Abstract
A condition involving the growth of the myocardium that exceeds hemodynamic needs has been reported and called as inappropriate left ventricular mass (LVM). The appropriateness of LVM can be estimated by the ratio of observed LVM to predicted LVM. The excessive growth of LVM is frequently noted in patients with chronic kidney disease (CKD). This study is designed to assess whether the ratio of observed to predicted LVM is a useful prognostic indicator of cardiovascular events in patients with moderate to advanced CKD. We consecutively enrolled 485 patients with CKD stages 3–5 from our Outpatient Department of Internal Medicine. Inappropriate LVM was defined as observed LVM more than 28% greater than the predicted value. The relative risk of cardiovascular events was analyzed by Cox-regression methods. There was a significant trend for a stepwise increase in the observed/predicted LVM ratio (P<0.001) and the prevalence of inappropriate LVM (P=0.003) corresponding to advances in CKD stages. In the multivariate analysis, old age, a history of coronary artery disease, congestive heart failure, atrial fibrillation, wide pulse pressure, decreased serum albumin and hemoglobin levels, left atrial diameter >4.7 cm and increased observed/predicted LVM were independently associated with increased cardiovascular events. Our findings show that increased observed/predicted LVM is independently associated with adverse cardiovascular outcomes in patients with CKD stages 3–5.
Similar content being viewed by others
Introduction
Cardiovascular disease is the leading cause of morbidity and mortality in patients with chronic kidney disease (CKD).1 This excess cardiovascular risk in CKD can be attributed to several risk factors, such as proteinuria, fluid retention, anemia, oxidative stress and structural and functional abnormalities of the heart.1, 2, 3, 4
A number of hemodynamic and metabolic disturbances affect the structure and function of the heart in patients with CKD.5 To compensate for the hemodynamic and metabolic alterations, an excessive increase in the left ventricular mass (LVM), a condition that has been termed ‘inappropriate LVM’, is frequently found in patients with CKD.6 The predicted LVM based on sex, height2, 7 and hemodynamic load can be used as an appropriate reference for the observed LVM.7, 8 The appropriateness of the LVM can be estimated by the ratio of the observed LVM to the predicted LVM. Recently, the presence of inappropriate LVM has been found in a significant proportion of patients with arterial hypertension or aortic stenosis and has been reported to have a negative impact on cardiovascular prognosis.9, 10, 11, 12 In addition, inappropriate LVM is also strongly correlated with the presence and magnitude of CKD.7, 13 However, a limited number of studies have evaluated the association between observed/predicted LVM and cardiovascular events in patients with moderate to advanced CKD stages. Accordingly, the aims of this study were to assess the determinants of observed/predicted LVM and whether observed/predicted LVM is a useful prognostic indicator of cardiovascular events in patients with CKD stages 3–5.
Methods
Study patients and design
The study was conducted in a regional hospital in southern Taiwan. In total, 485 patients with CKD stages 3–5 were enrolled consecutively from our Outpatient Department of Internal Medicine from January 2007 to May 2010. Patients with evidence of kidney damage lasting for more than 3 months were classified as CKD stage 3, 4, or 5 based on an estimated glomerular filtration rate (eGFR) (ml min−1 per 1.73 m2) of 30–59, 15–29, or <15, respectively, as recommended in the National Kidney Foundation-Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines.14 Patients with significant mitral valve disease and inadequate image visualization were excluded. Patients on dialysis treatment were also excluded. The protocol for this study was approved by our Institutional Review Board, and all of the enrolled patients gave written informed consent.
