Abstract
Among subfractions of low-density lipoprotein cholesterol (LDL-C), small dense LDL-C (SdLDL-C) has been highlighted as the most atherogenic lipoprotein cholesterol. The present study aimed to compare the relationship of SdLDL-C with blood viscosity, a surrogate marker for cardiovascular disease, with that of other lipid fractions with blood viscosity in essential hypertensives (EHTs). In 128 untreated, early-stage EHTs, blood viscosity was measured with a falling-ball microviscometer, and serum levels of lipid fractions were determined. Blood and plasma viscosity was significantly higher in 49 patients with dyslipidemia (fasting serum level of LDL-C >140 mg dl−1, triglyceride >150 mg dl−1 or high-density lipoprotein cholesterol (HDL-C)<40 mg dl−1) compared with 79 patients without dyslipidemia, although hematocrit and RBC rigidity index ‘k’ did not differ between the two groups. Together, SdLDL-C, LDL-C, triglyceride and large LDL-C were positively correlated with blood viscosity, but for HDL-C, the correlation was negative. After adjusting for non-lipid variables that correlated with blood viscosity (that is, the age, body mass index, resting diastolic blood pressure, sex, hematocrit, plasma viscosity and homeostasis model of assessment of insulin resistance), SdLDL-C was most strongly associated with blood viscosity among the lipid fractions. These data suggest that SdLDL-C could strongly increase blood viscosity in EHTs.
Similar content being viewed by others
Introduction
Increased blood viscosity can elevate peripheral viscous resistance, reduce blood flow and enhance shear stress in the cardiovascular system, as shown by the Poiseuille equation.1, 2 Therefore, increased blood viscosity could have an important role in the pathogenesis of hypertension and other cardiovascular diseases. Indeed, blood viscosity and its determinants (that is, hematocrit, plasma fibrinogen, and erythrocyte aggregability and deformability) are altered in hypertension,3, 4 and hemorheological abnormalities are correlated with the severity of hypertension or hypertensive cardiovascular complications.5, 6, 7
It is well known that in hypertensive patients, metabolic disorders, such as dyslipidemia, metabolic syndrome and diabetes mellitus, are often clustered, thereby accelerating the development of cardiovascular complications, including atherosclerosis.8, 9, 10, 11, 12 Because abnormalities in lipid or glucose metabolism affect hemorheological parameters,13, 14, 15, 16 metabolic disorders, such as dyslipidemia, can contribute to the genesis of atherosclerosis by their effects on hemorheological properties, in addition to their direct influences on the vascular wall. However, it has not been determined how blood rheology is modulated in essential hypertensives (EHTs) when complicated with dyslipidemia.
Serum total cholesterol distributes among three major lipoprotein classes (that is, low-density lipoprotein (LDL), very low-density lipoprotein and high-density lipoprotein (HDL)). LDL is also separated by density into two different subfractions (that is, LDL pattern A, including large buoyant LDL, and intermediate density LDL and LDL pattern B, including small dense LDL (SdLDL)).17 Recently, several clinical studies have shown that SdLDL-cholesterol (SdLDL-C) had the highly atherogenic potential compared with other lipoprotein cholesterols.17, 18, 19, 20 However, no study has investigated whether the influences of lipids on blood viscosity could differ among the subfractions of lipoprotein cholesterol, including SdLDL-C, in EHTs.
In the present study, therefore, blood viscosity was compared between early-stage EHTs complicated with and without dyslipidemia. The associations of lipid fractions, particularly SdLDL-C with hemorheological parameters, were also investigated.
