Abstract
The majority of the patients enrolled in the rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation (J-ROCKET AF) trial had hypertension. In this subgroup analysis, we investigated differences in the safety and efficacy of rivaroxaban and warfarin in subjects with and without hypertension. The baseline blood pressure (BP) measurements of patients with hypertension in the rivaroxaban and warfarin groups were 130/77 mm Hg and 131/77 mm Hg, respectively, whereas those of patients without hypertension were 123/74 mm Hg and 124/73 mm Hg, respectively. The incidence rates of the principal safety outcomes in the rivaroxaban and warfarin groups were 18.39% per year and 16.81% per year, respectively, among patients with baseline hypertension (hazard ratio (HR): 1.10; 95% confidence interval (CI): 0.84–1.45) and 16.71% per year and 15.00% per year, respectively, among patients without hypertension at baseline (HR: 1.14; 95% CI: 0.66–1.97), indicating no significant interaction (P=0.933). The incidence rates of the primary efficacy endpoints in the rivaroxaban group and the warfarin group were 0.54% per year and 2.24% per year, respectively, in patients without baseline hypertension (HR: 0.25; 95% CI: 0.03–2.25), and 1.45% per year and 2.71% per year, respectively, in patients with baseline hypertension (HR: 0.54; 95% CI: 0.25–1.16), indicating no significant interaction (P=0.509). In conclusion, the safety and efficacy profile of rivaroxaban was similar to that of warfarin, independent of baseline hypertensive status.
Similar content being viewed by others
Introduction
The prevalence and incidence of atrial fibrillation (AF), one of the most common diseases worldwide, is steadily increasing as the global population ages.1 The presence of AF is strongly associated with the increased risk of stroke and thromboembolism, and in Japan, the morbidity and mortality associated with stroke are still higher than those associated with ischemic heart disease or myocardial infarction.2
Hypertension is an independent risk factor for stroke, myocardial infarction and chronic kidney disease. The prevalence of hypertension in Japan, which has increased as the population ages, is now approximately 40 million.3 Studies in Europe and the US have also shown that hypertension causes an approximately 1.5-fold increase in the risk of developing AF.4 Moreover, because hypertension increases the risk of thromboembolism in patients with AF, blood pressure (BP) management is critical in these patients.5, 6
For patients with AF, warfarin has traditionally been the only clinically available oral anticoagulant that allows effective reduction in the risk of stroke and non-central nervous system (CNS) systemic embolism. Recently, however, the new anticoagulant rivaroxaban, which inhibits thrombus formation by direct inhibition of Factor Xa through a mechanism of action that is different from that of warfarin,7, 8, 9 has been approved and now offers a new treatment option for patients with AF.
The J-ROCKET AF trial compared the safety and efficacy of rivaroxaban with those of dose-adjusted warfarin among Japanese patients with AF, in accordance with the Japanese AF guidelines from The Japanese Circulation Society.10 The J-ROCKET AF trial was conducted in patients with a moderate or high risk of stroke and who presented with a CHADS2 score of ⩾2. Hypertension, which affected approximately 80% patients enrolled in this trial, is a risk factor contributing to the CHADS2 score. In this subgroup analysis of J-ROCKET AF, the safety and efficacy of rivaroxaban and of dose-adjusted warfarin were investigated in the presence or absence of baseline hypertension.
Methods
Study design, participants and procedure
The design and results of J-ROCKET AF have been described previously.10 In brief, J-ROCKET AF was a prospective, randomized, double-blind, double-dummy, parallel-group, active-controlled, multicenter clinical trial comparing the safety of rivaroxaban with that of dose-adjusted warfarin used in accordance with Japanese guidelines in patients with non-valvular AF. The study was approved by the Institutional Review Boards and all patients gave informed consent. The trial was conducted in accordance with Japanese Good Clinical Practice. Japanese patients aged ⩾20 years with non-valvular AF (documented electrocardiographically ⩽30 days before enrollment) were randomized at 167 participating facilities in Japan. Patients had a history of prior ischemic stroke, transient ischemic attack (TIA), or non-CNS systemic embolism, or had two or more of the following risk factors for thromboembolism: congestive heart failure and/or left ventricular ejection fraction of ⩽35%, hypertension (defined as use of antihypertensive medications within 6 months before the screening visit, persistent systolic BP >140 mm Hg or diastolic BP >90 mm Hg), age ⩾75 years, or diabetes mellitus (that is, a history of type 1 or type 2 diabetes mellitus or the use of anti-diabetic medications ⩽6 months before screening visit). Enrollment of patients without prior stroke, TIA or non-CNS systemic embolism and with only two risk factors for stroke was limited to 10% of the total number of target patients. Patients with creatinine clearance <30 ml min−1 were excluded, and patients with sustained, uncontrolled hypertension (systolic BP ⩾180 mm Hg or diastolic BP ⩾100 mm Hg) were also excluded.
