Abstract
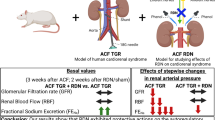
Although Ren-2 transgenic rat (TGR) is defined as a model of angiotensin II-dependent hypertension, we studied whether the renin–angiotensin system (RAS) is really the main contributor to blood pressure (BP) elevation in hetero- and homozygous TGRs. Moreover, we examined whether repeated antisense (AS) therapy against AT1 receptors would have a similar effect on the BP and the contribution of the principle vasoconstrictor/vasodilator systems to BP regulation in young and adult TGRs. From the age of 30 (young) and 100 (adult) days, rats were injected with AS for 40 days in 10-day intervals. After 10 and 40 days of AS therapy, the basal BP and acute BP responses to the sequential blockade of the RAS, sympathetic nervous (SNS) and nitric oxide systems were determined in conscious rats. The RAS system was the major system maintaining elevated BP in young homozygous animals, whereas there was an increasing contribution of the SNS in heterozygous TGR with age. The AS therapy in the young TGR had a transient BP-lowering effect that was associated with reduced cardiac hypertrophy; the AS therapy was most effective in young homozygous TGR, causing a substantial reduction of angiotensin-dependent vasoconstriction. In heterozygous rats, AS therapy at earlier stages was related to an inhibition of sympathetic vasoconstriction, whereas to RAS inhibition in established hypertension. In conclusion, repeated AS therapy had transient antihypertensive effects exclusively in young TGR. The contribution of the RAS to BP maintenance is highly important only in homozygous TGRs, whereas it is surpassed by SNS in heterozygous TGR.
Similar content being viewed by others
Introduction
Ren-2 transgenic rat (TGR) is a typical monogenic form of hypertension and represent a well-established model of angiotensin II (ANG II)-dependent hypertension, with a sustained local activation of the renin–angiotensin system (RAS).1 However, the exact pathophysiological mechanisms responsible for the development and maintenance of hypertension in this model remain unclear. The homozygous line develops severe hypertension and typical signs, that is, impaired kidney and cardiac functions, lead to a high mortality at a young age. Therefore, experiments in homozygous animals can be performed only until 2–3 months of age. In contrast, heterozygous animals become hypertensive at the age of 7–8 weeks, and they survive normally. Originally, TGRs were characterized as a low-renin form of hypertension,1, 2, 3 with similar levels of ANG II in the TGRs and their normotensive Hannover Sprague-Dawley (HanSD) controls. However, controversial findings of either increased or decreased ANG II levels were reported in the plasma and kidneys of anesthetized animals. Recently, Huskova et al.4 have found that the ANG II levels were increased in conscious TGR, as compared with age-matched HanSD, showing that the increased activity of the RAS might contribute to the hypertension in this experimental model. On the basis of the studies performed using tail arteries, Arribas et al.5 suggested that higher norepinephrine release and alpha2-adrenoreceptor-mediated contractions could contribute to the elevated blood pressure (BP) in TGR. However, oxidative stress, which is thought to be an important factor in hypertension, has been shown to have a negligible role in this particular model.6 Finally, the chronic blockade of cyclooxygenase 2 did not affect the development of hypertension in TGRs,7 whereas the acute blockade of nitric oxide (NO) synthesis induced greater BP elevation in young (prehypertensive) TGR than in HanSD.8 Although many data are available on heterozygous TGR, only scarce information dealing with BP regulation and the activity of the RAS system in homozygous TGR can be found.
The regulation of BP is based on the balance between vasoconstrictor and vasodilator systems. Most of the models of experimental hypertension studied so far in our laboratory [genetic (SHR), hereditary hypertriglyceridemic (HTG),9 NO-deficient (L-NAME-treated)10 and salt-dependent (Dahl)11] were characterized by augmented sympathetic vasoconstriction. Thus, we were interested, whether the same is true for a model with an activated RAS (due to the insertion of the murine Ren-2 renin gene into the rat genome). Moreover, we investigated the effect of RAS inhibition using gene therapy based on the binding of antisense (AS) oligodeoxynucleotides to the mRNA for AT1 receptors.