Evaluation of cardiac structure and function
The echocardiographic examination was performed by two experienced cardiologists with a VIVID 7 ultrasound machine (General Electric Medical Systems, Horten, Norway), with the participant respiring quietly in the left decubitus position. The cardiologists were blind to the data for the patients. Two-dimensional and two-dimensionally guided M-mode images were recorded from the standardized views. The echocardiographic measurements included the left atrial (LA) diameter, left ventricular internal diameter in diastole (LVIDd), LVPWTd (left ventricular posterior wall thickness in diastole), IVSTd (interventricular septal wall thickness in diastole), E-wave deceleration time, peak early transmitral filling wave velocity (E), peak late transmitral filling wave velocity (A) and E/A ratio. Left ventricular systolic function was assessed by the left ventricular ejection fraction (LVEF) and midwall fractional shortening (mwFS).15 The observed LVM was calculated using the Devereux-modified method, that is, LVM=1.04 × [(IVSTd+LVIDd+LVPWTd)3−LVIDd3]−13.6 g.16 The left ventricular mass index (LVMI) was calculated by dividing the LVM by the body surface area. Left ventricular hypertrophy (LVH) was defined as suggested by the 2007 European Society of Hypertension/European Society of Cardiology guidelines.17 The LVRWT (left ventricular relative wall thickness) was calculated as the ratio of 2 × LVPWTd/LVIDd. Concentric LVH was defined as an LVMI of more than 125 g m−2 in men and more than 110 g m−2 in women, with an LVRWT of more than 0.45; eccentric LVH was defined as an LVMI of more than 125 g m−2 in men and more than 110 g m−2 in women, with an LVRWT of less than 0.45. Inappropriate LVM was also assessed as the ratio between the observed and predicted LVM (observed/predicted LVM). The predicted LVM was estimated using the following equation: predicted LVM=55.37+6.64 × height (m2.7)+0.64 × stroke work−18.07 × sex (in which sex was coded as male=1 and female=2).8 Stroke work was estimated as the product of the systolic blood pressure and the stroke volume and converted into gram meters by multiplying with 0.0144. The LVM was defined as ‘inappropriate’ when the observed LVM was more than 28% greater than the predicted value (that is, observed/predicted LVM >128%).7, 8
Collection of demographic, medical and laboratory data
Demographic and medical data, including age, gender, smoking history (ever vs. never) and comorbid conditions were garnered from medical records or interviews with patients. The BMI (body mass index) was calculated as the ratio of weight in kg to the square of height in meters. Blood and urine samples were obtained within 1 month of enrollment. Laboratory data were measured from fasting blood samples using an autoanalyzer (Roche Diagnostics GmbH (Mannheim, Germany), D-68298 Mannheim COBAS Integra 400). The serum creatinine was measured by the compensated Jaffé (kinetic alkaline picrate) method in a Roche/Integra 400 chemistry analyzer (Roche Diagnostics) using a calibrator traceable to isotope-dilution mass spectrometry.18 The value of eGFR was calculated using the 4-variable equation in the Modification of Diet in Renal Disease (MDRD) study.19 A test result of 1+ or more was defined as positive. In addition, information regarding patient medications, including angiotensin-converting enzyme inhibitors, angiotensin II-receptor blockers, β-blockers, calcium-channel blockers and diuretics during the study period, was obtained from medical records.
Definition of cardiovascular events
Cardiovascular events were defined as cardiovascular death, hospitalization for unstable angina, nonfatal myocardial infarction, sustained ventricular arrhythmia, hospitalization for congestive heart failure, transient ischemia attack and stroke. The cardiovascular events were ascertained and adjudicated by cardiologists from the hospital course and medical record. Patients who experienced cardiovascular events were followed until the first episode of cardiovascular events. The other patients were followed until February 2011.
Statistical analysis
The data are expressed as percentages or the mean± s.d. or median (25th–75th percentile) for triglyceride. The differences between two groups were checked by a chi-square test for categorical variables or by an independent t-test for continuous variables. The relationship between two continuous variables was assessed using a bivariate correlation method (Pearson’s correlation). Linear regression analysis was used to identify the factors associated with observed/predicted LVM. The time to cardiovascular events and the covariates of the risk factors were modeled using a Cox proportional hazards model. Significant variables in the univariate analysis were selected for a multivariate analysis. A P-value of less than 0.05 was considered to be significant. All of the statistical operations were performed using SPSS (Statistical Package for the Social Sciences) 12.0 for Windows (SPSS, Chicago, IL, USA).
