Abstract
Antihypertensive drugs have been linked to new-onset atrial fibrillation (NAF); however, the way in which these drugs affect the development of NAF in hypertensive patients has not been thoroughly examined. Herein, we report a population-based study in which we investigated the relationship between antihypertensive drug therapy and the risk of NAF. The population sample consisted of 47 682 hypertensive patients identified from claim forms provided to the central regional branch of the Bureau of National Health Insurance in Taiwan between January 2005 and December 2010. Prescriptions for antihypertensive drugs prescribed before the index date were retrieved from a prescription database. From these data, we estimated the hazard ratio (HR) of NAF associated with antihypertensive drug use; non-NAF subjects served as the reference group. After adjusting for age and sex, we observed that the risk of NAF was higher among the patients taking diuretics (HR, 1.39; 95% confidence interval (CI), 1.06–1.82) compared with the patients not taking diuretics. Patients who took angiotensin-converting enzyme (ACE) inhibitors (HR, 0.79; 95% CI, 0.65–0.97) showed a lower risk of developing NAF compared with the nonusers of ACE inhibitors. Angiotensin receptor blockers, alpha-blockers, beta-blockers and calcium channel blockers were not associated with a risk of NAF. The results of this study suggest that hypertensive patients who take diuretics have a significant increase in the risk of NAF, whereas patients who take ACE inhibitors are at lower risk of NAF.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common type of cardiac arrhythmia1 and is responsible for considerable morbidity and mortality worldwide.2, 3 Numerous studies have demonstrated that certain classes of antihypertensive medications can affect the development of new-onset atrial fibrillation (NAF).4, 5, 6, 7, 8, 9, 10 However, reports on the relationship between antihypertensive drugs and the risk of NAF show inconsistent results. There is a paucity of data from studies comparing large groups of patients taking more than two classes of antihypertensive medications.4, 5, 6, 7, 8, 10 Therefore, we conducted a retrospective cohort study to explore the relationship between antihypertensive drugs and NAF in the general population. We conducted a retrospective study in a population from central Taiwan examining whether diuretics, alpha-blockers, beta-blockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) were independently associated with NAF.
Methods
Study design, setting and participants
The data were obtained from claim forms provided to the central regional branch of the Bureau of National Health Insurance (BNHI) in Taiwan between January 2005 and December 2010. The BHNI stores information from the claim forms in two tables: a visit table and a prescription table. The visit table contains information regarding patient identification numbers, sex, age, three diagnostic codes, medical expenditures and information regarding the treating hospital and physician. The prescription table contains the quantity and the cost of a patient’s medications, operations and treatments. Patients were included in the study if they had hypertension treated with monotherapy without AF at baseline (1 January 2005). We summarized the data from the individual claim records into one record.
We used the International Classification of Diseases, Ninth Revision (ICD-9), Clinical Modification codes to define hypertension (ICD-9 codes 401–405) and AF (ICD-9 codes 427.31). The primary end point was NAF, which was defined as the first time that an AF code appeared in the patient’s diagnostic codes in the outpatient claim records. We identified all prescriptions for antihypertensive drugs administered to patients within a 6-year period before the date that NAF was diagnosed. In Taiwan, these drugs are available only by prescription. Patients who had used only one type of antihypertensive drug in the 90 days before the date that NAF was diagnosed were categorized according to their prescribed antihypertensive drug class: diuretics, alpha-blockers, beta-blockers, calcium channel blockers, ACE inhibitors, and ARBs. Patients using more than one type of antihypertensive drug in the 90 days before the date that NAF was diagnosed were categorized as combined users. Patients were excluded if: (1) missing data could not be obtained from their claim forms; (2) they had a diagnosis of paroxysmal AF between 1 January 2003, and 1 January 2005; (3) the patients were not available for follow-up or died during the study period; or (4) they had a diagnosis of heart failure, coronary heart disease, valvular heart disease, thyrotoxicosis, alcoholism or chronic obstructive pulmonary disease at any time during the study period. Initially (in January 2005), 47 860 patients between the ages of 20 and 80 years were identified from the claim forms provided to the central regional branch of the BNHI. We excluded 178 patients who were unavailable for follow-up or had died. A total of 47 682 outpatients were selected for this study (Figure 1).