Although gene therapy has been suggested to be a promising therapy for treating various cardiovascular diseases,12, 13, 14 the original potential has not been fully realized. Nevertheless, the AS therapy based on phosphorothioated oligonucleotides still has its supporters. Our previous study revealed that single dose of AS against ANG II receptor type 1 (AT1R) applied intravenously to young heterozygous TGR had transient antihypertensive effects.15 Other studies have also shown that the long-term effect of AS therapy against angiotensinogen or AT1R persisted for 3 months in young spontaneously hypertensive rats (SHRs),16, 17 whereas the effect lasted only 1 month in adult SHRs.18 Interestingly, AS therapy had an antihypertensive effect (∼20 mm Hg) in young TGRs, which was associated with attenuated cardiac hypertrophy.19 We were, therefore, interested whether the repeated application of AS therapy against AT1R could prevent hypertension development in young animals or abolish the already-established hypertension in adult rats.
Therefore, the aim of this study was to investigate (1) the contribution of the principal vasoconstrictor and vasodilator systems to BP regulation in homo- and heterozygous TGRs in comparison with their transgene-negative HanSD controls, evaluated at different stages of hypertension development, that is, during the developmental and established phases of hypertension, and (2) the effect of AS therapy against AT1R on the balance between the main vasoconstrictor and vasodilator systems in young and adult homo- and heterozygous TGRs.
Methods
Animals
Male heterozygous and homozygous TGRs (strain name TGR[mRen2]27) and their normotensive HanSD controls were housed at 23 °C under a 12 h light/dark cycle and had free access to a standard ST1 chow (containing 1% NaCl) and tap water ad libitum. All of the animals used in this study were bred at the Institute of Physiology from stock animals supplied from Max Delbrück Center for Molecular Medicine in Berlin, Germany. From the age of 30 (young) or 100 (adult) days, the rats were injected with AS (250 μg kg−1 body weight of phosphorothioated AS oligonucleotides against the AT1R of ANG II; dissolved in saline) into the jugular vein for 40 days at 10-day intervals. This interval was adopted based on our previous study,15 in which we applied a single dose of AS to young animals at the age of 30 days. In these animals, the BP-lowering effect persisted for almost 3 weeks. The systolic blood pressure was measured in 3 to 5-day intervals in a subgroup of the young heterozygous TGR using the tail plethysmography method. The measurements of vasoactive balances (showing the contribution of the vasoconstrictor/vasodilator systems—RAS, sympathetic nervous system (SNS) and NO synthase systems) were performed at 10 and 40 days after the start of the AS application. All of the procedures and experimental protocols were approved by the Ethical Committee of the Institute of Physiology Academy of Sciences of the Czech Republic and conform to the European Convention on Animal Protection and Guidelines on Research Animal Use.
Oligonucleotides
Antisense oligodeoxynucleotides (Generi Biotech, Hradec Králové, Czech Republic) were synthesized as 15-mer phosphorothioated oligodeoxynucleotides complementary to bases +63 to +77 of the AT1R mRNA, as described previously.20
Experimental procedure
One day before the measurement of the vasoactive balance, polyethylene catheters were inserted into left carotid artery and jugular vein and were exteriorized in the interscapular region under light isoflurane anesthesia. The BP and its changes after the acute blockade of particular vasoactive systems were assessed simultaneously in four conscious animals 24 h later using a pressure transducer and a multichannel recorder (ADInstruments, Bella Vista, Australia).
