Abstract
Hypertension is an important modifiable risk factor for cardiovascular (CV) morbidity and mortality, and a highly prevalent condition in both men and women. However, the prevalence of hypertension is predicted to increase more among women than men. Combined oral contraceptives (COCs) can induce hypertension in a small group of women and, increase CV risk especially among those with hypertension. Both COC-related increased CV risk and blood pressure (BP) returns to pretreatment levels by 3 months of its discontinuation. The effects of menopause and hormone replacement therapy (HRT) on BP are controversial, and COCs and HRT containing the new generation progestin drospirenone are preferred in women with established hypertension. Despite the high incidence of cancer in women, CV disease remains the major cause of death in women and comparable benefit of antihypertensive treatment have been demonstrated in both women and men.
Similar content being viewed by others
Introduction
Hypertension is an important modifiable risk factor for cardiovascular (CV) morbidity and mortality, and a highly prevalent condition in both men and women. Blood pressure (BP) is generally higher in men than in women regardless of age. Mean systolic BP in the overall population increases progressively throughout adult life in both men and women. During early adulthood mean systolic BP is higher in men than women, but the subsequent rate of rise in BP is steeper for women than men. Prevalence and severity of hypertension increase markedly with advancing age in women, such that a higher percentage of women than men have high BP after 65 years.1, 2, 3, 4, 5 Furthermore, BP control is more difficult to achieve in older women. Data from the Framingham Heart Study showed gender differences in BP control rates and in the pattern of antihypertensive medications prescribed.3 An age-related decrease in BP control rates were more pronounced in women than in men. Among the oldest participants with hypertension, only 23% of women (vs. 38% of men) were controlled to BP <140/90 mm Hg. Treatment with thiazide diuretics was also more frequent among women than men (38 vs. 23%). It is unknown whether the age-related decline in BP control among women is related to true treatment resistance because of biological factors or to inappropriate drug choices in the clinical setting.
This article discusses practical aspects related to hypertension in women and some topics are discussed in detail in separate articles in this special review edition.
Prevalence of hypertension and menopause effects on BP
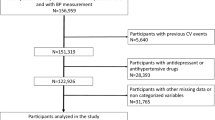
The general prevalence of hypertension is slightly higher among men than women. The National Health and Nutrition Examination Survey (NHANES) data show that more men than women have hypertension until 45 years of age. From 45 to 64 years of age, the percentages of men and women with hypertension are similar and, after that, a higher percentage of women than men have high BP.1 However, it has been predicted that more women than men will have hypertension in the near future.6 The worldwide prevalence of hypertension is predicted to increase by 9% in men and 13% in women between 2000 and 2025. In terms of absolute numbers, 483.5 million women had hypertension in 2000 and this is predicted to increase to 793.3 million in 2025 (Figure 1). Aging of world population by 2025 and longer life expectancies in women than in men are possibly related to the greater increases in the prevalence of hypertension among women.
Number of men and women with hypertension in 2000 and 2025. (Data from Kearney et al.6)
The effect of menopause on BP is controversial and confounded by the effects of aging and clustering of other CV risk factors, such as body weight and lipid levels.7, 8, 9, 10, 11, 12, 13 A European study that utilized 24-h BP monitoring for diagnosis of hypertension showed that, after adjustment for age and body mass index, the prevalence of hypertension in postmenopausal women was more than twice that in premenopausal women. Furthermore, rise in systolic BP tended to be steeper in postmenopausal compared with premenopausal women.9 Cross-sectional studies have generally found significantly higher BP in postmenopausal vs. premenopausal women and prospective studies have reported variable results, including a lack of association between menopause and BP, and even a negative association between BP and years post menopause.7
Changes in BP after menopause seem to be related with alterations in estrogen and progesterone levels. Clinical and experimental studies have showed that estrogen induces vasodilatation, prevents vascular remodeling processes, inhibits vascular response to injury, provides renoprotection and decreases basal sympathetic tone. Similar to estrogen, progesterone induces endothelium-dependent vascular relaxation.14 However, the effects of natural estrogen and progesterone appear to be different from the synthetic preparations.