Drug classes
The antihypertensive drugs were categorized into six drug classes (alpha-blockers, ACE inhibitors, ARBs, beta-blockers, calcium channel blockers and diuretics). There are 43 drugs in the alpha-blocker class, 132 drugs in the ACE inhibitor class, 9 drugs in the ARBs class, 279 drugs in the beta-blocker class, 228 drugs in the calcium channel blocker class and 205 drugs in the diuretics class.
Statistical methods
The statistical analyses were conducted using SAS 9.0 (SAS Institute, Cary, NC, USA). The central tendency and variability of the continuous variables are presented as the mean±s.d. The means of the variables were compared with the Welch’s t-test. The categorical and discrete variables are presented as frequencies and percentages; when appropriate, these data were compared with Fisher’s exact test or with the chi-square test. This study was designed to determine the relationship between antihypertensive drug classes and the incidence of NAF. Multivariate analyses, such as Kaplan–Meier and Cox survival analyses, were used to compare the hazard ratio (HR) of the NAF group with the HR of the non-NAF group. A P-value of <0.05 was considered statistically significant.
Results
Incidence and baseline characteristics
Of the 47 682 patients included in the study, 819 (1.72%) developed NAF. The mean age of the patients was 61.7±12.4 years; the mean age was significantly different between the NAF (69.7±10.0 years) group and the non-NAF (61.5±12.3 years; P<0.001) group. Women comprised more than half (25 571, 53.6%) of the sample population. There was a significant difference in the sex between the NAF group and the non-NAF group (male 50.4% vs. 46.3%, P=0.031). Of the 47 682 patients, 17 914 patients (37.6%) took calcium blockers, 11 372 patients (23.8%) took beta-blockers, 8614 patients (18.1%) took ACE inhibitors, 4215 patients (8.8%) took diuretics, 3073 patients (6.4%) took ARB and 2494 (5.2%) patients took alpha-blockers.
There were significant differences in the number of NAF and non-NAF patients taking alpha-blockers (7.6% vs. 5.2%, P=0.020), ACE inhibitors (13.3% vs. 18.1%, P=0.015), beta-blockers (20.1% vs. 23.9%, P=0.045), calcium channel blockers (39.8% vs. 37.5%, P=0.025) and diuretics (14.0% vs. 8.8%, P<0.001). The number of patients taking ARBs was not significantly different between the two groups (5.3% vs. 6.5%, P=0.365). As for baseline concomitant medications, there were no significant differences between the two groups for patients taking aspirin, lipid-lowering agents or statins (Table 1).
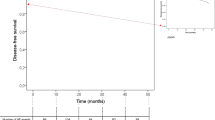
Cox survival univariate analysis
The risk estimate of NAF for patients taking ACE inhibitors (HR, 0.73; 95% confidence interval (CI), 0.60–0.90) and beta-blockers (HR, 0.84; 95% CI, 0.70–1.00) was lower (P<0.05) than the risk for non-users. ARBs (HR, 0.83; 95% CI, 0.54–1.29) and calcium channel blockers (HR, 1.15; 95% CI, 0.99–1.33) were not associated with an increased risk of NAF (P>0.05). Alpha-blockers (HR, 1.70; 95% CI, 1.19–2.49) and diuretics (HR, 1.76; 95% CI, 1.34–2.30) had the highest risk estimates for NAF (P<0.05; Figure 2).
Cox survival analysis adjusted for age and sex
After adjusting for age and sex, the patients who took diuretics (HR, 1.39; 95% CI, 1.06–1.82) had a higher conditional HR than the patients who did not take diuretics. Alpha-blockers (HR, 1.20; 95% CI, 0.83–1.73), beta-blockers (HR, 1.08; 95% CI, 0.91–1.29), ARBs (HR, 0.90; 95% CI, 0.58–1.38) and calcium channel blockers (HR, 0.98; 95% CI, 0.85–1.14) were not associated with an increased risk of NAF (P>0.05). ACE inhibitors (HR, 0.79; 95% CI, 0.65–0.97) had the lowest risk estimates for NAF (P<0.05; Figure 2).
