Abstract
The development of atherosclerosis is associated with disturbances in mitochondrial function that impair effective adenosine triphosphate (ATP) production, increase generation of superoxide and induce subsequent apoptosis in vascular smooth muscle cells (VSMCs). As peroxisome proliferator-activated receptor gamma (PPARγ) has a potentially important role in the regulation of mitochondrial metabolism, we studied effects of the partial PPARγ agonist and angiotensin receptor blocker telmisartan, on mitochondria-related cellular responses in VSMC. In human VSMC, telmisartan increased ATP levels and activation of mitochondrial complex II, succinate dehydrogenase, reduced the release of H2O2 and attenuated H2O2-induced increases in caspase 3/7 activity, a marker of cellular apoptosis. Eprosartan, an angiotensin II receptor blocker that lacks the ability to activate PPARγ, had no effect on these mitochondria-related cellular responses in VSMC. Studies in PPARγ-deficient VSMC revealed that the effects of telmisartan on mitochondrial function were largely independent of PPARγ although the presence of PPARγ modulated effects of telmisartan on H2O2 levels. These findings demonstrate that telmisartan can have significant effects on mitochondrial metabolism in VSMC that are potentially relevant to the pathogenesis of cardiovascular disease and that involve more than just angiotensin receptor blockade and activation of PPARγ.
Similar content being viewed by others
Introduction
Mitochondria have a key role in energy production, generation of reactive oxygen species and promotion of cellular apoptosis. Disturbances in mitochondria function may occur in several cardiovascular disorders including atherosclerosis, in which inefficient mitochondrial production of ATP is associated with increases in superoxide generation and apoptosis.1 Ballinger et al.2 reported that aortic samples from atherosclerotic patients had greater mitochondria DNA damage than non-atherosclerotic age-matched aortic samples. They also reported that ApoE knockout mice exhibited mitochondria DNA damage in aorta even at 3 weeks of age when no inflammatory cells adhere to the vessel wall. As mitochondrial DNA is more prone to reactive oxygen species-induced damage than nuclear DNA,3 more efficient energy production with reduced reactive oxygen species generation may protect from mitochondria DNA damage in the vasculature. Thus, identification of drugs that improve mitochondrial function in the vasculature is of potential therapeutic interest. Peroxisome proliferator-activated receptors (PPARs) belong to a superfamily of nuclear transcription factors that can regulate mitochondrial biogenesis and function at least in part through interactions with PPARγ coactivator 1α.4 Among PPARs, PPARγ is a master regulator of adipocyte differentiation, and activation of PPARγ by thiazolidinediones such as pioglitazone is associated with mitochondrial biogenesis and increased energy expenditure in several different tissues.5 The mechanisms whereby thiazolidinediones modulate mitochondrial biogenesis and function are not completely understood and some of their actions may also be mediated in a PPARγ-independent manner.6 Recent reports using smooth muscle-specific PPARγ-deficient mice have shown that PPARγ in vascular smooth muscle cells (VSMCs) has a crucial role in the protection from atherosclerosis and hypertension,7 and that pioglitazone attenuates the development of atherosclerosis via smooth muscle cell-specific interaction with PPARγ.8 Indeed, the anti-atherosclerotic effect of pioglitazone was shown by the recent clinical trial.9 However, the effects of PPARγ agonists on mitochondrial function in VSMCs have not been extensively studied.
Recently, it has been reported that certain angiotensin II receptor type 1 (AT1) blockers such as telmisartan can function as partial agonists of PPARγ10, 11 and can influence several cellular mechanisms of atherosclerosis independent of their ability to block AT1 receptors or lower blood pressure. Although PPARγ appears to be involved in mediating some of the cellular effects of telmisartan,12, 13, 14 we have found that the ability of telmisartan to inhibit proliferation of VSMC may not require either the presence of PPARγ or AT1 receptors.15 Given these observations and the potentially important role of VSMC mitochondria in atherosclerosis, we investigated the effects of telmisartan on mitochondrial-related cellular responses in both wild-type VSMC and in VSMC lacking PPARγ.
Methods
Materials
Telmisartan was obtained from Boehringer Ingelheim (Ingelheim, Germany). Eprosartan and pioglitazone were purchased from Sigma-Aldrich (St Louis, MO, USA).