The scheme of the measurement of the vasoactive balance is based on the modified protocol of Minami et al.,21 which is used regularly in our laboratory.9 The successive steps of the blockade of the distinct vasoactive systems in the homo- and heterozygous TGR and their age-matched HanSD controls are depicted in Figure 1. Briefly, the baseline levels of the systolic, diastolic and mean arterial pressures (MAPs) were recorded for 30 min, followed by a sequential blockade of the RAS (10 mg kg−1 body weight captopril), to estimate the existing pressor action of endogenous ANG II, the SNS (5 mg kg−1 body weight pentolinium), to evaluate the actual vasopressor SNS activity and the nitric oxide synthase (30 mg kg−1 body weight L-NAME), to determine the vasodilator effects of the available endogenous NO. Following the blockade of NO synthesis with L-NAME, the maximal vasodilation was induced with nitroprusside, a direct donor of NO (20 μg kg−1 body weight), to obtain the lowest level of BP, marked as the residual pressure. All of the drugs were purchased from Sigma (St Louis, Missouri, USA) and injected as intravenous bolus injection in a volume of 1 ml kg−1 body weight.
The time course of the MAP changes achieved after the sequential blockade of the renin–angiotensin (RAS), sympathetic nervous (SNS) and nitric oxide (NO) systems in young 6-week-old homozygous and heterozygous TGRs and their age-matched controls (HanSD rats). The arrows indicate the time points at which captopril (RAS inhibitor; 10 mg kg−1 body weight (BW)), pentolinium (SNS blocker; 5 mg kg−1 BW) and L-NAME (NO synthesis inhibitor; 30 mg kg−1 BW) were administered (n=8–10 animals per group). HanSD, Hannover Sprague-Dawley rat; MAP, mean arterial pressure; TGR, transgenic rat.
Statistical analysis
The results are expressed as the mean±standard error of the mean. The statistical differences were evaluated by a one-way analysis of variance followed by the appropriate post hoc test. Values of P<0.05 were considered statistically significant.
Results
The effect of genotype and age
The basal MAP of young TGR (129±4 mm Hg in heterozygous and 151±2 mm Hg in homozygous) significantly exceeded that of the control HanSD (102±4 mm Hg; Figure 1). In contrast, the final BP (that is, the BP after the sequential blockade of the three major vasoactive systems) was the highest in HanSD (144±2 mm Hg) and almost identical in both of the TGR groups (120±4 mm Hg in the heterozygous and 119±3 mm Hg in the homozygous). Owing to the high mortality of the homozygous TGR, reaching 70% at the age of 100 days, no evaluation of adult rats of this strain was performed.
The MAP of the control HanSD rats was in the normotensive range throughout the entire study. The BP of the young TGR was significantly elevated, as compared with the HanSD controls, and the BP increased earlier in the homozygous vs. the heterozygous TGR (Figure 2a). The BP of both of the TGR strains reached similarly elevated levels at the age of 70 days and was always substantially higher in the adult heterozygous TGR when compared with the normotensive controls (Figure 2b).
The effect of the genotype on the basal MAP (a, b) and residual pressure (c, d) in young rats at the age of 40 and 70 days and in adult rats (110 and 140 days old). *P<0.05 vs. control HanSD animals, @P<0.05 vs. heterozygous TGR, #P<0.05 vs. the corresponding group of younger animals. BP, blood pressure; HanSD, Hannover Sprague-Dawley rat; MAP, mean arterial pressure; TGR, transgenic rat.
Figure 2c shows a significant increase in the residual BP (that is, the BP measured after the maximal vasodilation evoked by the nitroprusside injection) during the development of hypertension in young homo- and heterozygous TGRs. Moreover, there was a clearly different correlation between the residual pressure and age in the control HanSD (r=−0.4989, n=26, P<0.01) and in the heterozygous TGRs (r=0.4076, n=32, P<0.02). At the age of 150 days, the adult heterozygous TGRs exhibited significantly higher residual pressure in comparison with the control HanSD (Figure 2d).