Oral contraceptives and BP
Combined oral contraceptives (COCs) induce small increases in BP in the entire population of users and has been associated with a small excess risk of CV disease among women, especially in those with hypertension.15 Hypertension is two to three times more common among women taking oral COCs, especially in those obese and at advanced age, than in those not taking these medications.16, 17 Modern preparations that contain lower doses (<30 μg) of estrogen can also lead to development of hypertension and can precipitate accelerated or malignant hypertension. Environmental characteristics, including pre-existing pregnancy-induced hypertension, occult renal disease, obesity, middle age (>35 years) and duration of COC use, as well as genetic characteristics, such as family history of hypertension, increase susceptibility to COC-induced hypertension.17, 18
Controlled prospective studies have consistently demonstrated a return of BP to pretreatment levels within 3 months of discontinuing COCs.16, 19 In the Health Survey for England, a cross-sectional survey, mean BP was significantly higher among premenopausal women who were current users of oral contraceptives (COCs and progestin-only) than among non-users.20 The BP difference tended to increase with age. However, BP tended to be lower among the progestin-only users than among non-users, suggesting that progestin-only contraceptives are a better choice for women with established hypertension.
Drospirenone, which is a new fourth generation progestin with antimineralocorticoid diuretic effects, seems to reduce BP when combined to estrogen. In a randomized study, 80 women received the combination drospirenone 3 mg plus ethinylestradiol 30, 20 or 10 μg or levonorgestrel 150 μg plus ethinylestradiol 30 μg during six cycles.21 Systolic and diastolic BP reduced by 1–4 mm Hg with any of drospirenone combinations and increased by 1–2 mm Hg with levonorgestrel combination. Women treated with drospirenone also presented significantly weight loss from 0.8–1.7 kg. Based on these and other data, progestin-only contraceptives or COCs containing drospirenone are recommended for women with established hypertension.
The Table 1 summarizes contraindications for COCs use based on World Health Organization recommendations.22
Hormone replacement therapy and BP
Conflicting results have been reported by studies that evaluated the effects of hormone replacement therapy (HRT) on BP.23 Differences in patient populations studied, methods of measuring BP, hormone preparations and routes of administration partially explain the discrepancy between the studies.24 Minimal BP effects in normotensive women have been showed in most studies. For example, in the Baltimore Longitudinal Study on Aging, women receiving HRT (oral or transdermal estrogen and progestin) had a significantly smaller (1.6 mm Hg) increase in systolic BP over time than nonusers (8.9 mm Hg) and diastolic BP was not affected by HRT.25 In the Women's Health Initiative's (WHI) cross-sectional analysis, the effect of HRT on BP was evaluated on almost 100 000 women aged 50–79 years.26 Current HRT use was associated with a 25% greater likelihood of having hypertension compared with past use or no prior use of HRT. However, in a placebo-controlled trial of HRT with 16 608 postmenopausal women, the estrogen plus progestin arm was related to a small (∼1 mm Hg) increase is systolic BP compared with placebo.2
Similar to oral contraceptives, HRT containing drospirenone seems to reduce BP due to its antimineralocorticoid receptor effects. The combination of 17-β-estradiol and drospirenone was tested in postmenopausal hypertensive women.27, 28 In a randomized, double-blind, placebo-controlled study, 750 postmenopausal women with stage 1 and 2 hypertension received drospirenone 1 mg, 2 mg or 3 mg in combination with estradiol, or estradiol alone or placebo. Drospirenone 2 mg and 3 mg, but not 1 mg, in combination with estradiol significantly reduced 24 h systolic BP by 6.1 mm Hg and 4.7 mm Hg, respectively.27