Discussion
The present study demonstrates that diuretics are independently associated with an increased risk of NAF in patients with hypertension without heart failure. The use of ACE inhibitors was independently associated with a decreased risk of NAF. Alpha-blockers, beta-blockers, calcium channel blockers and ARBs were not associated with NAF.
To the best of our knowledge, this is the first study showing that diuretics are associated with a high risk of NAF in hypertensive outpatients. Disertori et al.11 demonstrated using their ‘Gruppo Italiano per lo Studio della Sopravvivenza neII’Infarto Miocardico-Atrial Fibrillation’ (GISSI-AF) study population that diuretics were independently associated with an increased risk of AF recurrence. Heckbert et al.10 reported that ACE inhibitors or ARBs were associated with a decreased risk of NAF compared with the risk associated with diuretic use (adjusted odds ratio (OR) 0.63; 95% CI 0.44–0.91). The occurrence of hypokalemia might explain the association between diuretic therapy and NAF; diuretic therapy may induce hypokalemia and facilitate atrial beats by re-entry or automatic mechanisms.12, 13 Other mechanisms that might be involved in this proarrhythmic effect are ventricular electrical instability and serious ventricular arrhythmias in ischemic heart disease.12 AF can be induced with diuretic administration in patients with intra-atrial conduction defects or in bypass patients. AF is more likely to occur with accelerated repolarization of the atrial muscle, which can result from hypokalemia.13 However, the relationship between diuretic treatment in patients with hypertension and the proarrhythmic effects with NAF has not been examined.11
Beta-blockers may decrease the risk of NAF via several mechanisms. These drugs might have a positive effect on premature atrial contractions because of the decrease in sympathetically mediated effects on automaticity and conduction; the decreases in these sympathetically mediated effects result in inhibited renin secretion and decreased atrial remodeling.14, 15, 16, 17 Many studies have reported that the use of beta-blockers is independently associated with a decreased risk of NAF.17 Differences between our findings and the findings of Schaer et al.17 might be attributed to the older age of patients in their study sample and their decision to exclude individuals with clinical risk factors from their study. However, our results are similar to those of a case–control study by the Group Health Cooperative in Washington, USA.10 In that study, 2320 patients (810 AF cases and 1512 controls) without heart failure were treated for hypertension between 1 October 2001 and 31 December 2004. The authors found that single-drug use of beta-blockers was not significantly associated with NAF (OR 1.05; 95% CI 0.73–1.52).
The renin–angiotensin–aldosterone system has an important role in AF. Evidence shows that blocking the renin–angiotensin–aldosterone system with ACE inhibitors and ARBs has a definite role in preventing NAF and in maintaining sinus rhythm in patients with recurrent AF.18, 19, 20, 21 In our study, we found that ARBs were not associated with NAF, and ACE inhibitors had a protective effect in outpatients with hypertension; however, this result could have been caused by the relatively small sample size of patients taking ARBs (6.4%) and the fact that these patients did not have underlying heart failure. Our results concerning ARBs are the same as the reports from a case–control study by the General Practice Research Database in the United Kingdom.10 That study showed that adults aged ⩾18 years with hypertension who were single-drug users of ACE inhibitors or ARBs were not at an increased risk of NAF (relative risk: 1.04; 95% CI: 0.93–1.17). However, our results regarding ACE inhibitors are similar to those reported by Schaer et al.,17 who found that the use of ACE inhibitors was associated with a decrease in the incidence of NAF (OR: 0.75; 95% CI: 0.65–0.87) compared with patients taking calcium channel blockers for the treatment of hypertension in a typical care setting.
Some studies have reported that the use of calcium channel blockers is independently associated with an increased risk of NAF.17, 22 However, Heckbert et al.10 reported that single-drug use of calcium channel blockers was not significantly associated with an increased risk of NAF (adjusted OR: 0.76; 95% CI: 0.45–1.29). Similarly, our findings showed that the use of calcium channel blockers was not significantly associated with an increased risk of NAF. A potential explanation for the association between calcium channel blocker therapy and NAF is the differences in the baseline comorbidities of the patients.23
In this study, alpha-blockers were not found to be associated with NAF in outpatients with hypertension. No previous studies have reported that alpha-blockers are not associated with a risk of NAF, and to the best of our knowledge, this is the first to show that alpha-blockers are not associated with a risk of NAF.