Patients were randomized to receive either 15 mg oral rivaroxaban once daily (10 mg once daily in patients with creatinine clearance 30–49 ml min−1 at randomization) or dose-adjusted warfarin, to achieve a target INR of 2.0–3.0 (in patients aged <70 years, or a reduced target INR of 1.6–2.6 in patients aged ⩾70 years, based on the Japanese guidelines). The pre-specified maximum exposure period was 30 months. At the end-of-study visit (or at an early discontinuation visit), patients were transitioned from study medication to open-label commercial warfarin or other appropriate therapy by the investigator, according to usual clinical practice. Follow-up assessments of patients were completed at the follow-up visit (performed 30 days after the end-of-study visit) or at an early discontinuation visit.
Outcomes
The principal safety outcome was the composite of major bleeding events and non-major clinically relevant bleeding events.
The primary efficacy endpoint was the composite of stroke and non-CNS systemic embolism. An independent clinical endpoint committee adjudicated all the suspected cases of stroke, systemic embolism, myocardial infarction, death and bleeding events that contributed to the pre-specified endpoints.
Statistical analysis
Although the study was not designed to test efficacy hypotheses, efficacy endpoints were evaluated in an exploratory manner after treatment in the per-protocol population (patients in the safety population without any major protocol violations). The primary objective of the J-ROCKET AF trial was to test whether rivaroxaban was non-inferior to warfarin, with respect to the principal safety outcome in the safety population, as evaluated by non-stratified Cox proportional hazards modeling. Safety outcomes were analyzed in the safety population, which included all patients who had received ⩾1 dose of the investigational drug. In this subgroup analysis, the population for analysis was divided into two groups (based on the presence or absence of hypertension), and the safety outcomes and rate of the efficacy endpoints were compared between the groups.
The time to event was assessed using the Kaplan–Meier method and by determining the hazard ratio (HR) of rivaroxaban vs. warfarin, with its 95% CIs assessed using the Cox proportional hazard model. For conducting analysis using the Cox proportional hazards regression model, factors including a history of hypertension, treatment groups and the interaction of treatment groups were considered as covariates, to assess the interaction between the differential effects of rivaroxaban and of warfarin on the events in patients with and without hypertension.
Results
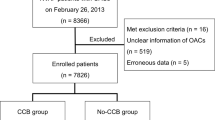
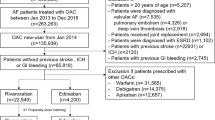
Patient characteristics
The rate of patients with baseline hypertension was 79.5% (508/639 patients) in the rivaroxaban group, which was equal to that in the warfarin group (79.5%; 508/639 patients), as shown in Table 1. The mean baseline BPs in the rivaroxaban and warfarin groups were 130/77 mm Hg and 131/77 mm Hg, respectively, in patients with baseline hypertension, and 123/74 mm Hg and 124/73 mm Hg, respectively, in patients without baseline hypertension. The mean CHADS2 scores were 3.4 in the group with hypertension and 2.7 in the group without hypertension. In addition, the rates of prior history of congestive heart failure and diabetes (which are also risk factors contributing to the CHADS2 score) were higher in the group with hypertension. The rate of prior history of stroke/TIA, conversely, tended to be higher in patients without hypertension. The rate of administration of antihypertensive medication at baseline did not differ between the rivaroxaban and the warfarin groups (Table 2).
Safety outcomes
The event rates of the principal safety outcomes in the rivaroxaban and warfarin groups were 18.39% per year and 16.81% per year, respectively, in patients with baseline hypertension (HR: 1.10; 95% CI: 0.84–1.45) and 16.71% per year and 15.00% per year, respectively, in patients without baseline hypertension (HR: 1.14; 95% CI: 0.66–1.97), which indicates no significant interaction (P=0.933). In the rivaroxaban group, patients without hypertension showed a marginally favorable trend of the incidence rates of major bleeding events compared with patients with hypertension; however, there were no significant differences in incidence rates between the warfarin and rivaroxaban groups (HR 0.25; 95% CI: 0.03–2.23 and HR: 0.93; 95% CI: 0.54–1.62, respectively; P-value for interaction: 0.249) (Figures 1a and b).
Principal safety outcomes in the safety population in the on-treatment analysis according to hypertensive status. (a) Principal safety outcomes in patients with and without hypertension. (b) Kaplan–Meier curve of time to first major bleeding event or first non-major clinically relevant bleeding event. CI, confidence interval; HR, hazard ratio; N/A, not applicable.
