Abstract
The relationship between arterial stiffness, measured as pulse wave velocity (PWV), and the left ventricle is confounded by the effects of blood pressure. We evaluated the relationship between carotid–femoral PWV and cardio-ankle vascular index (CAVI), a less pressure-dependent measurement of the stiffness constant (β) of the aorta and the iliac, femoral and tibial arteries, and obtained prognostically relevant measurements of left ventricular structure and systolic function. CAVI, carotid–femoral PWV and echocardiographic left ventricular mass and systolic function were determined in 133 subjects with either hypertension or high–normal blood pressure (33% treated; 56±16 years, blood pressure 145/89±21/12 mm Hg). Carotid–femoral PWV exhibited a direct relationship with systolic and diastolic blood pressure (r=0.33/0.26, P<0.001/0.014), whereas CAVI demonstrated no such relationship (r=0.12/−0.05, both P>0.1). Both CAVI and PWV correlated significantly with left ventricular mass index (r=0.31, P<0.001; r=0.21, P=0.014). Subjects with inappropriately high left ventricular masses for a given cardiac workload (n=44) had higher CAVI values (9.1±2.0 vs. 7.9±1.6, P<0.001), but not higher PWV values (8.5±2.5 vs. 8.7±2.4, P>0.1). In a multivariate regression model, CAVI was independently associated with inappropriate left ventricular mass (β=0.40, P<0.001), along with body mass index. CAVI also demonstrated a negative relationship with left ventricular midwall fractional shortening (r=−0.41, P=0.001) that was independent of age, sex, blood pressure and left ventricular mass in a multivariate analysis. In conclusion, a high CAVI is associated with inappropriately high left ventricular mass and low midwall systolic function. As a marker of arterial diastolic-to-systolic stiffening, CAVI may have a relationship with left ventricular structure and function that is independent of blood pressure levels.
Similar content being viewed by others
Introduction
Arterial stiffness is both a major contributor to systolic hypertension and an independent predictor of cardiovascular morbidity and mortality in the general population,1, 2, 3 as well as in the settings of high-risk conditions such as hypertension4 and type 2 diabetes.5 Measurement of carotid–femoral pulse wave velocity (PWV), a direct measure of large-artery stiffness, improves model fit and reclassifies risk for future cardiovascular events in models that include standard risk factors.6 Consequently, the assessment of aortic PWV has been recommended by the European Societies of Hypertension and Cardiology for cardiovascular risk stratification in hypertensive subjects.7
Arterial wall stiffness is a major determinant of left ventricular (LV) afterload. Carotid–femoral PWV, a direct measure of aortic stiffness, has a significant and direct relationship with LV mass.8, 9, 10 However, PWV is intrinsically dependent on blood pressure (BP),11,12 and the above relationships between PWV and LV mass are generally no longer significant when the effects of BP are taken into account.8, 9, 10 Notably, PWV is measured using diastolic pressure, as transit time is calculated at the foot of the pulse wave. As arterial elastic behavior is pressure dependent,13,14 aortic PWV, which is used to estimate diastolic stiffness, may be a less suitable means of determining effective cardiac afterload. Previous studies have suggested that increases in arterial stiffness, which may be observed during physical exercise15 and throughout the cardiac cycle using diastolic and systolic BP levels,16 may be more closely related to LV mass, although there is a need for simple, easy-to-use bedside markers of the pressure dependency of arterial stiffness.
