Abstract
Atherothrombosis is the primary pathophysiology that underlies ischemic cerebral infarction. Osteopontin (OPN) is produced in atherosclerotic lesions and is cleaved by activated thrombin. We hypothesized that the rupture or damage of an unstable atherosclerotic plaque increases plasma levels of thrombin-cleaved OPN (trOPN). This study included 90 patients who received carotid angioplasty with stenting (CAS), 23 patients with essential hypertension (EHT) and 10 patients who were treated with carotid endarterectomy (CEA). The CAS patient group included 36 patients that had pre- and post-operative blood tests, diffusion-weighted imaging (DWI) using cerebral MRIs and estimated thrombus debris within the protection device. Immunohistochemistry of CEA specimens revealed that trOPN was detected around intra-plaque vessels. The highest tertile of plasma trOPN levels in CAS patients was higher than trOPN levels in EHT patients. Post-operative trOPN levels were significantly higher in symptomatic compared with asymptomatic patients (P=0.003). New ipsilateral DWI-positive patients revealed higher post-operative trOPN levels (P=0.003) and a higher grade of thrombi (P<0.001) than DWI-negative patients. TrOPN may be a novel biomarker that reflects the atherothrombotic status in ischemic stroke.
Similar content being viewed by others
Introduction
Lesions of the extracranial cerebral arteries, such as artery-to-artery thromboembolism, acute thrombotic occlusion resulting from plaque rupture and reduced cerebral perfusion resulting from critical stenosis or occlusion caused by progressive plaque growth, may cause ischemic stroke and transient cerebrovascular ischemia (TIA).1 However, the thrombotic status of a patient is difficult to detect using a peripheral blood sample alone.
Osteopontin (OPN) is an extracellular matrix protein that is localized around calcified or inflammatory tissue.2 OPN is secreted by many cell types, such as lymphocytes, macrophages, endothelial cells and vascular smooth muscle cells,3 and exacerbates inflammation through the recruitment of monocyte macrophages and the regulation of cytokine production in macrophages, dendritic cells and T-cells.4, 5, 6 Clinically, plasma OPN levels have a positive relationship with carotid atherosclerosis in patients with essential hypertension (EHT) and an absence of cardiovascular disease.7 OPN expression in atherosclerotic plaques correlated with plasma OPN levels, and it was a significant predictor of future cardiovascular events in other vascular locations.8 These data suggest that OPN is a key component in the pathophysiology of atherosclerosis.
OPN contains a thrombin cleavage site. The cleaved fragments maintain OPN adhesive function and expose new active domains that may impart new activities. The SVVYGLR cryptic domain that is exposed after thrombin cleavage induces adhesion and migration through the α4 and α9 integrins in vitro.9 An antibody that neutralizes only the SLAYGLR domain of mouse OPN (homologous to the SVVYGLR of human OPN) greatly reduces the proliferation of synovial cells in a murine model of rheumatoid arthritis, which leads to bone erosion and inflammatory cell infiltration in arthritic joints.9, 10 We hypothesized that the highly thrombotic environment within atherosclerotic plaques in symptomatic stroke/TIA patients are rich in thrombin and thrombin-cleaved OPN (trOPN). TrOPN release following plaque ruptures is potentially detectable in the blood. The distribution of trOPN in atherosclerotic plaques that were removed by carotid endarterectomy was detected using immunohistochemistry to investigate this hypothesis. The plasma trOPN concentration was measured in two patient groups, asymptomatic carotid artery stenosis and symptomatic carotid artery stenosis, before and after carotid angioplasty with stenting (CAS), which mechanically alters plaque conformation. The relationship between plasma trOPN concentration and new ipsilateral cerebral ischemic lesions on diffusion-weighted imaging (DWI) was analyzed using magnetic resonance imaging (MRI).