With regards to intracranial hemorrhage (ICH), which is one of the most serious of all bleeding events, 14/15 patients in the overall population presented with baseline hypertension (5/5 in the rivaroxaban group, 9/10 in the warfarin group). The mean baseline BP of patients with ICH was 139/82 mm Hg in the rivaroxaban group and 134/83 mm Hg in the warfarin group. The mean CHADS2 scores of patients with ICH was 3.8 in both the rivaroxaban and the warfarin groups. The rate of ICH was higher in patients with a history of prior stroke/TIA than in those with baseline hypertension (with or without ICH), as shown in Table 3.
Efficacy outcomes
The incidence rates of the primary efficacy endpoints in the rivaroxaban and warfarin groups were 0.54% per year and 2.24% per year, respectively, in patients without baseline hypertension (HR: 0.25; 95% CI: 0.03–2.25), and 1.45% per year and 2.71% per year, respectively, in patients with baseline hypertension (HR: 0.54; 95% CI: 0.25–1.16); this indicates no significant interaction (P=0.509). The incidence of the primary efficacy endpoint (stroke or non-CNS systemic embolism) was consistent with rivaroxaban, independent of the patient’s baseline hypertensive status.
Discussion
Our results confirmed that the efficacy and safety of rivaroxaban, as evaluated in the J-ROCKET AF study, is consistent in the subgroup of patients with AF and baseline hypertension and in the overall study population. In addition, in both the rivaroxaban and warfarin groups, the rates of the principal safety outcome (major or non-major bleeding) and the primary efficacy endpoint (stroke/non-CNS systemic embolism) were higher in patients with hypertension than in those without hypertension.
Stroke and blood pressure management
As discussed above, rivaroxaban reduces the rate of the primary efficacy endpoint (stroke or non-CNS systemic embolism), independent of baseline hypertensive status. However, in the rivaroxaban group, patients with hypertension had three times higher incidence of primary endpoints than those without. In addition, in the rivaroxaban group, patients without hypertension showed a marginally favorable trend of the frequency of major bleeding events compared with those with hypertension. Moreover, all patients with ICH had baseline hypertension, except for one patient in the warfarin group. The patients with ICH had higher baseline BP and higher CHADS2 scores, and were therefore at higher risk of stroke (Table 3). Hypertensive status is also an important component of the HAS-BLED score,11 a bleeding risk score that has recently been recommended by international guidelines (from the European Society of Cardiology12 and the Canadian Cardiovascular Society13) to assess bleeding risk. These factors suggest that stringent BP management is required for administering anticoagulant therapy.
Development of AF and the control of blood pressure
Hypertension is the risk factor most closely associated with the onset of AF.4 In particular, left ventricular hypertrophy and left atrial enlargement are independent risk factors for new-onset AF, and the reduction of left ventricular hypertrophy by anti-hypertensive therapy has been shown to decrease the incidence of new-onset AF.14 These pathologies are associated with the renin-angiotensin system (RAS) centering on angiotensin II as an accelerating factor. Several clinical studies have reported previously that inhibition of the RAS suppressed at least the new onset of AF.15, 16 On the basis of these results, inhibition of the RAS was expected to be developed into a novel AF therapy; however, multiple clinical studies17, 18, 19, 20 and their meta-analyses produced varied results. First, inhibitors of the RAS did not suppress new-onset AF in patients with hypertension but without left ventricular hypertrophy or cardiac failure. Second, efficacy was not demonstrated in patients who had already been diagnosed with AF in a study investigating the preventative effect of angiotensin receptor blockers on the recurrence of AF; this indicated that the efficacy of RAS inhibition against AF was not as high as initially expected. Although there is at present no anti-hypertensive drug that specifically inhibits new-onset AF, the current consensus is that the BP itself should be reduced (regardless of the concomitant use of anti-hypertensive drugs) in all patients with hypertension, including those with existing AF.
Limitations
First, as noted above (‘Method’), hypertension was defined as use of antihypertensive medications ⩽6 months before the screening visit, persistent systolic BP >140 mm Hg or diastolic BP >90 mm Hg. This means that, in this study, some patients with hypertension were already taking anti-hypertensive medications at baseline (Table 2). In addition, patients with sustained uncontrolled hypertension (systolic BP ⩾180 mm Hg or diastolic BP ⩾100 mm Hg) were excluded, which could have influenced the results, because this fact suggests that the patients with hypertension who were included in this trial are fairy well controlled.