Cell culture
Human aortic VSMC were purchased from Kurabo (Osaka Japan). Human aortic VSMC were maintained in HuMedia-SB2 (Kurabo) supplemented with 5% fetal bovine serum, 0.5 ng ml−1 human recombinant epidermal growth factor, 2 ng ml−1 basic fibroblast growth factor, 5 μg ml−1 insulin and antibiotics. Aortic VSMC were isolated from smooth muscle cell-specific PPARγ-knockout mice and wild-type littermate controls as described previously.15 These cells were maintained in Dulbecco’s modified Eagle’s medium/F12 (Wako, Osaka, Japan) containing 10% fetal bovine serum (Nichirei Bioscience, Tokyo, Japan) and antibiotics.
ATP assay
Human and mouse aortic VSMC were plated at 1 × 105 cells per well in the indicated medium. After attachment, cells were exposed to pioglitazone, eprosartan or telmisartan dissolved in dimethylsulphoxide (DMSO) added to the same growth medium at selected concentrations. Untreated cells were incubated with an equivalent volume of DMSO added to the medium. Following drug treatment for 24 h, cells were washed with phosphate-buffered saline twice, removed from plates using cell scrapers and subjected to ATP measurement using the ATP Bioluminescence Assay Kit CLS II (Roche, Basel, Switzerland) according to the manufacturer’s instructions. Luciferase luminescence was measured using ARVO SX (PerkinElmer, Waltham, MA, USA) and the concentration of ATP in each sample was estimated by standard curve analysis.
Estimation of mitochondrial succinate dehydrogenase activity by WST-8 assay
Human and mouse aortic VSMC were plated at 5 × 103 cells per well on 96-well plates in the indicated medium. After attachment, cells were exposed to pioglitazone, telmisartan or DMSO vehicle for 48 h. We then performed a WST-8 colorimetric assay according to the manufacturer’s instruction with use of a microplate reader (Viento, Dainippon, Osaka, Japan) to measure absorbance at 450 nm. Counting of viable cells with Trypan blue staining showed that there was no difference in cell numbers among the treatments at the time of measurement (data not shown).
Detection of hydrogen peroxide
Human and mouse aortic VSMC were plated at 2 × 104 cells per well on 24-well plates in 400 μl of the indicated medium. After attachment, cells were exposed to pioglitazone, eprosartan, telmisartan or DMSO vehicle for 24 h. The medium was then replaced including the specified reagents and the cells were incubated for an additional 24 h.
A 50 μl aliquot of conditional medium was transferred to wells in duplicate in a 96-well black plate and measurement of hydrogen peroxide was performed using amplex red according to the manufacturer’s instruction (Invitrogen, Carlsbad, CA, USA). The detection of fluorescence was performed using ARVO SX instrumentation (PerkinElmer) with excitation and emission wavelengths set at 544 and 590 nm, respectively.
Detection of caspase 3/7 activity
Human and mouse aortic VSMC were plated in the indicated medium on 96-well plates at 1 × 104 and 5 × 103 cells per well, respectively. After attachment, cells were exposed to pioglitazone, eprosartan, telmisartan or DMSO vehicle in the indicated medium without fetal bovine serum. VSMC were cultured for 24 h before stimulating them with hydrogen peroxide at a concentration of 700 μM in studies with the human cells or at 400 μM in studies with the mouse cells. The concentrations of hydrogen peroxide used in the study were empirically determined to be sufficient to induce detectable increases in caspase 3/7 activity in control cells. After 6-h stimulation with hydrogen peroxide in the presence of the indicated reagents, measurement of caspase 3/7 activity was performed using Apo-ONE Homogeneous Caspase-3/7 Assay kit according to the manufacturer’s instruction (Promega, Fitchburg, WI, USA) adenosine triphosphate (ATP). The detection of fluorescence was performed using ARVO SX (PerkinElmer, ex/em; 485/535 nm).
Mitochondrial DNA assay
We used the ratio of mitochondrial to nuclear DNA to estimate the influence of telmisartan and pioglitazone on mitochondrial copy number. Human VSMC and wild-type mouse VSMC were treated with pioglitazone, telmisartan or control vehicle in the indicated media for 48 h and DNA was extracted using QIAamp DNA mini kit (Qiagen, Venlo, the Netherlands). In all, 1 pg of DNA template was amplified by real-time PCR to determine relative mitochondrial and nuclear DNA quantity using THUNDERBIRD SYBR qPCR Mix (TOYOBO, Osaka, Japan) on a model 7900 Sequence Detector (Applied Biosystems, Foster City, CA, USA) with primers for human VSMC mitochondrial ND1 gene (Fw: 5′-CCTAAAACCCGCCACATCTA-3′, Rv: 5′-GCCTAGGTTGAGGTTGACCA-3′) and nuclear NEB1 gene (Fw: 5′-AGGGGGAAGAGGAACTGTGT-3′, Rv: 5′-CCATGGGATATTGGGATCTG-3′) and primers for mouse VSMC (mitochondrial 16s gene (Fw: 5′-CCGCAAGGGAAAGATGAAAGAC-3′, Rv: 5′-TCGTTTGGTTTCGGGGTTTC-3′) and nuclear HK6 gene (Fw: 5′-GCCAGCCTCTCCTGATTTTAGTGT-3′, Rv: 5′-GGGAACACAAAAGACCTCTTCTGG-3′).
