Abstract
The ambulatory arterial stiffness index (AASI) has been introduced as an index of arterial function, predicting cardiovascular events. However, treatment-induced changes in AASI are rather equivocal. This study aims to: (i) present the results of treatment-induced changes in AASI in untreated subjects with elevated blood pressure (BP), subjected to antihypertensive treatment for 1 year and (ii) perform a meta-analysis of studies reporting on treatment-induced change in AASI. A total of 104 subjects (mean age 51.4±10.3 years, 62% males, mean follow-up: 13.6±2.4 months) were analyzed. Despite significant reductions in 24-h ambulatory systolic/diastolic BP, pulse pressure and pulse wave velocity (mean change: −15.9±12/−10.4±7.6 mm Hg, −5.4±6.8 mm Hg, −0.7±1.9 m s−1, respectively, all P<0.05), there was no significant change (Follow up—Baseline) in AASI values (mean change: 0.01±0.17, P=not significant). The treatment-induced change in AASI was correlated with baseline AASI (r=−0.61), baseline 24-h pulse pressure (−0.26), treatment-induced change in 24-h pulse pressure (0.26) and in systolic/diastolic nocturnal dipping (−0.25/−0.40, respectively). Meta-analysis of eight trials (n=990) revealed a marginal decrease in AASI with antihypertensive treatment (pooled change: −0.018 (95% confidence interval (CI): −0.033,−0.003)). When the analysis was restricted to data with renin-angiotensin system blockers (n=755, 76% of total), the results did not significantly change (pooled change −0.028 (95% CI −0.048, −0.007)). In conclusion, although AASI is an independent predictor of cardiovascular events, its response to antihypertensive treatment is only marginal and clinically uncertain, which may render its use as a therapeutic target in clinical practice questionable.
Similar content being viewed by others
Introduction
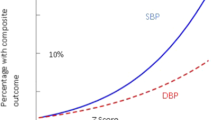
Ambulatory arterial stiffness index (AASI) was introduced in 2006 as a measure of the dynamic relationship between systolic and diastolic blood pressure (BP).1, 2 More specifically, it is derived from the regression slope of diastolic on systolic BP during 24-h ambulatory BP monitoring.1, 2 Although it was initially regarded as an index of arterial stiffness, subsequent studies revealed that it is a more composite index of arterial function determined by several arterio-ventricular coupling factors.3, 4 More importantly, a large number of studies have shown AASI to be associated with several indices of arterial damage, including arterial stiffness, and to independently predict cardiovascular events, mainly stroke.5, 6, 7, 8
The superiority of ambulatory BP monitoring over clinic BP in terms of diagnostic and prognostic value is well established and recent guidelines support its increasing use in clinical practice.9, 10 This led to an initial enthusiasm about the broad use of AASI in clinical practice as an additional piece of information which is easily derived from routine ambulatory BP monitoring and has independent prognostic value.
However, doubts have been raised regarding the response of AASI to antihypertensive treatment, an issue that has not been systematically addressed. Some studies have reported a significant decline in AASI values with antihypertensive treatment,11, 12 whereas others have failed to show any difference.13, 14 Some of these studies have implied that the response of AASI to treatment may be drug-class-specific with the largest response seen with the blockers of the renin-angiotensin system.11 However, several issues regarding the response profile of AASI by antihypertensive treatment remain uncertain.
This study aimed to: (i) present the data of a prospective study regarding treatment-induced changes in AASI in subjects receiving antihypertensive treatment for 1 year15 and (ii) perform a systematic review and meta-analysis of relevant studies on the response of AASI to antihypertensive treatment.