Cardio-ankle vascular index (CAVI) is a noninvasive indirect estimate of the arterial stiffness index, β, of the aorta and the iliac, femoral and tibial arteries based on the formula of Bramwell–Hill.17 The stiffness parameter β is based on changes in vascular diameter corresponding to changes in arterial pressure, and its value does not depend on BP at the time of measurement.13,18 As a measure of the increase in arterial stiffness occurring between diastolic and systolic BP values, β incorporates information on arterial properties during the entirety of systole (diastolic-to-systolic ‘stiffening’).17 CAVI is less pressure dependent than PWV that samples arterial stiffness at a given point of the cardiac cycle—usually end-diastole—and is therefore strongly dependent on BP.17
To the best of our knowledge, the impacts of CAVI and carotid-femoral PWV on cardiac structure and function have never been compared directly. As pressure-dependent changes in arterial stiffness affect arterial compliance and LV afterload, we hypothesized that CAVI, an indirect marker of diastolic-to-systolic ‘stiffening’, may be related to LV mass and systolic function. Therefore, we undertook the present study with the aim of investigating the links between CAVI and carotid–femoral PWV with LV mass and systolic function in subjects with either high–normal or high BP. We focused particularly on the impact of arterial stiffness indices on two prognostically relevant markers of subclinical cardiac organ damage, namely inappropriately high LV mass, or values of LV mass exceeding levels needed to compensate for a given hemodynamic load,19,20 and LV systolic dysfunction, defined as low afterload-corrected midwall fractional shortening.21, 22, 23
Methods
Subjects
We analyzed data from 161 consecutive subjects with either high–normal or high BP who were referred to our hypertension outpatient clinic by their general practitioners. Subjects with either high–normal BP (office BP between 130/85 and 139/89 mm Hg on ⩾3 visits at 1-week intervals) or essential hypertension (office BP ⩾140/90 mm Hg on ⩾3 visits at 1-week intervals or receiving BP-lowering drug treatment) were enrolled. Hypertensive subjects were included if they were either untreated or receiving stable drug treatment: subjects who had started or changed their antihypertensive treatment within a year of the study were excluded. We also excluded subjects with an LV ejection fraction <50%, clinical or laboratory evidence of heart failure, coronary heart disease, previous stroke, valvular defects or secondary causes of hypertension, atrial fibrillation or important concomitant disease. A total of 18 individuals (11%) were excluded because of poor-quality echocardiograms. As lower-extremity arterial disease artificially decreases lower-extremity arterial stiffness,24 we excluded 10 subjects with an ankle-brachial BP index of <1, leaving 133 patients for analysis. All subjects provided informed consent to participate in the study that was approved by the institutional ethics committee.
Clinical and vascular assessment
All measurements were conducted in a quiet room kept at a constant temperature. Office BPs were measured by a physician in the hospital outpatient clinic with a mercury sphygmomanometer, with the subject sitting for ⩾10 min. The average of six measurements from ⩾2 sessions was used for analysis.
CAVI was recorded using a Vasera VS-1500 vascular screening system (Fukuda Denshi, Tokyo, Japan) immediately following the echocardiographic examination, with the patient resting in a supine position. CAVI is used to measure arterial stiffness from the aortic valve to the ankle.17 Briefly, CAVI is an indirect estimate of the arterial stiffness index, β, as described by Hayashi et al.,13 with PWV replacing arterial distension according to the equation of Bramwell–Hill. CAVI was determined using the following equation:

where SBP and DBP are systolic and diastolic blood pressure, ρ is blood density, PWV is calculated from the aortic valve to the ankle, and a and b are constants. ECG electrodes were placed on both wrists: a microphone to detect heart sounds was placed on the sternum, and cuffs were wrapped around both arms and both ankles. Following automatic measurements, data were analyzed using VSS-10 software (Fukuda Denshi), and right and left CAVI values were calculated. The higher of the two CAVI values was used for analysis. In our laboratory, the intraobserver coefficient of variation of CAVI was 5.7% in 40 healthy young volunteers.
Carotid–femoral PWV was determined with the SphygmoCor system (SphygmoCor Vx, AtCor Medical, Sydney, Australia) that uses a high-fidelity applanation tonometer to sequentially measure pressure pulse waveforms in two peripheral artery sites. PWV was obtained using measurements of common carotid and femoral artery waveforms as described previously.25 Transit time was calculated using the R-wave of the surface ECG as a common reference. PWV was automatically calculated using measurements of pulse transit time and the distance between the two sites according to the following formula: PWV (m s−1)=distance (m)/transit time (s). Path length was calculated by subtracting the distance between the carotid artery measurement site and the suprasternal notch from the distance between the femoral artery site and the suprasternal notch, all of which were measured directly using a caliper. The intraobserver coefficient of variation of carotid–femoral PWV in our laboratory was 5.1%.26
Echocardiography
M-mode echocardiographic studies of the left ventricle were performed under two-dimensional control as reported previously27 by two investigators (GS and GP) who were unaware of patients’ clinical data. LV mass was indexed by height2.7 to correct for weight.28 LV hypertrophy was defined as an LV mass index ⩾51 g × m−2.7 in both sexes. Relative wall thickness was calculated as follows: (2 × posterior wall thickness/LV internal diameter). LV end-diastolic and end-systolic volumes and stroke volume were calculated using the formula of Teichholz et al.29 In our laboratory, the intraobserver test–retest 90% interval of agreement for LV mass measurements was −16 to +14 g.30 The interobserver test–retest 90% interval of agreement was −20 to +18 g.
