.10 CHA has been reported to produce significant anti-hypertensive effects in SHR at a dose of ~300 mg kg−1 day−1.37 However, the estimated CHA intake in the HFD-ELE group was only 8.2 mg kg−1 day−1, suggesting that the CHA in ELE might be too small to cause the anti-hypertensive effect. Although the present study demonstrated that ELE administration had anti-hypertensive and anti-obesity effects associated with reduced aortic media thickness and an increased adiponectin/leptin ratio, it did not investigate how active ELE constituents contribute to these effects; therefore, further studies are necessary.
In this study, the HFD diet-induced mild obesity with hypertension, a low adiponectin/leptin ratio and arterial hypertrophy in the WKY rats. These results suggested that the imbalance in adipocytokine secretion might gradually promote arterial morphological changes, such as aortic media hypertrophy, which was an important determinant of arteriosclerosis. In fact, arterial stiffening caused by arterial wall remodeling is used as an early indicator of cardiovascular complications due to metabolic disease.38 Although ELE is a health food and not a drug, the preventive effect of the disease may be attributed to the therapeutic effect of ELE. To our knowledge, the present study is the first to demonstrate that chronic administration of ELE significantly improved aortic media thickness and blood adiponectin levels in early-stage obesity with hypertension in WKY rats receiving a HFD. Therefore, ELE treatment may reduce the risk of CVD by preventing arterial hypertrophy during early-stage obesity with hypertension.
In conclusion, our study showed that long-term administration of ELE reduced weight gain effectively and improved blood pressure, aortic morphology, and blood adiponectin levels in WKY rats receiving a HFD. These data suggest that the supplementation of ELE may prevent aortic media hypertrophy in early-stage obesity and reduce the risk of arteriosclerosis development in the future.
References
World Health OrganizationA Global Brief on Hypertension-Silent Killer, Global Public Health Crisis. WHO Reference Number: WHO/DCO/WHD/2013.2. WHO: Geneva, Switzerland, 2013..
Hirata C, Miyai N, Idoue A, Utsumi M, Hattori S, Iwahara A, Uematsu Y, Shiba M, Arita M . Effect of metabolic syndrome components and their clustering on carotid atherosclerosis in a sample of the general Japanese population. Hypertens Res 2016; 39: 362–366.
Nagai M, Ohkubo T, Murakami Y, Takashima N, Kadota A, Miyagawa N, Saito Y, Nishi N, Okuda N, Kiyohara Y, Nakagawa H, Nakamura Y, Fujiyoshi A, Abbott RD, Okamura T, Okayama A, Ueshima H, Miura K . NIPPON DATA80/90/2010 Research Group. Secular trends of the impact of overweight and obesity on hypertension in Japan, 1980-2010. Hypertens Res 2015; 38: 790–795.
Matsuzawa Y . Adiponectin: identification, physiology and clinical relevance in metabolic and vascular disease. Atheroscler Suppl 2005; 6: 7–14.
Dorresteijn JA, Visseren FL, Spiering W . Mechanisms linking obesity to hypertension. Obes Rev 2012; 13: 17–26.
Fujii M, Ohnishi H, Saitoh S, Akasaka H, Miura T, Mori M . The combination of abdominal obesity and high-sensitivity C-reactive protein predicts new-onset hypertension in the general Japanese population: the Tanno-Sobetsu study. Hypertens Res 2015; 38: 426–432.
Krzesiński P, Stańczyk A, Piotrowicz K, Gielerak G, Uziębło-Zyczkowska B, Skrobowski A . Abdominal obesity and hypertension: a double burden to the heart. Hypertens Res 2016; 39: 349–355.
Guizhou Province Institute for Drug Control and Guizhou Province Chinese Medicine Research Laboratories. A hypertensive clinical study on Eucommia leaves. Chin Med Herbs Res 1978; 8: 59–63.
Namba T, Hattori M, Yie JN, Ma YH, Nomura Y, Kaneko S, Kitamura Y, Koizumi T, Katayama K, Lu W . Studies on Tu-Chung leaves (I) pharmacological effects of the water extract in vivo. Wakan Iyaku Gakkaishi 1986; 3: 89–97.