Methods
Prospective study
A prospective randomized study was conducted in untreated subjects that compared the BP reduction, the hypertension control rate and the regression of target-organ damage achieved after 12 months of treatment based either on home BP monitoring alone or on office BP measurement combined with occasional use of ambulatory BP monitoring.15 Details for the study protocol and patients’ characteristics have been published previously.15, 16 In brief, adults aged >30 years who fulfilled the study entry criteria were enrolled and participated in a 2-week run-in period during which they were evaluated with the following: (i) measurements of BP in the clinic, at home and with ambulatory monitoring; (ii) laboratory investigations (full blood count and routine blood biochemistry); and (iii) assessment of preclinical target-organ damage (electrocardiogram, echocardiography, carotid–femoral pulse wave velocity and urinary albumin excretion). Participants who fulfilled the study selection criteria and had a BP above target were subjected to antihypertensive treatment using a stepwise add-on treatment strategy until preset BP goals were reached. Treatment was initiated with full-dose angiotensin receptor blocker (irbesartan 300 mg, telmisartan 80 mg or valsartan 320 mg once daily) (step 1). Amlodipine 5 mg once daily was added as a second drug (step 2) and titrated to 10 mg once daily if required (step 3). In case of amlodipine-induced ankle edema, the dose was reduced or the drug discontinued according to the intensity of edema. If the BP goal was not reached, hydrochlorothiazide 12.5 mg once daily was added (step 4) and titrated to 25 mg once daily if required (step 5). Carvedilol 12.5 mg twice daily was added as a fourth drug (step 6) and titrated to 25 mg twice daily according to BP levels (step 7). Treatment initiation and titration were based on either clinic BP and ambulatory BP measurement or home BP measurement alone, with participants randomized to the two treatment strategy arms. After 12 months of treatment, the participants underwent the same evaluation as at baseline. Ambulatory BP was monitored on a routine workday at 20-min intervals for 24 h using validated oscillometric devices: SpaceLabs 90207 or 90217 (Healthcare, Issaquah, WA, USA) or Microlife WatchBP O3 (Microlife AG, Widnau, Switzerland). Each individual used the same type of ambulatory BP monitor throughout the study. Ambulatory BP recordings with <20 valid awake and 7 asleep readings were repeated.
The regression slope of diastolic on systolic BP was computed for each individual on the basis of ambulatory BP readings and AASI was defined as one minus the respective regression slope.1, 2 Symmetrical AASI was calculated using the formula 1−(1−AASI)/r, with r being the correlation coefficient between systolic and diastolic ambulatory BP.17
Analysis
Participants with complete 24-h ambulatory BP and pulse wave velocity evaluations both at baseline and at the end of follow-up were analyzed. The Kolmogorov–Smirnov test was used to check the normality of the distribution of the study samples. Student’s paired t-test was used to compare BP and AASI values at baseline and at the end of the study, and the Wilcoxon’s test was used for paired comparisons of non-parametric data. Pearson correlations were used to assess the relationship between treatment-induced changes in AASI and the corresponding changes in BP and pulse wave velocity. Stepwise multivariate regression was performed for the identification of independent determinants of treatment-induced change in AASI. Statistical analysis was performed using the IBM SPSS Statistics (Version 21.0., IBM Corp, Armonk, NY, USA). A P-value of 0.05 was considered statistically significant.
Meta-analysis
Search strategy
A systematic literature search was performed by a single investigator (AK) at PubMed during the period from 2006 (when AASI was introduced) to August 2014, using the keywords: ‘ambulatory arterial stiffness index’ and ‘treatment’.
Selection criteria, data extraction and statistical analysis
By taking the PRISMA guidelines into consideration (www.prisma-statement.org), a systematic review was performed of articles written in English and presenting data from prospective studies on antihypertensive treatment-induced changes in AASI. Eligible studies were those that examined AASI values before and after antihypertensive treatment in untreated subjects, or in treated patients who were subjected to wash-out period, or were subjected to treatment change or up-titration. In case of randomized placebo studies, only the treated group was included in the analysis.
