Abstract
Assessing an individual’s salt intake is necessary for providing guidance with respect to salt restriction. However, the methods that exist for assessing salt intake have both merits and limitations. Therefore, the evaluation methods should be selected for their appropriateness to the patients and the environment of the medical facilities. The purpose of the present study was to investigate the validity of a brief self-administered diet-history questionnaire (BDHQ) by comparing the responses with 24-h urinary salt excretion. A total of 136 hypertensive outpatients (54 men and 82 women) were included in this study. All subjects were given the BDHQ and performed 24-h home urine collection. The energy-adjusted salt intake as assessed by the BDHQ was 12.3 (95% confidence interval: 11.8–12.9) g per day, and the urinary salt excretion evaluated by 24-h urinary collection was 9.0 (8.4–9.5) g per day. The energy-adjusted salt intake assessed by the BDHQ correlated significantly with the urinary salt excretion evaluated by 24-h urinary collection (r=0.34, P<0.001). In conclusion, the estimated salt intake evaluated by the BDHQ weakly, but significantly, correlated with 24-h urinary salt excretion. In clinical practice, it seems important to utilize both methods to assess an individual’s salt intake in order to provide adequate guidance for salt restriction.
Similar content being viewed by others
Introduction
Salt restriction is the most important lifestyle modification for managing hypertension.1, 2, 3, 4 However, we previously reported that there is only a slight difference in urinary salt excretion between individuals with and without awareness of salt reduction.5 Because awareness of salt reduction does not always lead to an actual salt restriction, it is necessary to evaluate an individual’s salt intake. Several methods have been proposed to assess salt intake, and each method has both merits and limitations.6 Measurement of urinary salt excretion via 24-h urine collection or a dietitian-administered survey on dietary content has been recommended as a reliable method, but these methods are complicated and therefore unsuitable for primary care clinic.6 Sasaki et al.7 developed a brief self-administered diet-history questionnaire (BDHQ) that requires 15–20 min to answer. The BDHQ results correlated with an assessment based on dietary records, suggesting that the BDHQ is useful as a tool for providing salt-reduction guidance.8
To our knowledge, however, the validity of the BDHQ based on comparisons with 24-h urinary salt excretion, particularly in hypertensive patients, has not been confirmed. In the present study, we compared the dietary intake levels of salt estimated by the BDHQ and the urinary excretion levels measured by 24-h urine collection in hypertensive patients.
Methods
We undertook the BDHQ and 24-h home urine collection in 157 hypertensive outpatients who visited the National Kyushu Medical Center, Fukuoka, Japan, between October 2011 and April 2012. The BDHQ was administered on the day on which the patients submitted their 24-h urine collection samples. The samples were collected by using a partition cup (proportional sampling method), which collects a 1/50 portion of the 24-h urine. If the 24-h creatinine excretion was within ±30% of the estimated values, the urine collection was considered successful. Patients who failed to complete the 24-h urine collection were excluded from further analysis to ensure the accuracy of the study. After the exclusion of patients who failed to complete the 24-h urine collection and could not retry within 30 days, 136 hypertensive outpatients (54 men and 82 women) were enrolled in the present study.
Doctors used a sphygmomanometer to measure the blood pressure while the patients were seated quietly. Information on the number of antihypertensive medications the patients were taking was obtained at the clinical visit during which the patients responded to the BDHQ.
Estimation of salt intake from the BDHQ
The BDHQ is a four-page, fixed-portion questionnaire that asks about the consumption frequency of the selected food items to estimate the dietary intake of 58 food and beverage items in the preceding month. The food and beverage items listed on the BDHQ were selected to represent foods commonly consumed in Japan, mainly from a food list used in the National Health and Nutrition Survey of Japan. The BDHQ has information on habitual intake, dietary patterns, cooking and seasoning. Although it is ideal to evaluate using crude values, they do not reflect the quantity of the selected foods and thus are likely to underestimate actual salt intake. Therefore, we also used values adjusted by the age- and sex-specific general Japanese standard energy intake.7
Statistical analysis
Values are expressed as the mean±s.d. or mean (95% confidence interval). The sex differences in the mean values of salt intake and urinary excretion were tested using a t-test. The validity of these was examined by using Pearson correlation coefficients. All statistical analyses were performed by using the SAS statistical software, version 9.2 (SAS Institute, Cary, NC, USA). P values of <0.05 were considered statistically significant.