Overall, HRT induces, if any, small changes in BP and should not preclude HRT use in either normotensive or hypertensive women. Nevertheless, all hypertensive women treated with HRT should have their BP measured initially and then at 3–6-month intervals depending on the difficulty of control.16
Pregnancy
Hypertensive disorders in pregnancy are a major cause of maternal, fetal, and neonatal morbidity and mortality.29 Patients with chronic hypertension, who are likely to become pregnant, need to be assessed for severity of hypertension, presence of target organ damage, adjustment of medication therapy, lifestyle changes and investigation of potentially reversible causes. The diagnosis and treatment of hypertension in pregnancy can be difficult, and BP management in pregnant women is a matter of debate.30 Preeclampsia usually occurs after 20 weeks of gestation and is likely to be related to impaired placental development in early pregnancy, which causes placental oxidative stress and inflammation. Subsequent release of placental factors including soluble fms-like tyrosine kinase-1, angiotensin II type 1 receptor autoantibody and cytokines into the maternal circulation leads to widespread dysfunction of the maternal vascular endothelium.31 Preeclampsia, which is a pregnancy-specific syndrome of exaggerated vasoconstriction and reduced organ perfusion, must be differentiated from pre-existing chronic hypertension as the former can threaten the lives of both mother and fetus, and requires specialized care.29 Treatment of hypertension during pregnancy, particularly in the second half of gestation, reduces maternal and fetus risk. Furthermore, it has been clearly shown that preeclampsia places women at long-term risk for CV diseases and that careful follow-up and aggressive preventive strategies are recommended.32, 33, 34 For example, a meta-analysis which includes >3 million women and almost 200 00 women with preeclampsia showed that women who had preeclampsia are 2.7 times more likely to develop hypertension, and almost twice more likely to have ischemic heart disease, stroke or venous thromboembolism.34
Secondary hypertension in women
Secondary hypertension is underdiagnosed and its true prevalence is unknown. Some conditions have increased prevalence in women and need to be investigated. For example, fibromuscular dysplasia, a nonatherosclerotic noninflammatory vascular disease that can affect renal arteries and cause renovascular hypertension, primarily affects women aged from age 20 to 60, but can also affects men and children.35 Fibromuscular dysplasia should be investigated with noninvasive tests, such as renal artery duplex ultrasound, computed tomography angiography and magnetic resonance angiography, in young women with cervical bruits or development of hypertension <35 years. Percutaneous balloon angioplasty is the preferred treatment.
Primary aldosteronism (PA), once considered being a rare condition and not worth seeking unless hypokalemia was present, has been demonstrated to be much more prevalent than previously thought and is probably the commonest cause of secondary hypertension.36 Correct diagnosis and treatment of PA can not only lead to cure of hypertension in patients with unilateral forms of PA, but can also prevent and reverse organ deterioration independent of aldosterone effects on BP.37 The prevalence of PA is similar in men and women, but estrogen and progesterone can affect aldosterone and renin levels and, consequently, can interfere with the investigation of PA. Screening with aldosterone–renin ratio can be affected by the phase of menstrual cycle and by different forms of contraception. We have demonstrated that false positive may occur during the luteal phase, especially, if direct renin concentration is used instead of plasma renin activity.38 In a different study, the COCs ethinylestradiol plus drospirenone, but not subdermal etonogestrel, significantly increase the risk of false positives when direct renin concentration was used to measure renin.39 These studies have shown that some oral contraceptives and menstrual phase must be taken into consideration when interpreting results of aldosterone–renin ratio determined by measuring direct renin concentration.