Meta-analysis was performed based on aggregate data from selected studies (not individual patients’ data). In one case, the exact aggregate AASI values were retrieved from the authors as these were contained in a graph.18 Average values pooled by random effects meta-analysis were estimated for treatment-induced changes in AASI. Random rather than fixed effects models were performed as more appropriate for balancing weights across large and small studies and to allow for variation in study effects, owing to the expected dispersion in the effect size across studies (attributed to factors such as age, ethnicity, methodology, different treatment strategies, duration of treatment, etc). A standard formula for combining subgroup means and s.ds. for AASI was performed where necessary.19 Publication bias was evaluated by means of Begg’s funnel plots and Begg’s and Egger’s statistical tests.20, 21 Meta-analysis and meta-regression were performed using the STATA SE version 11.2 (StataCorp, College Station, TX, USA). Heterogeneity was tested using I2 statistics. Two-sided P-values <0.05 were considered significant. Data are given as mean±s.d., unless stated otherwise.
Results
Prospective study
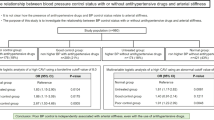
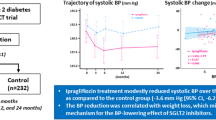
A total of 104 subjects had complete data for the purpose of this study (mean age 51.4±10.3 years, 62% males, body mass index: 28.9±4.3 kg m−2, mean follow-up: 13.6±2.4 months). Despite significant decreases in 24 h BP (systolic, diastolic and pulse pressure) as well as in pulse wave velocity with the antihypertensive treatment, there were no significant changes in AASI values (Table 1). The change in AASI values (Follow up—Baseline) was correlated with baseline AASI, baseline pulse pressure, the treatment-induced change in pulse pressure and with the change in nocturnal dipping; however, no association was observed with the treatment-induced change in pulse wave velocity (Table 2). Only subjects with baseline AASI values at the upper quartile (average baseline AASI: 0.55±0.06) exhibited a significant decrease in AASI with antihypertensive treatment (mean change: −0.10±0.17, P<0.01). Stepwise multivariate regression analysis using the treatment-induced change in AASI as the dependent variable and all the variables showing significant correlations with this change as independent variables, revealed that baseline AASI values (beta coefficient±s.e.: −0.70±0.09) and the change in diastolic nocturnal dipping (−0.63± 0.13) were the sole determinants of the variation of the change in AASI (R2=0.70). Likewise, the treatment-induced change in symmetrical AASI was determined (R2=0.66) by baseline symmetrical AASI values (−0.58±0.08), treatment-induced change in pulse pressure (0.006±0.002) and diastolic nocturnal dipping (−0.37±0.13).
Meta-analysis
Seventy-eight studies were identified by the original search. Seven of them satisfied the inclusion criteria and were included in the analysis along with the data of this prospective study.11, 12, 13, 14, 18, 22, 23 Their characteristics are shown in Table 3. The rest of the articles were irrelevant or did not satisfy the aforementioned inclusion criteria.
The meta-analysis of these eight studies (n=990) revealed a pooled change (Follow up—Baseline) in AASI of −0.018 (−0.033, −0.003) (Figure 1). Both Begg’s and Egger’s tests did not identify any publication bias (P values non-significant). Meta-regression analysis did not identify any significant determinants (baseline age, baseline AASI, duration of treatment) of the AASI change, although there was a trend for higher differences with higher baseline AASI values (Figure 2). When the analysis was performed by including only data for patients receiving antihypertensive treatment based on angiotensin-renin system blockers (n=755, 76% of total), the pooled difference was −0.028 (−0.048, −0.007).
Discussion
There is considerable evidence supporting the prognostic significance of AASI in terms of cardiovascular morbidity and mortality.5, 6, 7, 8 Although this index is promptly derived from routine 24-h ambulatory BP monitoring, its use in everyday clinical practice is restricted by the lack of data regarding its usefulness as a therapeutic measure.8 This study investigated the response of AASI to antihypertensive treatment by means of a 1-year prospective study and a meta-analysis of relevant data. The main findings are that AASI: (i) presents only marginal decrease with antihypertensive treatment which raises doubts about its clinical utility in clinical practice and (ii) there seems to be no association between treatment-induced changes in AASI and in arterial stiffness.
