Abstract
Gallstones have been linked to dyslipidemia, metabolic syndrome and cardiovascular disease. Arterial stiffness is an indicator of subclinical atherosclerosis. The aim of this study was to prospectively examine the relationship between gallstone disease and arterial stiffness progression in 347 men and 454 women. These subjects were followed for 7 years. Arterial stiffness progression was measured based on increases in brachial-ankle pulse wave velocity. Changes in brachial-ankle pulse wave velocity during the study period were significantly greater in patients with gallstones than in subjects without gallstones. After adjusting for multiple risk factors, gallstone disease was found to be a significant and independent predictor of brachial-ankle pulse wave velocity progression (β=0.189; P<0.001). In conclusion, gallstone disease is an independent predictor of arterial stiffness progression, even after adjusting for other cardiovascular risk factors.
Similar content being viewed by others
Introduction
Gallstone disease is one of the most common and costly gastroenterological disorders in western countries. Recent reports have shown that gallstone disease is associated with dyslipidemia, hyperinsulinemia, metabolic syndrome, type 2 diabetes mellitus and cardiovascular disease,1, 2, 3, 4 all of which are related to atherosclerosis.
Arterial stiffness caused by decreased arterial compliance is one of the major signs of vascular aging.5 Elevated arterial stiffness, an index of subclinical atherosclerosis, is an independent predictor of future cardiovascular events in patients with coronary artery disease and cardiovascular morbidity and mortality in patients with hypertension, type 2 diabetes, end-stage renal disease and advanced age.6, 7 Pulse wave velocity (PWV) is a simple, non-invasive and highly reproducible measure of central arterial stiffness and is widely used as an index of arterial stiffness. Brachial-ankle PWV (baPWV) measurements are strongly correlated with aortic PWV measurements.8 Previous reports have shown that increased baPWV is associated with metabolic syndrome, cardiovascular diseases, stroke and renal disease, as well as increased overall mortality.9, 10, 11, 12
To date, no studies have investigated the association between gallstone disease and subclinical atherosclerosis. Therefore, the aim of this study was to determine the relationship between gallstone disease and arterial stiffness progression.
Methods
Study design
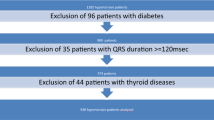
This was a prospective study comprising 600 patients with gallstone disease and 600 subjects without gallstone disease who visited the International Physical Examination and Health Center, Harbin, China, from January 2006 to June 2007. Chinese Health Law requires all employees to undergo annual health examinations. All participants in this study underwent annual heath examinations at the International Physical Examination and Health Center. Patients with gallstone disease and control subjects were randomly selected from a computer-generated randomization list. All participants underwent baPWV measurements as part of their routine health assessments, which also included clinical histories, clinical examinations, 12-lead electrocardiograms, biochemical analyses and abdominal ultrasonography. Patients with a history of anemia, chronic hepatic or renal disease, cancer, cystic fibrosis, Crohn’s disease, gastrectomy, prophylactic cholecystectomy, atrial fibrillation, peripheral arterial disease (ankle-brachial index <0.95) and medical treatment with hormone replacement therapy or lipid-lowering agents were excluded (n=142). We also excluded 171 participants with hypertension, diabetes and cardiovascular diseases at baseline, as well as 34 participants without follow-up data and 52 participants with missing covariate data. Thus, the final study population comprised 801 participants (347 men and 454 women), who were followed-up annually for 7 years. This study was approved by the Institutional Review Board of the Second Hospital of Harbin Medical University. Written informed consent was obtained from each patient.
Clinical examination
All participants underwent a baseline evaluation and provided information regarding their medical history, smoking history, alcohol consumption history, physical activity level and medication history, and underwent a physical examination, laboratory testing and gallbladder ultrasound. Alcohol consumption was defined as having drunk at least 30 g of alcohol per week for 1 year or more. Cigarette smoking was defined as having smoked at least 100 cigarettes in a lifetime. Regular leisure-time physical activity was defined as participating in moderate-to-vigorous activity for 30 min or more per day for 3 days or more per week. Blood pressures were measured using a mercury column sphygmomanometer after 10 min of rest in the supine position. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured twice during each examination, and the mean of each measurement was used for analysis. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2).