CV risk in women
Although the myth that certain types of cancer, such as breast cancer, are the main cause of death in women still prevails, CV diseases remain the main cause of death in women. In 2007, death rates for CV diseases and cancer among women were 211.6 and 151.3 per 100 000, respectively. One in 4.5 females died of cancer, whereas 1 in 2.9 died of CV diseases.1 In the data from the NHANES 1999–2004 women were at significantly higher CV risk compared with men, with 53% of women and 41% of men with ⩾3 of the six risk factors studied.5
However, hypertension control in women remains poor, especially among elderly women. The NHANES 1999–2004 showed that 50.8% of men and 55.9% of women had uncontrolled hypertension adjusted for age.5 Rates of uncontrolled hypertension were positively related with age with only 29% of hypertensive women aged 70–79 years having clinic BP <140/90 mm Hg compared with 41 and 37% of those 50–59 and 60–69 years of age, respectively (Figure 2).26 An increased prevalence of concomitant CV factors, including central obesity, elevated total cholesterol and low high-density lipoprotein cholesterol levels are likely to contribute to poor BP control in elderly women.5
Blood pressure control rates in women according to age. (Data from Wassertheil-Smoller et al.26)
In the Women's Health Initiative, the prevalence of prehypertension (BP 120–139/80–89 mm Hg) and its association with other CV risk factors, and the risk for incident CV disease events were determined in 60 785 postmenopausal women who were followed for 7.7 years.40 Prehypertension was identified in 39% of women at baseline. Compared with normotensive women, those with prehypertension had 58% increased risk for CV death, 76% increased risk for myocardial infarction, 93% increased risk for stroke, 36% increased risk for hospitalized heart failure and 66% increased risk for any CV event. CV risk for women with established hypertension was even greater (nearly threefold increase for any CV event). Interestingly, the increased CV risk associated with prehypertension was greater than that associated with smoking (34%), reinforcing the need for treatment in the prehypertensive group. Prehypertension was associated with other modifiable risk factors, that is, high total cholesterol and body mass index, emphasizing the importance of global risk factor reduction for prevention of both hypertension and CV disease outcomes.
Outcomes of antihypertensive trials by gender
Major outcome trials of antihypertensive treatment have generally shown comparable benefit in both women and men.41, 42, 43, 44, 45 However, additional analyses and other trials have demonstrated gender differences in both benefit and adverse effects of treatment.46, 47, 48, 49 In the prespecified subgroup analysis of the VALUE (Valsartan Antihypertensive Long-term Use Evaluation) study, women, but not men, assigned to valsartan-based treatment presented a relative increased risk of the primary endpoint of cardiac mortality and morbidity compared with those who received amlodipine-based treatment.47 Furthermore, the trend toward less congestive heart failure with valsartan-based treatment was not statistically significant in women. Although the difference in BP reduction between the women treated with amlodipine and valsartan (2.8 mm Hg vs. 1.8 mm Hg, respectively) was small, it could partially explain the differences in outcomes. Similarly to VALUE, the ALLHAT (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial) showed a slightly greater BP response to amlodipine compared with lisinopril in women, and this finding was associated with a more pronounced reduction in stroke.
In contrast, in the LIFE (Losartan Intervention For Endpoint Reduction) study, a prespecified subgroup analysis of outcomes in 4963 women with hypertension and left ventricular hypertrophy showed significantly greater reductions in primary end point and most secondary endpoints with losartan compared with the atenolol.46 Despite similar BP reduction, fewer events occurred in women than in men.
Gender considerations in the treatment of hypertension
Non-pharmacological interventions such as weight loss, dietary salt reduction, increased physical activity, reduction of alcohol consumption and a diet rich in fruits and vegetables are recommended for both men and women.16, 50 BP reduction achieved with antihypertensive medications is also similar in men and women. However, some special considerations may dictate treatment choices for women.51, 52 In an overview analysis, the Blood Pressure Lowering Treatment Trialists Collaboration reviewed 31 randomized trials that included 87 349 women and 103 268 men. The main objective was to quantify the effects of BP-lowering treatment according to gender and to determine whether there are important differences in the proportional benefits of treatment between women and men.53 Despite baseline BP levels were slightly higher among women than men, there was no evidence that women and men present different levels of protection from total major CV events (stroke, coronary heart disease events, heart failure and other CV death) from BP lowering. Furthermore, the data showed no evidence of an interaction of sex with BP-lowering treatment for the outcomes of coronary heart disease, heart failure, CV death or total mortality. Treatment regimens based on calcium antagonists conferred marginally (P=0.05) greater protection than regimens based on angiotensin-converting enzyme inhibitors in women compared with men. Treatment with beta blockers or diuretics showed similar benefit to other drug classes for either gender. Further analyses showed no difference in treatment effects between women and men categorized by age. A limitation of this analysis was the small number of events in the young-age subgroup.