Results
The mean values or frequencies of clinical characteristics in the subjects are shown in Table 1. The success rate of urine collection, based on our criteria, was 86.6% (136 out of the 157 subjects), and there was no difference in age between the success and failure groups. In this study, 39.7% of patients were males, and the mean age was 68.1±11.3 years. The number of antihypertensive medications being taken by each patient was 2.1±1.0 drugs.
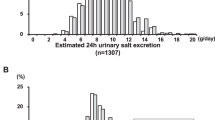
Table 2 shows the salt intake as assessed by the BDHQ and urinary salt excretion evaluated by 24-h urinary collection. The salt intake as estimated by the BDHQ was generally higher than the urinary salt excretion evaluated by 24-h urinary collection. The crude salt intake assessed by the BDHQ was 10.5 (95% confidence interval: 10.0–11.2) g per day (men 11.3 (10.0–12.5) g per day, women 10.1 (9.4–10.8) g per day) and the energy-adjusted value was 12.3 (11.8–12.9) g per day. The energy-adjusted salt intake was widely distributed, ranging from 6.0 to 21.3 g per day (Figure 1). The energy-adjusted salt intake was significantly higher in males than in females (14.1 (13.3–14.9) vs. 11.2 (10.6–11.8) g per day, P<0.001).
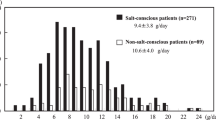
By contrast, the urinary salt excretion evaluated by 24-h urinary collection was 9.0 (8.4–9.5) g per day (range: 2.0–17.8 g per day). Again, urinary salt excretion was significantly higher in males than in females (10.1 (9.2–10.9) vs. 8.3 (7.6–9.0) g per day, P<0.001) (Figure 2). We also analyzed the characteristics of the cases that were under and over the 95th percentile. The patients under the 95th percentile of salt intake estimated by the BDHQ or urinary salt excretion had a lower body mass index. The patients over the 95th percentile of urinary salt excretion were younger.
We also examined the correlation between salt intake and urinary salt excretion. The energy-adjusted salt intake assessed by the BDHQ showed a significant positive correlation with urinary salt excretion (r=0.34, P<0.001, Figure 3).
Discussion
The present study demonstrated that salt intake evaluated by the BDHQ correlates with urinary salt excretion evaluated by 24-h urinary collection in hypertensive patients. No prior investigation has evaluated the correlation between salt intake evaluated by the BDHQ and 24-h urinary salt excretion in hypertensive patients.
One previous study examined the relationship between dietary intake of Na assessed by a self-administered diet-history questionnaire (DHQ), which estimated the dietary intake of 150 food and beverage items, and urinary sodium excretion measured by 24-h urine collection.9 The authors reported that DHQ had a reasonable ability to estimate sodium intake in females but that the sodium intake results were not conclusive. Although the BDHQ is a simplified version of the DHQ, its validity seems equivalent to that of the DHQ because it accurately reflects foods that are commonly consumed in Japan.10 The BDHQ is a questionnaire for evaluating the dietary content over a period of 1 month, which may explain the present observation that the salt intake assessed by the BDHQ weakly correlated with urinary salt excretion measured by 24-h urine collection for a single day. Regarding the method used to collect 24-h urine, in the present study urine samples were collected using a partition cup. Assessment of urinary salt excretion via total urine collection is surely considered the ‘gold standard.’ However, even when total urine collection is used, the success rate for collecting 24-h urine completely is not 100%. Indeed, in the INTERSALT study, 5% of the subjects were reported to have failed to collect all their urine.11 We provided the subjects with precise instructions on how to use the partition cup, and the success rate, as judged from estimated 24-h urinary creatinine excretion, was 88%. There was no significant difference between the success rates of old (aged 65 and over) and young subjects in the present study (88.1 vs. 87.5%, respectively; P=0.91). Considering the merits of the partition cup method, such as its portability, we believe that this method is applicable in clinical practice. With regard to the validity of the partition cup method, Tochikubo et al.12 reported that the correlation coefficient between urinary sodium excretions measured by total urine collection and those obtained by using the partition cup method was high (r=0.98).