Methods
Subjects
The study design was approved by the Ethics Committee at the University of Toyama. A total of 128 untreated EHTs (84 men, mean age 56±12 years) were consecutively enrolled into the study after providing informed consent. Hypertension was diagnosed based on a sitting diastolic blood pressure (measured with a sphygmomanometer) of >90 mm Hg and/or a systolic blood pressure >140 mm Hg on three separate occasions over a 4-week period.21 The patients were considered to be in the early stage of hypertension because no patients had either macroalbuminuria (that is, urinary albumin >300 mg per day), impaired renal function (that is, creatinine clearance <60 ml min−1 per 1.73 m2) or clinically evident cardiovascular diseases. Secondary hypertension, diabetes mellitus and anemia were also absent in all subjects. Among the 44 female patients, 31 (70%) were postmenopausal, and none were undergoing hormone replacement therapy. Dyslipidemia was diagnosed based on the criteria of the Japanese Atherosclerosis Society22 if one or more of the following three elements was present: fasting serum level of LDL-cholesterol (LDL-C) >140 mg dl−1, triglyceride >150 mg dl−1 and HDL-cholesterol (HDL-C) <40 mg dl−1.
Study protocol
Blood viscosity and plasma viscosity were determined at the outpatient clinic in the morning. Patients were instructed not to consume food, alcohol and caffeine and not to smoke cigarettes within the 12-h period before blood samplings. A venous catheter was inserted into the antecubital vein, and after 30 min of rest in the supine position, the blood pressure and pulse were measured. Thereafter, venous blood was collected gently without vein occlusion. Blood samples for measurements of blood viscosity and plasma viscosity were collected in tubes containing potassium EDTA as an anticoagulant. Blood samples were also used to analyze parameters affecting hemorheology,11, 23, 24, 25, 26, 27, 28 including lipid parameters, as well as hematocrit, biochemical indices for glucose metabolism, high-sensitive C-reactive protein as a marker of inflammation and plasma fibrinogen. Subsequently, 24-h urine collection was used to measure creatinine clearance and urinary albumin excretion.
Blood viscosity and plasma viscosity were determined using a falling-ball microviscometer (AMVn-200, Anton Paar, Graz, Austria).7, 11 This instrument comprises a glass capillary tube (0.16 mm internal diameter) containing a 0.15-mm diameter metallic ball. Fluid viscosity is determined by the falling time of the ball in the tube filled with blood or plasma inclined at 70° at 20 °C.7, 11 In this setting, fluid viscosity is measured at a high shear rate between 2500 and 3000 s−1, which allows the measurement of blood viscosity in a completely disaggregated structure. Theoretically, in such a situation, blood viscosity mainly depends on three parameters: hematocrit, RBC deformability and plasma viscosity.29 RBC rigidity (that is, the index for RBC deformability) was evaluated using RBC rigidity index ‘k’ calculated according to the Quemada equation.30
As for the lipid parameter measurements, serum total cholesterol and triglyceride levels were determined using enzymatic methods. LDL-C and HDL-C levels were directly measured using a homogenous method with the assay kits provided by Denka Seiken (Tokyo, Japan). SdLDL-C level was measured using the precipitation method of Ito et al.,31 with the BM6070 clinical automated analyzer (JEOL, Tokyo, Japan). This method consists of two steps: removing apolipoprotein B-containing SdLDL-free lipoproteins from the blood samples by precipitation with heparin and magnesium, followed by measuring LDL-C with the homogenous method. Large LDL-C and non-HDL-C levels were determined by calculating LDL-C minus SdLDL-C and total cholesterol minus HDL-C, respectively. Other biochemical parameters, including serum insulin, blood glucose and plasma levels of high-sensitive C-reactive protein and fibrinogen, were measured using conventional laboratory techniques. Insulin resistance was estimated according to the homeostasis model of assessment of insulin resistance (HOMA-IR) calculated as fasting glucose (mg dl−1) × fasting plasma insulin (μIU ml−1)/405.
Data analysis
The data are presented as the mean±s.d. Comparisons were made between EHTs with and without dyslipidemia using the Student’s t-test for continuous variables and the χ2-test for categorical variables. Pearson’s correlation was used for the univariate analyses. Multivariate correlation was also tested by multiple regression analysis. A P-value <0.05 was considered to be statistically significant.
