Abstract
Aortic stiffness (pulse wave velocity, PWV) and pressure wave reflections (augmentation index, AI) are two interrelated markers of mortality. Their potential synergistic effect on mortality has never been studied. We sought to investigate the association as well as the combined effect of PWV and AI on mortality in a cohort (PROTEGER Study) of very old (>70 years, mean age (±s.d.): 85.4±7.4 years). Aortic PWV and pressure wave AI were assessed by pulse wave analysis; carotid structure and cardiac function were analyzed by ultrasound. The analysis was performed in 259 patients who had all the data available. Neither PWV nor AI was, in separate, predictors of mortality (log-rank test: P=0.278 and P=0.433, respectively, Kaplan–Meier analysis). No linear association was found between PWV and AI (P=0.278). To investigate the possible synergistic effect of PWV and AI on mortality, the population was analyzed according to the tertiles of PWV and AI. Subjects with combined high PWV (third tertile) and moderate-to-high AI (second and third tertiles) had lower survival compared with the rest of the population (Kaplan–Meier survival curve, log-rank test: P=0.030). Cox regression analysis showed that this effect was independent from age, gender, blood pressure, cardiac/carotid parameters and other confounders, except creatinine and insulin resistance. The present study provides further insight on the pathophysiological association between large artery stiffness and pressure wave reflections, suggesting that when both are elevated they may increase the mortality in the elderly.
Similar content being viewed by others
Introduction
In elderly populations, traditional cardiovascular (CV) risk factors are known to be less informative regarding the prediction of mortality.1, 2 The PROTEGER Study was designed to detect markers (arterial, cardiac, metabolic or nutritional) that further provide prognostic information on the survival of elderly subjects with CV disease or high CV risk. Aortic stiffness, assessed by the carotid-femoral pulse wave velocity (PWV), is a robust predictor of mortality in the general as well as in the elderly population.3, 4, 5 In the PROTEGER Study, no association between carotid-femoral PWV and mortality was found.6, 7 Augmentation index (AI), a marker of pressure wave reflections, is also an independent predictor of mortality.8 The current theory of wave reflections suggests that AI is positively associated with aortic PWV. This association may represent a mechanism, which is at least partly responsible for the deleterious effects of aortic stiffening, as it leads to increased left ventricular afterload. However, it is not consistent; it is disrupted by aging,9, 10 inflammation11 or insulin resistance.12
In the present study, our aim was to investigate the potential synergistic effect of aortic PWV and AI on mortality, which has never been investigated before. We tested whether the classical linear association between these two hemodynamic parameters (PWV and AI) is disrupted in the frail and elderly population of the PROTEGER Study, as previously described in other cohorts.9 Moreover, we performed a post hoc analysis to investigate the potential synergistic effect of PWV and AI (as assessed by dividing the population in tertiles of PWV and AI) on mortality, independently from blood pressure (BP) level and other confounders.
Methods
Study cohort
From May 2000 to November 2001, all patients entering the Geriatric Departments of Charles Foix and Emile Roux Hospitals, Ile de France, and meeting the following inclusion criteria: age >70 years old, history of CV disease (including coronary heart disease, cerebro–vascular disease or any other CV events of the upper or lower limbs, thoracic or abdominal aorta, or renal arteries) or hypertension, mini mental status examination >15/30, absence of fatal disease with life expectancy<1 month, willingness to give a written informed consent to participate in this study were included in the PROTEGER Study. Patients with cachexia (body mass index, BMI<17 kg m−2) and/or evolutive cancer and/or advanced renal failure (plasma creatinine >250 μmol l−1) were excluded from the study.
The study cohort was then composed of 331 subjects (86 men and 245 women) with mean age (±s.d.) of 85±7 years. Approximately 13% were hospitalized because of dementia or neuropsychological problems, 35% because of traumatism, 23% because of CV disease event, 9% because of infectious disease, 9% because of social reasons and 11% for other miscellaneous causes. The PROTEGER Study was approved by the Committee for the Protection of Human Subjects in Biomedical Research of Saint Germain Hospital (Ile de France). Written informed consent was obtained from all participants, after informing them as well as their relatives.