We previously investigated the variability of urinary salt excretion in hypertensive and normotensive subjects using a self-monitoring device that estimates 24-h urinary salt excretion on the basis of night-time urine.13 The mean salt excretion for 30 days was 8.4±1.5 g per day, and the range (maximum–minimum value) was 5.5±2.1 g per day. Other studies have also shown a long-term chronological change or variability of salt excretion following repeated mesurements.14, 15, 16, 17 Wakai18 reviewed the validity of dietary questionnaires in assessing energy and nutrient intake and showed that the medians of the coefficients for energy and nutrients obtained in dietary records and questionnaires ranged from 0.31 to 0.56. Given this evidence of the variability of salt intake, the present observation that salt intake as assessed by the BDHQ significantly, but weakly, correlated with urinary excretion measured by 24-h urine collection seems reasonable.
In the present study, salt intake estimated by the BDHQ was generally higher than urinary salt excretion evaluated by 24-h urinary collection. It is known that the entire volume of ingested salt is not excreted in urine and that 10–20% is lost in the digestive tract or as sweat.5 Therefore, it may be reasonable that urinary salt excretion is lower than the actual salt intake.
In a clinical practice, urinary salt excretion is preferable for evaluating the target of less than 6 g of salt per day because frequent administration of the BDHQ would be impractical. However, BDHQ is quite effective for investigating dietary patterns and providing patients with specific instructions for salt restriction. Thus, we believe that more detailed guidance for salt restriction can be provided by using a combination of the urinary salt excretion assessment and the information obtained from dietary questionnaires such as the BDHQ.
A limitation of the present study should be noted. Assessment of salt intake by the BDHQ may not be fully valid because the algorithm used to calculate food intake from the BDHQ was written by using unpublished observations, leading to potentially insufficient reliability.19 However, it is obvious that the advantage of the BDHQ is the disclosure of foods or dietary habits that lead to excessive salt intake. Doctors or medical staff can therefore provide adequate guidance for reducing salt intake based on a patient’s responses to the BDHQ.
In conclusion, to our knowledge, this is the first study to examine the relationship between salt intake evaluated by the BDHQ and urinary salt excretion evaluated by 24-h urinary collection in hypertensive subjects.
To achieve effective guidance for reducing salt intake, it seems important to utilize both methods to assess an individual’s salt intake.
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo J, Joseph L, Jones DW, Materson BJ, Oparil S, Wright J, Jackson T, Roccella EJ, Committee. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA 2003; 289: 2560–2572.
National High Blood Pressure Education Program Working Group. National High Blood Pressure Education Program Working Group report on primary of hypertension. Arch Intern Med 1993; 153: 186–208.
Whelton P, He J, Appel L, Cutler J, Havas S, Kotchen T, Roccella E, Stout R, Karimbakas J, Committee. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA 2002; 288: 1882–1888.
Ohta Y, Tsuchihashi T, Kiyohara K, Oniki H . High salt intake promotes a decline in renal function in hypertensive patients: a 10-year observational study. Hypertens Res 2013; 36: 172–176.
Ohta Y, Tsuchihashi T, Ueno M, Kajioka T, Onaka U, Tominaga M, Eto K . Relationship bteween the awareness of salt restriction and actual salt intake in hypertensive patients. Hypertens Res 2004; 27: 243–246.