Results
Clinical characteristics
Dyslipidemia was present in 49 patients (38%). No significant differences were observed in age, gender, prevalence of familial clustering of hypertension and menopause and proportion of smokers between the EHTs with and without dyslipidemia (Table 1). Although body weight was greater in the EHTs with dyslipidemia than in the EHTs without dyslipidemia, height and body mass index did not differ between the two groups. The resting diastolic blood pressure and pulse rate were higher in the EHTs with dyslipidemia than in the EHTs without dyslipidemia, although the clinic blood pressure and pulse rate did not differ between the two groups. Although there were no differences in the blood glucose levels between the two groups, the HOMA-IR values were higher in the EHTs with dyslipidemia compared with the EHTs without dyslipidemia. In addition, the high-sensitive C-reactive protein and plasma fibrinogen levels did not differ between the two groups. Although the urinary albumin excretion levels did not differ between the two groups, the creatinine clearance was lower in the EHTs with dyslipidemia than in the EHTs without dyslipidemia.
Lipids and hemorheological variables
Because of the study design, the levels of total cholesterol, non-HDL-C, LDL-C and triglycerides were higher in EHTs with dyslipidemia than in EHTs without dyslipidemia, although the HDL-C level was lower in EHTs with dyslipidemia than in EHTs without dyslipidemia (Table 2). Similarly, SdLDL-C and large LDL-C levels and the ratio of SdLDL-C to LDL-C were significantly greater in the EHTs with dyslipidemia compared with EHTs without dyslipidemia.
Blood and plasma viscosity was significantly higher in the EHTs with dyslipidemia than in the EHTs without dyslipidemia, although hematocrit and RBC rigidity index ‘k’ did not differ between the two groups.
Relationships between lipid parameters and hemorheological variables
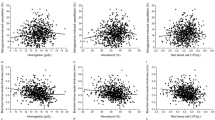
Figure 1 depicts the univariate correlations of lipid parameters with blood viscosity in all patients. SdLDL-C, LDL-C, triglycerides, non-HDL-C and large LDL-C positively correlated with blood viscosity (r=0.380, 0.332, 0.291, 0.215 and 0.200; P<0.001, P<0.001, P<0.001, P=0.015 and P=0.023, respectively). Conversely, HDL-C negatively correlated with blood viscosity (r=−0.289; P<0.001). Total cholesterol did not correlate significantly with blood viscosity.
Univariate correlations of SdLDL-C and other lipid fractions with blood viscosity in EHTs. Pearson’s correlation coefficients (r) and P-values are given. BV, blood viscosity; EHTs, essential hypertensives; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; SdLDL-C, small dense low-density lipoprotein cholesterol; TC, total cholesterol; TG, triglyceride.
Blood viscosity was influenced by non-lipid parameters in the present study, as follows. Together, age, body mass index and resting diastolic blood pressure were associated with blood viscosity (r=−0.178, 0.340 and 0.257; P=0.045, P<0.001 and P=0.004, respectively). Blood viscosity was also higher in male patients compared with female patients (4.32±0.49 vs. 3.82±0.34 mPa s, P<0.001). In addition, hematocrit, plasma viscosity and HOMA-IR correlated positively with blood viscosity (r=0.775, 0.235 and 0.275; P<0.001, P=0.008 and P=0.002, respectively), although either plasma fibrinogen or high-sensitive C-reactive protein was not associated with blood viscosity (r=0.047 or 0.142; not significant for each).
As shown in Figure 2, SdLDL-C, LDL-C and total cholesterol revealed an independent and positive correlation with blood viscosity after multiple adjustments using the above mentioned seven confounding variables. Particularly, SdLDL-C was most strongly associated with blood viscosity, as indicated by the adjusted standard regression coefficient (β-value) being 0.147 for SdLDL-C, 0.134 for LDL-C and 0.112 for total cholesterol. Conversely, triglyceride, large LDL-C, non-HDL-C and HDL-C did not show any significant associations with blood viscosity in the multiple regression models.