In this 1-year study, antihypertensive treatment based on a renin-angiotensin system blocker failed to decrease AASI values. This is in line with previously published studies using similar therapeutic regimens based on a renin-angiotensin system blocker for comparable durations of treatment.13, 14 Moreover, the change in AASI values appeared to be associated with baseline AASI and pulse pressure values, as well as with the treatment-induced change in pulse pressure, and with the change in nocturnal dipping; however, no association was observed with the change in pulse wave velocity. Moreover, subjects with baseline AASI values at the upper quartile exhibited a significant decrease with the antihypertensive treatment. This observation might imply that the treatment effect becomes evident only in subjects with higher AASI values indicating a more serious derangement in arterial function. The association between the changes in AASI and nocturnal dipping confirms previous observations on the dependence of AASI on the nighttime BP change.3, 17 Indeed, a previous study in untreated hypertensive subjects revealed that AASI is inversely related with nocturnal systolic and mainly diastolic BP reduction.3 In line with these data, the present findings demonstrated an inverse association of the treatment-induced change in AASI with the change in nocturnal diastolic BP dipping. However, even when symmetrical AASI, an index less dependent on the nocturnal BP fall was used, no significant treatment effect could be observed.24 More specifically, symmetrical AASI was less dependent on the change in diastolic BP dipping (although not devoid of it), but this advantage might be moderated by other characteristics such as its inferiority compared with AASI in terms of reproducibility.25 It should be mentioned that, in this study, a significant decrease in pulse wave velocity with antihypertensive treatment was observed. Indeed, pulse wave velocity represents an accurate index of arterial stiffness, can be measured noninvasively with different techniques and several studies have established the positive effects of antihypertensive treatment on this index.13, 14, 26, 27 The findings of this study that there was a significant decrease in pulse wave velocity with treatment and there was no association between the treatment-induced change in pulse wave velocity and AASI indicate that AASI monitoring during antihypertensive treatment appears not to offer accurate information on the change in the arterial stiffness.
Previous studies have provided contradictory results regarding the response of AASI to antihypertensive treatment. Two large studies have failed to show a significant decrease in AASI values with 6 or 12 months of treatment, which is in line with the present study,13, 14 whereas Andreadis et al.11 showed a significant decrease only in those subjects receiving a renin-angiotensin system blocker. When all the studies were examined in the context of the meta-analysis, a significant decrease in AASI values was observed. However, this decrease, which was in the range of 0.018, was only marginal with the upper 95% confidence interval reaching the value of zero. Thus, the response does not appear to be helpful in individualized monitoring of treatment in clinical practice.
The marginal response of AASI to antihypertensive treatment might imply that the treatment effect may be dependent on several factors determining heterogeneous responses. Indeed, several parameters such as baseline AASI values, duration and severity of arterial damage, duration and characteristics of treatment might influence the occurrence of treatment effects. However, there was no change in the results of the meta-analysis when data only from subjects treated with blockers of the renin-angiotensin system were included. In addition, the baseline AASI values, treatment duration and participants’ age did not appear to have a predictive role in the treatment-induced change in AASI. Although the trend towards larger decreases in subjects with higher baseline AASI values might imply that the treatment effect is related to the severity of the arterial dysfunction, it might also be due to regression to the mean.
The findings of the present meta-analysis should be interpreted in the context of some methodological weaknesses. The main limitation is that there was a considerable heterogeneity in the included studies, regarding patients’ characteristics, variation in ambulatory BP-monitoring protocols, and differences in therapeutic regimens, which may have affected the results. Another issue to be commented is that the oscillometric devices estimate systolic and diastolic BP through algorithms. Although the accuracy in this estimation has been validated for most of the used ambulatory BP monitors, as systolic and diastolic BP are not independently measured, their relationship is partly determined by the algorithm used for their determination, which in turn might influence the AASI estimation.