It is of importance that angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are contraindicated for women who are or intend to become pregnant because of the risk of fetal developmental abnormalities. Diuretics are particularly useful in women, notably elderly women, because their use is associated with decreased risk of stroke and hip fracture. Increasing evidence suggests that antihypertensive drugs have gender-specific adverse effect profiles. In the Treatment of Mild Hypertension Study, 902 women and men received nonpharmacologic treatment plus treatment with a drug chosen at random from each class of antihypertensive agent available. Women reported twice as many adverse effects as men.54 Similarly, women in the LIFE study had more total adverse events but fewer serious drug-related adverse events than men.46
Biochemical responses to drugs appear to be gender dependent. For example, angiotensin-converting enzyme inhibitor–induced cough is two to three times more common in women than in men, and women are more likely to complain of calcium channel blocker-related peripheral edema and minoxidil-induced hirsutism. Furthermore, women are more likely to develop hyponatremia or hypokalemia and men more likely to develop gout in response to diuretic therapy.52 Sexual dysfunction related to antihypertensive therapy, which is more commonly discussed with men than women, seems to be a problem in women as well as in men. This effect is most often associated with centrally acting agents, β-blockers and thiazide diuretics, whereas angiotensin receptor blocker therapy may improve these symptoms.55, 56
Conclusion
Prevalence of hypertension is expected to increase more in women than men. Although the BP effects of menopause or HRT remain controversial, hypertension importantly contributes to CV morbidity and mortality in women. Development of hypertension with COCs can occur and, usually, it resolves with withdrawal of the COC. Renal artery stenosis secondary to fibromuscular dysplasia primarily affects young women and need to be investigated. Antihypertensive treatments have comparable benefits in both women and men, but additional analyses and other trials have demonstrated gender differences in both benefit and adverse effects of treatment.
References
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, Carnethon MR, Dai S, de Simone G, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Greenlund KJ, Hailpern SM, Heit JA, Ho PM, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, McDermott MM, Meigs JB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Rosamond WD, Sorlie PD, Stafford RS, Turan TN, Turner MB, Wong ND, Wylie-Rosett J . Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation 2011; 123: e18–e209.
Wassertheil-Smoller S, Hendrix SL, Limacher M, Heiss G, Kooperberg C, Baird A, Kotchen T, Curb JD, Black H, Rossouw JE, Aragaki A, Safford M, Stein E, Laowattana S, Mysiw WJ . Effect of estrogen plus progestin on stroke in postmenopausal women. The Women's Health Initiative: a randomized trial. JAMA 2003; 289: 2673–2684.
Lloyd-Jones DM, Evans JC, Levy D . Hypertension in adults across the age spectrum: current outcomes and control in the community. JAMA 2005; 294: 466–472.
Westheim A, Klemetsrud T, Tretli S, Stokke HP, Olsen H . Blood pressure levels in treated hypertensive patients in general practice in Norway. Blood Press 2001; 10: 37–42.
Ong KL, Tso AW, Lam KS, Cheung BM . Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension 2008; 51: 1142–1148.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J . Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365: 217–223.
Coylewright M, Reckelhoff JF, Ouyang P . Menopause and hypertension: an age-old debate. Hypertension 2008; 51: 952–959.