Our findings provide some support for the hypothesis that different antihypertensive drugs are associated with different levels of risk of developing NAF. Our results show that outpatients with hypertension who take ACE inhibitors are at a lower risk of developing NAF than are hypertensive patients who take other classes of antihypertensive drugs. Diuretics were associated with a significant increase in the risk of NAF.
Study limitations
Two limitations in this study need to be addressed. First, this was a retrospective and descriptive study in central Taiwan over a period of 6 years. Our analyses excluded untreated hypertensive participants. Thus caution must be exercised in interpreting our data.
Second, all the cases in this study were collected from secondary data of the claim data sets of primary care clinics under the central BNHI in Taiwan. We performed analyses restricted to participants who reported for regular follow-up during the study; therefore, it is not clear how our findings can be generalized to patients in different areas.
References
Hennersdorf MG, Schueller PO, Strauer BE . Prevalence of paroxysmal atrial fibrillation depending on the regression of left ventricular hypertrophy in arterial hypertension. Hypertens Res 2007; 30: 535–540.
Wolf PA, Abbott RD, Kannel WB . Atrial fibrillation as an independent risk for stroke: the Framingham Study. Stroke 1991; 22: 983–988.
Miyasaka Y, Barnes ME, Elailey KR, Cha SS, Gersh BJ, Seward JB, Tsang TSM . Mortality trends in patients diagnosed with first atrial fibrillation: a 21-year community-base study. J Am Coll Cardiol 2007; 49: 986–992.
Hansson L, Lindholm LH, Niskanen L, Lanke J, Hedner T, Niklason A, Luomanmäki K, Dahlöf B, Faire U, Mörlin C, Karlberg BE, Wester PO, Björck JE . Effect of angiotensin-converting- enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomized trial. Lancet 1999; 353: 611–616.
Wachtell K, Lehto M, Gerdts E, Olsen MH, Hornestam B, Dahlo'f B, Ibsen H, Julius S, Kjeldsen SE, Lindholm LH, Nieminen MS, Devereux RB . Angiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) study. J Am Coll Cardiol 2005; 45: 712–719.
Healey JS, Baranchuk A, Crystal E, Morillo CA, Garfinkle M, Yusuf S, Connolly SJ . Prevention of atrial fibrillation with angiotensin- converting enzyme inhibitors and angiotensin receptor blockers: a meta-analysis. J Am Coll Cardiol 2005; 45: 1832–1839.
Anand K, Mooss AN, Hee TT, Mohiuddin SM . Meta-analysis: inhibition of renin-angiotensin system prevents new-onset atrial fibrillation. Am Heart J 2006; 152: 217–222.
Nasr IA, Bouzamondo A, Hulot JS, Dubourg O, Le Heuzey JY, Lechat P . Prevention of atrial fibrillation onset by beta-blocker treatment in heart failure: a meta-analysis. Eur Heart J 2007; 28: 457–462.
Dorian P, Singh BN . Upstream therapies to prevent atrial fibrillation. Eur Heart J 2008; 10 (suppl H): H11–H31.
Heckbert SR, Wiggins KL, Glazer NL, Dublin S, Psaty BM, Smith NL, Longstreth WT Jr, Lumley T . Antihypertensive treatment with ACE inhibitors or beta-blockers and risk of incident atrial fibrillation in a general hypertensive population. Am J Hypertens 2009; 22: 538–544.
Disertori M, Lombardi F, Barlera S, Latini R, Maggioni AP, Zeni P, Pasquale GD, Cosmi F, Franzosi MG . Clinical predictors of atrial fibrillation in the Gruppo Italiano per lo Studio della Sopravvivenza nell’lnfarto Miocardico-Atrial Fibrillation’ (GISSI-AF) trial. Am Heart J 2010; 159: 857–863.
Emara MK, Saadet AM . Transient atrial fibrillationin hypertensive patients with thiazide induced hypokalemia. Postgrad Med 1986; 62: 1125–1127.
Schauerte P, Scherlag BJ, Patterson E, Scherlag MA, Matsudaria K, Nakagawa H, Lazzara R, Jackman WM . Focal atrial fibrillation: experimental evidence for a pathophysiologic role of the autonomic nervous system. J Cardiovasc Electrophysiol 2001; 12: 592–599.
