Abstract
Salt-reduction guidance to hypertensive patients should be performed by evaluating salt intake of the individuals. However, each method to assess salt intake has both merits and limitations. Therefore, evaluation methods must be selected in accordance with the subject and facility’s environment. In special facilities for hypertension treatment, measurement of sodium (Na) excretion with 24-h pooled urine or a survey on dietary contents by dietitians is recommended. In medical facilities in general, measurement of the levels of Na and creatinine (Cr) using second urine samples after waking-up or spot urine samples is recommended. The reliability of this method improves by using formulae including a formula to estimate 24-h Cr excretion. A method to estimate salt intake based on the Na excretion per gram Cr using the Na/Cr ratio in spot urine is simple, but not reliable. The method to estimate the daily excretion of salt from nighttime urine using an electronic salt sensor installed with a formula is recommended to hypertensive patients. Although its reliability is not high, patients themselves can measure this parameter simply at home and thus useful for monitoring salt intake and may intensify consciousness regarding salt reduction. Using these methods, salt intake (excretion) should be evaluated, and salt-reduction guidance targeting <6 g (Na: 100 mmol) per day should be conducted in the management of hypertension.
Similar content being viewed by others
Introduction
The relationship between salt and hypertension is clear. However, excessive salt intake may cause not only hypertension but also various diseases, such as stroke, heart failure, nephropathy and gastric cancer. Therefore, dietary salt restriction must be promoted not only in hypertensive patients but also in general population. The salt intake in Japanese is still higher than in various countries. According to the National Health and Nutritional Survey in 2010, the mean salt intake in males and females aged 20 years or older was 11.4 and 9.8 g per day, respectively.1 In the ‘Dietary Intake Standards in Japanese (2010 version)’ issued by the Ministry of Health, Labor and Welfare, it was proposed that the target levels of salt intake in males (12 years or older) and females (10 years or older) at the national level should be <9 and 7.5 g per day, respectively.2 However, the attainment rates in male and female adults in 2009 were 31.6 and 29.8%, respectively.1 On the other hand, a target salt-restriction level of <6 g per day in hypertensive patients was proposed in the Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH2009).3 However, the target attainment rate is extremely low.4, 5
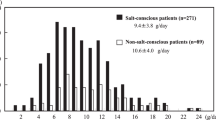
It is commonly recognized that, among lifestyle modifications for hypertension, salt reduction is most important. However, a study reported that there was only a slight difference in the urinary salt excretion related to the presence or absence of consciousness regarding salt reduction, suggesting that consciousness regarding salt reduction does not always contribute to actual salt restriction (Figure 1).6 Thus, it is essential to evaluate salt intake in individuals for salt-reduction guidance. In other words, guidance to achieve the target should be conducted after the assessment of salt intake, and effective salt-reduction guidance may be accomplished by evaluating the response. The assessment of salt intake is classified into two types: dietary surveys by dietitians and monitoring of the urinary sodium (Na) level. Various procedures are used in accordance with environments, such as clinical practice regarding hypertension treatment or clinical/epidemiological studies. However, reliable assessment methods are generally difficult to perform.
Consciousness regarding salt reduction and actual salt excretion (quoted from Ohta et al.6).
The Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension (current name: Salt Reduction Committee) published a report on the ‘Assessment of Salt Intake in the Management of Hypertension’ in 2006.7 In this article, we introduce the type and characteristics of methods to assess salt intake, which are available, based on the subsequent study results, and propose their application in hypertension treatment.
Assessment of salt intake
The assessment of salt intake is classified into two types: assessment based on the dietary contents and the urinary excretion of Na. However, concerning the two procedures, simple methods are not reliable (Table 1). Furthermore, the whole volume of ingested salt is not excreted in urine, and ∼10–20% is lost in the digestive tract or as sweat. Therefore, it must be considered that the urinary excretion of Na is lower than the actual salt intake. Na is an important factor for hypertension. Its greater portion is ingested as salt (sodium chloride: NaCl). One gram of salt corresponds to 17 mmol of Na (17 mEq), and 6 g of salt to ∼100 mmol of Na. In the Health Promotion Law, it is described that the Na level should be expressed in the food composition. However, it must be considered that the actual salt level is 2.54 times higher (Na at 400 mg corresponds to ∼1 g of salt).
Assessment based on the dietary contents
Analysis from a prepared meal
The daily salt intake can be calculated by preparing a surplus meal for one person and scientifically analyzing the Na content of this meal. This method is highly reliable if performed precisely. The accuracy of hospital and test meals for clinical research is sometimes confirmed using this method. However, specific procedures are required for sample preparation, and relatively high expenditure is required for analysis. Therefore, this method is not appropriate for long-term or large-scale strategies.