Methods
Study population
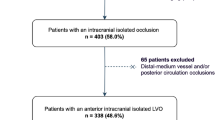
This study was a multicenter trial between Ehime University Hospital, Ehime Prefectural Imabari Hospital, Mazda Hospital (Hiroshima), Asa Citizen Hospital (Hiroshima) and Miyoshi Central Hospital (Hiroshima) from April 2008 to March 2010. The ethics committee of the Ehime University Graduate School of Medicine provided approval for the study. Informed consent was obtained from all participating patients. Patients with moderate- to high-grade carotid artery stenosis with a >70% diameter reduction who were scheduled to have CAS (n=90) or carotid endarterectomy (CEA, patients in Ehime University Hospital) were prospectively included in this study. The study design is outlined in Supplementary Figure 1. The indications for CAS or CEA were determined using CT and/or MR angiographic appearance, color duplex ultrasound, and clinical evaluation, as described previously.11 No patients were diagnosed with acute stroke within 1 month as determined by neurological symptoms. Patients with EHT, no symptomatic cardiovascular events and no antihypertensive medications were also enrolled for comparison (Supplementary Table 1). The systolic blood pressure and diastolic blood pressure were measured in the supine position using a brachial automatic sphygmomanometer in the catheterization laboratory for CAS patients. EHT patients were measured in the seated position in the outpatient clinic. Systolic blood pressure and diastolic blood pressure were averaged using a 3-fold determination. Hypertension was defined as a systolic blood pressure over 140 mm Hg or a diastolic blood pressure over 90 mm Hg. The exclusion criteria were as follows: patients with malignant neoplasm, chronic renal failure on hemodialysis or peritoneal dialysis, autoimmune disease, or chronic inflammatory status. Patients with atrial fibrillation, a known history of cardiac thrombosis or prescribed anticoagulants were also excluded. Furthermore, all patients undergoing CAS in Ehime University Hospital were divided into two groups by pre-operative status—asymptomatic and symptomatic (Table 1). ‘Symptomatic’ was defined as ipsilateral cerebrovascular or ocular ischemic symptoms by a neurosurgeon before the CAS procedure within 180 days of treatment and confirmed by cerebral CT or MRI. Silent ischemic events in symptomatic patients were not included. All procedures were performed in a fasting state. Blood was collected from the peripheral veins of all CAS patients at the catheterization laboratory before the determination of OPN and trOPN levels. The same protocol was performed in all five hospitals. In Ehime University, a blood sample from peripheral veins was collected as soon as possible after the stenting procedure in 36 patients. Blood was collected from EHT patients in the morning in a fasted state after a 20-minute rest in a supine position.
Histological Examination
Plaques were divided into 5-mm-thick segments along the longitudinal axis using a standardized protocol. Segments with the greatest and smallest plaque burdens were subjected to histological examination and classified based on plaque morphology as reported previously.12, 13 Immunohistochemistry was performed on paraffin-embedded sections. Serial sections were stained with primary antibodies against macrophages (CD68, mouse monoclonal, clone PGM1, DAKO, Copenhagen, Denmark), OPN (Rabbit polyclonal, LB-4225, Cosmo Bio, Japan) and trOPN (mouse monoclonal, clone 34E3, IBL, Japan). Staining was visualized using 3,3′-diaminobenzidine tetrachloride (DAB, DAKO). Omission of the primary antibody served as specificity controls.
Carotid artery stenting
All 36 patients received antiplatelet agents. Heparin was administered (5000 IU i.v.) before stent delivery. All patients were treated with distal filter devices with a mesh size of approximately 100 μm (Angioguard Xp; Cordis). Procedures were performed under local anesthesia through percutaneous transfemoral access by three experienced interventional neurosurgeons. Ipsilateral carotid and intracranial angiography was performed to assess technical success. The amount of trapped thrombi/debris in the filters were separated into four grades after the withdrawal of protection devices: Grade 0: none, Grade 1: <20%, Grade 2: 20–50%, Grade 3: over 50%. Samples were further grouped into low grade (Grades 0 and 1) or high grade (Grades 2 and 3) (Supplementary Figure 2).