In the young rats (aged 40 and 70 days), the contribution of the RAS to BP maintenance was proportional to the number of Ren-2 alleles because the captopril-induced BP reduction was smallest in the control HanSD rats and greatest in the homozygous TGR (Figure 3a). These data confirm the ANG II-dependent BP control in this form of hypertension. However, this ANG II dependency was lost with the further development of hypertension because there was no difference in the BP reduction after the RAS blockade between the adult heterozygous TGR and control HanSD rats (Figure 3b). This surprising finding can be explained by the progressive replacement of the enhanced ANG II-dependent vasoconstriction by augmented sympathetic vasoconstriction. Indeed, increased pentolinium-induced BP decreases appeared in the 70-day-old heterozygous TGRs (Figure 3c), and the same was true for the adult heterozygous animals aged between 110 and 150 days (Figure 3d), indicating that sympathetic vasoconstriction became the major contributor to the increased BP. In contrast, the BP decrease after sympathetic blockade was attenuated with age in the homozygous TGRs.
The effect of genotype on the MAP changes elicited by RAS (a, b), SNS (c, d) and NOS (e, f) blockades in young rats (left panels) and adult rats (right panels). *P<0.05 vs. control HanSD animals, @P<0.05 vs. heterozygous TGR. HanSD, Hannover Sprague-Dawley rat; MAP, mean arterial pressure; NOS, nitric oxide synthase; RAS, renin–angiotensin system; SNS, sympathetic nervous system; TGR, transgenic rat.
The endogenous NO-dependent vasodilation was attenuated in the early phases of hypertension development, as evidenced by the reduction of the L-NAME-induced BP rise in both the heterozygous and homozygous 40-day-old TGRs. Thereafter, the NO-dependent vasodilation became enhanced in the heterozygous TGR aged between 70 and 150 days (Figures 3e and f); however, this was not the case for the homozygous TGR in which the L-NAME-induced BP elevation did not surpass that observed in the HanSD controls (Figure 3e).
The comparison of the vasoconstrictor and vasodilator mechanisms shows a remarkable difference between the control HanSD and heterozygous and homozygous TGRs (Figures 4a–c). In the normotensive HanSD controls, the vasodilator mechanisms always surpassed the vasoconstrictor mechanisms (Figure 4a), whereas the BP change elicited by the acute NO synthesis inhibition (L-NAME) was practically equal to the sum of the BP changes evoked by the blockade of the RAS and SNS (captopril and pentolinium, respectively) in the heterozygous rats. However, the NO-dependent vasodilation did not match the sum of vasoconstrictor systems in homozygous TGR studied (aged 40 and 70 days).
Comparison of the magnitude of BP changes elicited by the blockade of the vasoconstrictor (SNS+RAS—hatched bars) and vasodilator (NO—black bars) systems in young control HanSD (a) and heterozygous (b) and homozygous (c) TGRs. *P<0.05, NO vs. RAS+SNS. BP, blood pressure; HanSD, Hannover Sprague-Dawley rat; NO, nitric oxide; RAS, renin–angiotensin system; SNS, sympathetic nervous system; TGR, transgenic rat.
The effect of AS application
The chronic systolic blood pressure measurements using tail-cuff plethysmography revealed a significant BP reduction (30–40 mm Hg) induced by the repeated AS application in the young heterozygous TGR compared with the untreated animals that lasted for ∼30 days (Figure 5). A significantly lower BP was observed as early as 5 days after the first injection of AS. However, the BP-lowering effect of the AS application disappeared after the fourth AS injection, that is, at the age of 70 days. The injections of scrambled AS did not cause any significant effect on the BP. The acute experiments in conscious cannulated rats confirmed the results obtained using tail-cuff plethysmography, showing that the AS therapy significantly lowered the systolic blood pressure in the heterozygous and young homozygous TGRs after the first AS injection, that is, in rats aged 40 days (Figures 6a and b). This BP reduction was accompanied by reduced cardiac hypertrophy (Table 1). However, no significant BP-lowering effect was found after the fourth injection of AS at the age of 70 days in either young homo- or heterozygous TGRs; there was no effect of AS therapy on the residual pressure within the groups aged 40 or 70 days (Figure 6f). Thus, it is evident that the AS therapy lowered the ANG II-dependent vasoconstriction, especially in homozygous TGR (Figure 6c). Surprisingly, the BP reduction induced by the first AS injection in the young heterozygous TGR was due to the attenuated sympathetic vasoconstriction and/or enhanced NO-dependent vasodilation (without significant changes in the ANG II-dependent vasoconstriction; Figures 6d and e).