Standardized regression coefficients (β-values) for multivariate associations of SdLDL-cholesterol and other lipid fractions with blood viscosity in EHTs. An adjustment was made using seven variables, including age, sex difference, body mass index, resting diastolic blood pressure, hematocrit, plasma viscosity and HOMA-IR. *P<0.05, **P<0.01. EHTs, essential hypertensives; HDL-C, high-density lipoprotein cholesterol; HOMA-IR, homeostasis model assessment index of insulin resistance; LDL-C, low-density lipoprotein cholesterol; SdLDL-C, small dense low-density lipoprotein cholesterol; TC, total cholesterol; TG, triglyceride.
The univariate correlations between SdLDL-C and the determinants for blood viscosity were also evaluated in all the patients. SdLDL-C was positively correlated with hematocrit and RBC rigidity index ‘k’ (r=0.261 and 0.161; P=0.003 and 0.073, respectively), although the latter relationship had marginal significance. Contrarily, SdLDL-C was not associated with plasma viscosity.
Although triglyceride correlated significantly with plasma viscosity in the univariate analysis, all other lipid parameters did not correlate with plasma viscosity. Both plasma fibrinogen and high-sensitive C-reactive protein were also positively associated with plasma viscosity (r=0.530 and 0.465; P<0.001 for each one).
Discussion
The major findings of the present study are as follows. First, blood viscosity and plasma viscosity were higher in EHTs with dyslipidemia than in those without dyslipidemia, a finding that is consistent with previous studies in healthy subjects without cardiovascular diseases.14, 15, 16, 27, 28 Second, SdLDL-C was most closely associated with blood viscosity among all fractions of lipoprotein cholesterol tested in the present study.
Associations of blood lipids with blood viscosity in EHTs
A number of studies demonstrated in healthy adults that serum levels of total cholesterol, LDL-C and triglyceride correlated positively with blood viscosity, although serum HDL-C did so negatively.1, 14, 28, 32, 33 In the present study, the similar univariate relationships between blood lipids and blood viscosity were observed in untreated, early stage EHTs. Because blood viscosity is affected by many variables other than blood lipids, including plasma viscosity, hematocrit, sex, body weight, blood pressure, blood sugar, insulin sensitivity, inflammation and plasma fibrinogen,23, 24, 25, 26 the influences of these confounding factors on the relationships were removed by multivariate analysis in the present study. Thus, lipid fractions including SdLDL-C, LDL-C and total cholesterol emerged as independent markers for increased blood viscosity in EHT. Furthermore, SdLDL-C was the strongest marker for increased blood viscosity among lipid fractions in EHTs, a finding that is consistent with the influence of LDL-C on blood viscosity being enhanced along with the reduction in LDL diameter in healthy subjects.16
Concerning the relationship between blood lipids and plasma viscosity, triglyceride correlated positively with plasma viscosity despite no associations of the other lipids with plasma viscosity in EHT. Conversely, Irace et al.34 reported that in healthy subjects without hypertriglyceridemia, LDL-C correlated positively with plasma viscosity, and HDL-C correlated negatively with plasma viscosity, despite no relationship between triglyceride and plasma viscosity. A large observational, long-term study from the WHO (that is, MONICA project) also demonstrated a positive linear relationship between total serum cholesterol and plasma viscosity, and demonstrated a weak negative correlation between HDL-C and plasma viscosity in 4022 residents.15 Thus, the relationships between blood lipids and plasma viscosity might be affected by the background of the studied populations, particularly the serum level of triglyceride, because triglyceride-enriched lipoproteins (that is, chylomicron and very low-density lipoprotein) can increase plasma viscosity profoundly to mask the relationships between other lipids and plasma viscosity.32, 34
Possible mechanisms and clinical implications of the interaction between blood lipids and blood viscosity in EHTs