OPN enzyme-linked immunosorbent assay
Blood samples were centrifuged and stored at −80 °C until measurement. Plasma OPN and trOPN levels were measured using a commercial enzyme-linked immunosorbent assay kit (Immuno Biological Laboratory, Gunma, Japan, code 27156 and 27258, respectively) according to the described procedures. All measurements were performed in duplicate.
Radiological assessment
Carotid stenosis was classified using CT angiography according to consensus criteria.14 DWI was performed within 7 days before and 2 days after the CAS procedure, and assessed by experienced radiologists who were blinded to all of the clinical details.
Statistical analysis
Comparisons of two groups, such as symptomatic or asymptomatic and EHT or CAS patients, were analyzed using the Student's t test, χ2-test, or Mann–Whitney U test. The relationship between OPN, trOPN and other parameters in CAS patients were analyzed using the Pearson’s correlation test or Spearman’s rank-order test. The paired t test and Wilcoxon test analyzed changes in OPN and trOPN levels, respectively. A P value of <0.05 was considered statistically significant.
Results
The presence of trOPN in atherosclerotic plaques was examined using Haematoxylin and Eosin (HE) stain and immunohistochemistry (IHC). OPN (Figures 1e, k and n) co-localized with CD68-positive cells, alpha smooth muscle actin (αSMA)-positive cells, lipid core and calcified nodules in a plaque that contained intraplaque hemorrhage, intraplaque vessels and a ‘thin fibrous cap’, as determined previously.15 TrOPN was detected in intraplaque hemorrhages and partially co-localized with perivascular CD68-positive cells (Figures 1l and o). αSMA-positive cells in lesions with diffuse intimal thickening were OPN-positive, but trOPN was not detected (Figure 1f). OPN and trOPN was also detected in the debris on protection filters (Supplementary Figure 3).
Representative immunohistochemistry of CEA specimens. (a, g); HE stain, (b, h, m); CD68, (c, i); αSMA, (d, j); CD34, (e, k, n); OPN, (f, l, o); trOPN. (a); Pathological intimal thickening. (g); Plaque with intraplaque hemorrhage; boxes i and ii are enlarged in (h-l) and (m-o), respectively. *OPN and trOPN within the extracellular matrix.
EHT patients were compared with CAS patients to clarify the profile of OPN and trOPN levels (Supplementary Table 1). The CAS patients were older and more commonly male, with a higher prevalence of current smokers, lower body mass index, lower diastolic blood pressure, lower HDL-cholesterol, higher creatinine, higher HbA1c and higher triglycerides than EHT patients. Plasma OPN levels were divided into tertiles (low, middle and high). TrOPN levels were not normally distributed, and the majority of trOPN levels were lower than the detection limit (n=62, 54.8%). The data were divided into three groups: beneath the detection limit, low trOPN and high trOPN levels. A small but significant difference between CAS and EHT patients was observed in the high OPN group (934±287 ng ml–1 vs. 762±151 ng ml–1, respectively, P=0.032). Importantly, trOPN levels in the high CAS group were significantly higher than trOPN levels in the high EHT group (median 8.1 pmol l–1, range 5.1–14.0, median 2.8 pmol l–1, range 2.54–3.81, respectively, P<0.001) (Figure 2). The relationship between OPN, trOPN and other clinical parameters in CAS patients was analyzed (Supplementary Tables 2 and 3). Diabetes patients and bilateral carotid stenosis patients demonstrated higher OPN levels than the other patients (P=0.015, P=0.015, respectively). HDL-C was negatively correlated with trOPN, but creatinine and OPN were positively correlated with trOPN (ρ=−0.235, P=0.037, ρ=0.260, P=0.016, ρ=0.359, P=0.001, respectively).