Do KA, Green A, Guthrie JR, Dudley EC, Burger HG, Dennerstein L . Longitudinal study of risk factors for coronary heart disease across the menopausal transition. Am J Epidemiol 2000; 151: 584–593.
Staessen J, Bulpitt CJ, Fagard R, Lijnen P, Amery A . The influence of menopause on blood pressure. J Hum Hypertens 1989; 3: 427–433.
Casiglia E, Tikhonoff V, Caffi S, Bascelli A, Schiavon L, Guidotti F, Saugo M, Giacomazzo M, Martini B, Mazza A, D’Este D, Pessina AC . Menopause does not affect blood pressure and risk profile, and menopausal women do not become similar to men. J Hypertens 2008; 26: 1983–1992.
Cifkova R, Pitha J, Lejskova M, Lanska V, Zecova S . Blood pressure around the menopause: a population study. J Hypertens 2008; 26: 1976–1982.
Zanchetti A, Facchetti R, Cesana GC, Modena MG, Pirrelli A, Sega R . Menopause-related blood pressure increase and its relationship to age and body mass index: the SIMONA epidemiological study. J Hypertens 2005; 23: 2269–2276.
Staessen JA, Ginocchio G, Thijs L, Fagard R . Conventional and ambulatory blood pressure and menopause in a prospective population study. J Hum Hypertens 1997; 11: 507–514.
Dubey RK, Oparil S, Imthurn B, Jackson EK . Sex hormones and hypertension. Cardiovasc Res 2002; 53: 688–708.
Curtis KM, Mohllajee AP, Martins SL, Peterson HB . Combined oral contraceptive use among women with hypertension: a systematic review. Contraception 2006; 73: 179–188.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ . Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42: 1206–1252.
Rosenthal T, Oparil S . Oral contraceptives, hormones replacement therapy, and hypertension. In Lip G, Hall J (eds) Comprehensive Hypertension, 1st edn. Elsevier/Mosby: New York 2008.
Chasan-Taber L, Willett WC, Manson JE, Spiegelman D, Hunter DJ, Curhan G, Colditz GA, Stampfer MJ . Prospective study of oral contraceptives and hypertension among women in the United States. Circulation 1996; 94: 483–489.
Weir RJ, Briggs E, Mack A, Naismith L, Taylor L, Wilson E . Blood pressure in women taking oral contraceptives. Br Med J 1974; 1: 533–535.
Dong W, Colhoun HM, Poulter NR . Blood pressure in women using oral contraceptives: results from the Health Survey for England 1994. J Hypertens 1997; 15: 1063–1068.
Oelkers W, Foidart JM, Dombrovicz N, Welter A, Heithecker R . Effects of a new oral contraceptive containing an antimineralocorticoid progestogen, drospirenone, on the renin-aldosterone system, body weight, blood pressure, glucose tolerance, and lipid metabolism. J Clin Endocrinol Metab 1995; 80: 1816–1821.
World Health Organization. Improving Access to Quality Care in Family Planning: Medical Eligibility Criteria for Contraceptive Use. World Health Organization: Geneva, 2004.
Boldo A, White WB . Blood pressure effects of the oral contraceptive and postmenopausal hormone therapies. Endocrinol Metab Clin North Am 2011; 40: 419–432.
Pimenta E, Oparil S . Gender and blood pressure. In Izzo J, Sica D, Black H (eds), Hypertension Primer. The Essentials of High Blood Pressure: Basic Science, Population Science, and Clinical Managemement, 4th edn. LWW: Philadelphia, PA 2008 pp. 269–273.
Scuteri A, Bos AJ, Brant LJ, Talbot L, Lakatta EG, Fleg JL . Hormone replacement therapy and longitudinal changes in blood pressure in postmenopausal women. Ann Intern Med 2001; 135: 229–238.
Wassertheil-Smoller S, Anderson G, Psaty BM, Black HR, Manson J, Wong N, Francis J, Grimm R, Kotchen T, Langer R, Lasser N . Hypertension and its treatment in postmenopausal women: baseline data from the Women's Health Initiative. Hypertension 2000; 36: 780–789.