Systolic blood pressure (SBP) (a), MAP (b), and MAP changes due to RAS (c), SNS (d), and NOS (e) blockades and the residual blood pressure (f) in young rats after the first (40 days) and last (70 days) AS applications. *P<0.05 vs. control HanSD animals, #P<0.05 vs. the corresponding group of younger animals. AS, antisense; HanSD, Hannover Sprague-Dawley rat; MAP, mean arterial pressure; NOS, nitric oxide synthesis; RAS, renin–angiotensin system; SNS, sympathetic nervous system; TGR, transgenic rat.
In agreement with a prevalent opinion that pharmacological interventions are more effective when adopted in young animals,22 no significant effect of the AS therapy on BP was found in the heterozygous TGR, in which the AS therapy was started at the age of 3 months. No effect of the AS on the contribution of the vasoconstrictor (RAS and SNS) or vasodilator (NO) systems to BP regulation were found in the adult heterozygous TGR (data not shown).
Discussion
Genotype and age
The enhanced participation of the SNS in BP maintenance has been demonstrated by our group in various models of experimental hypertension, namely, in genetic (SHR),9 salt-sensitive (Dahl S) rats23 and NO-deficient (L-NAME-treated) rats,10 suggesting that the increased sympathetic tone is a common feature in most of the models of experimental hypertension.24 In all of these models, the acute blockade of RAS induced only a mild BP fall of approximately 10 mm Hg. It is well known that TGRs represent an ANG II-dependent form of hypertension. Indeed, the rapid fall of BP after the captopril administration in the young heterozygous (−21 mm Hg) and even more in the homozygous TGR (−44 mm Hg) at the age of 40 days and −34 mm Hg and −58 mm Hg at the age of 70 days, respectively, reflected a strong activation of the RAS given by the increasing Ren-2 allele number. In accordance with these results, there are recent data comparing the ANG II levels of hetero- and homozygous TGRs at the age of 32 and 52 days (Husková Z and Cervenka L, personal communication) showing a renin copy number-dependent increase in renal ANG II concentrations in heterozygous and homozygous TGR vs. control HanSD, which was accompanied by an increase in plasma ANG II levels in both the hetero- and homozygous TGRs. In addition, our present study has shown that there was a tendency for the attenuation of the ANG II-dependent BP component in the heterozygous TGR with aging that was replaced by increased sympathetic vasoconstriction.
Figure 7 shows that the basal MAP of TGR was dependent not only on the RAS but also on the SNS and that the degree of BP dependence was similar for both vasoconstrictor systems. Importantly, these vasoconstrictor effects were additive, yielding a very strong correlation between the basal MAP and BP response to combined RAS and SNS blockade (Figure 7c).
The relationship of the basal mean arterial pressure (MAP) to the RAS-dependent (captopril-induced BP decrease; a), sympathetic (pentolinium-induced BP decrease; b), combined RAS+SNS-dependent (c) and NO-dependent (L-NAME-induced BP increase; d) components of the MAP in TGR. For the analysis, the values from 164 rats were used; r-values (correlation coefficients) were highly significant for all of the regression lines (P<0.001). BP, blood pressure; NO, nitric oxide; RAS, renin–angiotensin system; SNS, sympathetic nervous system; TGR, transgenic rat. A full color version of this figure is available at the Hypertension Research journal online.