Excess LV mass, determined relative to the mass needed to sustain cardiac load, a well-known physiologic concept referred to as inappropriately high LV mass,31 was estimated on the basis of the following equation developed using a reference population of 121 normotensive, normal-weight adults, aged 18 to 84 years (R2=0.53, standard error of the estimate 27.3 g, P<0.001): predicted LV mass (g)=−11.4+(0.44 × stroke work)+(17.9 × height2.7)+(18.2 × sex), where sex=2 for men and 1 for women.30 Stroke work was estimated as systolic BP multiplied by stroke volume and converted to g × m by multiplying by 0.0144.32 Total external myocardial work may be dimensionally represented by the force (maximal systolic pressure) needed to eject a certain amount of blood into the aorta. Maximal systolic pressure may be surrogated using cuff systolic pressure under the assumption that kinetic energy is negligible in resting conditions.33 This allows for an efficient determination of stroke work and an individual assessment of compensatory and noncompensatory LV modifications using fully noninvasive methods. An observed/predicted LV mass ratio of 133% identified the 95th percentile of its distribution in the reference population. The subjects with observed/predicted LV mass ratios of >133% were classified as having inappropriately high LV masses.30
LV mechanics was assessed at the chamber level as endocardial fractional shortening, and at the midwall level using a geometric model that takes into account the nonuniform systolic thickening of the LV wall.21,22 Fractional shortening was considered both in absolute terms and after correcting for afterload, as a percentage of the value predicted from end-systolic circumferential wall stress with regression equations from previously studied normotensive subjects.23 A midwall fractional shortening value below the 5th percentile of afterload-corrected midwall fractional shortening for normotensive subjects was defined as midwall systolic dysfunction, and a midwall fractional shortening value of >5th percentile was defined as normal midwall systolic function.
Statistical analysis
Descriptive statistics are provided as means and s.d. or as frequencies and percentages. Pearson’s correlation coefficients were used when appropriate and compared using the z-test. The associations of continuous parameters in univariate analyses were evaluated using Pearson’s correlation. Characteristics of participants with appropriate and inappropriate LV masses were compared using the unpaired-sample t-test. Before performing the linear regression analysis, we assessed whether the relationship between CAVI and LV parameters was any different between treated and untreated subjects using linear regression models for CAVI with terms for LV mass, treatment status and an LV mass × treatment status interaction term. As the interaction terms were not significant, the study population as a whole was used to assess the independent predictors of appropriate LV mass and midwall fractional shortening using stepwise multivariate linear regression. Variables were included in the model if they were established or putative determinants, or if they achieved a significance value of <0.30 in an initial regression analysis with an ‘entry’ model. The final models were evaluated for other linear relationships among variables (multicollinearity) that have the potential to render significance testing unreliable. A variance inflation factor of <5 was assumed to exclude significant collinearity among the covariates in the models.34
Results
We examined 33 individuals with high–normal BP and 100 patients with essential hypertension. Fifty-six hypertensive subjects were untreated, and 44 had been receiving stable BP-lowering drug treatment for ⩾1 year. Primary characteristics of the study population are reported in Table 1.
As expected, carotid–femoral PWV significantly and directly correlated with both systolic BP (r=0.33, P<0.001) and diastolic BP (r=0.25, P<0.01). CAVI had no significant relationships with either systolic BP (r=0.15, P=0.11; Figure 1, left panel) or diastolic BP (r=−0.02, P=0.76). The relationship between systolic BP and PWV was significantly stronger than that between systolic BP and CAVI (P=0.014, z-test for comparison between r values). CAVI and carotid–femoral PWV correlated significantly with each other, although the strength of the correlation was only moderate (r=0.46, P<0.001; Figure 1, right panel).
As the analysis of the interaction term ‘treatment status × inappropriate LV mass’ revealed no significant effects of treatment status on the relationship between CAVI and inappropriate LV mass (P=0.45), the study population as a whole was used to assess the relationships between CAVI and inappropriate LV mass. CAVI significantly and directly correlated with LV mass when indexed by body surface area (r=0.33, P<0.001) and height2.7 (r=0.31, P<0.001; Figure 2, left panel). Carotid–femoral PWV also correlated with LV mass index among the entire population (r=0.20, P=0.033 and r=0.21, P=0.014, respectively), as well as within the subgroup with appropriate LV masses (r=0.26, P=0.017 and r=0.29, P=0.008, respectively). Participants with inappropriate LV masses (n=44) did not differ in age from the subjects whose LV masses were appropriate for their cardiac workloads (n=89; 58.5±15 years vs. 54.1±16 years, P=0.13). As shown in Figure 3, individuals with inappropriate LV masses had significantly higher CAVIs, although the two groups did not differ in terms of carotid–femoral PWV. In a multivariate linear regression model (multiple R2=0.20), inappropriately high LV mass was independently predicted by CAVI (β=0.40, P<0.001) and body mass index (β=0.19, P=0.022). Systolic BP, age, sex, body height, serum lipids and glucose, antihypertensive drug treatment and smoking habits failed to enter the model. When the analysis was limited to only untreated subjects (n=89), CAVI remained an independent predictor of inappropriate LV mass (β=0.57, P<0.001).