Blood viscosity is determined mainly by RBC concentration, aggregation and deformability and plasma viscosity.1, 16 Blood viscosity is also affected by plasma fibrinogen, which increases plasma viscosity and aggregates erythrocytes. The influences of these determinants of blood viscosity depend upon the existing shear forces (that is, shear rates). In particular, for the high shear rate adopted in the present study, RBC aggregation tends to be broken up, and the effect of erythrocyte aggregation on blood viscosity is negligible.16, 23 Therefore, the mechanisms by which blood lipids affect blood viscosity can be explained by the association of blood lipids with hematocrit, RBC deformability and plasma viscosity. In the present study, SdLDL-C correlated positively with hematocrit and RBC rigidity index ‘k’, but not with plasma viscosity. Therefore, SdLDL-C might influence blood viscosity by modifying hemoconcentration and RBC deformability in EHTs. Indeed, cell deformability is considered to be determined by mechanical properties of cell membrane, such as membrane fluidity, which can be influenced by membrane lipid compositions or redox status.35, 36 Therefore, dyslipidemia, particularly increased SdLDL-C, might alter the exchange between circulating and cell membrane lipids or induce oxidative stress,37, 38 thereby decreasing RBC deformability and increasing blood viscosity. However, the reason for the association of SdLDL-C with hematocrit cannot be deduced based on the present study. Additional measurements of blood viscosity using low shear rate (1–100 s−1) would also be needed to explore the influence of lipids on RBC aggregation.1, 16
As shown in some reports of healthy subjects,14, 16, 33 HDL-C inversely correlated with blood viscosity, although LDL-C did positively correlate with blood viscosity in EHTs. This opposite influence of HDL-C and LDL-C on blood viscosity could lead to opposite influences of these lipids on cardiovascular trees. Namely, HDL-C may protect the cardiovascular system by antagonizing the LDL-induced hemorheological changes likely associated with the genesis of cardiovascular disease.
The causal relationship between elevated LDL-C and cardiovascular diseases has been well established in previous cohort studies.39, 40 Recently, it has become apparent that the cardiovascular risk potential of LDL-C differs with respect to its size and density, and SdLDL-C is the most atherogenic subfraction of LDL-C.41, 42 Compared with large LDL-C, SdLDL-C has several characteristics associated with the genesis of atherosclerosis,38, 41, 42 such as (1) lower affinity to the LDL receptors in the liver, leading to reduced clearance and longer retention time in the circulation, (2) easier penetration into arterial wall, (3) higher susceptibility to oxidative modification and (4) induction of oxidative stress. Indeed, SdLDL-C was elevated in patients with coronary arterial disease.18 Furthermore, recent prospective cohort studies in Western and non-Western populations (the Québec Cardiovascular Study and the Suita Study) revealed that elevated SdLDL-C was a powerful predictor of the onset of coronary artery diseases compared with the other lipid fractions.19, 20 The present study demonstrated that the strong association between SdLDL-C and blood viscosity could at least partially explain why SdLDL-C presents the most powerful cardiovascular risk among all fractions of lipoprotein cholesterol.
Study limitations
The present study has several limitations. First, a causal relationship between dyslipidemia and increased blood viscosity was not confirmed in the present study because of the observational nature of the study. Long-term longitudinal studies are needed to clarify this issue. Second, the present study did not include normotensive subjects with and without dyslipidemia. These two groups should have been included to draw a definite conclusion concerning the additive effects of hypertension and dyslipidemia on blood rheology. Third, therapeutic intervention against SdLDL-C would be helpful to clarify the relationships between SdLDL-C and blood viscosity. Actually, the influences of blood lipids on hemorheological properties were attenuated along with a reduction in the LDL-C level by lipid-lowering therapies.43, 44, 45 Finally, EHTs in more advanced stages should be studied, as the subjects in the present study were limited to EHTs without cardiovascular complications.