Only the parameters that were relevant to the present analysis are presented below.
Social, anthropometric and clinical parameters
Information compiled from the questionnaire filled out at inclusion included gender, age, weight and height, history of CV event, the presence of diabetes mellitus, dyslipidemia, hypertension, smoking habits and previous diseases. The reason for hospitalization as well as the level of education (1: primary school, 2: college degree, 3: bachelor degree, 4: university degree) was registered.
Medications
Antihypertensive drugs included: diuretics (38.0%), calcium channel antagonists (27.9%), angiotensin-converting enzyme inhibitors (26.1%), β-blockers (12.3%), α-blockers (4.0%) and central acting agents (3.1%), either alone or in combination. Approximately 3% of the patients were medically treated for dyslipidemia (drugs, including statins or fibrates) and 14% for diabetes mellitus (drugs, including sulfonamides and/or biguanids, or insulin).
Assessment of BP, arterial stiffness and pressure wave reflections
The measurements were performed in the morning, after an overnight fast, in supine position. Brachial BP was measured after 15 min rest, using the semi-automatic oscillometric device, Dynamap (Kontron, Paris, France). Five measurements, 2 min apart, were averaged.
AI was assessed by means of applanation tonometry and by application of pulse wave analysis (PWA) at the level of the carotid artery; the carotid pressure waveform was calculated as previously described.6, 13
Aortic PWV was determined using the foot-to-foot method as previously described6 (Complior, Colson, Paris, France). The superficial distance covered by the pulse wave was measured directly from the carotid to the femoral artery.
Measurement of carotid and cardiac ultrasound parameters
The presence of carotid plaques was assessed by a high-resolution B-mode (7.5 MHz transducer, Kontron 440). Echocardiograms were recorded with an ultrasound system (Kontron 440) using a 2.5-MHz phased-array transducer. Cardiac measurements were performed according to the American Society of Echocardiography by M-mode measurements (LV mass: 0.8 (1.04 ([LVIDD+PWTD+IVSTD]3− [LVIDD]3))+ 0.6 g) where LVIDD=left ventricular internal diameter in diastole; PWTD=posterior wall thickness in diastole; IVSTD=interventricular septum thickness in diastole . It was possible to evaluate left ventricular volumes only with left ventricular diameters (D) assuming that the geometric shape of the ventricle was an ellipse. Then the volume of this ellipse was expressed as: V=(4π/3) (2D/2) (D/2) (D/2)=πD3/3≈D3. Cardiac output (Q) was calculated with the formula: stroke volume (SV) × heart rate. Total peripheral vascular resistance (TPR), as: TPR=MBP/Q. Echocardiograms were also used to evaluate the diastolic index: E wave deceleration slope time.
Measurement of biological parameters
Venous blood samples were obtained in subjects after an overnight fast. Plasma was separated without delay at 4°C in a refrigerated centrifuge and stored at 4°C (for the determination of routine chemistry profile by standard methods) until analysis. Total cholesterol and triglycerides were determined with the use of a Technicon Chem assay (Technicon Instruments), and HDL cholesterol was measured in the supernatant after precipitation of apolipoprotein B-containing lipoproteins with heparin-manganese chloride. Low-density lipoprotein cholesterol was calculated by the formula of Friedewald for patients with serum triglyceride concentrations<4.0 mmol l−1. Blood cells counts were determined (Argos 3, ABX, Montpellier, France), and the plasma creatinine (Hitachi 911 analyzer with Roche reagents, Roche Hitachi, Paris, France) levels were measured. Plasma albumin was determined using immunonephelometric methods on Immage system (Beckman Coulter, Villepinte, France).
Follow-up procedures
Follow-up started from the baseline examination and lasted until April 2004. Information was obtained from the patient himself, from relatives or from general practitioners. Interim telephone and clinic contacts were used to assess all hospitalizations and outpatient CV diagnoses, and overall mortality. In case of hospitalization, discharge reports from medical specialists were obtained. Follow-up time was defined as the time from the baseline visit until the first event (for those who had an event) or it was censored at the last contact date (for those who did not have any event or for the three patients that were lost to follow-up). Of all 331 participants in the present study, 3 were lost to follow-up; the mean duration of follow up was 380±196 days.