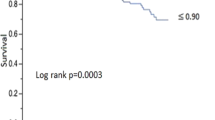
An inverse relationship was observed between CAVI and LV fractional shortening, the latter of which was assessed at both endocardial (r=−0.33, P<0.001) and midwall levels (r=−0.41, P<0.001; Figure 2, right panel). Carotid–femoral PWV was not significantly related to measurements of LV systolic function (endocardial fractional shortening, r=−0.04, P=0.66; midwall fractional shortening, r=−0.14, P=0.14). Participants with low LV midwall systolic function (n=24) were older (62.7±17 vs. 53.9±16 years) and had a higher systolic BP (149/89±21/13 vs. 144/89±20/11 mm Hg) than subjects with normal systolic function (n=109), although the difference in BP was not significant. As shown in Figure 4, individuals with low LV midwall systolic function had a significantly higher CAVI than subjects with normal systolic function, although the two groups did not differ in terms of carotid–femoral PWV. In a multivariate linear regression model (multiple R2=0.29), midwall fractional shortening was independently predicted by and inversely related to LV mass (β=−0.37, P<0.001) and CAVI (β=−0.31, P<0.001). Body mass index, systolic BP, age, sex, body height, serum lipids and glucose, antihypertensive drug treatment and smoking habits failed to enter the model. The independent relationship between CAVI with LV midwall fractional shortening was also confirmed in untreated subjects (β=0.27, P<0.01).
Discussion
The primary novel finding of the present paper is that the CAVI parameter of arterial stiffness is higher in patients with subclinical heart disease, defined as inappropriately high LV mass or LV systolic dysfunction among subjects with hypertension or with high–normal BP. CAVI was independently associated with important, prognostically adverse markers of LV structure and function, such as inappropriate LV mass and low LV midwall fractional shortening, relationships independent of BP. We also confirmed that CAVI is a less pressure-dependent measurement than aortic PWV.
Arterial stiffness determines the premature return of reflected waves in systole that increases central pulse pressure and left ventricular afterload. The heart adapts to face the arterial stiffness-related increase in LV afterload by developing ventricular hypertrophy that eventually leads to systolic dysfunction. Although aortic stiffness, which is assessed by carotid–femoral PWV, has been linked to LV remodeling and dysfunction in cross-sectional studies,8, 9, 10 the relationship between PWV and the left ventricle is confounded by the effects of BP that is both a major determinant of LV mass35,36 and a strong correlate of arterial PWV.11,12 Previous studies have generally shown that aortic PWV does not significantly correlate with LV mass when the effects of BP are taken into account.8, 9, 10 The present study confirms that carotid–femoral PWV does not have a significant BP-independent relationship with LV mass. Moreover, we found that PWV has an inverse relationship with LV midwall systolic function, although the above relationship was not insignificant and was not independent of BP values. Taken together, our findings and previous data16 suggest that diastolic arterial stiffness may not have a major impact on LV mass and function once the role of BP is taken into account.
Among the various noninvasive markers of arterial stiffness, CAVI has been theoretically proposed as an indirect estimate of the stiffness parameter, β, that is obtained by the logarithmic expression of the change in internal pressure of the vessel wall and changes in vascular diameter and is independent of BP.13 It should be noted that although systolic and diastolic BP are included in the equation, CAVI itself may not be pressure dependent, as it expresses the theoretically pressure-independent stiffness parameter, β. Previous studies have demonstrated that the contribution of BP to CAVI was weaker than its contribution to carotid–femoral PWV.17 Our findings also support the weak correlation between CAVI and systolic and diastolic BP.