Biochemical analyses
Blood specimens were collected following a 12-h fast. Total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), gamma-glutamyl transpeptidase (GGT) and fasting plasma glucose (FPG) levels were measured with standardized laboratory assays (Modular Analytics, Roche, Mannheim, Germany). All measurements were performed within 2 h of sampling.
baPWV measurement
Before being tested, all subjects abstained from caffeine and fasted for at least 4 h. baPWV was measured using an automated device (model MB3000, M&B Electronic Instruments, Beijing, China). baPWV was calculated automatically based on the distance between two arterial recording sites divided by the transit time, according to the formula (L/PTT), where L is the difference between the distance from the heart to the ankle and the distance from the heart to the brachium, and PTT is the pulse transit time between the brachial and tibial arterial waveforms. The mean value of the right and left baPWVs was used for analysis. All measurements were conducted by a single examiner who was blinded to patient clinical data. The reproducibility and validity of measuring baPWV with the above method have been demonstrated previously.13, 14
Diagnostic criteria
An experienced ultrasonographer performed the abdominal ultrasounds using a sonography machine (Voluson E8, GE, Milwaukee, WI, USA) equipped with a 3.5 MHz probe. The ultrasonographer was unaware of the objectives of the study and was blinded to patient laboratory values. Gallstone disease was diagnosed based on the presence of strong intraluminal echoes that were gravity-dependent or attenuated ultrasound transmission (acoustic shadow).
Estimated glomerular filtration rates (eGFRs) were estimated based on creatinine values via the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation as follows: eGFR=141 × min (Scr/k, 1)a × max (Scr/k, 1)1.209 × 0.993age × 1.018 (if female), where Scr is serum creatinine, k is 0.7 for females and 0.9 for males, a is 0.329 for females and 0.411 for males, min indicates the minimum of Scr/k or 1, and max indicates the maximum of Scr/k or 1.
Statistical analysis
All data are expressed as the means±s.d. or as medians (inter quartile ranges) or percentages. Sex, alcohol, smoking, physical activity, hypertension and gallstones were categorized as 0 (absent) or 1 (present) and were analyzed using a χ2-test. Age, BMI, SBP, DBP, TC, LDL-C and eGFR are continuous variables with normally distributed data, and Student's t-test was used for comparisons of these variables between the two groups. FPG, TG, HDL-C and GGT are continuous variables with non-normally distributed data, and the Mann–Whitney U-test was used for comparisons of these variables between the two groups. Univariate analysis was performed using a linear regression model to determine the relationships between changes in baPWV and various clinical parameters. Variables exhibiting a P-value <0.05 in univariate analysis were included in a multivariate linear regression model using a stepwise strategy. Variables such as TG, HDL-C, FPG and GGT were log-transformed to reduce the effects of a skewed data distribution. Two-sided P-values <0.05 were considered significant. All analyses were performed using SPSS (SPSS version 22.0, SPSS, Chicago, IL, USA).
Results
The baseline characteristics of the participants according to gallstones status are shown in Table 1. Higher BMIs, as well as higher TG and physical activity levels and lower HDL-C levels, were observed in patients with gallstone disease than in control subjects. However, age, SBP, DBP, baPWV and heart rate; FPG, TC, LDL-C and GGT levels; and eGFR, sex, smoking history and alcohol history were not different between the two groups.
The 7-year follow-up characteristics of the participants according to gallstone status are shown in Table 2. Patients with gallstone disease exhibited higher baPWVs and BMIs, as well as higher FPG and TG levels and lower HDL-C levels, than control subjects. However, SBP, DBP and heart rate; TC, LDL-C and GGT levels; and eGFR, smoking history, alcohol history and physical activity levels were not significantly different between the two groups.
The changes in baPWV between the baseline and final examinations in patients with and without gallstone disease, after adjusting for confounding covariates, are shown in Figure 1. After adjusting for age, sex, BMI, SBP, DBP and heart rate; HDL-C, LDL-C, TG, TC, GGT and FPG levels; and eGFR, physical activity levels, smoking history and drinking history, the mean baPWV changes among patients with gallstone disease and control subjects were 76.3 (63.0) and 46.0 (49.4) cm s−1, respectively (P<0.001).
Univariate analysis showed that sex, gallstone status, BMI and SBP; TC, HDL-C, LDL-C, and FPG levels; and changes in BMI and eGFR and GGT, HDL-C, TG and FPG levels were significantly associated with changes in baPWV (Table 3). Therefore, all 14 variables were subsequently entered into the multiple linear regression analysis model using a stepwise strategy. The results revealed that gallstones, sex, baseline SBP and changes in TG, HDL-C and GGT levels were associated with changes in baPWV (Table 4). Notably, gallstone disease was found to be a significant determinant of increases in baPWV (β=0.189; P<0.001).
Discussion
In this study, we found that gallstone disease is an independent and significant determinant of changes in baPWV after adjusting for other cardiovascular risk factors.