Results
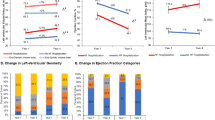
As can be seen in Table 1, a summary of baseline and echocardiographic characteristics, we studied 485 non-dialyzed patients with CKD (303 men and 182 women, mean age 66.0±12.3 years). The value of observed/predicted LVM was 156.6±54.1%, and the prevalence of inappropriate LVM was 68.5%. There was a significant trend for a stepwise increase in observed/predicted LVM (P<0.001 for trend) (Figure 1a) and the prevalence of inappropriate LVM (60.0%, 71.1% and 76.7%, respectively; P=0.003 for trend) (Figure 1b) corresponding to the advancement in chronic kidney disease from stage 3 to stage 5. In addition, Figure 2 shows the significant trend for a stepwise increase in LVMI (A) and in the prevalence of LVH (B) corresponding to the advancement in CKD from stage 3 to stage 5.
There was a significant trend for a stepwise increase in observed/predicted left ventricular mass (LVM) (P<0.001 for trend) (a) and the prevalence of inappropriate LVM (60.0%, 71.1% and 86.7%, respectively; P=0.003 for trend) (b) corresponding to the advancement in chronic kidney disease from stage 3 to stage 5.
There was a significant trend for a stepwise increase in left ventricular mass index (LVMI) (P<0.001 for trend) (a) and in the prevalence of left ventricular hypertrophy (LVH) (50.5%, 65.8% and 80.8%, respectively; P<0.001 for trend) (b) corresponding to the advancement in chronic kidney disease from stage 3 to stage 5.
Risk of inappropriate LVM and increased observed/predicted LVM
The comparison of baseline and echocardiographic characteristics between patients with appropriate and inappropriate LVMs is shown in Table 2. Compared with patients with appropriate LVM, patients with inappropriate LVM were significantly associated with a higher prevalence of diabetes, more advanced CKD stages, lower systolic blood pressure, lower pulse pressure, higher BMI, lower albumin, higher fasting glucose, lower hemoglobin, lower baseline eGFR, higher uric acid, greater use of diuretics and use of a higher number of antihypertensive drugs. In addition, patients with inappropriate LVM exhibited a higher prevalence of LA diameter >4.7 cm, higher prevalence of concentric LVH and eccentric LVH, higher observed/predicted LVM value, and higher prevalence of LVEF<50% and mwFS<14%.
As shown in Table 3, which summarizes our findings on the possible determinants of observed/predicted LVM in our study patients, the univariate analysis revealed a significant positive correlation between observed/predicted LVM and a history of coronary artery disease and congestive heart failure, advanced CKD stages, BMI, proteinuria, diuretics use, LA diameter >4.7 cm, concentric and eccentric LVH, LVEF<50% and mwFS<14% and a negative correlation between observed/predicted LVM and albumin and hemoglobin. Furthermore, the multivariate analysis revealed a significant correlation between increase in observed/predicted LVM and advanced CKD stages (P=0.01), high BMI (P<0.001), concentric LVH (P<0.001), eccentric LVH (P<0.001), LVEF<50% (P=0.002) and mwFS<14% (P<0.001).
Risk of increased cardiovascular events
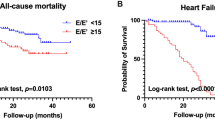
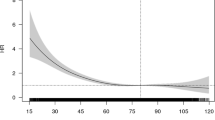
The follow-up period was 25.9±12.6 months in all patients and 28.6±11.1 months in patients without cardiovascular events. In all, 86 cardiovascular events were documented during the follow-up period, including cardiovascular death (n=11), hospitalization for unstable angina and nonfatal myocardial infarction (n=16), sustained ventricular arrhythmia (n=9), hospitalization for congestive heart failure (n=29) and transient ischemia attack and stroke (n=21). A Cox proportional hazards regression analysis for cardiovascular events is shown in Table 4. In the univariate regression analysis, old age, a history of diabetes, coronary artery disease, cerebrovascular disease, congestive heart failure, atrial fibrillation, high systolic blood pressure, wide pulse pressure, low albumin, low hemoglobin, low baseline eGFR, proteinuria, diuretic use, LA diameter >4.7 cm, concentric and eccentric LVH, increased observed/predicted LVM, decreased LVEF and decreased mwFS were significantly associated with an increase in cardiovascular events. In the multivariate forward analysis, old age, a history of coronary artery disease, congestive heart failure and atrial fibrillation, wide pulse pressure, decreased albumin, decreased hemoglobin, LA diameter >4.7 cm, and increased observed/predicted LVM (HR (hazard ratio), 1.004; 95% CI (confidence interval), 1.001–1.008, P=0.015) were independently associated with increased cardiovascular events. Figure 3 illustrates the Kaplan–Meier curves for cardiovascular event-free survival in patients subdivided according to inappropriate or appropriate LVM (log-rank P=0.036).