White WB, Hanes V, Chauhan V, Pitt B . Effects of a new hormone therapy, drospirenone and 17-beta-estradiol, in postmenopausal women with hypertension. Hypertension 2006; 48: 246–253.
White WB, Pitt B, Preston RA, Hanes V . Antihypertensive effects of drospirenone with 17beta-estradiol, a novel hormone treatment in postmenopausal women with stage 1 hypertension. Circulation 2005; 112: 1979–1984.
No authors listed (as given in PubMed) . Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol 2000; 183: S1–S22.
Lindheimer MD, Taler SJ, Cunningham FG . Hypertension in pregnancy. J Am Soc Hypertens 2008; 2: 484–494.
Gilbert JS, Ryan MJ, LaMarca BB, Sedeek M, Murphy SR, Granger JP . Pathophysiology of hypertension during preeclampsia: linking placental ischemia with endothelial dysfunction. Am J Physiol Heart Circ Physiol 2008; 294: H541–H550.
Wilson BJ, Watson MS, Prescott GJ, Sunderland S, Campbell DM, Hannaford P, Smith WC . Hypertensive diseases of pregnancy and risk of hypertension and stroke in later life: results from cohort study. BMJ 2003; 326: 845.
Ray JG, Vermeulen MJ, Schull MJ, Redelmeier DA . Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet 2005; 366: 1797–1803.
Bellamy L, Casas JP, Hingorani AD, Williams DJ . Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 2007; 335: 974.
Olin JW, Sealove BA . Diagnosis, management, and future developments of fibromuscular dysplasia. J Vasc Surg 2011; 53: 826–836.
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, Young Jr WF, Montori VM . Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2008; 93: 3266–3281.
Stowasser M . Update in primary aldosteronism. J Clin Endocrinol Metab 2009; 94: 3623–3630.
Ahmed AH, Gordon RD, Taylor PJ, Ward G, Pimenta E, Stowasser M . Are women more at risk of false-positive primary aldosteronism screening and unnecessary suppression testing than men? J Clin Endocrinol Metab 2010; 96: E340–E346.
Ahmed AH, Gordon RD, Taylor PJ, Ward G, Pimenta E, Stowasser M . Effect of contraceptives on aldosterone/renin ratio may vary according to the components of contraceptive, renin assay method, and possibly route of administration. J Clin Endocrinol Metab 2011; 96: 1797–1804.
Hsia J, Margolis KL, Eaton CB, Wenger NK, Allison M, Wu L, LaCroix AZ, Black HR . Prehypertension and cardiovascular disease risk in the Women's Health Initiative. Circulation 2007; 115: 855–860.
Turnbull F, Woodward M, Anna V . Effectiveness of blood pressure lowering: evidence-based comparisons between men and women. Expert Rev Cardiovasc Ther 2010; 8: 199–209.
Dahlof B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, Fyhrquist F, Ibsen H, Kristiansson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS, Omvik P, Oparil S, Wedel H . Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359: 995–1003.
Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, Hua T, Laragh J, McInnes GT, Mitchell L, Plat F, Schork A, Smith B, Zanchetti A . Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004; 363: 2022–2031.
Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O’Brien E, Ostergren J . Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005; 366: 895–906.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Os I, Franco V, Kjeldsen SE, Manhem K, Devereux RB, Gerdts E, Hille DA, Lyle PA, Okin PM, Dahlof B, Oparil S . Effects of losartan in women with hypertension and left ventricular hypertrophy: results from the Losartan Intervention for Endpoint Reduction in Hypertension Study. Hypertension 2008; 51: 1103–1108.