The second factor that could have influenced the results of this trial is the timing of BP assessment. In the BAT (Bleeding with Antithrombotic Therapy) trial,21 which was also conducted in Japan, BP—when measured during the administration of anticoagulant therapy—was independently associated with development of ICH, after adjustment for established ICH predictors. Several large-scale clinical studies have reported that baseline BP could not be considered a predictor of major bleeding events.6, 22, 23 Nevertheless, only baseline BP could be assessed in this trial. At present, in Japan, a post-marketing surveillance of rivaroxaban is being conducted, with the planned number of enrolled patients set at 10 000. We expect this surveillance to produce further data showing the significance of the use of anti-hypertensive therapy in conjunction with the use of rivaroxaban in clinical practice, by assessing the BP not only at the time of patient enrollment but also during the course of treatment and, in addition, before the onset of major bleeding events.
In conclusion, the safety and efficacy of rivaroxaban vs. dose-adjusted warfarin were consistent, regardless of the baseline BP.
References
Wolf PA, Abbott RD, Kannel WB . Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch Intern Med 1987; 147: 1561–1564.
Ueshima H . Explanation for the Japanese paradox: prevention of increase in coronary heart disease and reduction in stroke. J Atheroscler Thromb 2007; 14: 278–286.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H, Japanese Society of Hypertension Committee. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Kannel WB, Wolf PA, Benjamin EJ, Levy D . Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 1998; 82: 2N–9N.
Rienstra M, Van Veldhuisen DJ, Crijns HJ, Van Gelder IC, RACE Investigators. Enhanced cardiovascular morbidity and mortality during rhythm control treatment in persistent atrial fibrillation in hypertensives: data of the RACE study. Eur Heart J 2007; 28: 741–751.
Lip GY, Frison L, Grind M, SPORTIF Investigators. Effect of hypertension on anticoagulated patients with atrial fibrillation. Eur Heart J 2007; 28: 752–759.
Kubitza D, Becka M, Roth A, Mueck W . Dose-escalation study of the pharmacokinetics and pharmacodynamics of rivaroxaban in healthy elderly subjects. Curr Med Res Opin 2008; 24: 2757–2765.
Kubitza D, Becka M, Wensing G, Voith B, Zuehlsdorf M . Safety, pharmacodynamics, and pharmacokinetics of BAY 59-7939—an oral, direct Factor Xa inhibitor—after multiple dosing in healthy male subjects. Eur J Clin Pharmacol 2005; 61: 873–880.
Perzborn E, Strassburger J, Wilmen A, Pohlmann J, Roehrig S, Schlemmer KH, Straub A . In vitro and in vivo studies of the novel antithrombotic agent BAY 59-7939—an oral, direct Factor Xa inhibitor. J Thromb Haemost 2005; 3: 514–521.
Hori M, Matsumoto M, Tanahashi N, Momomura S, Uchiyama S, Goto S, Izumi T, Koretsune Y, Kajikawa M, Kato M, Ueda H, Iwamoto K, Tajiri M, J-ROCKET AF study investigators. Rivaroxaban vs warfarin in Japanese patients with atrial fibrillation - the J-ROCKET AF study. Circ J 2012; 76: 2104–2111.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY . A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010; 138: 1093–1100.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Hindricks G, Kirchhof P, ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 2012; 33: 2719–2747.
Skanes AC, Healey JS, Cairns JA, Dorian P, Gillis AM, McMurtry MS, Mitchell LB, Verma A, Nattel S, Canadian Cardiovascular Society Atrial Fibrillation Guidelines Committee. Focused 2012 update of the Canadian Cardiovascular Society atrial fibrillation guidelines: recommendations for stroke prevention and rate/rhythm control. Can J Cardiol 2012; 28: 125–136.
Okin PM, Wachtell K, Devereux RB, Harris KE, Jern S, Kjeldsen SE, Julius S, Lindholm LH, Nieminen MS, Edelman JM, Hille DA, Dahlöf B . Regression of electrocardiographic left ventricular hypertrophy and decreased incidence of new-onset atrial fibrillation in patients with hypertension. JAMA 2006; 296: 1242–1248.
Wachtell K, Lehto M, Gerdts E, Olsen MH, Hornestam B, Dahlöf B, Ibsen H, Julius S, Kjeldsen SE, Lindholm LH, Nieminen MS, Devereux RB . Angiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) study. J Am Coll Cardiol 2005; 45: 712–719.
Anand K, Mooss AN, Hee TT, Mohiuddin SM . Meta-analysis: inhibition of renin-angiotensin system prevents new-onset atrial fibrillation. Am Heart J 2006; 152: 217–222.