Because low LVEF could influence the calculation of inappropriate LVM, we performed a subgroup analysis after excluding 14 cases with LVEF<40% and found similar results, that is, increased observed/predicted LVM (HR, 1.004; 95% CI, 1.001–1.007, P=0.024) was independently associated with increased cardiovascular events.
Discussion
In this study, we evaluated the determinants of observed/predicted LVM and the impact of observed/predicted LVM on cardiovascular outcomes in patients with CKD stages 3–5. We found a significant trend for a stepwise increase in observed/predicted LVM and the prevalence of inappropriate LVM corresponding to advancement in CKD stages; we also noted that increased observed/predicted LVM was independently associated with an increase in cardiovascular events.
The hemodynamic and metabolic disturbances in patients with CKD may synergistically activate a variety of pathophysiological alterations, including hemodynamic abnormalities (that is, increased preload and afterload) and non-hemodynamic abnormalities (that is, neurohormonal stressors and factors promoting myocardial fibrosis and atherosclerosis), and thus result in the excessive growth of the LVM.1, 2, 3, 4, 20 Nardi et al.7 evaluated the prevalence of inappropriate LVM in CKD stage 2–5 patients with a mean eGFR of 39 ml min−1 per 1.73 m2 and found that patients with CKD had a higher prevalence of inappropriate LVM than hypertensive patients with normal renal function (52.6% vs. 30.5%, P<0.001). Cioffi et al.12 also studied the relationship between inappropriate LVM and renal function in patients with a mean eGFR of 67 ml min−1 per 1.73 m2 and found that there was an inverse relation between observed/predicted LVM and eGFR. In our study, we consistently demonstrated a significant trend for a stepwise increase in the observed/predicted LVM and in the prevalence of inappropriate LVM corresponding to advancement in CKD stages in patients with a mean eGFR of 26.1 ml min−1 per 1.73 m2. Additionally, CKD stage was still a major determinant of observed/predicted LVM after the multivariate analysis.
Previous studies have shown that inappropriate LVM is associated with several unfavorable cardiac characteristics, including concentric left ventricular geometry and decreased left ventricular systolic and diastolic function.21, 22 Chinali et al.9 have demonstrated that inappropriate LVM is associated with low LVEF, long isovolumic relaxation time and prolonged E-deceleration time in 359 hypertensive patients. Our study also demonstrated that concentric and eccentric LVH, LVEF<50% and mwFS<14% were significantly associated with increased observed/predicted LVM, consistent with previous findings.21, 22
Inappropriate LVM is associated with clusters of markers of cardiovascular risk.21, 22 Recently, an adverse impact of inappropriate LVM on cardiovascular outcomes has been observed in hypertensive patients.10, 11 For instance, de Simone et al.10 studied the impact of inappropriate LVM on cardiovascular prognosis in 294 hypertensive patients and found that inappropriate LVM predicted poor cardiovascular prognosis independently of age and systolic blood pressure. They also found that inappropriate LVM remained a significant predictor of cardiovascular events in a more complete model with a larger number of covariates in 1019 white hypertensive patients.11 Our study also demonstrated that increased observed/predicted LVM was significantly associated with increased cardiovascular events. Hence, observed/predicted LVM was a useful indicator of poor cardiovascular outcomes in patients with moderate to advanced CKD stages.
