Abstract
Recently, the development of two-dimensional speckle-tracking (2DST) technology has allowed the direct measurement of the elastic parameters of the carotid arterial wall. The aims of this study were to determine the feasibility of measuring peak circumferential strain (CS) of the carotid arterial wall using 2DST and to compare this value with conventional arterial stiffness parameters in subjects with and without hypertension. The study included 90 healthy subjects and 40 age-and sex-matched patients with hypertension. The short-axis view of the right common carotid artery was recorded. The CS in the posterior region of the carotid artery was calculated by 2DST using special software and corrected by the following equation: ɛcirc=ln (systolic blood pressure/diastolic blood pressure)/CS. We simultaneously measured the stiffness index β (β) at the same location and the brachial-ankle pulse wave velocity (baPWV). Sixty randomly selected healthy subjects were used to assess the inter/intra-observer variability of ɛcirc and β. In healthy subjects, ɛcirc was significantly correlated with β, age and baPWV. These correlations were slightly better than the corresponding correlations of β with age and baPWV. The hypertensive patients had a significantly larger ɛcirc than the healthy subjects (0.112±0.074 vs. 0.066±0.029/%, P<0.001). The inter/intra-observer variability for ɛcirc was significantly lower than that for β. Our data suggest that the measurement of carotid ɛcirc using 2DST is feasible and has better reproducibility than conventional carotid arterial stiffness.
Similar content being viewed by others
Introduction
Increased arterial stiffness is one of the early manifestations of adverse structural and functional changes within the vessel wall and an important independent predictor of future adverse cardiovascular events and all-cause mortality in various populations.1, 2 In addition, several pharmacological and nonpharmacological interventions have been reported to improve arterial stiffness.2 Therefore, the simple, accurate measurement of arterial stiffness with high reproducibility is very important. Thus far, various noninvasive parameters of arterial stiffness have been evaluated using various devices.2 The stiffness index β (β) is one of the parameters of arterial stiffness determined by carotid ultrasound in the clinical setting. However, this parameter is estimated from the extension of the arterial wall based on the systolic and diastolic lumen diameter along with pulse pressure and does not take into account the expansion of the intima-media wall.
Recently, two-dimensional speckle-tracking (2DST) echocardiography has been shown to provide an angle-independent, well-validated method for strain measurement in human heart.3, 4, 5, 6, 7, 8, 9 Although this method can be applied to the human carotid arterial wall to directly assess arterial elasticity, it has not been well assessed. Therefore, the aims of this study were to evaluate the feasibility of direct measurement of peak circumferential strain (CS) of the carotid arterial wall using 2DST, to compare the reproducibility of CS with conventional arterial stiffness parameters in healthy subjects, and to compare CS between subjects with and without hypertension.
Methods
Study population
Ninety-four consecutive healthy subjects without risk factors for atherosclerosis such as hypertension, dyslipidemia, diabetes mellitus and current smoking were enrolled. In addition, 41 age- and sex-matched patients with hypertension were enrolled. The presence of risk factors for atherosclerosis were defined as follows: hypertension as systolic blood pressure ⩾140 mm Hg and/or diastolic blood pressure ⩾90 mm Hg measured at the time of ultrasound examination or current antihypertensive therapy; dyslipidemia as either serum low-density lipoprotein cholesterol ⩾140 mg dl−1, triglycerides ⩾150 mg dl−1, high-density lipoprotein cholesterol<40 mg dl−1 or current antilipid therapy; and diabetes mellitus as either serum fasting blood glucose ⩾126 mg dl−1, HbA1c⩾6.5% or current antiglycemic therapy. All patients were required to be in sinus rhythm at the time of the ultrasound examination. Exclusion criteria included subjects with known coronary artery disease, significant valvular heart disease, ejection fraction ≦60% as assessed by echocardiography, renal disease, stroke, significant peripheral vascular disease (ankle to brachial blood pressure ratio ≦0.9) and other disease conditions such as fever and malaise. Four healthy subjects and one patient with hypertension were excluded because of speckle-tracking failure with poor two-dimensional images. The remaining 90 healthy subjects and 40 patients with hypertension were included in the analysis. Several metabolic variables, including fasting blood glucose, HbA1c, insulin, total cholesterol, high-density lipoprotein cholesterol, triglycerides and low-density lipoprotein cholesterol levels, were measured in all participants on the morning of the ultrasound studies. All drugs were discontinued at least 24 h before evaluation in the patients with hypertension. This study was approved by the ethics committee of Ehime University Graduate School of Medicine, and all patients and subjects gave informed consent before participation.