Yamashita T, Inoue H, Okumura K, Kodama I, Aizawa Y, Atarashi H, Ohe T, Ohtsu H, Kato T, Kamakura S, Kumagai K, Kurachi Y, Koretsune Y, Saikawa T, Sakurai M, Sato T, Sugi K, Nakaya H, Hirai M, Hirayama A, Fukatani M, Mitamura H, Yamazaki T, Watanabe E, Ogawa S, J-RHYTHM II Investigators. Randomized trial of angiotensin II-receptor blocker vs dihydropiridine calcium channel blocker in the treatment of paroxysmal atrial fibrillation with hypertension (J-RHYTHM II study). Europace 2011; 13: 473–479.
Goette A, Schon N, Kirchhof P, Breithardt G, Fetsch T, Häusler KG, Klein HU, Steinbeck G, Wegscheider K, Meinertz T . Angiotensin II-antagonist in paroxysmal atrial fibrillation (ANTIPAF) trial. Circ Arrhythm Electrophysiol 2012; 5: 43–51.
GISSI-AF Investigators Disertori M, Latini R, Barlera S, Franzosi MG, Staszewsky L, Maggioni AP, Lucci D, Di Pasquale G, Tognoni G . Valsartan for prevention of recurrent atrial fibrillation. N Engl J Med 2009; 360: 1606–1617.
ACTIVE I Investigators Yusuf S, Healey JS, Pogue J, Chrolavicius S, Flather M, Hart RG, Hohnloser SH, Joyner CD, Pfeffer MA, Connolly SJ . Irbesartan in patients with atrial fibrillation. N Engl J Med 2011; 364: 928–938.
Toyoda K, Yasaka M, Uchiyama S, Nagao T, Gotoh J, Nagata K, Koretsune Y, Sakamoto T, Iwade K, Yamamoto M, Takahashi JC, Minematsu K, Bleeding with Antithrombotic Therapy (BAT) Study Group. Blood pressure levels and bleeding events during antithrombotic therapy: the Bleeding with Antithrombotic Therapy (BAT) Study. Stroke 2010; 41: 1440–1444.
Bleeding during antithrombotic therapy in patients with atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators. Arch Intern Med 1996; 156: 409–416.
Gorter JW . Major bleeding during anticoagulation after cerebral ischemia: patterns and risk factors. Stroke Prevention In Reversible Ischemia Trial (SPIRIT). European Atrial Fibrillation Trial (EAFT) study groups. Neurology 1999; 53: 1319–1327.
Acknowledgements
The rivaroxaban clinical development program is co-sponsored by Janssen Pharmaceuticals (Raritan, NJ, USA) and Bayer HealthCare Pharmaceuticals AG (Leverkusen, Germany). The trial was funded by Bayer HealthCare Pharmaceuticals AG’s Japanese subsidiary, Bayer Yakuhin. Dr Hori has received consultancy fees from Bayer, Boehringer Ingelheim, Bristol Myers-Squibb and Pfizer. Dr Matsumoto and Dr Momomura have received consultancy fees from Bayer. Dr Tanahashi has received consultancy fees from Bayer and Mitsubishi Tanabe, and honoraria from Mitsubishi Tanabe and Sanofi-Aventis. Dr Uchiyama has received consultancy fees from Bayer and Boehringer Ingelheim and research grants from Bayer, Boehringer Ingelheim and Daiichi-Sankyo. Dr Goto has received research grants from Astellas, AstraZeneca, Daiichi, Eisai, Kowa, Ono, Otsuka, Pfizer, Sanofi-Aventis, and Takeda, and honoraria from Daiichi-Sankyo, Eisai, Otsuka, Sanofi-Aventis and Schering-Plough. Dr. Izumi has received consultancy fees from Bayer and Pfizer. Dr Koretsune has received honoraria from Bayer, Boehringer Ingelheim, Daiichi-Sankyo and Bristol Myers-Squibb. Drs Iekushi, Yamanaka, Kajikawa and Ueda, and Mr Tajiri and Mr Kato report employment by Bayer Yakuhin. No other conflicts of interest are reported.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Matsumoto, M., Hori, M., Tanahashi, N. et al. Rivaroxaban versus warfarin in Japanese patients with non-valvular atrial fibrillation in relation to hypertension: a subgroup analysis of the J-ROCKET AF trial. Hypertens Res 37, 457–462 (2014). https://doi.org/10.1038/hr.2014.1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.1
Keywords
This article is cited by
-
Novel Oral Anticoagulants for the Prevention of Stroke in Patients with Atrial Fibrillation and Hypertension: A Meta-Analysis
American Journal of Cardiovascular Drugs (2019)