Although limited for these reasons, the present study demonstrated that increased SdLDL-C levels were associated with increased blood viscosity in early-stage EHTs. Therapeutic interventions against SdLDL-C could normalize the hemorheological disturbances, thereby preventing cardiovascular complications in EHTs with dyslipidemia.
References
Cowan AQ, Cho DJ, Rosenson RS . Importance of blood rheology in the pathophysiology of atherothrombosis. Cardiovasc Drugs Ther 2012; 26: 339–348.
Chabanel A, Chien S . Blood viscosity in human hypertension. In Laragh JH, Brenner BM (eds). Hypertension: Pathophysiology, Diagnosis, and Management, (2nd edn) Raven Press: New York. 1995 pp 365–376.
Fowkes FG, Lowe GD, Rumley A, Lennie SE, Smith FB, Donnan PT . The relationship between blood viscosity and blood pressure in a random sample of the population aged 55 to 74 years. Eur Heart J 1993; 14: 597–601.
Smith WC, Lowe GD, Lee AJ, Tunstall-Pedoe H . Rheological determinants of blood pressure in a Scottish adult population. J Hypertens 1992; 10: 467–472.
Devereux RB, Drayer JI, Chien S, Pickering TG, Letcher RL, DeYoung JL, Sealey JE, Laragh JH . Whole blood viscosity as a determinant of cardiac hypertrophy in systemic hypertension. Am J Cardiol 1984; 54: 592–595.
Zannad F, Voisin P, Brunotte F, Bruntz JF, Stoltz JF, Gilgenkrantz JM . Haemorheological abnormalities in arterial hypertension and their relation to cardiac hypertrophy. J Hypertens 1988; 6: 293–297.
Sugimori H, Tomoda F, Koike T, Kurosaki H, Masutani T, Ohara M, Kagitani S, Inoue H . Increased blood viscosity is associated with reduced renal function and elevated urinary albumin excretion in essential hypertensives without chronic kidney disease. Hypertens Res 2013; 36: 247–251.
Castelli WP, Anderson K . A population at risk. Prevalence of high cholesterol levels in hypertensive patients in the Framingham Study. Am J Med 1986; 80: 23–32.
Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J, ASCOT investigators. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial—Lipid Lowering Arm (ASCOT-LLA): a multicenter randomised controlled trial. Lancet 2003; 361: 1149–1158.
Kondo T, Osugi S, Shimokata K, Honjo H, Morita Y, Yamashita K, Maeda K, Muramatsu T, Shintani S, Matsushita K, Murohara T . Metabolic syndrome and all-cause mortality, cardiac events, and cardiovascular events: a follow-up study in 25 471 young- and middle-aged Japanese men. Eur J Cardiovasc Prev Rehabil 2011; 18: 574–580.
Sugimori H, Tomoda F, Koike T, Kinuno H, Kurosaki H, Masutani T, Inoue H . Blood rheology and platelet function in untreated early-stage essential hypertensives complicated with metabolic syndrome. Int J Hypertens 2012; 2012 109830; doi:10.1155/2012/109830.
Brook RD, Julius S . Autonomic imbalance, hypertension, and cardiovascular risk. Am J Hypertens 2000; 13: 112S–122S.
Høieggen A, Fossum E, Moan A, Enger E, Kjeldsen SE . Whole-blood viscosity and the insulin-resistance syndrome. J Hypertens 1998; 16: 203–210.
Sloop GD, Garber DW . The effects of low-density lipoprotein and high-density lipoprotein on blood viscosity correlate with their association with risk of atherosclerosis in humans. Clin Sci (Lond) 1997; 92: 473–479.
Koenig W, Sund M, Ernst E, Mraz W, Hombach V, Keil U . Association between rheology and components of lipoproteins in human blood. Results from the MONICA project. Circulation 1992; 85: 2197–2204.
Slyper A, Le A, Jurva J, Gutterman D . The influence of lipoproteins on whole-blood viscosity at multiple shear rates. Metabolism 2005; 54: 764–768.