Routine carotid ultrasound and echocardiographic examination
Subjects were examined in the morning (0830–0900 hours) after a 12-h overnight fast in a quiet, temperature-controlled laboratory (22 °C after 15 min of rest in the supine position. The ultrasound examinations were performed by two vascular ultrasound experts who were blinded to the subject’s identity and clinical profile. Ultrasound imaging was performed with a GE Vivid 7 ultrasound imaging system (GE Medical System, Milwaukee, WI, USA) with a high-resolution linear array transducer centered at 12 MHz (carotid) and a M4S probe (heart). All acquisitions were performed during short breath holding to minimize the effect of motion artifacts. The transducer was placed with the least possible pressure to avoid compressing the overlying jugular vein and to allow expansion of the carotid artery. The intima-media thickness (IMT) was obtained using B-mode imaging of the right common carotid artery in the longitudinal plane and calculated as the distance from the leading edge interface between lumen and intima to the leading edge interface between media and adventitia in the far wall of the artery. Five IMT measurements at 3-mm intervals were obtained starting 1 cm proximal to the bulb and moving proximally.10 The mean IMT was obtained from five IMTs in the final analysis. The internal luminal diameter during end-diastole (Dd) and end-systole (Ds) 1 cm proximal to the bulb were measured using M-mode ultrasound over five cardiac cycles and averaged. The inner lumen diameter was assessed as the distance between the intima-lumen interface at the near wall and the lumen-intima interface at the far wall. In addition, three brachial artery blood pressure measurements were obtained in the right arm with an automated digital oscillometric sphygmomanometer (Omron Healthcare, Kyoto, Japan) and averaged to determine the resting blood pressure. The stiffness index β (β) was estimated according to the following equation: β=ln(Ps/Pd) × Dd/(Ds−Dd), where Ps and Pd are the systolic and diastolic blood pressure in mm Hg, respectively.
In addition, several cardiac function parameters were also measured.11 Left ventricular (LV) end-diastolic and end-systolic volumes and ejection fraction were estimated by a modified Simpson’s rule from apical imaging planes and normalized to body surface area. The E/A ratio and early diastolic mitral annular velocity on the septal side (e′) were obtained using pulse Doppler imaging and tissue Doppler imaging.
The measurement of CS
The short axial B-mode image at the same level of the right common carotid artery used for measuring β was acquired during three cardiac cycles with novel software developed for the ‘rodent’ heart.12, 13 This application was capable of obtaining high-frame rate two-dimensional images. All images were recorded with a high frame rate (>100 frames s−1; mean frame rate: 143±45 frames s−1). Offline speckle-tracking analysis was performed on digitally stored gray scale images using custom software (EchoPAC PC BT08: GE Healthcare, Milwaukee, WI, USA). First, the endovascular border was manually traced at end-systole. The width of the region of interest (ROI) was reduced to a minimum by the software to avoid the mis-tracking of extravascular tissue, because it depends on the depth resolution (no fixed value). The software then automatically detected frame-to-frame movement of the natural ultrasound reflections (speckles) on standard ultrasonic images in two dimensions based on the block-matching and autocorrelation search algorithms.3 The carotid arterial wall was equally divided into six segments, and each segment was analyzed individually. CS, which is expressed as the circumferential stretch during systole, was automatically determined from each time-strain curve for all six segments. In the present study, CS only in the posterior region of carotid artery was analyzed because the measurement of IMT in the far wall has less discrepancy with histological findings.14Figure 1 shows an example of CS measurement using 2DST. In addition, we corrected CS because of the nonlinear stress–strain relationship using the following equation: ɛcirc(%−1)=[ln(Ps/Pd)/CS] × 100.15