Zanchetti A, Julius S, Kjeldsen S, McInnes GT, Hua T, Weber M, Laragh JH, Plat F, Battegay E, Calvo-Vargas C, Cieslinski A, Degaute JP, Holwerda NJ, Kobalava J, Pedersen OL, Rudyatmoko FP, Siamopoulos KC, Storset O . Outcomes in subgroups of hypertensive patients treated with regimens based on valsartan and amlodipine: an analysis of findings from the VALUE trial. J Hypertens 2006; 24: 2163–2168.
Wing LM, Reid CM, Ryan P, Beilin LJ, Brown MA, Jennings GL, Johnston CI, McNeil JJ, Macdonald GJ, Marley JE, Morgan TO, West MJ . A comparison of outcomes with angiotensin-converting–enzyme inhibitors and diuretics for hypertension in the elderly. N Engl J Med 2003; 348: 583–592.
Trenkwalder P, Elmfeldt D, Hofman A, Lithell H, Olofsson B, Papademetriou V, Skoog I, Zanchetti A . The Study on COgnition and Prognosis in the Elderly (SCOPE) - major CV events and stroke in subgroups of patients. Blood Press 2005; 14: 31–37.
Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, Ganiats TG, Gomes AS, Gornik HL, Gracia C, Gulati M, Haan CK, Judelson DR, Keenan N, Kelepouris E, Michos ED, Newby LK, Oparil S, Ouyang P, Oz MC, Petitti D, Pinn VW, Redberg RF, Scott R, Sherif K, Smith Jr SC, Sopko G, Steinhorn RH, Stone NJ, Taubert KA, Todd BA, Urbina E, Wenger NK . Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation 2007; 115: 1481–1501.
Neaton JD, Grimm Jr RH, Prineas RJ, Stamler J, Grandits GA, Elmer PJ, Cutler JA, Flack JM, Schoenberger JA, McDonald R et al. Treatment of Mild Hypertension Study. Final results. Treatment of Mild Hypertension Study Research Group. JAMA 1993; 270: 713–724.
August P, Oparil S . Hypertension in women. In: Oparil S, Weber M (eds) Hypertension, a Companion to Brenner & and Rector's The Kidney. WB Saunders: Philadelphia, 1999 pp. 546–551.
Turnbull F, Woodward M, Neal B, Barzi F, Ninomiya T, Chalmers J, Perkovic V, Li N, MacMahon S . Do men and women respond differently to blood pressure-lowering treatment? Results of prospectively designed overviews of randomized trials. Eur Heart J 2008; 29: 2669–2680.
Lewis CE, Grandits A, Flack J, McDonald R, Elmer PJ . Efficacy and tolerance of antihypertensive treatment in men and women with stage 1 diastolic hypertension. Results of the Treatment of Mild Hypertension Study. Arch Intern Med 1996; 156: 377–385.
Os I, Oparil S, Gerdts E, Hoieggen A . Essential hypertension in women. Blood Press 2004; 13: 272–278.
Wassertheil-Smoller S, Blaufox MD, Oberman A, Davis BR, Swencionis C, Knerr MO, Hawkins CM, Langford HG . Effect of antihypertensives on sexual function and quality of life: the TAIM Study. Ann Intern Med 1991; 114: 613–620.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pimenta, E. Hypertension in women. Hypertens Res 35, 148–152 (2012). https://doi.org/10.1038/hr.2011.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.190
Keywords
This article is cited by
-
Perimenopausal syndrome and hypertension during perimenopause in South China: prevalence, relationships and risk factors
BMC Women's Health (2024)
-
Association between past oral contraceptive use and the prevalence of hypertension in postmenopausal women: the fifth (2010–2012) Korea National Health and Nutrition Examination Survey (KNHANES V)
BMC Public Health (2022)
-
The role of sex and gender in hypertension
Journal of Human Hypertension (2022)
-
Profile of Tabriz Older People Health Survey (TOPS-2019): a representative community-based cross-sectional study
Scientific Reports (2022)
-
Hemorrhage in pheochromocytoma surgery: evaluation of preoperative risk factors
Endocrine (2022)