Hirayama S, Miida T . Small dense LDL: an emerging risk factor for cardiovascular disease. Clin Chim Acta 2012; 414: 215–224.
Ai M, Otokozawa S, Asztalos BF, Ito Y, Nakajima K, White CC, Cupples LA, Wilson PW, Schaefer EJ . Small dense LDL cholesterol and coronary heart disease: results from the Framingham Offspring Study. Clin Chem 2010; 56: 967–976.
St-Pierre AC, Cantin B, Dagenais GR, Mauriège P, Bernard PM, Després JP, Lamarche B . Low-density lipoprotein subfractions and the long-term risk of ischemic heart disease in men: 13-year follow-up data from the Québec Cardiovascular Study. Arterioscler Thromb Vasc Biol 2005; 25: 553–559.
Arai H, Kokubo Y, Watanabe M, Sawamura T, Ito Y, Minagawa A, Okamura T, Miyamato Y . Small dense low-density lipoproteins cholesterol can predict incident cardiovascular disease in an urban Japanese cohort: the Suita study. J Atheroscler Thromb 2013; 20: 195–203.
ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens 2013; 31: 1925–1938.
Teramoto T, Sasaki J, Ueshima H, Egusa G, Kinoshita M, Shimamoto K, Daida H, Biro S, Hirobe K, Funahashi T, Yokote K, Yokode M . Executive summary of Japan Atherosclerosis Society (JAS) guideline for diagnosis and prevention of atherosclerotic cardiovascular diseases for Japanese. J Atheroscler Thromb 2007; 14: 45–50.
Brun JF . Hormones, metabolism and body composition as major determinants of blood rheology: potential pathophysiological meaning. Clin Hemorheol Microcirc 2002; 26: 63–79.
Contreras T, Vaya A, Palanca S, Sola E, Corella D, Aznar J . Influence of plasmatic lipids on the hemorheological profile in healthy adults. Clin Hemorheol Microcirc 2004; 30: 423–425.
Wannamethee SG, Lowe GD, Shaper AG, Rumley A, Lennon L, Whincup PH . The metabolic syndrome and insulin resistance: relationship to haemostatic and inflammatory markers in older non-diabetic men. Atherosclerosis 2005; 181: 101–108.
Wannamethee SG, Tchernova J, Whincup P, Lowe GD, Kelly A, Rumley A, Wallace AM, Sattar N . Plasma leptin: associations with metabolic, inflammatory and haemostatic risk factors for cardiovascular disease. Atherosclerosis 2007; 191: 418–426.
de Simone G, Devereux RB, Chien S, Alderman MH, Atlas SA, Laragh JH . Relation of blood viscosity to demographic and physiologic variables and to cardiovascular risk factors in apparently normal adults. Circulation 1990; 81: 107–117.
Aloulou I, Varlet-Marie E, Mercier J, Brun JF . Hemorheological disturbances correlate with the lipid profile but not with the NCEP-ATPIII score of the metabolic syndrome. Clin Hemorheol Microcirc 2006; 35: 207–212.
Fons C, Brun JF, Supparo I, Mallard C, Bardet L, Orsetti A . Evaluation of blood viscosity at high shear rate with a falling ball viscometer. Clin Hemorheol 1993; 13: 651–659.
Quemada D . Rheology of concentrated disperse systems. II. A model of non-newtonian shear viscosity in steady flows. Rheologica Acta 1978; 17: 632–642.
Ito Y, Fujimura M, Ohta M, Hirano T . Development of a homogeneous assay for measurement of small dense LDL cholesterol. Clin Chem 2011; 57: 57–65.
Stamos TD, Rosenson RS . Low high density lipoprotein levels are associated with an elevated blood viscosity. Atherosclerosis 1999; 146: 161–165.
Moriarty PM, Gibson CA . Association between hematological parameters and high-density lipoprotein cholesterol. Curr Opin Cardiol 2005; 20: 318–323.