Statistics
The current analysis was performed only in those subjects who had all the needed data available (n=259). Linear regression analysis was used to detect the presence of association between AI and PWV. To investigate the incidence of mortality according to the level of PWV and AI, we divided the population according to tertiles of PWV and AI. Kaplan–Meier survival curve analysis and log-rank test were applied to detect differences in the survival of the patients according to the level of AI or PWV independently or in combination. Cox regression analysis was applied to investigate the combined effect AI and PWV on mortality independently from other confounding factors. Statistical tests such as t- and χ2-tests, as appropriate, were applied to detect the presence of differences regarding CV risk factors, drugs, metabolic, biochemical and inflammatory parameters between subgroups according to the level of AI and PWV. Analysis of covariance was applied to detect differences in hemodynamic, cardiac and vascular parameters among subgroups of the population, after adjustment for covariates. Statistical analysis was performed on a SPSS 11.5 version. A P<0.05 was considered statistically significant.
Results
Out of the 259 subjects, 87 (33.6%) died during the follow-up period. Their demographics are provided in Table 1.
In total population, no linear association was found between AI and PWV (r=−0.068, P=0.278). Neither AI (divided in tertiles) nor PWV (divided in tertiles) was associated with mortality (log-rank test for total mortality by Kaplan–Meier analysis: P=0.433 and P=0.192, respectively).
Mortality according to the level (tertile) of PWV and AI is provided in Table 2. Subjects in the third tertile of PWV (higher level of stiffness) had higher than the average (>33.6%) mortality, except from those who had at the same time low AI (first tertile of AI). On the contrary, subjects in the third tertile of AI (higher level of wave reflections) had lower than average (<33.6%) mortality, except from those who had at the same time very high PWV (third tertile of PWV).
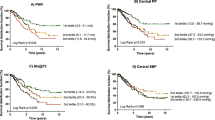
We further explored the presence of potential excess mortality in subjects with both impaired PWV and AI as suggested by Table 2 (gray boxes: group A). Kaplan–Meier survival curve analysis showed that group A had higher overall mortality than the rest of the population (group B), log-rank P=0.030 (Figure 1). When performing Kaplan–Meier analysis for non-CV (n=60) and for established CV (n=27) death separately, we found a similar (but nonsignificant) trend (P=0.115 and P=0.123, respectively).
Kaplan–Meier survival curve analysis and log-rank test were applied to detect differences in the survival of the patients according to the level of pulse wave velocity (PWV) and augmentation index (AI), as defined in Table 2.
To investigate the potential causes that may lead to higher overall mortality in subjects with high PWV combined with moderate-to-high AI (group A), we compared by independent groups t-test and χ2-test (Table 3) the potential confounding factors between group A and group B. No significant differences regarding: age, gender, weight, educational status, mini mental scale, as well as regarding the presence of diabetes mellitus, hypertension, arrhythmia, smoking, renal function, history for stroke and coronary heart disease, the use of drugs (except from calcium channel antagonists, P=0.037), as well as metabolic and biochemical were observed. Similarly we tested for differences between group A and group B regarding hemodynamic and vascular parameters (Table 4). Group A had significantly higher SBP, DBP, MBP, PP, PWV (even after adjustment for age, gender, MBP), AI (even after adjustment for age, gender, HR), as well as lower HR and TPR. Cardiac and carotid parameters (LV mass, EF, diastolic function, percentage of carotid plaques) were similar between the two groups.
Cox regression analysis (Table 5) showed that subjects with both high PWV and moderate-to-high AI (group A) had (independent of age, gender, center effect, heart rate and MBP) higher mortality than the rest of the population (group B). Similar results were found when MBP was replaced by DBP or SBP or PP (these data are not shown). The same result was also observed after using (one step at a time) different models for additional adjustment regarding: mental status, history of stroke and coronary heart disease, CV risk factors (DM, smoking, hypercholesterolemia), nutritional status, cardiac parameters (LV mass, EF, LV diastolic function), drug treatment (data not shown) and carotid atherosclerosis as assessed by the presence of carotid plaques (data not shown).