Quantitative real-time PCR
Wild-type mice VSMC were treated with pioglitazone, or telmisartan in the indicated media for 2.5, 5, 10 or 24 h. Cells treated with vehicle DMSO for 24 h were used as baseline control (0 h). All RNA samples were simultaneously purified using a RNeasy Mini Kit (Qiagen). The RNA samples were converted into cDNA with High Capacity cDNA Reverse Transcription Kit (Applied Biosystems). Quantitative real-time PCR was performed and analyzed on a model 7900 Sequence Detector (Applied Biosystems) with Taqman gene expression assays for cytochrome c oxidase subunit IV isoform 1, PPARγ coactivator 1α, sirtuin 1, mitochondrial cytochrome c oxidase subunit I, mitochondrial transcription factor A and manganese superoxide dismutase (MnSOD) (TaqMan gene expression assays, Applied Biosystems). The expression level of each gene was normalized by 18s ribosomal RNA as an internal control.
Statistical analysis
Data are expressed as mean±s.e.m. To compare multiple treatments, statistical analysis was performed by one-way analysis of variance and post hoc analysis with the Holm–Sidak test to adjust for multiple comparisons of individual data groups against control.
Results
Effects of telmisartan on ATP production and H2O2 levels in human aortic VSMC
We first assessed mitochondrial function in human aortic VSMC by measuring ATP levels and activity of mitochondrial complex II, succinate dehydrogenase as estimated by the WST-8 assay after 24 h of exposure to telmisartan, pioglitazone, eprosartan or vehicle control. Both telmisartan and pioglitazone increased ATP levels and mitochondrial succinate dehydrogenase activity, whereas eprosartan, an angiotensin receptor blocker that lacks the ability to activate PPARγ did not (Figure 1 upper panel). Previous studies have established that the drug concentrations tested are sufficient for telmisartan and pioglitazone to achieve their maximal levels of PPARγ activation and for telmisartan and eprosartan to fully block AT1 receptors.10, 16 The effect of telmisartan on ATP levels was dose dependent, whereas mitochondrial succinate dehydrogenase activity in cells treated by telmisartan did not differ at concentrations between 1 and 10 μM (Figure 1 lower panel).
ATP levels and mitochondrial succinate dehydrogenase activity in human vascular smooth muscle cell (VSMC). ATP levels (upper panel) and mitochondrial succinate dehydrogenase activity measured by WST-8 assay (lower panel) in human aortic VSMC. Results were normalized relative to 0 μM vehicle control. *Statistically significant vs. 0 μM vehicle control by one-way analysis of variance.
As inefficiencies in mitochondrial electron transport generate superoxide anion, which is reduced by superoxide dismutase to hydrogen peroxide, we measured the effects of telmisartan on H2O2 levels in the growth medium of human VSMC. We found that telmisartan at a concentration of 10 μM was associated with reduced levels of H2O2 (Figure 2). Pioglitazone also reduced levels of H2O2 in human VSMC. In contrast, eprosartan had no effect on H2O2 release (Figure 2).
Effect of telmisartan on hydrogen peroxide-induced apoptosis of human aortic VSMC
In addition to regulating energy production and generation of reactive oxygen species, mitochondria have a key role in apoptosis by activating caspase signaling in response to cellular damage.17 To test the effects of telmisartan on cellular apoptosis, human VSMC were exposed to 700 μM H2O2. Six-hour exposure to hydrogen peroxide significantly increased caspase 3/7 activity in human VSMC. Telmisartan at concentrations of 2.5 μM and above attenuated the effects of H2O2 on caspase activity in a dose-independent manner (Figure 3) In contrast, pioglitazone appeared to enhance H2O2-induced increases in caspase 3/7 activity (Figure 3). Eprosartan at concentration of 10 and 20 μM had no or little effect on caspase 3/7 activity in human VSMC (Figure 3).