Diet-recording method
The weights and volumes of foods to be ingested are measured/recorded in scientific units using a balance and measuring cup/spoon, or values described on the container are recorded, and salt intake is calculated using the Food Composition Table. Among dietary survey methods, this is highly reliable. However, an interview by dietitians and calculation require much time; therefore, it is difficult to evaluate salt intake for a long period. This method is not always appropriate for frequent use in long-term intervention studies to verify the effects of salt-reduction guidance or clinical practice.
Twenty-four hour recall method
Foods ingested by each person the previous day or within the past 24 h are ascertained by an interviewer, and salt intake is calculated using the Food Composition Table. If adequate training for interviewers, standardization of survey procedures and accuracy of management are maintained, then the Na level obtained is similar to the actual analytical value, and is correlated with Na excretion in 24-h urine.8, 9
Survey on the frequency of food ingestion and diet history
A questionnaire involving foods that are frequently consumed is prepared to investigate the frequency of consumption during a specific period (the past 1 month) and food intake per meal using writing or interview methods. This method is simpler than diet-recording and 24-h recall methods. However, it has some limitations: the assessment of salt intake is limited; and the same questionnaire cannot be used in a population in which the dietary habit markedly differs. According to several studies, the assessment of salt intake with the semi-quantitative, self-administered diet history questionnaire, in which dietary contents during 1 month are investigated using a questionnaire, and quantitative, brief-type, self-administered diet history questionnaire is correlated with assessment based on the 24-h urine/dietary records, suggesting that this assessment method is useful as a tool for salt-reduction guidance.10, 11
Assessment with a salt sensor
It is possible to measure the concentration of salt in liquid foods to be ingested using a salt sensor at home, but it is difficult to assess salt intake unless the amount of food intake is simultaneously evaluated. However, this method may be available for strengthening/maintaining hypertensive patients’ consciousness regarding salt reduction (for example, this method should be used for measurement of the miso soup concentration of salt to enhance motivation for salt reduction).
Measurement of urinary Na excretion
Twenty-four hour urine collection
The excretion of Na measured using 24-h urine is the most reliable among all methods to assess salt intake. This parameter is used in epidemiological (INTERSALT) and clinical studies.12 There are two methods: methods with whole-urine collection and the collection using partition cup (Urinemate P, Sumitomo Bakelite Co., Ltd., Tokyo, Japan). The latter requires complex operations, but the collector can be easily taken on going-out or to the hospital. The assessment based on the 24-h urine is a gold standard to evaluate salt intake, but has some limitations: (1) this method is not simple, making repeated assessment difficult; (2) it is necessary to evaluate the validity of urine collection by assessing 24-h creatinine (Cr) excretion; and (3) urine collection may influence subjects’ dietary contents and activities, and the results of one session of measurement do not always reflect their daily diet. As a portion of ingested Na is lost in stools or sweat, as described above, the salt intake calculated from the 24-h urinary excretion of Na is ∼0.5–3 g lower than the actual intake.13
Nighttime urine
Measurement of Na excretion using urine collected at night or early morning urine, which consists of nighttime urine, is simpler than that using 24-h urine. It has been shown that there is a correlation between the nighttime and 24-h urinary excretions of Na. However, there are diurnal changes in Na excretion. As Na excretion at night is ∼20% lower than that during the daytime,14 it is necessary to estimate 24-h Cr excretion from the lean body mass, as well as 24-h Na excretion based on the nighttime urinary Na and Cr excretions using this value, for a more precise estimation.15 Furthermore, a study indicated that sympathetic activity was reduced at night, and that pressure natriuresis became marked.16 It must be considered that the nighttime urinary excretion of Na may have been influenced by blood pressure.
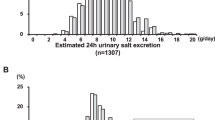
Recently, a ‘salt monitor’ to estimate 24-h salt excretion with an installed formula using 8-h nighttime urine was developed. It is applied in clinical practice as a method facilitating self-measurement.17 A study reported that the mean salt excretion self-measured for 30 days using the salt monitor was correlated with that measured five times using 24-h urine (Figure 2).18 The validity of values estimated using the salt monitor at various salt intake levels should be further investigated. However, it is possible to monitor the daily salt intake at home, and this method may be useful for motivating patients to reduce salt intake or maintain it.19
Relationship between the urinary salt excretion estimated from nighttime urine (mean during a 30-day period) and mean of 24-h urine samples collected five times (quoted from Ohta et al.18).