In this study, compared with patients with appropriate LVM, patients with inappropriate LVM had a narrower pulse pressure. This correlation has also been noted in previous studies,9, 23 in which patients with inappropriate LVM exhibited lower systolic blood pressure but comparable diastolic blood pressure relative to patients with appropriate LVM. The reasons for the negative association between pulse pressure and inappropriate LVM might be related to a higher number of antihypertensive drugs used and an early asymptomatic deterioration in cardiac pump function in patients with inappropriate LVM. Similarly, our patients with inappropriate LVM had used a higher number of antihypertensive drugs and had a higher prevalence of LVEF<50% and mwFS<14%, which might explain the negative correlation between pulse pressure and inappropriate LVM in the present study.
The calculation of predicted LVM is based on age, gender, height and stroke work. Thus, a single blood pressure measurement may have a great impact on the calculation of predicted LVM. An average ambulatory blood pressure over 24 h may be more closely related to LVM than a single clinical blood pressure measurement. In addition, low LVEF and low systolic blood pressure can also influence the calculation of predicted LVM. Therefore, we performed a subgroup analysis after excluding cases with LVEF<40% and still found that increased observed/predicted LVM was independently associated with increased cardiovascular events. Finally, treatment with antihypertensive drugs can potentially influence LV geometry and functional parameters. In particular, the use of diuretics may reduce LV diameter and thus cause a greater prevalence of inappropriate LVM. For ethical reasons, we did not withhold any drugs at the time of the echocardiography evaluation. However, to elucidate the influence of drugs, we had added different classes of antihypertensive drugs in the analysis and found that there was no association between antihypertensive drugs used and cardiovascular events in the multivariate analysis.
In conclusion, our study in patients with CKD stages 3–5 demonstrated that there was a significant trend for a stepwise increase in observed/predicted LVM and the prevalence of inappropriate LVM. Increased observed/predicted LVM was closely associated with advanced CKD stages and adverse cardiovascular outcomes. The ratio of observed LVM to predicted LVM may help identify a high-risk group for adverse cardiovascular outcomes in patients with CKD stages 3–5.
References
Ritz E . Heart and kidney: fatal twins? Am J Med 2006; 119: S31–S39.
Levin A, Singer J, Thompson CR, Ross H, Lewis M . Prevalent left ventricular hypertrophy in the predialysis population: identifying opportunities for intervention. Am J Kidney Dis 1996; 27: 347–354.
Levin A, Thompson CR, Ethier J, Carlisle EJ, Tobe S, Mendelssohn D, Burgess E, Jindal K, Barrett B, Singer J, Djurdjev O . Left ventricular mass index increase in early renal disease: impact of decline in hemoglobin. Am J Kidney Dis 1999; 34: 125–134.
Pedersen TR, Kjekshus J, Berg K, Haghfelt T, Faergeman O, Thorgeirsson G, Pyorala K, Miettinen T, Wilhelmsen L, Olsson AG, Wedel H . Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994; 344: 1383–1389.
Veves A, Akbari CM, Primavera J, Donaghue VM, Zacharoulis D, Chrzan JS, DeGirolami U, LoGerfo FW, Freeman R . Endothelial dysfunction and the expression of endothelial nitric oxide synthetase in diabetic neuropathy, vascular disease, and foot ulceration. Diabetes 1998; 47: 457–463.
Palmieri V, de Simone G, Roman MJ, Schwartz JE, Pickering TG, Devereux RB . Ambulatory blood pressure and metabolic abnormalities in hypertensive subjects with inappropriately high left ventricular mass. Hypertension 1999; 34: 1032–1040.
Nardi E, Palermo A, Mule G, Cusimano P, Cottone S, Cerasola G . Left ventricular hypertrophy and geometry in hypertensive patients with chronic kidney disease. J Hypertens 2009; 27: 633–641.
de Simone G, Devereux RB, Kimball TR, Mureddu GF, Roman MJ, Contaldo F, Daniels SR . Interaction between body size and cardiac workload: influence on left ventricular mass during body growth and adulthood. Hypertension 1998; 31: 1077–1082.