Pulse wave analysis
The measurement of brachial-ankle pulse wave velocity (baPWV) was performed at the same position immediately after the ultrasound examination using the volume-plethysmographic method with previously validated equipment (from PWV/ABI; Colin Medical Technology, Komaki, Japan). A detailed description of this device has been reported previously.16, 17 Cuffs were connected to both the plethysmographic and oscillometric sensors and wrapped around both arms and ankles while the patient was supine. Transit time (δTba) between the brachial and ankle pulse waves was automatically measured based on the time delay between the foot of the pressure increase (sharp initial systolic upstroke of the wave) in the arm and ankle. The distance between the two recording sites was calculated automatically based on the height of the subject (H) and anthropomorphic data for the Japanese population. The path length from the suprasternal notch to the brachium (Lb) and ankle (La) was calculated using the following equation: Lb=0.2195 × H (cm)−2.0734, La=0.8129 × H (cm)+12.328. The baPWV was then calculated using the following equation: baPWV=(La−Lb)/δTba. The average of right and left baPWV was used in the final analysis. All measurements were carried out by the same trained investigator.
Statistical analysis
All values are expressed as the mean±s.d. The clinical and ultrasound parameters and baPWV were compared with an unpaired t-test between healthy subjects and patients with hypertension. Linear regression analysis was performed to evaluate the relationship of age or baPWV with the two stiffness parameters (β and ɛcirc). The correlations between age and baPWV and the carotid stiffness parameters were compared using analysis of covariance. Multivariate logistic regression analysis that included all subjects was performed to determine the independent predictors of ɛcirc. Age, gender, body mass index, the presence of hypertension, LV ejection fraction, metabolic variables, the use of each class of antihypertensive medications, Dd and IMT were used as dependent variables in the regression model. The inter-observer and intra-observer variability were assessed for measuring β and ɛcirc in 60 randomly selected healthy subjects and compared with a paired t-test. The inter-observer variability was calculated as the s.d. of the differences between the measurements of two independent observers who were unaware of the other data and expressed as a percentage of the average value. The intra-observer variability was calculated as the s.d. of the differences between the first and second determination (2-week interval) for a single observer and expressed as a percentage of the average value. All statistical analyses except for the Bland–Altman plot were performed using SPSS 15.0 J software for Windows (SPSS, Chicago, IL, USA). The analysis for Bland–Altman plot was performed using Medcalc Version 12.1.3 for windows (Mariakerke, Belgium).
Results
The overall baseline characteristics of healthy subjects and patients with hypertension are shown in Table 1. The patients with hypertension had significantly higher body weight, body mass index, blood pressure, pulse pressure, diabetic parameters, carotid diameter, IMT and lower LV diastolic parameters than those in healthy subjects.
The correlation between age and baPWV and carotid stiffness parameters in healthy subjects
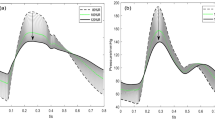
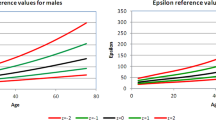
In the healthy subjects, ɛcirc was significantly correlated with β (r=0.363, P<0.001). ɛcirc was positively correlated with age and baPWV, and these correlations were better than the corresponding correlations of β with age and baPWV, but the differences were not statistically significant (Figure 2).
Comparison of stiffness parameters between healthy subjects and patients with hypertension
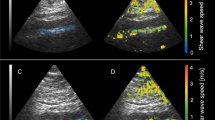
The stiffness parameters in both groups are displayed in Figure 3. The patients with hypertension had significantly higher baPWV, β and ɛcirc than those in healthy subjects. Representative examples are shown in Figure 4.