Second urine sample after waking-up
A study reported a method to measure the Na and Cr concentrations using a second urine sample after waking-up (within 4 h after waking-up, before eating breakfast), and estimate the 24-h urinary excretion of Na using a formula with the 24-h urinary excretion of Cr estimated from gender, height, body weight and age (Figure 3).20 This method may be more reliable than the spot urine-based estimation described below. In particular, when adding a postural condition to maintain the sitting or standing position after waking-up, the correlation with 24-h urine is enhanced, and the daily salt intake is consistent with the value estimated using 24-h urine.21 This assessment method may be useful in persons who can consult a physician early in the morning or in whom urine collection at home is possible.
Estimation of 24-h urinary sodium excretion using second urine samples after waking-up (quoted from Kawasaki et al.20 and partially modified).
Spot urine
For estimation with spot urine, in which there are no restrictions regarding the time of urine collection, an estimation formula prepared using the database from Japanese subjects who participated in the INTERSALT study is used (Figure 4).22 The estimated 24-h urinary excretion of Na, which was calculated using a formula involving the estimated 24-h urinary excretion of Cr, was favorably correlated with the actual excretion of Na. Its simplicity is a merit. However, as described above, there are diurnal changes in urinary Na excretion, and the influence of the diet cannot be avoided; therefore, the relationship between estimated and actual values may vary according to the time of urine collection or salt intake (Figure 5).23 Therefore, the reliability of the 24-h urinary Na excretion estimated using this procedure is limited.
Estimation of 24-h urinary sodium excretion using spot urine (quoted from Tanaka et al.22 and partially modified).
Relationship between the time of urine collection and estimated salt excretion with respect to various levels of salt intake (quoted from Kawamura et al.23).
Another method is to calculate Na excretion per gram Cr based on the spot urine levels of Na and Cr, and estimate the daily Na intake. Although its reliability is not high, this method is simple and clinically available as a parameter of motivation for salt-reduction or intensified guidance.
Test paper, salt sensor
A method to measure the spot or early morning urine concentrations of salt by detecting the concentration of chloride (Cl) using test paper or an electronic salt sensor, and estimate salt intake is the simplest.24 Although self-measurement is possible, the quantitativity and reliability of this method are low. Therefore, this method is used only to intensify consciousness regarding salt reduction. However, the values measured using nighttime urine by a salt monitor, as described above, may be reliable to some extent.
Assessment of salt intake for the management of hypertension
As described above, there are many procedures to evaluate salt intake. However, there is no highly reliable, simple method; therefore, an adequate procedure must be selected in accordance with the purpose of assessment, subjects and facility environments. Although the diet-recording method and assessment of urinary Na excretion with 24-h pooled urine are the most reliable, salt intake on a specific day is evaluated, and the results may not always reflect daily changes in salt intake. In contrast, estimation using spot urine or self-measurement with early morning urine (nighttime urine) is less reliable, but repeated measurement is possible. These methods are appropriate for evaluating a trend in salt intake in individual persons. Furthermore, it must be considered that urinary Na excretion is lower than the actual salt intake calculated using the weighing method.
The Salt Reduction Committee of the Japanese Society of Hypertension proposes the guidelines presented in Table 2 with respect to the assessment of salt intake for the management of hypertension.
Special facilities for hypertension treatment
In facilities involving hypertension specialists and dietitians, measurement of urinary Na excretion with 24-h pooled urine and assessment using the weighing method or a questionnaire by dietitians are the most reliable and recommendable. When evaluating salt intake with 24-h pooled urine, the validity of urine collection should be investigated by measuring 24-h urinary Cr excretion. As shown in Figure 6 decrease in salt excretion in hypertensive patients can be confirmed by repeating the evaluation of urinary Na excretion using 24-h urine collection and nutritional guidance.25 However, these procedures are difficult to perform frequently, and thus it is recommended to combine these with assessment using simpler methods, such as measurement with spot or nighttime urine, as described below.
Changes in salt excretion repeatedly measured using 24-h pooled urine (quoted from Ohta et al.25) 103 hypertensive patients in whom 24-h urine collection was performed 11.4 times (mean), with a mean follow-up of 8.6 years.
Medical facilities in general
In facilities or health checkup organizations in which it is difficult to conduct urine collection or a survey by dietitians, assessment with spot urine is simple, and can be readily performed. If conditions to collect urine can be specified, then assessment with second urine samples after waking-up (Figure 3) is recommendable. However, when it is difficult to establish conditions, assessment with spot urine should be carried out (Figure 4). To evaluate the effects of salt-reduction guidance in hypertensive patients, measurement under specific urine collection conditions is useful.