Chinali M, De Marco M, D'Addeo G, Benincasa M, Romano C, Galderisi M, de Simone G . Excessive increase in left ventricular mass identifies hypertensive subjects with clustered geometric and functional abnormalities. J Hypertens 2007; 25: 1073–1078.
de Simone G, Palmieri V, Koren MJ, Mensah GA, Roman MJ, Devereux RB . Prognostic implications of the compensatory nature of left ventricular mass in arterial hypertension. J Hypertens 2001; 19: 119–125.
de Simone G, Verdecchia P, Pede S, Gorini M, Maggioni AP . Prognosis of inappropriate left ventricular mass in hypertension: the MAVI Study. Hypertension 2002; 40: 470–476.
Cioffi G, Tarantini L, Frizzi R, Stefenelli C, Russo TE, Selmi A, Toller C, Furlanello F, de Simone G . Chronic kidney disease elicits excessive increase in left ventricular mass growth in patients at increased risk for cardiovascular events. J Hypertens 2011; 29: 565–573.
Muiesan ML, Salvetti M, Paini A, Monteduro C, Galbassini G, Bonzi B, Poisa P, Belotti E, Agabiti Rosei C, Rizzoni D, Castellano M, Agabiti Rosei E . Inappropriate left ventricular mass changes during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension 2007; 49: 1077–1083.
Levey AS, Coresh J, Bolton K, Culleton B, Harvey KS, Ikizler TA, Johnson CA, Kausz A, Kimmel PL, Kusek J, Levin A, Minaker KL, Nelson R, Rennke H, Stettes M, Witten B . K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39: S1–266.
Shimizu G, Conrad CH, Gaasch WH . Phase-plane analysis of left ventricular chamber filling and midwall fiber lengthening in patients with left ventricular hypertrophy. Circulation 1987; 75: I34–I39.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N . Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B . Management of arterial hypertension of the European Society of hypertension; European Society of Cardiology 2007 guidelines for the management of arterial hypertension. The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Vickery S, Stevens PE, Dalton RN, van Lente F, Lamb EJ . Does the ID-MS traceable MDRD equation work and is it suitable for use with compensated Jaffe and enzymatic creatinine assays? Nephrol Dial Transplant 2006; 21: 2439–2445.
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D . A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in Renal Disease Study Group. Ann Intern Med 1999; 130: 461–470.
Hunter JJ, Chien KR . Signaling pathways for cardiac hypertrophy and failure. N Engl J Med 1999; 341: 1276–1283.
de Simone G, Kitzman DW, Palmieri V, Liu JE, Oberman A, Hopkins PN, Bella JN, Rao DC, Arnett DK, Devereux RB . Association of inappropriate left ventricular mass with systolic and diastolic dysfunction: the HyperGEN study. Am J Hypertens 2004; 17: 828–833.
Mureddu GF, Pasanisi F, Palmieri V, Celentano A, Contaldo F, de Simone G . Appropriate or inappropriate left ventricular mass in the presence or absence of prognostically adverse left ventricular hypertrophy. J Hypertens 2001; 19: 1113–1119.
Palmieri V, Wachtell K, Gerdts E, Bella JN, Papademetriou V, Tuxen C, Nieminen MS, Dahlöf B, de Simone G, Devereux RB . Left ventricular function and hemodynamic features of inappropriate left ventricular hypertrophy in patients with systemic hypertension: the LIFE study. Am Heart J 2001; 141: 784–791.
Acknowledgements
The research presented in this article is supported by a grant from Kaohsiung Municipal Hsiao-Kang Hospital (kmhk-100-001), Kaohsiung Medical University, Kaohsiung, Taiwan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Chen, SC., Chang, JM., Liu, WC. et al. The ratio of observed to predicted left ventricular mass is independently associated with increased cardiovascular events in patients with chronic kidney disease. Hypertens Res 35, 832–838 (2012). https://doi.org/10.1038/hr.2012.40
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.40
Keywords
This article is cited by
-
Association between sleep quality and cardiovascular damage in pre-dialysis patients with chronic kidney disease
BMC Nephrology (2014)
-
Sex differences in the association between serum uric acid levels and cardiac hypertrophy in patients with chronic kidney disease
Hypertension Research (2014)
-
Inappropriately high left ventricular mass: marker of very high cardiovascular risk in patients with chronic kidney disease?
Hypertension Research (2012)