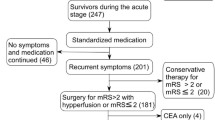
Preoperative OPN and trOPN levels were compared in symptomatic (n=14) and symptomatic (n=22) CAS patients (Table 1). The ratios of angiotensin I receptor blockers (ARB) use and BMI were lower in the symptomatic group. The mean duration of pre- and post-blood sampling was 2.7±1.2 h. No differences in baseline OPN or trOPN levels between the two groups were observed (Figures 3a and b). Plasma OPN levels were elevated significantly in all patients after carotid artery stenting (asymptomatic, 502±233 ng ml–1 to 773±304 ng ml–1, P<0.001; symptomatic, 599±301 ng ml–1 to 908±383 ng ml–1, P<0.001, Figure 3a), but no difference in OPN increase was observed between the two groups (asymptomatic, 271±149 ng ml–1; symptomatic 181±38 ng ml–1, P=0.519). In contrast, plasma trOPN increased significantly in the symptomatic group post-procedure (median 0 to 2.0 pmol l–1, P<0.001, Figure 3b), but no significant increase in the asymptomatic group was observed.
Post-operative DWI was analyzed to detect new ipsilateral cerebral ischemic lesions. A greater number of DWI-positive patients (n=21) were pre-operative symptomatic patients who demonstrated a higher grade of debris in the filter device and higher post-operative trOPN concentrations than DWI-negative patients (P=0.005, P<0.001, and P=0.003, respectively) (Table 2).
Discussion
This study revealed the presence of trOPN in atherosclerotic plaques and demonstrated that plasma trOPN levels increased significantly after CAS in symptomatic stroke/TIA patients. Furthermore, patients with new ischemic cerebral lesions, as estimated by DWI, showed higher post-operative trOPN levels than patients with no new lesions. These findings support the presence of trOPN in highly thrombotic plaques and the use of trOPN as a plaque-derived biomarker for thromboembolic status.
TrOPN was identified in atherosclerotic plaques, especially hemorrhagic areas, using immunohistochemistry and colocalized with CD68-positive cells in intraplaque neovascularity. This report is the first to clarify the localization of trOPN in human atherosclerotic plaques. In our study, OPN was observed in macrophages, αSMA-positive cells, endothelial cells, lipid core and calcified nodules, as reported previously.3 However, the distribution of trOPN was distinct. TrOPN was not observed in macrophage-rich areas in the absence of intraplaque vessels, which suggests a close relationship between trOPN and intraplaque hemorrhage and vessels.
TrOPN levels in CAS patients were significantly higher in the high trOPN group than trOPN levels in EHT patients (Figure 2). Because atherosclerosis is a systemic disease, extracranial carotid atherosclerosis frequently correlates with disease in other arteries, notably the aorta, coronary arteries and peripheral arteries.16, 17 This difference in OPN levels may reflect these situations in the two groups. Counter to our expectations, plasma OPN levels were only marginally higher in the CAS group compared with the EHT group. One reason for this difference could be the use of medication, because both atorvastatin and ARB decrease plasma OPN levels.18, 19 The difference in the relationships between OPN or trOPN and other clinical backgrounds (Supplementary Tables 2 and 3) suggests that different mechanisms regulate plasma OPN and trOPN levels.
The significant post-procedural increase in plasma trOPN levels in symptomatic patients was probably due to the protrusion of plaque contents that contained high levels of trOPN. Cholesterol crystals were evident in the filter protection devices, which supports the hypothesis that the disruption of plaques during the procedure releases plaque content into the circulation. The debris content in symptomatic patients was potentially different from asymptomatic patients. Alternatively, aortic plaques may be the source of trOPN-containing plaque contents. Rosenkranz et al. reported that embolus signals, which were estimated using transcranial Doppler, were detected during the CAS procedure before the involvement of the target lesion.17 This result suggests that the aortic arch and the proximal supra-aortic arteries may detach debris fragments or platelet aggregates from the endothelium or atherosclerotic plaques. Symptomatic stroke patients have complex plaques in the proximal descending aorta, and these plaques constitute an underestimated embolic cause of stroke.20 In support of these reports, symptomatic patients in our study demonstrated a higher thrombotic/embolic status than asymptomatic patients. Although blood pressure did not differ between the two groups, ARB use was lower in symptomatic patients than asymptomatic patients. Imanishi et al. reported that the combined treatment with an HMG-CoA reductase inhibitor and an ARB reduces atherosclerotic plaque formation and increases nitric oxide production.21 The clinical use of ARB decreases future cardiovascular events.22 These additive protective effects of ARB on endothelial function might occur in asymptomatic patients and stabilize the plaque to improve post-procedural trOPN levels.