Involvement of PPARγ in the effect of telmisartan on mitochondrial function
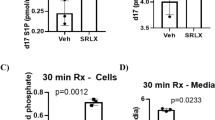
To investigate the role of PPARγ activation in the observed actions of telmisartan, we studied drug effects in VSMC from smooth muscle-specific PPARγ-deficient mice and wild-type control mice. Telmisartan increased ATP levels and activity of mitochondrial succinate dehydrogenase equally between PPARγ-deficient and wild-type control VSMC (Figure 4a left panel). The ability of pioglitazone to increase succinate dehydrogenase activity was attenuated in PPARγ-deficient cells vs. wild-type controls, whereas pioglitazone significantly increased ATP levels in both types of VSMC (Figure 4a right panel). Telmisartan and pioglitazone increased release of H2O2 levels in PPARγ-deficient VSMC. In contrast, telmisartan did not change H2O2 levels and pioglitazone reduced H2O2 levels in wild-type control cells, suggesting an antioxidative effect of PPARγ activation (Figure 4b). In wild-type VSMC, telmisartan did not alter H2O2-induced increase in caspase 3/7 activity, whereas telmisartan reduced H2O2-induced apoptosis in PPARγ-deficient VSMC (Figure 4c). In contrast, pioglitazone prominently enhanced H2O2-induced apoptosis in PPARγ-deficient and control VSMC although somewhat less so in the PPARγ knockout cells (Figure 4c).
ATP levels, mitochondrial succinate dehydrogenase activity and production of H2O2 in peroxisome proliferator-activated receptor gamma (PPARγ)-deficient and wild-type vascular smooth muscle cell (VSMC). Effects of 10 μM telmisartan and 10 μM pioglitazone on (a) ATP levels and mitochondrial succinate dehydrogenase activity, (b) H2O2 release and (c) H2O2-induced caspase 3/7 activation. Results were normalized relative to cell type-matched vehicle control. (a, b) *Statistically significant vs. cell type-matched vehicle control by one-way analysis of variance (ANOVA). (c) *Statistically significant vs. cell type-matched vehicle control with H2O2 treatment by one-way ANOVA.
Effect of telmisartan on mitochondrial DNA copy number and mitochondria-related gene expression
Mitochondrial DNA copy number was not altered by 2 days treatment of telmisartan and pioglitazone, suggesting that mitochondrial biogenesis was not involved in the observed effects on mitochondrial function in human and mouse wild-type VSMC (Figure 5a). We also measured relative expression levels of five genes, which are associated with the regulation of mitochondrial protein expression and or mitochondrial function in mouse VSMC (Figure 5b). Telmisartan and pioglitazone did not alter the expression levels of cytochrome c oxidase subunit IV isoform 1, sirtuin 1 and mitochondrial transcription factor A. Pioglitazone transiently induced significant increases in PPARγ coactivator 1α gene expression, whereas the stimulatory effect of telmisartan did not reach statistical significance. Pioglitazone induced sustained increases in expression of the gene for mitochondrial cytochrome c oxidase subunit I, whereas telmisartan induced a transient increase in expression of mitochondrial cytochrome c oxidase subunit I.
Effects of telmisartan vs. pioglitazone on mitochondrial copy number and the expression of mitochondria-related genes. (a) Mitochondrial/nuclear DNA ratio in human (left) and mouse (right) vascular smooth muscle cell (VSMC) treated with 10 μM telmisartan or 10 μM pioglitazone. Results were normalized relative to vehicle treated control. (b) Relative expression levels of mitochondria-related genes in mouse VSMC treated with 10 μM telmisartan or 10 μM pioglitazone at different time points. Results were normalized relative to expression levels of baseline control (0 h). *Statistically significant vs. baseline by one-way analysis of variance. Cox4l1, cytochrome c oxidase subunit IV isoform 1; PGC1α, peroxisome proliferator-activated receptor gamma coactivator 1-α; SIRT1, sirtuin 1; TFAM, mitochondrial transcription factor A.
Discussion
In this study, telmisartan increased ATP levels and mitochondrial succinate dehydrogenase activity in human VSMC. The increases in ATP levels induced by the drug were accompanied by decreases in cellular release of H2O2, an indirect marker for superoxide anion generation by mitochondria. We found that pioglitazone had similar effects on these mitochondria-related parameters. In contrast, we found that telmisartan and pioglitazone exerted markedly different effects on cellular apoptosis. Consistent with previous studies, pioglitazone enhanced H2O2 -induced cellular apoptosis as reflected by increases in caspase 3/7 activity in human VSMC.18, 19 Telmisartan attenuated H2O2-induced increases in caspase 3/7 activity and subsequent apoptosis. The clinical implications of the anti-apoptotic effects of telmisartan remain unclear. However, it has been reported that telmisartan can prevent aneurysm progression by inhibiting apoptosis in elastase-infused rat models of vascular disease.20
The observed effects of telmisartan in human VSMC appear to involve more than just AT1 blockade because (1) all the experiments were performed in the absence of exogenous application of angiotensin II and (2) eprosartan had no effect on the observed cellular responses when tested at concentrations known to be sufficient to induce AT1 blockade.