Interestingly, there was an age-dependent rise in the residual BP (that is, the BP after the maximal vasodilation induced by sodium nitroprusside that cannot be further reduced by such pharmacological intervention as nifedipine administration) in the heterozygous and homozygous TGRs that could be ascribed to a substantial structural remodeling of the vessels in young TGR during the developmental phase of hypertension. This result agrees with the results of Rossi et al.,25 who found a substantial increase in collagen deposition in TGR between the 4th and 8th weeks of life.
Figure 4 shows that the major vasoconstrictor systems (SNS and RAS) are in a good balance with the major vasodilator system (NO) in the heterozygous TGR (middle panel), whereas the inability of the NO system to counterbalance the vasoconstrictor systems, together with the activation of the RAS, have major roles in the maintenance of elevated BP in the homozygous TGR (lower panel). In contrast, the control HanSD rats exhibit a substantial excess of the vasodilator systems, especially at younger ages (upper panel).
Antisense
Our data are compatible with the generally accepted idea that therapeutic interventions are more efficient when applied in young vs. adult animals.22 This is also true for AS therapy because early AS administration had more prolonged effects in young animals compared with adult animals. Thus, the maximal BP-lowering effect (−35 mm Hg) was observed in young 5-day-old SHRs, in which the BP effect persisted for 3–4 months,17, 26 whereas the same procedure applied to adult rats decreased the BP for only 1 month.18 Similar results were obtained for other experimental model, namely, 2-kidney-1-clip.27 Our findings agree with those of Pachori et al.,19 who found moderate antihypertensive effects of AS therapy in young TGR that were accompanied by attenuated cardiac hypertrophy. Our data also demonstrated positive effects of AS therapy on cardiac hypertrophy, as indicated by the decrease in the relative heart weight. However, this effect was significant only in young rats during the developmental phase of hypertension, whereas it was absent if the AS therapy was repeatedly applied in animals with established hypertension. Thus, AS therapy had significant antihypertensive effects in young rats during the developmental phase of hypertension (accompanied by reduced cardiac hypertrophy), whereas its effect continuously vanished with time.
The relative inefficiency of this type of therapy is probably connected with the fact that AS blocks only the expression of mRNA and protein, whereas classical approaches, such as angiotensin receptor blockers, angiotensin-converting enzyme inhibitors or direct renin inhibitors, directly block the action of ANG II at one step of the RAS cascade. Our previous studies have repeatedly shown that blocking either ANG II binding to the AT1R with angiotensin receptor blockers (candesartan28 and losartan29) or the conversion of angiotensinogen to ANG I using the direct renin inhibitor, aliskiren,29 was able to normalize BP to the level of control animals.
Interestingly, in heterozygous TGR, the BP reduction following AS administration at the age of 40 days was caused by the substantial reduction of sympathetic vasoconstriction, which was accompanied by increased endogenous NO-dependent vasodilation. In contrast, BP reduction could be ascribed to the inhibited RAS-dependent vasoconstriction in young homozygous and heterozygous TGRs at the age of 70 days.
It is important to note that there are ‘developmental windows’ for antihypertensive therapy22 because RAS blockade applied early in life (prepuberty and puberty) has greater long-term BP effects than the same intervention applied to adult rats with fully established hypertension. This is also the explanation why AS therapy was not effective in our adult animals with established hypertension.
In conclusion, our present study has demonstrated that, although TGR is a typical model of ANG II-dependent hypertension, the RAS system is the main contributor to the final BP solely in homozygous TGR; in contrast, the SNS is the main system determining BP in heterozygous rats. Consequently, AS therapy directed against the AT1R was most effective in the homozygous TGR. Moreover, there is a strong dependency of the distinct vasoactive systems participating in BP regulation, in addition to the effectiveness of pharmacological interventions, with regard to the age of the animal.
References
Mullins JJ, Peters J, Ganten D . Fulminant hypertension in transgenic rats harbouring the mouse Ren-2 gene. Nature 1990; 344: 541–544.
Langheinrich M, Lee MA, Bohm M, Pinto YM, Ganten D, Paul M . The hypertensive Ren-2 transgenic rat TGR (mREN2)27 in hypertension research. Characteristics and functional aspects. Am J Hypertens 1996; 9: 506–512.