Examples of circumferential strain curves of the right carotid artery by speckle-tracking imaging (left) and carotid echocardiographic data from B-mode and M-mode recordings (right) in a 44-year-old healthy subject (a) and a 48-year-old patient with hypertension (b). The red arrowheads indicate the posterior region of carotid artery. The white arrow indicates peak circumferential strain.
The determinants of ɛcirc in all subjects
Multivariate logistic regression analysis showed that age, heart rate and the presence of hypertension were significant independent predictors of ɛcirc among the study parameters in all subjects (Table 2).
Observer variability
The inter-observer and intra-observer variability for the measurement of ɛcirc were significantly better than those for the measurement of β (Table 3, Figure 5).
Bland–Altman plot of inter- and intra-observer variability for the analysis of β (a) and ɛcirc (b). The horizontal solid line indicates the mean difference between the two measures, and the dashed lines indicate the 95% limits of agreement (mean difference±1.96 times the s.d. of the difference). A full color version of this figure is available at the Hypertension Research journal online.
Discussion
To our knowledge, this is the first report of the measurement of a new stiffness parameter, ɛcirc, using high-frame 2DST in healthy subjects and patients with hypertension. The major findings of this study are the following: (1) there were significant correlations between ɛcirc and age and between ɛcirc and baPWV, and those correlations were slightly better than those between β and age, and between β and baPWV; (2) patients with hypertension had a significantly higher ɛcirc than healthy subjects; (3) age, heart rate and the presence of hypertension were associated with ɛcirc, even after adjustment for clinical data, metabolic variables, ultrasound parameters and antihypertensive medications; and (4) the reproducibility of ɛcirc was significantly better than that of β.
Significance of ɛcirc compared with the conventional parameter β
Increased arterial stiffness leads to worsening of myocardial ischemia as a result of increased after load and oxygen demand (elevated systolic blood pressure) or impaired coronary blood supply (decreased diastolic blood pressure).18 Furthermore, increased arterial stiffness is an independent prognostic predictor of cardiovascular events in several populations.1 Thus, a non-invasive assessment of arterial stiffness is important in terms of an early stratification for future cardiovascular events. To date, several ultrasound parameters of arterial elasticity have been reported.2 Among them, carotid stiffness β is used to easily evaluate arterial stiffness in the clinical setting, because it was found to be independent of blood pressure within the normal physiological range and was associated with the severity of hypertension and coronary atherosclerosis.19, 20 However, this parameter is based on the cyclic changes of the internal luminal diameter of the artery and does not take into account the expansion of the intima-media wall itself. Currently, 2DST is available to detect regional myocardial deformation in various cardiac diseases.3, 4, 5, 6, 7, 8, 9 Furthermore, the sensitivity of high-frame 2DST in the circumferential direction was recently assessed in rat and mouse models with very thin myocardial thickness,12, 13 and this technique can be used in the clinical setting. Therefore, we applied it to the carotid arterial wall, because this technique enables the measurement of strain in very thin tissue segments with high reproducibility. Several studies have reported that aging is the most important determinant of arterial stiffness.1 Actually, aging was one of the significant independent predictors of ɛcirc in the present study. Thus, our results suggest that ɛcirc reflects similar or slightly better associations between age and systemic stiffness compared with the conventional parameter β. We think that two main mechanisms may be responsible for this result. First, in general, reproducibility is correlated with the accuracy of the study parameter. In the present study, we manually measured the internal luminal diameter using M-mode rather than two-dimensional ultrasound. However, CS was semi-automatically measured using 2DST software with high reproducibility.3, 4, 5, 6, 7, 8, 9, 12, 13 The difference in measurement methods may account for the significantly better reproducibility of ɛcirc compared with β. Second, ɛcirc is a parameter that directly measures the elasticity of the carotid arterial wall in the circumferential direction, whereas β is an indirect parameter that measures the change of the internal luminal diameter of the artery in the radial direction.