After adjustment for renal function (creatinine), the statistical significance of the effect of high arterial stiffness and moderate-to-high wave reflections on mortality was marginally lost (P=0.055, model 7, Table 5).
When subjects with diabetes mellitus (n=51) or when subjects under insulin treatment (n=17) were excluded from the analysis, the statistical significance of the effect of high arterial stiffness and moderate-to-high wave reflections on mortality were also marginally lost (data not shown).
Discussion
In the present study, three main findings merit further discussion: (1) the classically observed linear association between PWV and AI was disturbed; (2) the mortality was associated with age, gender, DBP, CV disease, denutrition (low albumin) and renal function, but neither with elevated aortic stiffness (carotid to femoral PWV) nor with pressure wave reflections (AI), when these two parameters were evaluated alone; (3) the combination of high PWV and moderate-to-high AI, but not the opposite (that is, high AI combined with moderate-to-high PWV), was a predictor of mortality independently age, gender and BP. Renal function and insulin resistance seem to modulate the effect of combined effect of PWV and AI on mortality.
The population of the PROTEGER Study has several particularities. It is composed mainly of ‘survivors’ and a high prevalence of overt atherosclerotic disease (almost 62%). Only 80 subjects were younger than 80 years of age and 131 were over 90 years old (mean age 85.4 years (70–103)). Carotid to femoral PWV was consistently augmented, over passing the 20 m sec−1 in almost 10% of the population. However, only 10% of the subjects had seriously impaired left ventricular function (ejection fraction <45%). These major traits of the population may be responsible for a number of CV particularities and results, which must be carefully considered and may limit the extrapolation of our results to other elderly populations.
In accordance with the study of McEniery et al.,9 the present data suggest that aging affects PWV and AI differently. In total, PWV was extremely high (mean PWV 14.4 m s−1), whereas AI was not (mean value 117%). Disassociation between these two hemodynamic factors has been previously described in various populations.10, 11, 12, 13, 14, 15 Several factors (in separate or in combination) such as: aging process, insulin resistance and metabolic disorders, drugs, as well as associated hemodynamic mechanisms: peripheral vasodilation, attenuation of the reflected wave, shift of the effective reflecting distance, impaired left ventricular function,10 might explain this phenomenon. In the present population, the left ventricular function was considerably preserved in both groups (A and B), and cannot be responsible for the outcome. However, it might be explained by peripheral vasodilation, attenuation of the amplitude and later timing of the reflected wave. The proposed mechanisms needs to be further elucidated. Because AI is influenced by both amplitude and timing of the wave reflections, it is difficult to delineate the underlying responsible mechanisms. The application of other types of analysis (for example, wave intensity analysis)16 might improve our ability to address this issue in future studies.
Carotid to femoral PWV is considered as a robust marker of CV risk and all-cause mortality17 and several studies, as well as a recent meta-analysis,18 have proved its ability to predict CV risk in the elderly.3, 4, 5 Accumulating data, but yet less robust, are available regarding the ability of AI to predict mortality;19, 20, 21, 22 in the elderly, such data are lacking. In the present study, mortality was independently associated with age, gender, BP, CV disease and denutrition, but neither with PWV nor with AI, as shown by Kaplan–Meier survival curve analysis. However, those subjects who had combined increased aortic stiffness (third tertile, PWV>15.18 m sec−1) and at the same time moderate-to-high pressure wave reflections (second and third tertiles, AI>112%) (group A) had almost double relative risk of mortality, than the rest of the population (group B). Increased mortality in this group was independent from age, gender, BP, history of CVD, denutrition and carotid/cardiac structure-function. In those subjects who presented a ‘dissociation’ between PWV and AI, that is, extreme values of aortic stiffness (third tertile, PWV>15 m s−1) with low values of pressure wave reflections (first tertile, AI<111%), no marked elevation in mortality was observed. Moreover, subjects with high AI (third tertile, AI>127%) and moderate-to-high PWV (second and third tertiles, PWV>12.49 m sec−1) had not significantly increased mortality compared with the rest of the population.