The reasons why CAVI may have a stronger impact on LV mass and function than carotid–femoral PWV may be twofold. First, CAVI is based on the pressure-independent stiffness constant (β), a marker of arterial diastolic-to-systolic stiffening, whereas PWV is a marker of diastolic arterial stiffness, as it accounts for foot-to-foot transit time that inherently involves measurements of diastolic BP. Diastolic-to-systolic stiffening, obtained from combined carotid ultrasound and tonometry recordings, may be more closely related to LV mass than to diastolic arterial stiffness,16 and indices of hemodynamic load provoked by isometric exercise predict LV mass in hypertension better than carotid–femoral PWV measured at rest.15 Taken together, these findings support our hypothesis that the pressure dependency of arterial stiffness, a marker of effective LV afterload,37 may be a strong determinant of LV mass. Second, CAVI and carotid–femoral PWV explore different arterial pathways. Specifically, CAVI measurements include the proximal ascending aortic segment, as well as the femoral, popliteal and tibial arteries. Wall stiffness of the ascending aorta assessed by tissue-Doppler imaging is independently related to LV mass index,38 and age-related elongation and stiffening of the ascending aorta assessed by magnetic resonance imaging are both related to LV mass and concentric remodeling.39 The inclusion of lower-limb arterial segments may also play a role. Previous studies have shown that measures of regional stiffness, which also include peripheral arterial studies such as cardio-ankle PWV, were more strongly associated with electrocardiographic LV hypertrophy than carotid–femoral PWV.40 Moreover, brachial-ankle PWV was more strongly related to echocardiographic LV mass than carotid–femoral PWV.41 These data raise the possibility that peripheral muscular arteries may contribute to the ventricular–arterial interaction in a manner independent of the central arteries.
The findings of the present study have several clinical implications. Although LV hypertrophy in hypertension is a physiological response to hemodynamic overload, ‘inappropriate’ LV mass, or an increase in LV mass that exceeds levels needed to compensate for hemodynamic load,28 independently predicts subsequent cardiovascular morbidity and mortality, with a predictive power similar to LV hypertrophy.5 Our study suggests that the ratio of observed/predicted LV mass may be particularly sensitive to the hemodynamic impact of increased CAVI as a measure of LV afterload, perhaps more than the effects of BP would be. In addition, the inverse relationship between CAVI and systolic LV midwall function is of interest because systolic dysfunction of the left ventricle assessed at the midwall level, which is observed in approximately one-fifth of hypertensive individuals,23 independently predicts myocardial infarction and heart failure in treated hypertension.22,42 In a group of 102 treated hypertensive subjects, Masugata et al.43 demonstrated an inverse relationship between CAVI and LV ejection fraction, although the relationship was no longer significant when examined with multivariate analysis. In a retrospective analysis of 30 subjects with acute heart failure, CAVI correlated inversely with LV ejection fraction.44 Our findings confirm the inverse relationship between CAVI and LV ejection fraction in a population without clinically overt heart disease, a relationship that was previously reported in patients with ischemic heart disease45 and reduced ejection fractions.44,46 Our findings of an independent relationship between CAVI and prognostically relevant measures of subclinical heart disease may partly explain the previously described relationship with the prevalence47 and incidence48 of cardiovascular disease.
The present study has limitations. First, the results of this relatively small study need to be confirmed in a larger population. Second, cross-sectional studies cannot establish causality in a potentially bidirectional relationship between CAVI and subclinical cardiac changes. In particular, we cannot exclude that low LV systolic function may play a role in increasing CAVI. As the velocity of the pulse wave is estimated using pulse transmission time between the aortic valve and the ankle, and the timing of cardiac sounds may be influenced by systolic function, the latter may also theoretically influence CAVI. Third, several unproven assumptions are involved in the CAVI definition. Arterial distensibility is not measured directly but is estimated on the basis of the Bramwell–Hill equation, and heart–ankle distance and travel time are also estimated indirectly. As an effect of the approximations contained in these assumptions, the relationship between CAVI and the stiffness index β is only moderate.49
Our study shows that in asymptomatic individuals with either high–normal BP or essential hypertension and no obvious LV systolic dysfunction (LV ejection fraction ⩾50%), CAVI is more strongly associated with prognostically relevant measures of preclinical heart disease, such as inappropriate LV mass and low midwall LV systolic function, than with carotid–femoral PWV. Although carotid–femoral PWV remains a mainstay in functional evaluations of the large arteries as a strong, independent predictor of all-cause and cardiovascular mortality,1, 2, 3, 4, 5, 6 parameters such as CAVI that assess changes in arterial stiffness during the entirety of the cardiac cycle also deserve consideration in cardiovascular risk assessments.
References
Sutton-Tyrrell K, Najjar SS, Boudreau RM, Venkitachalam L, Kupelian V, Simonsick EM, Havlik R, Lakatta EG, Spurgeon H, Kritchevsky S, Pahor M, Bauer D, Newman A ; Health ABC Study. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 2005; 111: 3384–3390.