It has been previously reported that the effects of thiazolidinediones including pioglitazone on mitochondrial function involve both PPARγ-dependent and -independent pathways.6 In the current studies, we studied PPARγ-deficient and control VSMC to elucidate the role of PPARγ in the observed effects of telmisartan on mitochondrial function. PPARγ knockout had little or no effect on the ability of telmisartan to increase ATP levels and mitochondrial succinate dehydrogenase activity suggesting that telmisartan is affecting these parameters of mitochondrial function through pathways that do not depend on activation of PPARγ. In contrast, PPARγ knockout significantly attenuated the ability of pioglitazone to increase mitochondrial succinate dehydrogenase activity.
Telmisartan reduced the release of H2O2 into culture media of human VSMC and pioglitazone reduced the release of H2O2 into culture media of both human VSMC and mouse VSMC. PPARγ knockout reversed these inhibitory effects of telmisartan and pioglitazone on H2O2 release; in the cells lacking PPARγ, both drugs appeared to stimulate release of H2O2. These observations suggest that PPARγ is involved in modulating effects of telmisartan and pioglitazone on mitochondrial oxidative stress and generation of H2O2. PPARγ activation is known to promote anti-oxidant effects including upregulation of glutathione peroxidase.21 PPARγ activation also affects expression of uncoupling proteins that may influence proton transport back into the mitochondria matrix.22 Such PPARγ-dependent anti-oxidative mechanisms could help to counteract increases in H2O2 that otherwise appear to be induced by telmisartan or pioglitazone in cells that lack PPARγ. In contrast, the presence or absence of PPARγ had less influence on the differential effects of pioglitazone and telmisartan on cellular apoptosis induced by H2O2. In cells with or without PPARγ, pioglitazone enhanced H2O2-induced apoptosis whereas telmisartan tended to inhibit H2O2-induced apoptosis. Overall, telmisartan appeared to protect against oxidative stress and cellular apoptosis more in human VSMC than in mouse VSMC, although the mechanism for the species differences in drug responsiveness remain to be defined.
In this study, we did not observe any changes in mitochondrial DNA copy number induced by pioglitazone or telmisartan. Previous studies have shown that pioglitazone can promote mitochondrial biogenesis in adipocytes5 and that telmisartan may promote mitochondrial biogenesis in human coronary artery endothelial cells.23 The differences between the results of the current studies in VSMC vs. those of previous studies in other cell types might be related to differences in cell-specific responses or in experimental conditions.5 Although we did not detect any obvious drug effects on mitochondrial DNA copy number, we did observe some differential effects of pioglitazone and telmisartan on expression of genes related to mitochondrial function. Pioglitazone induced greater increases than telmisartan in the expression of PPARγ coactivator 1α, a key modulator of mitochondrial gene expression,4 Compared with telmisartan, pioglitazone also induced a more sustained increase in the expression of mitochondrial cytochrome c oxidase subunit I that is encoded by mitochondrial DNA. These results suggest that pioglitazone and telmisartan differentially affect the expression of mitochondria-related genes.
We previously reported that telmisartan attenuated proliferation of VSMCs with reduction in AKT phosphorylation. Activation of phosphoinositide-3-kinase–AKT pathway has been reported to enhance mitochondrial function,24 although recent studies have also indicated that activation of mitochondrial function by phosphoinositide-3-kinase signaling may be independent of AKT phosphorylation.25 Based on these observations, it does not seem likely that reductions in AKT phosphorylation are mediating the effects of telmisartan on mitochondrial function that we observed in the current studies.
One of the features that distinguishes telmisartan from other angiotensin receptor blockers is that it is highly lipophilic and may have a greater ability to penetrate into cells than other angiotensin II antagonists. Indeed, it was reported that concentrations of telmisartan achieved inside of cells may be 10-fold greater than outside of cells.26 Recent reports have indicated that angiotensin II and its receptors are colocalized in mitochondrial inner membrane and that mitochondrial angiotensin II signaling may alter mitochondrial function.27, 28 Taken together, these observations may motivate future studies on the role of mitochondrial AT1 blockade in mediating some of the effects of telmisartan on mitochondrial function.