The data above imply that there is a synergistic effect on survival when both elevated aortic stiffness and pressure wave reflections are present. The combined effect of PWV and AI on mortality was primarily driven by elevated aortic stiffness, rather than elevated AI. Moreover, this combined effect was not clearly observed when subjects with insulin resistance (consisting almost the 20% of the population in both group A and group B) or subjects under insulin treatment were excluded. Within the present study, it is not possible to further examine the potential causality of this phenomenon. We have, however, shown previously that in PROTEGER population there is a ‘reverse metabolic syndrome’,7 as low BP, BMI and high insulin sensitivity predict mortality. A similar modulating effect of the presence of metabolic syndrome on the association between CV risk, PWV and AI has been also previously reported.14 Moreover, the potential role of renal function has to be elucidated further. It is well described that impaired renal function is associated with arterial stiffening and increase wave reflections, and that both PWV and AI are independent predictors of mortality in end-stage renal disease. In our study, renal function (assessed by plasma creatinine): (1) was not significantly different between group A and group B, (2) was linearly associated with PWV (r=0.174, P=0.006), but not with AI and (3) was an independent predictor of mortality. Finally, we have to acknowledge the fact that the present sub-analysis of PROTEGER Study may have low statistical power to provide solid results on CV mortality, as only 27 CV deaths were officially established—however, a similar trend was found in the analysis.
In conclusion, the present study provides further insight on the association between large artery stiffness, pressure wave reflections and mortality in the elderly, implying that a synergistic effect of PWV and AI may exist regarding their effect on survival. Future longitudinal studies need to address the following issues: (1) which factors lead to ‘disassociation’ between aortic stiffness and pressure wave reflections and (2) how this phenomenon might modulate mortality and potentially guide CV risk reduction strategies.
References
Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, Robbins JA, Gardin JM . Risk factors for 5-year mortality in older adults. the cardiovascular health study. JAMA 1998; 279: 585–592.
Weverling-Rijnsburger AWE, Blauw GJ, Lagaay M, Knook DL, Meinders E, Westendorp RGJ . Total cholesterol and risk of mortality in the oldest old. Lancet 1997; 350: 1119–1123.
Meaume S, Benetos A, Henry OF, Rudnichi A, Safar M . Aortic pulse wave velocity predicts cardiovascular mortality in subjects with >70 years of age. Arterioscler Thromb Vasc Biol 2001; 21: 2046–2050.
Sutton-Tyrrell K, Najjar SS, Boudreau RM, Venkitachalam L, Kupelian V, Simonsick EM, Havlick R, Lakatta EG, Spurgeon H, Kritchevsky S, Pahor M, Bauer D, Newman A, for the Health ABC Study. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 2005; 111: 3384–3390.
Mattace_Raso FUS, van der Cammen TJM, Hofman A, vam Popele NM, Bos ML, Schalekamp ADH, Asmar R, Reneman RS, Hoeks APG, Witteman B, Witteman JCM . Arterial stiffness and risk for coronary heart disease and stroke: The Rotterdam Study. Circulation. 2006; 112: 657–662.
Protogerou AD, Safar ME, Iaria P, Safar H, Le Dudal K, Filipovsky J, Henry O, Dumicetière P, Blacher J . Diastolic blood pressure and mortality in the elderly with cardiovascular disease. Hypertension 2007; 50: 172–180.
Vischer UM, Safar ME, Safar H, Iaria P, Le Dudal K, Henry O, Herrman FR, Ducimtier P, Blacher J . Cardiometabolic determinants of mortality in a geriatric population. Is there a ‘reverse metabolic syndrome’? Diabetes Metab 2009; 35: 108–114.
Vlachopoulos C, Aznaouridis K, O′Rourke MF, Safar ME, Baou K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J 2010; 31: 1865–1871.
McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR, ACCT Investigators. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol 2005; 46: 1753–1760.