In conclusion, although AASI might offer independent prognostic information, the available evidence does not appear to support its use to monitor the effects of antihypertensive drug treatment.
References
Dolan E, Li Y, Thijs L, McCormack P, Staessen JA, O'Brien E, Stanton A . Ambulatory arterial stiffness index: rationale and methodology. Blood Press Monit 2006; 11: 103–105.
Li Y, Wang JG, Dolan E, Gao PJ, Guo HF, Nawrot T, Stanton AV, Zhu DL, O'Brien E, Staessen JA . Ambulatory arterial stiffness index derived from 24-hour ambulatory blood pressure monitoring. Hypertension 2006; 47: 359–364.
Schillaci G, Parati G, Pirro M, Pucci G, Mannarino MR, Sperandini L, Mannarino E . Ambulatory arterial stiffness index is not a specific marker of reduced arterial compliance. Hypertension 2007; 49: 986–991.
Westerhof N, Lankhaar JW, Westerhof BE . Ambulatory arterial stiffness index is not a stiffness parameter but a ventriculo-arterial coupling factor. Hypertension 2007; 49: e7.
Dolan E, Thijs L, Li Y, Atkins N, McCormack P, McClory S, O'Brien E, Staessen JA, Stanton AV . Ambulatory arterial stiffness index as a predictor of cardiovascular mortality in the Dublin Outcome Study. Hypertension 2006; 47: 365–370.
Hansen TW, Staessen JA, Torp-Pedersen C, Rasmussen S, Li Y, Dolan E, Thijs L, Wang JG, O'Brien E, Ibsen H, Jeppesen J . Ambulatory arterial stiffness index predicts stroke in a general population. J Hypertens 2006; 24: 2247–2253.
Kikuya M, Staessen JA, Ohkubo T, Thijs L, Metoki H, Asayama K, Obara T, Inoue R, Li Y, Dolan E, Hoshi H, Hashimoto J, Totsune K, Satoh H, Wang JG, O'Brien E, Imai Y . Ambulatory arterial stiffness index and 24-hour ambulatory pulse pressure as predictors of mortality in Ohasama, Japan. Stroke 2007; 38: 1161–1166.
Kollias A, Stergiou GS, Dolan E, O'Brien E . Ambulatory arterial stiffness index: a systematic review and meta-analysis. Atherosclerosis 2012; 224: 291–301.
O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y, ; European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013; 31: 1731–1768.
National Institute for Health and Clinical Excellence (NICE) Hypertension. The Clinical Management of Primary Hypertension in Adults. Clinical Guideline 127. 2011 http://www.nice.org.uk/guidance/ CG127. Accessed 9 September 2014.
Andreadis EA, Sfakianakis ME, Tsourous GI, Georgiopoulos DX, Fragouli EG, Katsanou PM, Tavoularis EI, Skarlatou MG, Marakomichelakis GE, Ifanti GK, Diamantopoulos EJ . Differential impact of angiotensin receptor blockers and calcium channel blockers on arterial stiffness. Int Angiol 2010; 29: 266–272.
Andreadis EA, Angelopoulos ET, Kolyvas GN, Agaliotis GD, Mousoulis CG, Mousoulis GP . The effect of aliskiren versus ramipril-based treatment on the Ambulatory Arterial Stiffness Index in hypertensive patients. Int Angiol 2014; 33: 78–83.
Jin Y, Thijs L, Richart T, Li Y, Dolan E, Wang JG, Protogerou A, O'Brien E, Staessen JA, Safar ME . Responses of the ambulatory arterial stiffness index and other measures of arterial function to antihypertensive drugs. Hypertens Res 2011; 34: 489–495.
Matsui Y, O'Rourke MF, Ishikawa J, Shimada K, Kario K . Association of changes in ambulatory arterial stiffness index and pulse wave velocity during antihypertensive treatment: the J-CORE study. Am J Hypertens 2012; 25: 862–868.