Hansen TW, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ Arterial stiffness and cardiovascular events: the Framingham Heart Study. Circulation 2010; 121: 505–511.
Laurent S, Katsahian S, Fassot C, Tropeano AI, Gautier I, Laloux B, Boutouyrie P . Aortic stiffness is an independent predictor of fatal stroke in essential hypertension. Stroke 2003; 34: 1203–1206.
Cruickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG . Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 2002; 106: 2085–2090.
Ben-Shlomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, Boutouyrie P, Cameron J, Chen CH, Cruickshank JK, Hwang SJ, Lakatta EG, Laurent S, Maldonado J, Mitchell GF, Najjar SS, Newman AB, Ohishi M, Pannier B, Pereira T, Vasan RS, Shokawa T, Sutton-Tyrell K, Verbeke F, Wang KL, Webb DJ, Willum Hansen T, Zoungas S, McEniery CM, Cockcroft JR, Wilkinson IB . Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol 2014; 63: 636–646.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Task Force Members. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31: 1281–1357.
Boutouyrie P, Laurent S, Girerd X, Benetos A, Lacolley P, Abergel E, Safar M . Common carotid artery stiffness and patterns of left ventricular hypertrophy in hypertensive patients. Hypertension 1995; 25: 651–659.
Libhaber E, Woodiwiss AJ, Libhaber C, Maseko M, Majane OH, Makaula S, Dessein P, Essop MR, Sareli P, Norton GR . Gender-specific brachial artery blood pressure-independent relationship between pulse wave velocity and left ventricular mass index in a group of African ancestry. J Hypertens 2008; 26: 1619–1628.
Schillaci G, Mannarino MR, Pucci G, Pirro M, Helou J, Savarese G, Vaudo G, Mannarino E . Age-specific relationship of aortic pulse wave velocity with left ventricular geometry and function in hypertension. Hypertension 2007; 49: 317–321.
Cecelja M, Chowienczyk P . Dissociation of aortic pulse wave velocity with risk factors for cardiovascular disease other than hypertension: a systematic review. Hypertension 2009; 54: 1328–1336.
Schillaci G, Pucci G, Pirro M, Settimi L, Hijazi R, Franklin SS, Mannarino E . Combined effects of office and 24-hour blood pressure on aortic stiffness in human hypertension. J Hypertens 2011; 29: 869–875.
Hayashi K, Handa H, Nagasawa S, Okumura A, Moritake K . Stiffness and elastic behavior of human intracranial and extracranial arteries. J Biomech 1980; 13: 175–184.
Langewouters GJ, Wesseling KH, Goedhard WJA . The static elastic properties of 45 human thoracic and 20 abdominal aortas in vitro and the parameters of a new model. J Biomech 1984; 17: 425–435.
Chirinos JA, Segers P, Raina A, Saif H, Swillens A, Gupta AK, Townsend R, Emmi Jr AG, Kirkpatrick JN, Keane MG, Ferrari VA, Wiegers SE St, John Sutton MG . Arterial pulsatile hemodynamic load induced by isometric exercise strongly predicts left ventricular mass in hypertension. Am J Physiol Heart Circ Physiol 2010; 298: H320–H330.
Hermeling E, Vermeersch SJ, Rietzschel ER, de Buyzere ML, Gillebert TC, van de Laar RJ, Ferreira I, Hoeks AP, van Bortel LM, Reneman RS, Segers P, Reesink KD . The change in arterial stiffness over the cardiac cycle rather than diastolic stiffness is independently associated with left ventricular mass index in healthy middle-aged individuals. J Hypertens 2012; 30: 396–402.
Shirai K, Utino J, Otsuka K, Takata M . A novel blood pressure-independent arterial wall stiffness parameter; Cardio Ankle Vascular Index (CAVI). J Atheroscler Thromb 2006; 13: 101–107.
Buntin CM, Silver FH . Noninvasive assessment of mechanical properties of peripheral arteries. Ann Biomed Eng 1990; 18: 549–566.
de Simone G, Palmieri V, Koren MJ, Mensah GA, Roman MJ, Devereux RB . Prognostic implications of the compensatory nature of left ventricular mass in arterial hypertension. J Hypertens 2001; 19: 119–125.
Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Bonzi B, Poisa P, Belotti E, Agabiti Rosei C, Rizzoni D, Castellano M, Agabiti Rosei E . Inappropriate left ventricular mass changes during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension 2007; 49: 1077–1083.