Fujikawa T, Hirata T, Wada A, Kawamura N, Yamaguchi Y, Fujimura K, Ueda T, Yurugi Y, Soya H, Nishibe S . Chronic administration of Eucommia leaf stimulates metabolic function of rats across several organs. Br J Nutr 2010; 104: 1868–1877.
Metori K, Ohashi S, Takahashi S, Tamura T . Effects of du-zhong leaf extract on serum and hepatic lipids in rats fed a high-fat diet. Biol Pharm Bull 1994; 17: 917–920.
Yen GC, Hsieh CL . Reactive oxygen species scavenging activity of Du-zhong (Eucommia ulmoides Oliv.) and its active compounds. J Agric Food Chem 2000; 48: 3431–3436.
Lee MK, Kim MJ, Cho SY, Park SA, Park KK, Jung UJ, Park HM, Choi MS . Hypoglycemic effect of Du-zhong (Eucommia ulmoides Oliv.) leaves in streptozotocin-induced diabetic rats. Diabetes Res Clin Pract 2005; 67: 22–28.
Jin X, Amitani K, Zamami Y, Takatori S, Hobara N, Kawamura N, Hirata T, Wada A, Kitamura Y, Kawasaki H . Ameliorative effect of Eucommia ulmoides Oliv. leaves extract (ELE) on insulin resistance and abnormal perivascular innervation in fructose-drinking rats. J Ethnopharmacol 2010; 128: 672–678.
Tsukamoto S, Yamaguchi Y, Ueda T, Kajimoto O, Nakagawa Y, Nakagawa S, Kajimoto Y . Hypotensive effects of beverage containing ‘Eucommia leaf glycoside’ on high normal blood pressure and mild hypertensive subjects. Int Symp Eucommia Ulmoides 2007; 1: 47–54.
Hosoo S, Koyama M, Kato M, Hirata T, Yamaguchi Y, Yamasaki H, Wada A, Wada K, Nishibe S, Nakamura K . The restorative effects of Eucommia ulmoides Oliver leaf extract on vascular function in spontaneously hypertensive rats. Molecules 2015; 20: 21971–21981.
Yamori Y, Horie R . Analysis of genetic factors of atherogenesis, separation of normotensive atherogenic rats (NAR). J Jpn Atheroscler Soc 1980; 8: 105–108.
Fujikawa T, Hirata T, Hosoo S, Nakajima K, Wada A, Yurugi Y, Soya H, Matsui T, Yamaguchi A, Ogata M, Nishibe S . Asperuloside stimulates metabolic function in rats across several organs under high-fat diet conditions, acting like the major ingredient of Eucommia leaves with anti-obesity activity. J Nutr Sci 2012; 1: 1–11.
Hirata T, Kobayashi T, Wada A, Ueda T, Fujikawa T, Miyashita H, Ikeda T, Tsukamoto S, Nohara T . Anti-obesity compounds in green leaves of Eucommia ulmoides. Bioorg Med Chem Lett 2011; 21: 1786–1791.
Knight SF, Quigley JE, Yuan J, Roy SS, Elmarakby A, Imig JD . Endothelial dysfunction and the development of renal injury in spontaneously hypertensive rats fed a high-fat diet. Hypertension 2008; 51: 352–359.
Heeneman S, Sluimer JC, Daemen MJ . Angiotensin-converting enzyme and vascular remodeling. Circ Res 2007; 101: 441–454.
Bravo PE, Morse S, Borne DM, Aguilar EA, Reisin E . Leptin and hypertension in obesity. Vasc Health Risk Manag 2006; 2: 163–169.
Simonds SE, Cowley MA . Hypertension in obesity: is leptin the culprit? Trends Neurosci 2013; 36: 121–132.
Ghantous CM, Azrak Z, Hanache S, Abou-Kheir W, Zeidan A . Differential role of leptin and adiponectin in cardiovascular system. Int J Endocrinol 2015; 2015: 534320.