Stergiou GS, Karpettas N, Destounis A, Tzamouranis D, Nasothimiou E, Kollias A, Roussias L, Moyssakis I . Home blood pressure monitoring alone vs combined clinic and ambulatory measurements in following treatment-induced changes in blood pressure and organ damage. Am J Hypertens 2014; 27: 184–192.
Karpettas N, Destounis A, Kollias A, Nasothimiou E, Moyssakis I, Stergiou GS . Prediction of treatment-induced changes in target-organ damage using changes in clinic, home and ambulatory blood pressure. Hypertens Res 2014; 37: 543–547.
Gavish B, Ben-Dov IZ, Bursztyn M . Linear relationship between systolic and diastolic blood pressure monitored over 24 h: assessment and correlates. J Hypertens 2008; 26: 199–209.
Jekell A, Malmqvist K, Wallén NH, Mörtsell D, Kahan T . Markers of inflammation, endothelial activation, and arterial stiffness in hypertensive heart disease and the effects of treatment: results from the SILVHIA study. J Cardiovasc Pharmacol 2013; 62: 559–566.
Higgins JP, Green S . Cochrane handbook for systematic reviews of interventions. Version 5.1.0 The Cochrane Collaboration: Oxford. 2011.
Begg CB, Mazumdar M . Operating characteristics of a rank correlation test for publication bias. Biometrics 1994; 50: 1088–1101.
Egger M, Davey Smith G, Schneider M, Minder C . Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634.
Litvin AY, Sukmarova ZN, Elfimova EM, Aksenova AV, Galitsin PV, Rogoza AN, Chazova IE . Effects of CPAP on ‘vascular’ risk factors in patients with obstructive sleep apnea and arterial hypertension. Vasc Health Risk Manag 2013; 9: 229–235.
Boesby L, Elung-Jensen T, Strandgaard S, Kamper AL . Eplerenone attenuates pulse wave reflection in chronic kidney disease stage 3-4—a randomized controlled study. PLoS One 2013; 8: e64549.
Ben-Dov IZ, Gavish B, Kark JD, Mekler J, Bursztyn M . A modified ambulatory arterial stiffness index is independently associated with all-cause mortality. J Hum Hypertens 2008; 22: 761–766.
Stergiou GS, Kollias A, Rarra VC, Roussias LG . Ambulatory arterial stiffness index: reproducibility of different definitions. Am J Hypertens 2010; 23: 129–134.
Ring M, Eriksson MJ, Zierath JR, Caidahl K . Arterial stiffness estimation in healthy subjects: a validation of oscillometric (Arteriograph) and tonometric (SphygmoCor) techniques. Hypertens Res 2014; 37: 999–1007.
Seidlerová J, Filipovský J, Mayer O, Wohlfahrt P, Cífková R . Positive effects of antihypertensive treatment on aortic stiffness in the general population. Hypertens Res 2014; 37: 64–68.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kollias, A., Rarra, V., Karpettas, N. et al. Treatment-induced changes in ambulatory arterial stiffness index: one-year prospective study and meta-analysis of evidence. Hypertens Res 38, 627–631 (2015). https://doi.org/10.1038/hr.2015.44
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.44
Keywords
This article is cited by
-
Second derivative of the finger photoplethysmogram and cardiovascular mortality in middle-aged and elderly Japanese women
Hypertension Research (2017)
-
Cardiovascular calcification and subcortical bone demineralization in hypertension
Hypertension Research (2017)
-
New approach to arterial stiffness: BP-independent local carotid stiffness
Hypertension Research (2017)
-
Influence of the central-to-peripheral arterial stiffness gradient on the timing and amplitude of wave reflections
Hypertension Research (2016)
-
Ambulatory arterial stiffness in chronic kidney disease: a methodological review
Hypertension Research (2016)