In contrast, the increase in plasma OPN levels was similar in symptomatic and asymptomatic patients, and the increase in OPN was not correlated with trOPN levels. Different mechanisms may contribute to changes in OPN and trOPN levels. Heparin was injected before the CAS procedure in all patients. Heparin is an anticoagulant that inhibits the activation of thrombin. Heparin inhibits thrombin cleavage of OPN in vitro.23 In our study, heparin might have suppressed plasma OPN cleavage by thrombin, which may explain why the increase in OPN levels did not correlate with post-procedural trOPN levels. Endothelial cells also produce OPN,3 and the stress of the catheter and contrast medium could have induced OPN secretion from endothelial cells. Other inflammatory cytokines, such as interleukin-6, matrix metalloproteinases 3 and 9, high-sensitivity CRP and tumor necrosis factor, were also measured as reported previously.24 No immediate post-procedural alterations in these cytokines were observed, but an increase in cytokines was observed the following day (n=10, data not shown). DWI-MRI monitored post-procedural outcomes. The majority of post-stent DWI-positive patients had high-grade debris in the protection filter (n=18, 85.7%), and their post-stent trOPN levels were higher than DWI-negative patients. These results support our hypothesis of a close relationship between trOPN levels and thrombotic status. Pretreatment trOPN levels were not significantly different between DWI-negative and DWI-positive groups. A lack of statistical power may explain this result because trOPN levels were undetectable in 24 patients. This result may also be due to the selection of CAS or CEA. Surgeons selected CEA for plaques with a large thrombus burden, ulceration and frequent ischemic attacks, which were estimated by ultrasound or MRI.11 One emergent coronary artery bypass graft was performed 6 months after CAS, and one patient had a new bilateral DWI lesion after CAS in the group of patients with high trOPN levels (>2.8 pmol l–1, n=5, Supplementary Table 3) bfore surgery. Although the current study was relatively small, the results suggest that high trOPN levels before CAS reflect a systemically unstable situation.
This study suffers from some limitations. First, EHT patients with no symptomatic disease were compared with CAS patients, but a clarification of trOPN levels that constitute abnormal levels could not be established. Second, although thrombus was estimated, other coagulation factors were not measured. Third, imaging assessments before the treatment were not uniform, and precise data of the severity of carotid stenosis were not obtained. Therefore, the relationship between plaque volumes and plasma OPN or trOPN levels was difficult to assess. Fourth, the number of participants was small, which weakened the statistical power. Further studies that include a larger population are required.
The function of trOPN in human atherosclerotic plaques is not clear. However, trOPN colocalized with CD68-positive macrophages in our study. Yamamoto et al. reported that splenic monocytes from arthritic mice exhibited a significant capacity for cellular migration toward trOPN but not toward full-length OPN.25 A specific murine monoclonal antibody to a cryptic epitope of human OPN ameliorated established collagen-induced arthritis in cynomolgus monkeys,25 which suggests that trOPN is an important accelerator of inflammation in humans. Further experimental studies and prospective clinical studies are required to investigate these possibilities.
Conclusion
There was a significant increase in TrOPN levels after carotid artery stenting in patients with pre-operative symptoms. TrOPN may be a novel index of cardiovascular diseases as a biomarker for both atherosclerotic and thrombotic status.
References
Warlow C, Sudlow C, Dennis M, Wardlaw J, Sandercock P . Stroke. The Lancet 2003; 362: 1211–1224.
Marta Scatena LL, Cecilia M . Giachelli Osteopontin: a multifunctional molecule regulating chronic inflammation and vascular disease. Arterioscler Thromb Vasc Biol 2007; 27: 2302–2309.