The estimation of Na excretion based on the Na/Cr ratio in spot urine is simple, but not reliable. The daily excretion of Cr in Japanese is ∼1 g (∼10 mmol).12 If Na excretion per gram Cr is 100 mmol (100 mEq), then salt intake may be ∼6 g. This may become a reference value for salt-intake screening or salt-reduction guidance. However, the urinary excretion of Cr depends on the age, gender and physical status; therefore, Na excretion estimated from the Na/Cr ratio may be overestimated in small females, and underestimated in large males. In this case, assessment using a formula to estimate 24-h Cr excretion should be considered.
Self-monitoring by patients
The reliability of a method to estimate the daily excretion of salt from nighttime urine using an electronic salt sensor installed with a formula is not high, but patients themselves can measure it simply. Therefore, this method is available for monitoring salt intake and intensifying consciousness regarding salt reduction. As shown in Figure 7, a study reported that serial measurement led to a decrease in salt excretion in the absence of special guidance or intervention.18
Changes in the self-measured values of 24-h urinary salt excretion estimated from nighttime urine (quoted from Ohta et al.18), hypertensive patients (n=34) and healthy adults (n=25), 59 subjects in total.
A method to measure the early morning/spot urine concentrations of salt using test paper is the simplest. However, its quantitativity is limited, and this method is not available for the evaluation of absolute values or the effects of salt-reduction guidance. Similarly, measurement of the food salt concentration using test paper or a salt sensor is also available as a tool for salt-reduction guidance, but not for the estimation of salt intake.
Conclusion
The salt intake-assessing methods have merits and limitations. Although there is no reliable, simple method, it is important to evaluate salt intake, for performing salt-reduction guidance. Therefore, evaluation methods must be selected in accordance with the subject and facility’s environment. For the management of hypertension, it is strongly recommended to evaluate salt intake using one of the following methods:
-
1)
In special facilities for hypertension treatment, measurement of Na excretion with 24-h pooled urine or a survey on dietary contents by dietitians is recommended.
-
2)
In medical facilities in general, measurement of the levels of Na and Cr using second urine samples after waking-up or spot urine samples is recommended. The reliability of this method improves by using formulae including a formula to estimate 24-h Cr excretion. A method to estimate salt intake based on the Na excretion per gram Cr using the Na/Cr ratio in spot urine is simple, but not reliable.
-
3)
The method to estimate the daily excretion of salt from nighttime urine using an electronic salt sensor installed with a formula is recommended to hypertensive patients. Although its reliability is not high, patients themselves can measure this parameter simply at home. This method is useful for monitoring salt intake and may intensify consciousness regarding salt reduction.
Using these methods, salt intake (excretion) should be evaluated, and salt-reduction guidance targeting <6 g (Na: 100 mmol) per day should be conducted in the management of hypertension.
References
Lifestyle-related Disease Control Section, General Affairs Division, Health Service Bureau, Ministry of Health, Labour and Welfare. Outline of the results of the National Health and Nutritional Survey in 2010, 2012.
Ministry of Health, Labour and Welfare. Dietary Intake Standards in Japanese [2010 version], Daiichi Shuppan, Tokyo 2009.
The Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009), Japanese Society of Hypertension, Tokyo 2009.
Ohta Y, Tsuchihashi T, Onaka U, Eto K, Tominaga M, Ueno M . Long-term compliance with salt restriction in Japanese hypertensive patients. Hypertens Res 2005; 28: 953–957.
Hashimoto T, Yagami F, Owada M, Sugawara T, Kawamura M . Salt preference according to a questionnaire vs dietary salt intake estimated by a spot urine method in participants at a health check-up center. Intern Med 2008; 47: 399–403.
Ohta Y, Tsuchihashi T, Ueno M, Kajioka T, Onaka U, Tominaga M, Eto K . Relationship between the awareness of salt restriction and the actual salt intake in hypertensive patients. Hypertens Res 2004; 27: 243–246.
Kawano Y, Tsuchihashi T, Matsuura H, Ando K, Fujita T, Ueshima H . Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: Assessment of Salt Intake in the Management of Hypertension. Japanese Society of Hypertension: Tokyo. 2006.
Yoshita K, Miura K, Okayama A, Okuda N, Schakel SF, Dennis B, Saitoh S, Sakata K, Nakagawa H, Stamler J, Ueshima H . A validation study on food composition tables for the international cooperative INTERMAP study in Japan. Environ Health Prev Med 2005; 10: 150–156.
Anderson CA, Appel LJ, Okuda N, Brown IJ, Chan QZ, Ueshima H, Kesteloot H, Miura K, Curb JD, Yoshita K, Elliott P, Yamamoto ME, Stamler J . Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc 2010; 110: 736–745.