Vyas M, Izzo JI, Lacourciere Y, Arnold JAO, Dunlap ME, Amato JL, Pfeffer MA, Mitchell GF . Augmentation index and central arterial stiffness in middle-aged to elderly people. Am J Hypertens 2007; 20: 642–647.
Vlachopoulos C, Dima I, Aznaouridis K, Vasiliadou C, Ioakeimidis N, Aggeli C, Toutouza M, Stefanadis C . Acute systemic inflammation increases arterial stiffness and decreases wave reflections in healthy individuals. Circulation 2005; 112: 2193–2200.
Protogerou AD, Safar ME . Dissociation between central augmentation index and carotid - femoral pulse wave velocity: When and Why? Am J Hypertens 2007; 20: 648–649.
Van Bortel LM, Balkestein EJ, van der Heijden-Spek JJ, Vanmolkot FH, Staessen JA, Kragten JA, Vredeveld JW, Safar ME, Struijker Boudier HA, Hoeks AP . Non-invasive assessment of local arterial pulse pressure: comparison of applanation tonometry and echo-tracking. J Hypertens 2001; 19: 1037–1044.
Protogerou AD, Blacher J, Aslangul E, Le Jeunne C, Mavrikakis M, Lekakis J, Safar ME . Gender influence on metabolic syndrome's effects on arterial stiffness and pressure wave reflections in treated hypertensive subjects. Atherosclerosis. 2007; 193: 151–158.
Lacy PS, O'Brien DG, Stanley AG, Dewar MS, Swales PPR, Williams B . Increased pulse wave velocity is not associated with elevated augmentation index in patients with diabetes. J Hypertens 2004; 22: 1937–1944.
Westerhof BE, Guelen I, Westerhof N, Karemaker JM, Avolio A . Quantification of wave reflection in the human aorta from pressure alone: a proof of principle. Hypertension 2006; 48: 595–601.
Laurent S, Cockcroft J, Van Bortel LM, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos Ch, Wilkinson IB, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006; 27: 2588–2605.
Vlachopoulos C, Aznaouridis K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010; 55: 1318–1327.
London GM, Blacher J, Pannier B, Guerin A, Marchais S, Safar M . Arterial wave reflections and survival in end-stage renal failure. Hypertension 2001; 38: 434–438.
Weber T, Auer J, O'Rourke MF, Kvas E, Lassnig E, Lamm G, Stark N, Rammer M, Eber B . Increased arterial wave reflections predict severe cardiovascular events in patients undergoing percutaneous coronary interventions. Eur Heart J 2005; 26: 2657–2663.
Chirinos JA, Zambrano JP, Chakko S, Veerani A, Schob A, Willens HJ, Perez G, Mendez AJ . Aortic pressure augmentation predicts adverse cardiovascular events in patients with established coronary artery disease. Hypertension 2005; 45: 980–985.
Dart AM, Gatzka CD, Kingwell BA, Willson K, Cameron JD, Liang YL, Berry KL, Wing LM, Reid CM, Ryan P, Beilin LJ, Jennings GL, Johnston CI, McNeil JJ, Macdonald GJ, Morgan TO, West MJ . Brachial blood pressure but not carotid arterial waveforms predict cardiovascular events in elderly female hypertensives. Hypertension 2006; 47: 785–790.
Acknowledgements
We are deeply indebted to the PROTEGER patients and their relatives, who made this study possible. Sources of funding: This work was supported by the ‘Société Française d'Hypertension Artérielle’ and the ‘Fondation de France’.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Protogerou, A., Safar, M., Papaioannou, T. et al. The combined effect of aortic stiffness and pressure wave reflections on mortality in the very old with cardiovascular disease: the PROTEGER Study. Hypertens Res 34, 803–808 (2011). https://doi.org/10.1038/hr.2011.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.33
Keywords
This article is cited by
-
Reference values of office central blood pressure, pulse wave velocity, and augmentation index recorded by means of the Mobil‐O‐Graph PWA monitor
Hypertension Research (2020)
-
When the arteries get tough, the tougher do not get going
Hypertension Research (2011)