The mechanism underlying the effects of gallstones on baPWV changes remain unclear. Obesity, dyslipidemia, insulin resistance and metabolic syndrome are closely related to baPWV changes. Gallstone disease is associated with obesity, dyslipidemia, hyperinsulinemia, metabolic syndrome and type 2 diabetes mellitus.1, 2, 3, 4 Obesity increases cholesterol synthesis and secretion into bile.15 A meta-analysis confirmed that obesity is linked to increased levels of C-reactive protein, a marker of inflammation and a predictor of cardiovascular risk.16 Moreover, excess adipose tissue production induced by dysregulated adipokine production has been shown to lead to low-grade chronic inflammation, insulin resistance and endothelial dysfunction, all of which are related to arterial stiffness.17, 18 Obesity, dyslipidemia, insulin resistance and metabolic syndrome all frequently co-occur in the setting of gallstone disease and are considered risk factors for developing the disease.19 Furthermore, hepatic insulin resistance has been shown to facilitate increases in biliary cholesterol secretion in mice and thus represents a crucial link between metabolic syndrome and cholesterol gallstone risk.20 An insulin-resistant phenotype, metabolic syndrome has been linked to increases in the prevalence of gallstone disease,21 as more severe metabolic disease has been shown to increase the risk of developing cholesterol gallstones.22 Insulin resistance decreases intestinal cholesterol absorption, increases cholesterol synthesis and inhibits the expression of Cyp7a1, the enzyme that controls the rate-limiting step of bile acid synthesis.23 Furthermore, hyperinsulinemia increases gallstone formation by increasing hydroxyl-3-methylglutaryl-coenzyme activity and directly stimulating bile acid-independent bile flow into the liver.24, 25 Thus, the co-existence of multiple metabolic disorders contributes to baPWV changes and arterial stiffness development.
Our study has important clinical implications. We showed that gallstone disease is a predictor of baPWV changes and arterial stiffness development. Consistent with our results, a recent study demonstrated that gallstones are associated with increased common carotid intima-media thickness.2 Gallstones may predispose adults to developing arterial stiffness. Clinicians must be proactive with respect to preventing arterial stiffness in patients with gallstones.
Our study had some limitations. First, we could not obtain any information regarding genetic contributions to cholelithiasis. Second, this study lacked information regarding insulin resistance, which is an important risk factor for gallstone disease. Third, this study involved patients from one ethnic group; thus, additional studies involving patients from the other ethnic groups are necessary. Fourth, we used dichotomous values for alcohol history, smoking history and physical activity in our study, which may, therefore, have obscured the association between lifestyle risk factors and arterial stiffness, as some previous reports have noted a J-shaped relationship between alcohol intake and arterial stiffness progression.26, 27
In conclusion, our study showed that gallstone disease was an independent predictor of arterial stiffness progression. Additional large-scale randomized prospective studies are warranted to confirm this relationship.
References
Grundy SM . Cholesterol gallstones: a fellow traveler with metabolic syndrome. Am J Clin Nutr 2004; 80: 1–2.
Kim JH, Ryoo JG, Lee JW, Kim JH . Gallstones are associated with intima-media thickness of common carotid arteries in men. Korean J Fam Med 2014; 35: 136–142.
Nervi F, Miquel JF, Alvarez M, Ferreccio C, Garcia-Zattera MJ, Gonzalez R, Perez-Ayuso RM, Rigotti A, Villarroel L . Gallbladder disease is associated with insulin resistance in a high risk Hispanic population. J Hepatol 2006; 45: 299–305.
Weikert C, Weikert S, Schulze MB, Pischon T, Fritsche A, Bergmann MM, Willich SN, Boeing H . Presence of gallstones or kidney stones and risk of type 2 diabetes. Am J Epidemiol 2010; 171: 447–454.
Redheuil A, Yu WC, Wu CO, Mousseaux E, de Cesare A, Yan R, Kachenoura N, Bluemke D, Lima JA . Reduced ascending aortic strain and distensibility: earliest manifestations of vascular aging in humans. Hypertension 2010; 55: 319–326.
Otsuka K, Fukuda S, Shimada K, Suzuki K, Nakanishi K, Yoshiyama M, Yoshikawa J . Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res 2014; 37: 1014–1020.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K, Koji Y, Hori S, Yamamoto Y . Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002; 25: 359–364.
Satoh H, Kishi R, Tsutsui H . Metabolic syndrome is a significant and independent risk factor for increased arterial stiffness in Japanese subjects. Hypertens Res 2009; 32: 1067–1071.
Tomiyama H, Tanaka H, Hashimoto H, Matsumoto C, Odaira M, Yamada J, Yoshida M, Shiina K, Nagata M, Yamashina A . Arterial stiffness and declines in individuals with normal renal function/early chronic kidney disease. Atherosclerosis 2010; 212: 345–350.
Turin TC, Kita Y, Rumana N, Takashima N, Kadota A, Matsui K, Sugihara H, Morita Y, Nakamura Y, Miura K, Ueshima H . Brachial-ankle pulse wave velocity predicts all-cause mortality in the general population: findings from the Takashima study, Japan. Hypertens Res 2010; 33: 922–925.