Shimizu G, Hirota Y, Kita Y, Kawamura K, Saito T, Gaasch WH . Left ventricular midwall mechanics in systemic arterial hypertension: myocardial function is depressed in pressure-overload hypertrophy. Circulation 1991; 83: 1676–1684.
de Simone G, Devereux RB, Koren MJ, Mensah GA, Casale PN, Laragh JH . Midwall left ventricular mechanics. An independent predictor of cardiovascular risk in arterial hypertension. Circulation 1996; 93: 259–265.
Schillaci G, Verdecchia P, Reboldi G, Pede S, Porcellati C . Subclinical left ventricular dysfunction in systemic hypertension and the role of 24-hour blood pressure. Am J Cardiol 2000; 86: 509–513.
Motobe K, Tomiyama H, Koji Y, Yambe M, Gulinisa Z, Arai T, Ichihashi H, Nagae T, Ishimaru S, Yamashina A . Cut-off value of the ankle-brachial pressure index at which the accuracy of brachial-ankle pulse wave velocity measurement is diminished. Circ J 2005; 69: 55–60.
Schillaci G, Sarchielli P, Corbelli I, Pucci G, Settimi L, Mannarino MR, Calabresi P, Mannarino E . Aortic stiffness and pulse wave reflection in young subjects with migraine: a case-control study. Neurology 2010; 75: 960–966.
Pirro M, Schillaci G, Paltriccia R, Bagaglia F, Menecali C, Mannarino MR, Capanni M, Velardi A, Mannarino E . Increased ratio of CD31+/CD42− microparticles to endothelial progenitors as a novel marker of atherosclerosis in hypercholesterolemia. Arterioscler Thromb Vasc Biol 2006; 26: 2530–2535.
Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F . Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension 2000; 35: 580–586.
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, De Divitiis O, Alderman MH . Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and the impact of overweight. J Am Coll Cardiol 1992; 20: 1251–1260.
Teichholz LE, Kreulen T, Herman MV, Gorlin R . Problems in echocardiographic volume determinations: echocardiographic-angiographic correlations in the presence of absence of asynergy. Am J Cardiol 1976; 37: 7–11.
Schillaci G, Vaudo G, Pasqualini L, Reboldi G, Porcellati C, Verdecchia P . Left ventricular mass and systolic dysfunction in essential hypertension. J Hum Hypertens 2002; 16: 117–122.
de Simone G, Devereux RB, Kimball TR, Mureddu GF, Roman MJ, Contaldo F, Daniels SR . Interaction between body size and cardiac workload: influence on left ventricular mass during body growth and adulthood. Hypertension 1998; 31: 1077–1082.
de Simone G, Chinali M, Galderisi M, Benincasa M, Girfoglio D, Botta I, D'Addeo G, de Divitiis O . Myocardial mechano-energetic efficiency in hypertensive adults. J Hypertens. 2009; 27: 650–655.
Klabunde R (ed). Cardiovascular Physiology Concepts. Lippincott Williams & Wilkins: Hagerstown, MD, 2004.
Menard S . Applied Logistic Regression Analysis: SAGE University Series on Quantitative Applications in the Social Sciences. SAGE Publications: Thousand Oaks, CA, 1995.
Verdecchia P, Schillaci G, Borgioni C, Gattobigio R, Ambrosio G, Porcellati C . Prevalent influence of systolic over pulse pressure on left ventricular mass in essential hypertension. Eur Heart J 2002; 23: 658–665.
Fagard R, Staessen JA, Thijs L . The relationships between left ventricular mass and daytime and night-time blood pressures: a meta-analysis of comparative studies. J Hypertens 1995; 13: 823–829.
Craiem D, Graf S, Salvucci F, Chironi G, Megnien JL, Simon A, Armentano RL . The physiological impact of the nonlinearity of arterial elasticity in the ambulatory arterial stiffness index. Physiol Meas 2010; 31: 1037–1046.
Vitarelli A, Giordano M, Germanò G, Pergolini M, Cicconetti P, Tomei F, Sancini A, Battaglia D, Dettori O, Capotosto L, De Cicco V, De Maio M, Vitarelli M, Bruno P . Assessment of ascending aorta wall stiffness in hypertensive patients by tissue Doppler imaging and strain Doppler echocardiography. Heart 2010; 96: 1469–1474.
Redheuil A, Yu WC, Mousseaux E, Harouni AA, Kachenoura N, Wu CO, Bluemke D, Lima JA . Age-related changes in aortic arch geometry: relationship with proximal aortic function and left ventricular mass and remodeling. J Am Coll Cardiol 2011; 58: 1262–1270.