The comparison of stiffness parameters between healthy subjects and patients with hypertension
Patients with hypertension have been reported to have higher arterial stiffness than healthy subjects, and this association is independent of age.20, 21 Although the severity of hypertension was relatively mild in the present study and these patients did not have any other atherosclerotic risk factors, the patients with hypertension had significantly higher ɛcirc as well as conventional stiffness parameters compared with healthy subjects. In addition, the presence of hypertension was one of the independent predictors of ɛcirc. These results support the concept that ɛcirc could serve as an early marker of increased arterial stiffness.
Clinical implications
The present study showed that ɛcirc was more reproducible and had a similar or slightly better correlation with age and systemic stiffness compared with β. This raises the possibility that ɛcirc could be used as a simple and more accurate index of arterial stiffness in clinical practice.
Study limitations
The present study has several limitations. First, the number of patients in this study was small and the variation of ɛcirc was relatively large. Therefore, more clinical studies in larger patient populations must be performed to confirm the accuracy of ɛcirc as an index of arterial stiffness. Second, the stiffness parameters β and ɛcirc were calculated at only a single site without plaque in the right common carotid artery, and this might have increased the variation of those parameters among subjects. In addition, it is unknown whether carotid stiffness parameters measured at a single site reflect arterial stiffness in patients with heterogeneous regional arterial stiffness due to diffuse plaques. Multiple site measurements in the entire carotid artery and the development of new software might reduce the variation in stiffness among subjects and improve the precision of the measurement. Third, this study was an observational study. The clinical significance of ɛcirc as a predictor of future events is still lacking. Thus, prospective studies in larger patient populations are definitely necessary to establish the validity of ɛcirc as a predictor of future events. Fourth, the precise blood pressure in the common carotid artery could not be measured, and we used brachial artery pressure to calculate stiffness β, as was done in previous studies. Finally, in this speckle-tracking software, manual adjustment of the ROI width is not allowed. Thus, it might be difficult to completely adjust the ROI width to the IMT. Future development of speckle-tracking software would be useful to improve the tracking of carotid artery deformation and to provide a better instrument for the study of arterial stiffness.
Conclusions
This study showed that the measurement of carotid ɛcirc using 2DST was feasible and that ɛcirc was more reproducible and had a similar or slightly better correlation with age and systemic stiffness than the conventional carotid arterial stiffness parameter β. Moreover, patients with hypertension had a significantly higher ɛcirc than healthy subjects. This clinically promising parameter might be used as a novel surrogate marker for early arteriosclerosis.
References
Vlachopoulos C, Aznaouridis K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010; 55: 1318–1327.
Cavalcante JL, Lima JA, Redheuil A, Al-Mallah MH . Aortic stiffness: current understanding and future directions. J Am Coll Cardiol 2011; 57: 1511–1522.
Leitman M, Lysyansky P, Sidenko S, Shir V, Peleg E, Binenbaum M, Kaluski E, Krakover R, Vered Z . Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 2004; 17: 1021–1029.
Inoue K, Okayama H, Nishimura K, Saito M, Yoshii T, Hiasa G, Sumimoto T, Inaba S, Suzuki J, Ogimoto A, Funada J, Higaki J . Right ventricular septal pacing preserves global left ventricular longitudinal function in comparison with apical pacing. Circ J 2011; 75: 1609–1615.
Saito M, Okayama H, Nishimura K, Ogimoto A, Ohtsuka T, Inoue K, Hiasa G, Sumimoto T, Funada J, Shigematsu Y, Higaki J . Determinants of left ventricular untwisting behaviour in patients with dilated cardiomyopathy: analysis by two-dimensional speckle tracking. Heart 2009; 95: 290–296.
Saito M, Okayama H, Yoshii T, Hiasa G, Sumimoto T, Inaba S, Nishimura K, Inoue K, Ogimoto A, Ohtsuka T, Funada J, Shigematsu Y, Higaki J . The differences in left ventricular torsional behavior between patients with hypertrophic cardiomyopathy and hypertensive heart disease. Int J Cardiol 2011; 150: 301–306.