Law MR, Wald NJ, Morris JK, Jordan RE . Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ 2003; 326: 1427–1435.
Pesaro AE, de Matos Soeiro A, Serrano CV, Giraldez RR, Ladeira RT, Nicolau JC . Effect of beta-blockers on the risk of atrial fibrillation in patients with acute myocardial infarction. Clinics (Sao Paulo) 2010; 65: 265–270.
Hodgkinson JA, Taylor CJ, Hobbs FDR . Predictors of incident atrial fibrillation and influence of medications: a retrospective case-control study. Br J Gen Pract 2011; 61: e353–e361.
Schaer BA, Schneider C, Jick SS, Conen D, Osswald S, Meier CR . Risk for incident atrial fibrillation in patients who receive antihypertensive drugs. Ann Intern Med 2010; 152: 78–84.
Vermes E, Tardif JC, Bourassa MG, Racine N, Levesque S, White M, Guerra PG, Ducharme A . Enalapril decreases the incidence of atrial fibrillation in patients with left ventricular dysfunction: insight from the Studies Of Left Ventricular Dysfunction (SOLVD) trials. Circulation 2003; 107: 2926–2931.
Maggioni AP, Latini R, Carson PE, Singh SN, Barlera S, Glazer R, Glazer R, Masson S, Cerè E, Tognoni G, Cohn JN, for the Val-HeFT Investigators. Valsartan reduces the incidence of atrial fibrillation in patients with heart failure: results from the Valsartan Heart Failure Trial (Val-HeFT). Am Heart J 2005; 149: 548–557.
Ducharme A, Swedberg K, Pfeffer MA, Cohen-Solal A, Granger CB, Maggioni AP, Michelson EL, McMurray JJV, Olsson L, Rouleau JL, Young JB, Olofsson B, Puu M, Yusuf S, on behalf of the CHARM Investigators. Prevention of atrial fibrillation in patients with symptomatic chronic heart failure by candesartan in the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) program. Am Heart J 2006; 152: 86–92.
Cuspidi C, Negri F, Zanchetti A . Angiotensin II receptor blockers and cardiovascular protection: focus on left ventricular hypertrophy regression and atrial fibrillation prevention. Vasc Health Risk Manag 2008; 4: 67–73.
L’Allier PL, Ducharme A, Keller PF, Yu H, Guertin MC, Tardif JC . Angiotensin-converting enzyme inhibition in hypertensive patients is associated with a reduction in the occurrence of atrial fibrillation. J Am Coll Cardiol 2004; 44: 159–164.
Webb AJS, Rothwell PM . Blood pressure variability and risk of new-onset atrial fibrillation: a systematic review of randomized trial of antihypertensive drugs. Stroke 2010; 41: 2091–2093.
Acknowledgements
This study was supported by the Taichung Armed Forces General Hospital.
Author contributions
G-PJ was the main investigator, collected the data, wrote the first draft, and prepared the final manuscript. H-YC and Y-sL were the study supervisors. S-YL was the study advisor. All of the authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
All the authors report receiving lecture fees from various pharmaceutical companies in Taiwan.
Rights and permissions
About this article
Cite this article
Jong, GP., Chen, HY., Li, SY. et al. Long-term effect of antihypertensive drugs on the risk of new-onset atrial fibrillation: a longitudinal cohort study. Hypertens Res 37, 950–953 (2014). https://doi.org/10.1038/hr.2014.104
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.104
Keywords
This article is cited by
-
Renin–angiotensin blockade in atrial fibrillation: where are we now?
Journal of Human Hypertension (2017)
-
Preventive effect of renin-angiotensin system inhibitors on new-onset atrial fibrillation in hypertensive patients: a propensity score matching analysis
Journal of Human Hypertension (2017)
-
How to evaluate BP measurements using the oscillometric method in atrial fibrillation: the value of pulse rate variation
Hypertension Research (2016)
-
Comparison of the effects of barnidipine+losartan compared with telmisartan+hydrochlorothiazide on several parameters of insulin sensitivity in patients with hypertension and type 2 diabetes mellitus
Hypertension Research (2015)