O’Brien ER, Garvin MR, Stewart DK, Hinohara T, Simpson JB, Schwartz SM, Giachelli CM . Osteopontin is synthesized by macrophage, smooth muscle, and endothelial cells in primary and restenotic human coronary atherosclerotic plaques. Arterioscler Thromb 1994; 14: 1648–1656.
Liaw L, Almeida M, Hart CE, Schwartz SM, Giachelli CM . Osteopontin promotes vascular cell adhesion and spreading and is chemotactic for smooth muscle cells in vitro. Circ Res 1994; 74: 214–224.
Liaw L, Skinner MP, Raines EW, Ross R, Cheresh DA, Schwartz SM, Giachelli CM . The adhesive and migratory effects of osteopontin are mediated via distinct cell surface integrins. Role of alpha v beta 3 in smooth muscle cell migration to osteopontin in vitro. J Clin Invest 1995; 95: 713–724.
Weintraub AS, Giachelli CM, Krauss RS, Almeida M, Taubman MB . Autocrine secretion of osteopontin by vascular smooth muscle cells regulates their adhesion to collagen gels. Am J Pathol 1996; 149: 259–272.
Kurata M, Okura T, Watanabe S, Fukuoka T, Higaki J . Osteopontin and carotid atherosclerosis in patients with essential hypertension. Clin Sci (Lond) 2006; 111: 319–324.
de Kleijn DPV, Moll FL, Hellings WE, Ozsarlak-Sozer G, de Bruin P, Doevendans PA, Vink A, Catanzariti LM, Schoneveld AH, Algra A, Daemen MJ, Biessen EA, de Jager W, Zhang H, de Vries J-P, Falk E, Lim SK, van der Spek PJ, Sze SK, Pasterkamp G . Local atherosclerotic plaques are a source of prognostic biomarkers for adverse cardiovascular events. Arterioscler Thromb Vasc Biol 2010; 30: 612–619.
Smith LL, Cheung H-K, Ling LE, Chen J, Sheppard D, Pytela R, Giachelli CM . Osteopontin n-terminal domain contains a cryptic adhesive sequence recognized by alpha9beta1 integrin. J Biol Chem 1996; 271: 28485–28491.
Yamamoto N, Sakai F, Kon S, Morimoto J, Kimura C, Yamazaki H, Okazaki I, Seki N, Fujii T, Uede T . Essential role of the cryptic epitope slayglr within osteopontin in a murine model of rheumatoid arthritis. J Clin Invest 2003; 112: 181–188.
Roubin GS, Iyer S, Halkin A, Vitek J, Brennan C . Realizing the potential of carotid artery stenting: proposed paradigms for patient selection and procedural technique. Circulation 2006; 113: 2021–2030.
Hellings WE, Peeters W, Moll FL, Piers SRD, van Setten J, Van der Spek PJ, de Vries J-PPM, Seldenrijk KA, De Bruin PC, Vink A, Velema E, de Kleijn DPV, Pasterkamp G . Composition of carotid atherosclerotic plaque is associated with cardiovascular outcome: a prognostic study. Circulation 2010; 121: 1941–1950.
Sluimer JC, Kolodgie FD, Bijnens APJJ, Maxfield K, Pacheco E, Kutys B, Duimel H, Frederik PM, van Hinsbergh VWM, Virmani R, Daemen MJAP . Thin-walled microvessels in human coronary atherosclerotic plaques show incomplete endothelial junctions: Relevance of compromised structural integrity for intraplaque microvascular leakage. J Am Coll Cardiol 2009; 53: 1517–1527.
Anderson GB, Ashforth R, Steinke DE, Ferdinandy R, Findlay JM . Ct angiography for the detection and characterization of carotid artery bifurcation disease. Stroke 2000; 31: 2168–2174.
Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM . Lessons from sudden coronary death : A comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 2000; 20: 1262–1275.
Craven TE, Ryu JE, Espeland MA, Kahl FR, McKinney WM, Toole JF, McMahan MR, Thompson CJ, Heiss G, Crouse III JR . Evaluation of the associations between carotid artery atherosclerosis and coronary artery stenosis. a case-control study. Circulation 1990; 82: 1230–1242.