Xu L, Jiang CQ, Lam TH, Yue XJ, Cheng KK, Liu B, Jin YL, Zhang WS, Thomas GN . Brachial-ankle pulse wave velocity and cardiovascular risk factors in the non-diabetic and newly diagnosed diabetic Chinese: Guangzhou Biobank Cohort Study-CVD. Diabetes Metab Res Rev 2010; 26: 133–139.
Li RY, Cao ZG, Zhang JR, Li Y, Wang RT . Decreased serum bilirubin is associated with silent cerebral infarction. Arterioscler Thromb Vasc Biol 2014; 34: 946–951.
Li Y, Meng SY, Meng CC, Yu WG, Wang RT . Decreased serum bilirubin is associated with arterial stiffness in men. Nutr Metab Cardiovasc Dis 2013; 23: 375–381.
Stinton LM, Myers RP, Shaffer EA . Epidemiology of gallstones. Gastroenterol Clin North Am 2010; 39: 157–169.
Choi J, Joseph L, Pilote L . Obesity and C-reactive protein in various populations: a systematic review and meta-analysis. Obes Rev 2013; 14: 232–244.
Charakida M, O'Neil F, Masi S, Papageorgiou N, Tousoulis D . Inflammatory disorders and atherosclerosis: new therapeutic approaches. Curr Pharm Des 2011; 17: 4111–4120.
Ikeoka D, Mader JK, Pieber TR . Adipose tissue, inflammation and cardiovascular disease. Rev Assoc Med Bras 2010; 56: 116–121.
Stokes CS, Krawczyk M, Lammert F . Gallstones: environment, lifestyle and genes. Dig Dis 2011; 29: 191–201.
Biddinger SB, Haas JT, Yu BB, Bezy O, Jing E, Zhang W, Unterman TG, Carey MC, Kahn CR . Hepatic insulin resistance directly promotes formation of cholesterol gallstones. Nat Med 2008; 14: 778–782.
Mendez-Sanchez N, Chavez-Tapia NC, Motola-Kuba D, Sanchez-Lara K, Ponciano-Rodriguez G, Baptista H, Ramos MH, Uribe M . Metabolic syndrome as a risk factor for gallstone disease. World J Gastroenterol 2005; 11: 1653–1657.
Chen LY, Qiao QH, Zhang SC, Chen YH, Chao GQ, Fang LZ . Metabolic syndrome and gallstone disease. World J Gastroenterol 2012; 18: 4215–4220.
Pihlajamaki J, Gylling H, Miettinen TA, Laakso M . Insulin resistance is associated with increased cholesterol synthesis and decreased cholesterol absorption in normoglycemic men. J Lipid Res 2004; 45: 507–512.
Nepokroeff CM, Lakshmanan MR, Ness GC, Dugan RE, Porter JW . Regulation of the diurnal rhythm of rat liver beta-hydroxy-beta-methylglutaryl coenzmye A reductase activity by insulin, glucagon, cyclic AMP and hydrocortisone. Arch Biochem Biophys 1974; 160: 387–396.
Storer GB, Topping DL, Trimble RP . Direct stimulation by glucose and insulin of glycogen synthesis in perfused rat liver. FEBS Lett 1981; 136: 135–137.
Sierksma A, Muller M, van der Schouw YT, Grobbee DE, Hendriks HF, Bots ML . Alcohol consumption and arterial stiffness in men. J Hypertens 2004; 22: 357–362.
Sierksma A, Lebrun CE, der Schouw YT v, Grobbee DE, Lamberts SW, Hendriks HF, Bots ML . Alcohol consumption in relation to aortic stiffness and aortic wave reflections: a cross-sectional study in healthy postmenopausal women. Arterioscler Thromb Vasc Biol 2004; 24: 342–348.
Acknowledgements
We wish to thank the staff of the International Physical Examination and Health Center for their help with data collection. This study was supported by the Key Laboratory of Myocardial Ischemia, Harbin Medical University, Ministry of Education, Heilongjiang Province, China.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yu, Kj., Zhang, Jr., Li, Y. et al. Gallstone disease is associated with arterial stiffness progression. Hypertens Res 40, 31–34 (2017). https://doi.org/10.1038/hr.2016.109
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.109
Keywords
This article is cited by
-
Causal effect of gallstone disease on the risk of coronary heart disease or acute myocardial infarction: a Mendelian randomization study
Scientific Reports (2023)
-
Use of lipid parameters to identify apparently healthy men at high risk of arterial stiffness progression
BMC Cardiovascular Disorders (2021)
-
Risk of acute atherosclerotic cardiovascular disease in patients with acute and chronic pancreatitis
Scientific Reports (2021)
-
Sex-specific association between serum immunoglobulin-M and brachial ankle pulse wave velocity in a Chinese population: Danyang Study
Hypertension Research (2019)