Inoue K, Okayama H, Nishimura K, Ogimoto A, Ohtsuka T, Saito M, Hiasa G, Yoshii T, Sumimoto T, Funada J, Higaki J . Right ventricular pacing from the septum avoids the acute exacerbation in left ventricular dyssynchrony and torsional behavior seen with pacing from the apex. J Am Soc Echocardiogr 2010; 23: 195–200.
Amundsen BH, Helle-Valle T, Edvardsen T, Torp H, Crosby J, Lyseggen E, Støylen A, Ihlen H, Lima JA, Smiseth OA, Slørdahl SA . Noninvasive myocardial strain measurement by speckle trackingechocardiography validation against sonomicrometry and taggedmagnetic resonance imaging. J Am Coll Cardiol 2006; 47: 789–793.
Cho GY, Chan J, Leano R, Strudwick M, Marwick TH . Comparison of twodimensional speckle and tissue velocity based strain and validation with harmonic phase magnetic resonance imaging. Am J Cardiol 2006; 97: 1661–1666.
Celermajer DS, Sorensen KE, Bull C, Robinson J, Deanfield JE . Endothelium-dependent dilation of the systemic arteries of asymptomatic subjects relates to coronary risk factors and their interaction. J Am Coll Cardiol 1994; 24: 1468–1474.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ ; Chamber Quantification Writing Group American Society of Echocardiography's Guidelines and Standards Committee European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Peng Y, Popovic ZB, Sopko N, Drinko J, Zhang Z, Thomas JD, Penn MS . Speckle tracking echocardiography in the assessment of mouse models of cardiac dysfunction. Am J Physiol Heart Circ Physiol 2009; 297: H811–H820.
Popović ZB, Benejam C, Bian J, Mal N, Drinko J, Lee K, Forudi F, Reeg R, Greenberg NL, Thomas JD, Penn MS . Speckle-tracking echocardiography correctly identifies segmental left ventricular dysfunction induced by scarring in a rat model of myocardial infarction. Am J Physiol Heart Circ Physiol 2007; 292: H2809–H2816.
Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R . Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 1986; 74: 1399–1406.
VanBavel E, Siersma P, Spaan JA . Elasticity of passive blood vessels: a new concept. Am J Physiol Heart Circ Physiol 2003; 285: H1986–H2000.
Yamashina A, Tomiyama H, Takeda K . Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002; 25: 359–364.
Munakata M, Ito N, Nunokawa T, Yoshinaga K . Utility of automated brachial ankle pulsewave velocity measurements in hypertensive patients. Am J Hypertens 2003; 16: 653–657.
Saito M, Okayama H, Nishimura K, Ogimoto A, Ohtsuka T, Inoue K, Hiasa G, Sumimoto T, Higaki J . Possible link between large artery stiffness and coronary flow velocity reserve. Heart 2008; 94: e20.
Hirai T, Sasayama S, Kawasaki T, Yagi S . Stiffness of systemic arteries in patients with myocardial infarction. A noninvasive method to predict severity of coronary atherosclerosis. Circulation 1989; 80: 78–86.
Liao D, Arnett DK, Tyroler HA, Riley WA, Chambless LE, Szklo M, Heiss G . Arterial stiffness and the development of hypertension. The ARIC study.Hypertension 1999; 34: 201–206.
Tomiyama H, Arai T, Koji Y, Yambe M, Motobe K, Zaydun G, Yamamoto Y, Hori S, Yamashina A . The age-related increase in arterial stiffness is augmented in phases according to the severity of hypertension. Hypertens Res 2004; 27: 465–470.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saito, M., Okayama, H., Inoue, K. et al. Carotid arterial circumferential strain by two-dimensional speckle tracking: a novel parameter of arterial elasticity. Hypertens Res 35, 897–902 (2012). https://doi.org/10.1038/hr.2012.39
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.39
Keywords
This article is cited by
-
Effects of Different Long-Term Exercise Modalities on Tissue Stiffness
Sports Medicine - Open (2022)
-
Healthy aging and carotid performance: strain measures and β-stiffness index
Hypertension Research (2018)
-
Does the internal jugular vein affect the elasticity of the common carotid artery?
Cardiovascular Ultrasound (2015)