Irace C, Carallo C, Scavelli F, Esposito T, De Franceschi MS, Tripolino C, Gnasso A . Influence of blood lipids on plasma and blood viscosity. Clin Hemorheol Microcirc 2013; 23445635.
Zicha J, Kunes J, Devynck MA . Abnormalities of membrane function and lipid metabolism in hypertension: a review. Am J Hypertens 1999; 12: 315–331.
Leng GC, Smith FB, Fowkes FG, Horrobin DF, Ells K, Morse-Fisher N, Lowe GD . Relationship between plasma essential fatty acids and smoking, serum lipids, blood pressure and haemostatic and rheological factors. Prostaglandins Leukot Essent Fatty Acids 1994; 51: 101–108.
Terano T, Hirai A, Hamazaki T, Kobayashi S, Fujita T, Tamura Y, Kumagai A . Effect of oral administration of highly purified eicosapentaenoic acid on platelet function, blood viscosity and red cell deformability in healthy human subjects. Atherosclerosis 1983; 46: 321–331.
Rizzo M, Kotur-Stevuljevic J, Berneis K, Spinas G, Rini GB, Jelic-Ivanovic Z, Spasojevic-Kalimanovska V, Vekic J . Atherogenic dyslipidemia and oxidative stress: a new look. Transl Res 2009; 153: 217–223.
Law MR, Wald NJ, Rudnicka AR . Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. Br Med J 2003; 326: 1423–1427.
Prospective Studies Collaboration Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, Halsey J, Qizilbash N, Peto R, Collins R . Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55 000 vascular deaths. Lancet 2007; 370: 1829–1839.
Tan KC, Ai VH, Chow WS, Chau MT, Leong L, Lam KS . Influence of low density lipoprotein (LDL) subfraction profile and LDL oxidation on endothelium-dependent and independent vasodilation in patients with type 2 diabetes. J Clin Endocrinol Metab 1999; 84: 3212–3216.
Sharma SB, Garg S . Small dense LDL: risk factor for coronary artery disease (CAD) and its therapeutic modulation. Indian J Biochem Biophys 2012; 49: 77–85.
Richter WO, Jacob BG, Ritter MM, Sühler K, Vierneisel K, Schwandt P . Three-year treatment of familial heterozygous hypercholesterolemia by extracorporeal low-density lipoprotein immunoadsorption with polyclonal apolipoprotein B antibodies. Metabolism 1993; 42: 888–894.
Banyai S, Banyai M, Falger J, Jansen M, Alt E, Derfler K, Koppensteiner R . Atorvastatin improves blood rheology in patients with familial hypercholesterolemia (FH) on long-term LDL apheresis treatment. Atherosclerosis 2001; 159: 513–519.
Jaeger BR . Evidence for maximal treatment of atherosclerosis: drastic reduction of cholesterol and fibrinogen restores vascular homeostasis. Ther Apher 2001; 5: 207–211.
Acknowledgements
We thank Yumi Ohta for her technical assistance in measuring blood hemorheological indices.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Takiwaki, M., Tomoda, F., Koike, T. et al. Increased levels of small dense low-density lipoprotein cholesterol associated with hemorheological abnormalities in untreated, early-stage essential hypertensives. Hypertens Res 37, 1008–1013 (2014). https://doi.org/10.1038/hr.2014.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.111
Keywords
This article is cited by
-
An increase in calculated small dense low-density lipoprotein cholesterol predicts new onset of hypertension in a Japanese cohort
Hypertension Research (2023)
-
SLC12A3 variants modulate LDL cholesterol levels in the Mongolian population
Lipids in Health and Disease (2017)
-
Erythrocyte rheological properties but not whole blood and plasma viscosity are associated with severity of hypertension in older people
Zeitschrift für Gerontologie und Geriatrie (2017)
-
Hemorheological profiles of subjects with prehypertension
Hypertension Research (2016)
-
Metabolomic signatures in atherosclerotic disease: what is the potential use?
Hypertension Research (2016)