Tsuchihashi T, Kai H, Kusaka M, Kawamura M, Matsuura H, Miura K, Ando K, Maruyama S, Hayabuchi H, Takagi Y, Nakahigashi N, Sato T, Kawano Y . [Scientific statement] Report of the Salt Reduction Committee of the Japanese Society of Hypertension (3) Assessment and application of salt intake in the management of hypertension. Hypertens Res 2013; 36: 1026–1031.
Sasaki S, Yanagibori R, Amano K . Self-administered diet hitory quetionnaire developed for health education: a relative validation of the test-version by comparison with 3-day diet record in women. J Epidemiol 1998; 8: 203–215.
Kobayashi S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C . Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr 2011; 14: 1200–1211.
Sasaki S, Yanagibori R, Amano K . Validity of a self administered diet history questionnaire for assessment of sodium and potassium–comparison with single 24-hour urinary excretion-. Jpn Circ J. 1998; 62: 431–435.
Kobayashi S, Honda S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C . Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol 2012; 22: 151–159.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. BMJ 1988; 297: 319–328.
Tochikubo O, Uneda S, Kaneko Y . Simple portable device for sampling a whole day's urine and its application to hypertensive outpatients. Hypertension 1983; 5: 270–274.
Ohta Y, Tsuchihashi T, Eri M, Onaka U . Usefulness of self-monitoring of urinary salt excretion in hypertensive patients. Clin Exp Hypertens 2009; 31: 690–697.
Ohta Y, Tsuchihashi T, Onaka U, Eto K, Mitsuhiro. T, Ueno M . Long-term compliance with salt restriction in Japaniese hypertensive patients. Hypertens Res 2005; 28: 953–957.
Ohta Y, Tsuchihashi T, Onaka U, Miyata E . Long-term compliance of salt restriction and blood pressure control status in hypertensive outpatients. Clin Exp Hypertens 2010; 32: 234–238.
Sakaki M, Tsuchihashi T, Arakawa K, Fukui H, Kameda W, Tominaga M . Long-term variability urinary salt excretion and blood pressure in hypertensive patients. Hypertens Res 2014; 37: 939–943.
Hirota S, Sadanaga T, Mitamura H, Fukuda K . Long-term compliance with salt restriction assessed using the spot urine method in Japanese cardiology outpatients. Hypertens Res 2013; 36: 1096–1099.
Wakai K . A review of food frequency questionnaires developed and validated in Japan. J Epidemiol. 2009; 19: 1–11.
Ogawa K, Tsubono Y, Nishino Y, Watanabe Y, Ohkubo T, Watanabe T, Nakatsuka H, Takahashi N, Kawamura M, Tsuji I, Hisamichi S . Validation of a food-frequency questionnaire for cohort studies in rural Japan. Public Health Nutr 2003; 6: 147–157.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
TT has received funding for clinical research from MSD KK and honoraria from MSD KK and Dainippon Sumitomo Pharma. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sakata, S., Tsuchihashi, T., Oniki, H. et al. Relationship between salt intake as estimated by a brief self-administered diet-history questionnaire (BDHQ) and 24-h urinary salt excretion in hypertensive patients. Hypertens Res 38, 560–563 (2015). https://doi.org/10.1038/hr.2015.35
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.35
Keywords
This article is cited by
-
Achievement rate of target blood pressure in patients with hypertension treated by hypertension specialists and non-specialists in a real-world setting
Hypertension Research (2023)
-
Dietary salt intake in Japan - past, present, and future
Hypertension Research (2022)
-
Salt and potassium intake evaluated with spot urine and brief questionnaires in combination with blood pressure control status in hypertensive outpatients in a real-world setting
Hypertension Research (2021)
-
Practical and personal education of dietary therapy in hypertensive patients
Hypertension Research (2020)
-
Food items contributing to high dietary salt intake among Japanese adults in the 2012 National Health and Nutrition Survey
Hypertension Research (2018)