Springate JE, Feld LG, Ganten D . Renal function in hypertensive rats transgenic for mouse renin gene. Am J Physiol 1994; 266: F731–F737.
Huskova Z, Kramer HJ, Thumova M, Vanourkova Z, Burgelova M, Teplan V, Maly J, Cervenka L . Effects of anesthesia on plasma and kidney II ANG levels in normotensive and ANG II-dependent hypertensive rats. Kidney Blood Press Res 2006; 29: 74–83.
Arribas SM, Alonso MJ, Marin J, Fernandes F, Llergo JL, Sanchez-Ferrer CF, Salaices M . Noradrenergic transmission in the tail artery of hypertensive rats transgenic for the mouse renin gene Ren-2. J Auton Pharmacol 1996; 16: 69–77.
Kopkan L, Huskova Z, Vanourkova Z, Thumova M, Skaroupkova P, Maly J, Kramer HJ, Dvorak P, Cervenka L . Reduction of oxidative stress does not attenuate the development of angiotensin II-dependent hypertension in Ren-2 transgenic rats. Vascul Pharmacol 2009; 51: 175–181.
Vaneckova I, Skaroupkova P, Dvorak P, Certikova CV, Tesar V, Bader M, Ganten D, Kramer HJ . Effects of sodium restriction and cyclooxygenase-2 inhibition on the course of hypertension, proteinuria and cardiac hypertrophy in Ren-2 transgenic rats. Physiol Res 2005; 54: 17–24.
Vaneckova I, Kramer HJ, Novotna J, Kazdova L, Opocensky M, Bader M, Ganten D, Cervenka L . Roles of nitric oxide and oxidative stress in the regulation of blood pressure and renal function in prehypertensive Ren-2 transgenic rats. Kidney Blood Press Res 2005; 28: 117–126.
Kunes J, Dobesova Z, Zicha J . Altered balance of main vasopressor and vasodepressor systems in rats with genetic hypertension and hypertriglyceridaemia. Clin Sci (Lond) 2002; 102: 269–277.
Pechanova O, Dobesova Z, Cejka J, Kunes J, Zicha J . Vasoactive systems in L-NAME hypertension: the role of inducible nitric oxide synthase. J Hypertens 2004; 22: 167–173.
Zicha J, Dobesova Z, Kunes J . Relative deficiency of nitric oxide-dependent vasodilation in salt-hypertensive Dahl rats: the possible role of superoxide anions. J Hypertens 2001; 19: 247–254.
Melo LG, Pachori AS, Gnecchi M, Dzau VJ . Genetic therapies for cardiovascular diseases. Trends Mol Med 2005; 11: 240–250.
Krum H, Gilbert RE . Novel therapies blocking the renin-angiotensin-aldosterone system in the management of hypertension and related disorders. J Hypertens 2007; 25: 25–35.
Li SD, Huang L . Gene therapy progress and prospects: non-viral gene therapy by systemic delivery. Gene Therapy 2006; 13: 1313–1319.
Vaneckova I, Kopkan L, Huskova Z, Vanourkova Z, Schejbalova S, Cervenka L, Kramer HJ . AT1 receptor antisense therapy transiently lowers blood pressure in Ren-2 transgenic rats. Vasc Pharmacol 2007; 47: 63–67.
Kimura B, Mohuczy D, Tang X, Phillips MI . Attenuation of hypertension and heart hypertrophy by adeno-associated virus delivering angiotensinogen antisense. Hypertension 2001; 37: 376–380.
Iyer SN, Lu D, Katovich MJ, Raizada MK . Chronic control of high blood pressure in the spontaneously hypertensive rat by delivery of angiotensin type 1 receptor antisense. Proc Natl Acad Sci USA 1996; 93: 9960–9965.