Wohlfahrt P, Krajčoviechová A, Seidlerová J, Mayer O, Bruthans J, Filipovský J, Laurent S, Cífková R . Arterial stiffness parameters: how do they differ? Atherosclerosis 2013; 231: 359–364.
Yu WC, Chuang SY, Lin YP, Chen CH . Brachial-ankle vs carotid-femoral pulse wave velocity as a determinant of cardiovascular structure and function. J Hum Hypertens 2008; 22: 24–31.
Wachtell K, Gerdts E, Palmieri V, Olsen MH, Nieminen MS, Papademetriou V, Boman K, Dahlöf B, Aurigemma GP, Rokkedal JE, Devereux RB . In-treatment midwall and endocardial fractional shortening predict cardiovascular outcome in hypertensive patients with preserved baseline systolic ventricular function: the Losartan Intervention For Endpoint reduction study. J Hypertens 2010; 28: 1541–1546.
Masugata H, Senda S, Okuyama H, Murao K, Inukai M, Hosomi N, Yukiiri K, Nishiyama A, Kohno M, Goda F . Comparison of central blood pressure and cardio-ankle vascular index for association with cardiac function in treated hypertensive patients. Hypertens Res 2009; 32: 1136–1142.
Zhang C, Ohira M, Iizuka T, Mikamo H, Nakagami T, Suzuki M, Hirano K, Takahashi M, Shimizu K, Sugiyama Y, Yamaguchi T, Kawana H, Endo K, Saiki A, Oyama T, Kurosu T, Tomaru T, Wang H, Noike H, Shirai K . Cardio-ankle vascular index relates to left ventricular ejection fraction in patients with heart failure. A retrospective study. Int Heart J 2013; 54: 216–221.
Miyoshi T, Doi M, Hirohata S, Sakane K, Kamikawa S, Kitawaki T, Kaji Y, Kusano KF, Ninomiya Y, Kusachi S . Cardio-ankle vascular index is independently associated with the severity of coronary atherosclerosis and left ventricular function in patients with ischemic heart disease. J Atheroscler Thromb 2010; 17: 249–258.
Noguchi S, Masugata H, Senda S, Ishikawa K, Nakaishi H, Tada A, Inage T, Kajikawa T, Inukai M, Himoto T, Hosomi N, Murakami K, Noma T, Kohno M, Okada H, Goda F, Murao K . Correlation of arterial stiffness to left ventricular function in patients with reduced ejection fraction. Tohoku J Exp Med 2011; 225: 145–151.
Saji N, Kimura K, Shimizu H, Kita Y . Silent brain infarct is independently associated with arterial stiffness indicated by cardio-ankle vascular index (CAVI). Hypertens Res 2012; 35: 756–760.
Kubota Y, Maebuchi D, Takei M, Inui Y, Sudo Y, Ikegami Y, Fuse J, Sakamoto M, Momiyama Y . Cardio-ankle vascular index is a predictor of cardiovascular events. Artery Res 2011; 5: 91–96.
Takaki A, Ogawa H, Wakeyama T, Iwami T, Kimura M, Hadano Y, Matsuda S, Miyazaki Y, Matsuda T, Hiratsuka A, Matsuzaki M . Cardio-ankle vascular index is a new noninvasive parameter of arterial stiffness. Circ J 2007; 71: 1710–1714.
Acknowledgements
Fukuda-Denshi, Tokyo, Japan, donated the Vasera VS-1500 vascular screening system. GP’s position as an Assistant Professor at the University of Perugia was funded by a grant from the Fondazione Cassa di Risparmio di Terni e Narni. No other funds were obtained for the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
GS received grants from AtCor Medical as well as public speaking grants from Fukuda-Denshi. The other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schillaci, G., Battista, F., Settimi, L. et al. Cardio-ankle vascular index and subclinical heart disease. Hypertens Res 38, 68–73 (2015). https://doi.org/10.1038/hr.2014.138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.138
Keywords
This article is cited by
-
Comparison of the usefulness of the cardio-ankle vascular index and augmentation index as an index of arteriosclerosis in patients with essential hypertension
Hypertension Research (2022)
-
Relation of arterial stiffness to left ventricular structure and function in healthy women
Cardiovascular Ultrasound (2018)
-
Aortic stiffness improves the prediction of both diagnosis and severity of coronary artery disease
Hypertension Research (2018)
-
Greater reductions in plasma aldosterone with aliskiren in hypertensive patients with higher soluble (Pro)renin receptor level
Hypertension Research (2018)
-
Oscillometric assessment of arterial stiffness in everyday clinical practice
Hypertension Research (2017)