Previous studies have shown that telmisartan also activates PPARα and PPARδ. For example, telmisartan was shown to reduce hepatic and serum triglycerides by activating PPARα,29 and to attenuate weight gain and obesity through activation of PPARδ pathways.30 Although the PPARα-activating property of telmisartan was observed in hepatocytes at concentrations of >10 μM, telmisartan activated PPARδ in 3T3 adipocytes starting at concentrations as low as 1 μM. Accumulating evidence has shown that both PPARα and PPARδ isoforms can affect mitochondrial biogenesis and function. PPARα can stimulate mitochondrial fatty acid β-oxidation in liver and skeletal muscle31 and PPARα activation by adipose triglyceride lipase can regulate mitochondrial function in heart.32 The effect of PPARδ on mitochondrial biogenesis and function has been mainly observed in skeletal muscle and heart.33, 34 Although the roles of PPARα and PPARδ in regulating mitochondrial function of VSMCs remain to be determined, both PPARα and PPARδ agonists have been reported to inhibit the proliferation of VSMCs.35, 36 In light of the apparent pan-agonistic properties of telmisartan, future studies should also be conducted to investigate if telmisartan affects mitochondrial function in VSMCs through effects on multiple PPAR isoforms.
The primary therapeutic target of telmisartan is hypertension, a condition associated with increased mitochondrial DNA damage and vascular disturbances in mitochondrial function.37, 38, 39, 40 The current findings that telmisartan increases ATP levels and mitochondrial succinate dehydrogenase activity, and reduces generation of H2O2 in cultured VSMC suggest that telmisartan may have beneficial effects on mitochondrial function through mechanisms that do not simply depend on its ability to block plasma membrane AT1 receptors and reduce blood pressure. The current findings also indicate that some of the effects of telmisartan on mitochondrial function in VSMCs involve more than just PPARγ activation. In addition, accumulating evidences have suggested that altered mitochondrial function is associated with the development of several risk factors of atherosclerosis, such as diabetes and obesity.41 Thus, our results could serve to motivate future studies on the relationship between alterations in mitochondrial metabolism and the anti-atherosclerotic actions of telmisartan.
References
Madamanchi NR, Runge MS . Mitochondrial dysfunction in atherosclerosis. Circ Res 2007; 100: 460–473.
Ballinger SW, Patterson C, Knight-Lozano CA, Burow DL, Conklin CA, Hu Z, Reuf J, Horaist C, Lebovitz R, Hunter GC, McIntyre K, Runge MS . Mitochondrial integrity and function in atherogenesis. Circulation 2002; 106: 544–549.
Yakes FM, Van Houten B . Mitochondrial DNA damage is more extensive and persists longer than nuclear DNA damage in human cells following oxidative stress. Proc Natl Acad Sci USA 1997; 94: 514–519.
Liang H, Ward WF . PGC-1alpha: a key regulator of energy metabolism. Adv Physiol Educ 2006; 30: 145–151.
Bogacka I, Xie H, Bray GA, Smith SR . Pioglitazone induces mitochondrial biogenesis in human subcutaneous adipose tissue in vivo. Diabetes 2005; 54: 1392–1399.
Feinstein DL, Spagnolo A, Akar C, Weinberg G, Murphy P, Gavrilyuk V, Dello RC . Receptor-independent actions of PPAR thiazolidinedione agonists: is mitochondrial function the key? Biochem Pharmacol 2005; 70: 177–188.
Halabi CM, Beyer AM, de Lange WJ, Keen HL, Baumbach GL, Faraci FM, Sigmund CD . Interference with PPAR gamma function in smooth muscle causes vascular dysfunction and hypertension. Cell Metab 2008; 7: 215–226.
Subramanian V, Golledge J, Ijaz T, Bruemmer D, Daugherty A . Pioglitazone-induced reductions in atherosclerosis occur via smooth muscle cell-specific interaction with PPAR{gamma}. Circ Res 2010; 107: 953–958.
Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefebvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Koranyi L, Laakso M, Mokan M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J . Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005; 366: 1279–1289.
Benson SC, Pershadsingh HA, Ho CI, Chittiboyina A, Desai P, Pravenec M, Qi N, Wang J, Avery MA, Kurtz TW . Identification of telmisartan as a unique angiotensin II receptor antagonist with selective PPARgamma-modulating activity. Hypertension 2004; 43: 993–1002.
Schupp M, Janke J, Clasen R, Unger T, Kintscher U . Angiotensin type 1 receptor blockers induce peroxisome proliferator-activated receptor-gamma activity. Circulation 2004; 109: 2054–2057.
Clasen R, Schupp M, Foryst-Ludwig A, Sprang C, Clemenz M, Krikov M, Thone-Reineke C, Unger T, Kintscher U . PPARgamma-activating angiotensin type-1 receptor blockers induce adiponectin. Hypertension 2005; 46: 137–143.