Katovich MJ, Gelband CH, Reaves P, Wang HW, Raizada MK . Reversal of hypertension by angiotensin II type 1 receptor antisense gene therapy in the adult SHR. Am J Physiol 1999; 277: H1260–H1264.
Pachori AS, Numan MT, Ferrario CM, Diz DM, Raizada MK, Katovich MJ . Blood pressure-independent attenuation of cardiac hypertrophy by AT(1)R-AS gene therapy. Hypertension 2002; 39: 969–975.
Peng JF, Kimura B, Fregly MJ, Phillips MI . Reduction of cold-induced hypertension by antisense oligodeoxynucleotides to angiotensinogen mRNA and AT1-receptor mRNA in brain and blood. Hypertension 1998; 31: 1317–1323.
Minami N, Imai Y, Hashimoto J, Abe K . Contribution of vascular nitric oxide to basal blood pressure in conscious spontaneously hypertensive rats and normotensive wistar kyoto rats. Clin Sci (Lond) 1995; 89: 177–182.
Zicha J, Kunes J . Ontogenetic aspects of hypertension development: analysis in the rat. Physiol Rev 1999; 79: 1227–1282.
Dobesova Z, Kunes J, Zicha J . The altered balance between sympathetic nervous system and nitric oxide in salt hypertensive dahl rats: ontogenetic and F2 hybrid studies. J Hypertens 2002; 20: 945–955.
Zicha J, Vaneckova I, Kunes J . Systems analysis in hypertension: complementary role of physiologists and geneticists. Physiol Res 2010; 59: 837–839.
Rossi GP, Cavallin M, Belloni AS, Mazzocchi G, Nussdorfer GG, Pessina AC, Sartore S . Aortic smooth muscle cell phenotypic modulation and fibrillar collagen deposition in angiotensin II-dependent hypertension. Cardiovasc Res 2002; 55: 178–189.
Gyurko R, Tran D, Phillips MI . Time course of inhibition of hypertension by antisense oligonucleotides targeted to AT1 angiotensin receptor mRNA in spontaneously hypertensive rats. Am J Hypertens 1997; 10: 56S–62S.
Kagiyama S, Varela A, Phillips MI, Galli SM . Antisense inhibition of brain renin-angiotensin system decreased blood pressure in chronic 2-kidney, 1 clip hypertensive rats. Hypertension 2001; 37: 371–375.
Vaneckova I, Kopkan L, Huskova Z, Vanourkova Z, Schejbalova S, Cervenka L, Kramer HJ . Long-term prevention of hypertension and end-organ damage in Ren-2 transgenic rats is achieved only with persistent but not transient AT1 receptor blockade. Kidney Blood Press Res 2007; 30: 38–44.
Rakusan D, Kujal P, Kramer HJ, Huskova Z, Vanourkova Z, Vernerova Z, Mrazova I, Thumova M, Cervenka L, Vaneckova I . Persistent antihypertensive effect of aliskiren is accompanied by reduced proteinuria and normalization of glomerular area in Ren-2 transgenic rats. Am J Physiol Renal Physiol 2010; 299: F758–F766.
Acknowledgements
This study was supported by grant no. IAA 500110902 by The Grant Agency of Academy of Sciences of the Czech Republic and by grant no. 304/12/0259 awarded by the Czech Science foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vaněčková, I., Dobešová, Z., Kuneš, J. et al. The effects of repeated delivery of angiotensin II AT1 receptor antisense on distinct vasoactive systems in Ren-2 transgenic rats: young vs. adult animals. Hypertens Res 35, 761–768 (2012). https://doi.org/10.1038/hr.2012.29
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.29
Keywords
This article is cited by
-
Both central sympathoexcitation and peripheral angiotensin II-dependent vasoconstriction contribute to hypertension development in immature heterozygous Ren-2 transgenic rats
Hypertension Research (2022)
-
Exaggerated blood pressure response to fasudil or nifedipine in hypertensive Ren-2 transgenic rats: role of altered baroreflex
Hypertension Research (2019)