Wang ZV, Scherer PE . Adiponectin, cardiovascular function, and hypertension. Hypertension 2008; 51: 8–14.
Balsan GA, Vieira JL, Oliveira AM, Portal VL . Relationship between adiponectin, obesity and insulin resistance. Rev Assoc Med Bras 2015; 61: 72–80.
Ebrahimi-Mamaeghani M, Mohammadi S, Arefhosseini SR, Fallah P, Bazi Z . Adiponectin as a potential biomarker of vascular disease. Vasc Health Risk Manag 2015; 11: 55–70.
Matsuzawa Y, Funahashi T, Kihara S, Shimomura I . Adiponectin and metabolic syndrome. Arterioscler Thromb Vasc Biol 2004; 24: 29–33.
Beltowski J . Leptin and atherosclerosis. Atherosclerosis 2006; 189: 47–60.
Satoh N, Naruse M, Usui T, Tagami T, Suganami T, Yamada K, Kuzuya H, Shimatsu A, Ogawa Y . Leptin-to-adiponectin ratio as a potential atherogenic index in obese type 2 diabetic patients. Diabetes Care 2004; 27: 2488–2490.
Kappelle PJ, Dullaart RP, van Beek AP, Hillege HL, Wolffenbuttel BH . The plasma leptin/adiponectin ratio predicts first cardiovascular event in men: a prospective nested case-control study. Eur J Intern Med 2012; 23: 755–759.
Ferder L, Inserra F, Martínez-Maldonado M . Inflammation and the metabolic syndrome: role of angiotensin II and oxidative stress. Curr Hypertens Rep 2006; 8: 191–198.
Nakazawa Y . Studies on Functionality and Application of Eucommia leaf to Preservation of Health, PhD thesis Kyushu University, Fukuoka, Japan. 1998.
Tang S, Wang Z, Ma C, Hattori M . Simultaneous determination of ten bioactive constituents in Eucommia ulmoides leaves and Tochu tea products by high-performance liquid chromatography-diode array detector-mass spectrometry (HPLC-DAD-MS). J Trad Med 2008; 25: 112–118.
Hirata T, Ikeda T, Fujikawa T, Nishibe S . The chemistry and bioactivity of Eucommia ulmoides Oliver leaves. Studies Nat Prod Chem 2014; 41: 225–260.
Kawasaki T, Uezono K, Nakazawa Y . Antihypertensive mechanism of food for specified health use: ‘Eucommia leaf glycoside’ and its clinical application. J Health Sci 2000; 22: 29–36.
Suzuki A, Yamamoto N, Jokura H, Yamamoto M, Fujii A, Tokimitsu I, Saito I . Chlorogenic acid attenuates hypertension and improves endothelial function in spontaneously hypertensive rats. J Hypertens 2006; 24: 1065–1073.
Billaud M, Johnstone SR, Isakson BE . Loss of compliance in small arteries, but not in conduit arteries, after 6 weeks exposure to high fat diet. J Cardiovasc Transl Res 2012; 5: 256–263.
Acknowledgements
We thank Dr Sansei Nishibe, Emeritus Professor of Health Sciences University of Hokkaido, for his valuable suggestions and discussions on ELE.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Hosoo, S., Koyama, M., Watanabe, A. et al. Preventive effect of Eucommia leaf extract on aortic media hypertrophy in Wistar-Kyoto rats fed a high-fat diet. Hypertens Res 40, 546–551 (2017). https://doi.org/10.1038/hr.2016.189
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.189
This article is cited by
-
Effects of lactic acid bacteria on antioxidant activity in vitro and aroma component of Eucommia ulmoides tea
Journal of Food Science and Technology (2024)
-
Higher plasma leptin levels are associated with reduced left ventricular mass and left ventricular diastolic stiffness in black women: insights from the Genetic Epidemiology Network of Arteriopathy (GENOA) study
Hypertension Research (2018)
-
How does Eucommia leaf extract prevent smooth muscle cell proliferation induced by high-fat diets at the aortic tunica media?
Hypertension Research (2017)