Scalera F, Martens-Lobenhoffer J, Bukowska A, Lendeckel U, Tager M, Bode-Boger SM . Effect of telmisartan on nitric oxide--asymmetrical dimethylarginine system: role of angiotensin II type 1 receptor gamma and peroxisome proliferator activated receptor gamma signaling during endothelial aging. Hypertension 2008; 51: 696–703.
Walcher D, Hess K, Heinz P, Petscher K, Vasic D, Kintscher U, Clemenz M, Hartge M, Raps K, Hombach V, Marx N . Telmisartan inhibits CD4-positive lymphocyte migration independent of the angiotensin type 1 receptor via peroxisome proliferator-activated receptor-gamma. Hypertension 2008; 51: 259–266.
Yamamoto K, Ohishi M, Ho C, Kurtz TW, Rakugi H . Telmisartan-induced inhibition of vascular cell proliferation beyond angiotensin receptor blockade and peroxisome proliferator-activated receptor-gamma activation. Hypertension 2009; 54: 1353–1359.
Maillard MP, Perregaux C, Centeno C, Stangier J, Wienen W, Brunner HR, Burnier M . In vitro and in vivo characterization of the activity of telmisartan: an insurmountable angiotensin II receptor antagonist. J Pharmacol Exp Ther 2002; 302: 1089–1095.
Green DR, Reed JC . Mitochondria and apoptosis. Science 1998; 281: 1309–1312.
Aizawa Y, Kawabe J, Hasebe N, Takehara N, Kikuchi K . Pioglitazone enhances cytokine-induced apoptosis in vascular smooth muscle cells and reduces intimal hyperplasia. Circulation 2001; 104: 455–460.
Thorp E, Kuriakose G, Shah YM, Gonzalez FJ, Tabas I . Pioglitazone increases macrophage apoptosis and plaque necrosis in advanced atherosclerotic lesions of nondiabetic low-density lipoprotein receptor-null mice. Circulation 2007; 116: 2182–2190.
Kaschina E, Schrader F, Sommerfeld M, Kemnitz UR, Grzesiak A, Krikov M, Unger T . Telmisartan prevents aneurysm progression in the rat by inhibiting proteolysis, apoptosis and inflammation. J Hypertens 2008; 26: 2361–2373.
Chung SS, Kim M, Youn BS, Lee NS, Park JW, Lee IK, Lee YS, Kim JB, Cho YM, Lee HK, Park KS . Glutathione peroxidase 3 mediates the antioxidant effect of peroxisome proliferator-activated receptor gamma in human skeletal muscle cells. Mol Cell Biol 2009; 29: 20–30.
Villarroya F, Iglesias R, Giralt M . PPARs in the control of uncoupling proteins gene expression. PPAR Res 2007; 2007: 74364.
Nozaki T . Telmisartan enhances mitochondrial biogenesis and protects from endothelial cell damage through peroxisome proliferator-activated receptor-γindependent pathways. AHA annual meeting, Circulation 2009; 120: S1039–S1040.
O’Neill BT, Kim J, Wende AR, Theobald HA, Tuinei J, Buchanan J, Guo A, Zaha VG, Davis DK, Schell JC, Boudina S, Wayment B, Litwin SE, Shioi T, Izumo S, Birnbaum MJ, Abel ED . A conserved role for phosphatidylinositol 3-kinase but not Akt signaling in mitochondrial adaptations that accompany physiological cardiac hypertrophy. Cell Metab 2007; 6: 294–306.
Stiles BL . PI-3-Kand AKT: onto the mitochondria. Adv Drug Deliv Rev 2009; 61: 1276–1282.
Shao J, Nangaku M, Inagi R, Kato H, Miyata T, Matsusaka T, Noiri E, Fujita T . Receptor-independent intracellular radical scavenging activity of an angiotensin II receptor blocker. J Hypertens 2007; 25: 1643–1649.
Abadir PM, Foster DB, Crow M, Cooke CA, Rucker JJ, Jain A, Smith BJ, Burks TN, Cohn RD, Fedarko NS, Carey RM, O'Rourke B, Walston JD . Identification and characterization of a functional mitochondrial angiotensin system. Proc Natl Acad Sci USA 2011; 108: 14849–14854.
Cook JL, Re RN . Lessons from in vitro studies and a related intracellular angiotensin II transgenic mouse model. Am J Physiol Regul Integr Comp Physiol 2012; 302: R482–R493.
Clemenz M, Frost N, Schupp M, Caron S, Foryst-Ludwig A, Bohm C, Hartge M, Gust R, Staels B, Unger T, Kintscher U . Liver-specific peroxisome proliferator-activated receptor alpha target gene regulation by the angiotensin type 1 receptor blocker telmisartan. Diabetes 2008; 57: 1405–1413.