Sasaki S, Yanagimori R, Amano K . Validity of a self-administered diet history questionnaire for assessment of sodium and potassium—Comparison with single 24-hour urinary excretion. Jpn Circ J 1998; 62: 431–435.
Kobayashi S, Honda S, Murakami K, Sasaki S, Okubo H, Hirota N, Notsu A, Fukui M, Date C . Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J Epidemiol 2012; 22: 151–159.
INTERSALT COOPERATIVE RESEARCH GROUP. INTERSALT: an international study of electrolyte excretion and blood pressure. Results for 24 h urinary sodium and potassium excretion. Br Med J 1998; 297: 319–328.
Kuft FC, Fineberg NS, Sloan RS . Estimating dietary sodium intake in individuals receiving a randomly fluctuating intake. Hypertension 1982; 4: 805–808.
Kawano Y, Kawasaki T, Kawazoe N, Abe I, Uezono K, Ueno M, Fukiyama K, Omae T . Circadian variations of urinary dopamine, norepinephrine, epinephrine and sodium in normotensive and hypertensive subjects. Nephron 1990; 55: 277–282.
Kamata K, Tochikubo O . Estimation of 24-h urinary sodium excretion using lean body mass and overnight urine collected by a pipe-sampling method. J Hypertens 2002; 20: 2192–2197.
Staessen J, Broughton PMG, Fletcher AE, Markowe HLJ, Marmot MG, Rose G, Semmence A, Shipley MK, Bulpitt CJ . The assessment of the relationship between blood pressure and sodium intake using whole-day, daytime and overnight urine collections. J Hypertens 1991; 9: 1035–1040.
Yamasue K, Tochikubo O, Kono E, Maeda H . Self-monitoring of home blood pressure with estimation of daily salt intake using a new electrical device. J Hum Hypertens 2006; 20: 593–598.
Ohta Y, Tsuchihashi T, Miyata E, Onaka U . Usefulness of self-monitoring of urinary salt excretion in hypertensive patients. Clin Exp Hypertens 2009; 31: 690–697.
Yasutake K, Sawano K, Yamaguchi S, Sakai H, Amadera H, Tsuchihashi T . Self-monitoring urinary salt excretion in adults: a novel education program for restricting dietary salt intake. Exp Ther Med 2011; 2: 615–618.
Kawasaki T, Itoh K, Uezono K, Sasaki H . A simple method for estimating 24 h urinary sodium and potassium excretion from second morning urine specimen in adults. Clin Exp Pharmacol Physiol 1993; 20: 7–14.
Kawamura M, Hashimoto T, Owada M, Sugawara T . The influence of posture on the estimate of daily salt intake by the second morning urine method. Hypertens Res 2010; 33: 505–510.
Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, Hashimoto T . A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens 2002; 16: 97–103.
Kawamura M, Ohmoto A, Hashimoto T, Yagami T, Owada M, Sugawara T . Second morning urine method is superior to the casual urine method for estimating daily salt intake in patients with hypertension. Hypertens Res 2012; 35: 611–616.
Luft FC, Aronoff GR, Sloan RS, Fineberg NS, Miller JZ, Free AH . The efficacy of quantitative and qualitative chloride titrators in the estimation of human salt intake. Klin Woch 1985; 63: 62–67.
Ohta Y, Tsuchihashi T, Onaka U, Miyata E . Long-term compliance of salt restriction and blood pressure control status in hypertensive outpatients. Clin Exp Hypertens 2010; 32: 234–238.
Acknowledgements
We thank the cooperative members of the Salt Reduction Committee of the Japanese Society of Hypertension, Katsushi Yoshita, Naohiko Watanabe, and Hiroo Kawarazaki, for their cooperation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsuchihashi, T., Kai, H., Kusaka, M. et al. [Scientific Statement]. Hypertens Res 36, 1026–1031 (2013). https://doi.org/10.1038/hr.2013.103
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2013.103
Keywords
This article is cited by
-
Changing views on the common physiologic abnormality that mediates salt sensitivity and initiation of salt-induced hypertension: Japanese research underpinning the vasodysfunction theory of salt sensitivity
Hypertension Research (2019)
-
Effective uric acid-lowering treatment for hypertensive patients with hyperuricemia
Hypertension Research (2017)
-
Self-management of salt intake: clinical significance of urinary salt excretion estimated using a self-monitoring device
Hypertension Research (2016)
-
Salt intake and eating habits of school-aged children
Hypertension Research (2016)
-
Current dietary salt intake of Japanese individuals assessed during health check-up
Hypertension Research (2015)