Alexandrova NA, Gibson WC, Norris JW, Maggisano R . Carotid artery stenosis in peripheral vascular disease. J Vasc Surg 1996; 23: 645–649.
Tanaka N, Momiyama Y, Ohmori R, Yonemura A, Ayaori M, Ogura M, Sawada S, Kusuhara M, Nakamura H, Ohsuzu F . Effect of atorvastatin on plasma osteopontin levels in patients with hypercholesterolemia. Arterioscler Thromb Vasc Biol 2006; 26: e129–e130.
Kurata M, Okura T, Irita J, Enomoto D, Nagao T, Jotoku M, Miyoshi K, Desilva VR, Higaki J . Angiotensin ii receptor blockade with valsartan decreases plasma osteopontin levels in patients with essential hypertension. J Hum Hypertens 2010; 25: 334–339.
Harloff A, Simon J, Brendecke S, Assefa D, Helbing T, Frydrychowicz A, Weber J, Olschewski M, Strecker C, Hennig J, Weiller C, Markl M . Complex plaques in the proximal descending aorta: An underestimated embolic source of stroke * Supplementary data - video. Stroke 2010; 41: 1145–1150.
Imanishi T, Ikejima H, Tsujioka A, Kuroi A, Kobayashi K, Shiomi M, Muragaki Y, Mochizuki S, Goto M, Yoshida K, Akasaka T . Combined effects of an 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor and angiotensin ii receptor antagonist on nitric oxide bioavailability and atherosclerotic change in myocardial infarction-prone watanabe heritable hyperlipidemic rabbits. Hypertens Res 2008; 31: 1199–1208.
Mochizuki S, Dahl?f Br, Shimizu M, Ikewaki K, Yoshikawa M, Taniguchi I, Ohta M, Yamada T, Ogawa K, Kanae K, Kawai M, Seki S, Okazaki F, Taniguchi M, Yoshida S, Tajima N . Valsartan in a japanese population with hypertension and other cardiovascular disease (jikei heart study): A randomised, open-label, blinded endpoint morbidity-mortality study. The Lancet 2007; 369: 1431–1439.
Myles T, Leung LLK . Thrombin hydrolysis of human osteopontin is dependent on thrombin anion-binding exosites. J Biol Chem 2008; 283: 17789–17796.
Whiteley W, Jackson C, Lewis S, Lowe G, Rumley A, Sandercock P, Wardlaw J, Dennis M, Sudlow C . Association of circulating inflammatory markers with recurrent vascular events after stroke: a prospective cohort study. Stroke 2011; 42: 10–16.
Yamamoto N, Nakashima T, Torikai M, Naruse T, Morimoto J, Kon S, Sakai F, Uede T . Successful treatment of collagen-induced arthritis in non-human primates by chimeric anti-osteopontin antibody. Int Immunopharmacol 2007; 7: 1460–1470.
Acknowledgements
We thank M Fujita, S Matsumoto, D Oshita and M Teraoka for their contribution to patient clinical information, N Arita for specimen preparation, and M Koresawa, S Yamane for the ELISA assay. This work was supported by a Kakenhi grant, Grant-in-Aid for Young Scientists (B) (22790382), from The Ministry of Education, Culture, Sports, Science and Technology (MEXT), Japan Society for the Promotion of Science (JSPS).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Kurata, M., Okura, T., Kumon, Y. et al. Plasma thrombin-cleaved osteopontin elevation after carotid artery stenting in symptomatic ischemic stroke patients. Hypertens Res 35, 207–212 (2012). https://doi.org/10.1038/hr.2011.177
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.177
Keywords
This article is cited by
-
Plasma thrombin-cleaved osteopontin as a potential biomarker of acute atherothrombotic ischemic stroke
Hypertension Research (2017)
-
Structural and biochemical characteristics of arterial stiffness in patients with atherosclerosis and in healthy subjects
Hypertension Research (2012)