He H, Yang D, Ma L, Luo Z, Ma S, Feng X, Cao T, Yan Z, Liu D, Tepel M, Zhu Z . Telmisartan prevents weight gain and obesity through activation of peroxisome proliferator-activated receptor-delta-dependent pathways. Hypertension 2010; 55: 869–879.
Minnich A, Tian N, Byan L, Bilder G . A potent PPARalpha agonist stimulates mitochondrial fatty acid beta-oxidation in liver and skeletal muscle. Am J Physiol Endocrinol Metab 2001; 280: E270–E279.
Haemmerle G, Moustafa T, Woelkart G, Buttner S, Schmidt A, van de Weijer T, Hesselink M, Jaeger D, Kienesberger PC, Zierler K, Schreiber R, Eichmann T, Kolb D, Kotzbeck P, Schweiger M, Kumari M, Eder S, Schoiswohl G, Wongsiriroj N, Pollak NM, Radner FP, Preiss-Landl K, Kolbe T, Rulicke T, Pieske B, Trauner M, Lass A, Zimmermann R, Hoefler G, Cinti S, Kershaw EE, Schrauwen P, Madeo F, Mayer B, Zechner R . ATGL-mediated fat catabolism regulates cardiac mitochondrial function via PPAR-alpha and PGC-1. Nat Med 2011; 17: 1076–1085.
Burkart EM, Sambandam N, Han X, Gross RW, Courtois M, Gierasch CM, Shoghi K, Welch MJ, Kelly DP . Nuclear receptors PPARbeta/delta and PPARalpha direct distinct metabolic regulatory programs in the mouse heart. J Clin Invest 2007; 117: 3930–3939.
Wang P, Liu J, Li Y, Wu S, Luo J, Yang H, Subbiah R, Chatham J, Zhelyabovska O, Yang Q . Peroxisome proliferator-activated receptor {delta} is an essential transcriptional regulator for mitochondrial protection and biogenesis in adult heart. Circ Res 2010; 106: 911–919.
Gizard F, Nomiyama T, Zhao Y, Findeisen HM, Heywood EB, Jones KL, Staels B, Bruemmer D . The PPARalpha/p16INK4a pathway inhibits vascular smooth muscle cell proliferation by repressing cell cycle-dependent telomerase activation. Circ Res 2008; 103: 1155–1163.
Lim HJ, Lee S, Park JH, Lee KS, Choi HE, Chung KS, Lee HH, Park HY . PPAR delta agonist L-165041 inhibits rat vascular smooth muscle cell proliferation and migration via inhibition of cell cycle. Atherosclerosis 2009; 202: 446–454.
Atlante A, Seccia TM, Pierro P, Vulpis V, Marra E, Pirrelli A, Passarella S . ATP synthesis and export in heart left ventricle mitochondria from spontaneously hypertensive rat. Int J Mol Med 1998; 1: 709–716.
Graham D, Huynh NN, Hamilton CA, Beattie E, Smith RA, Cocheme HM, Murphy MP, Dominiczak AF . Mitochondria-targeted antioxidant MitoQ10 improves endothelial function and attenuates cardiac hypertrophy. Hypertension 2009; 54: 322–328.
Wang S, Li R, Fettermann A, Li Z, Qian Y, Liu Y, Wang X, Zhou A, Mo JQ, Yang L, Jiang P, Taschner A, Rossmanith W, Guan MX . Maternally inherited essential hypertension is associated with the novel 4263A>G mutation in the mitochondrial tRNAIle gene in a large Han Chinese family. Ccir Res 2011; 108: 862–870.
Wilson FH, Hariri A, Farhi A, Zhao H, Petersen KF, Toka HR, Nelson-Williams C, Raja KM, Kashgarian M, Shulman GI, Scheinman SJ, Lifton RP . A cluster of metabolic defects caused by mutation in a mitochondrial tRNA. Science 2004; 306: 1190–1194.
Hojlund K, Mogensen M, Sahlin K, Beck-Nielsen H . Mitochondrial dysfunction in type 2 diabetes and obesity. Endocrinol Metab Clin North Am 2008; 37: 713–731 x.
Acknowledgements
We are most grateful to Kazuko Iwasa, Takako Baba and Yuki Imaizumi at Osaka University for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takeuchi, K., Yamamoto, K., Ohishi, M. et al. Telmisartan modulates mitochondrial function in vascular smooth muscle cells. Hypertens Res 36, 433–439 (2013). https://doi.org/10.1038/hr.2012.199
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.199