Abstract
Nicotinamide and catecholamines are both degraded by S-adenosylmethionine-dependent methylation. Whether excess nicotinamide affects the degradation of catecholamines is unknown. The aim of this study was to investigate the effect of nicotinamide on the methylation status of the body and methylation-mediated catecholamine degradation in both normotensives and hypertensives. The study was conducted in 19 normotensives and 27 hypertensives, using a nicotinamide-loading test (100 mg orally). Plasma nicotinamide, N1-methylnicotinamide, homocysteine (Hcy), betaine, norepinephrine, epinephrine, normetanephrine and metanephrine levels before and 5 h after nicotinamide loading were measured. Compared with normotensives, hypertensives had higher baseline (fasting) levels of plasma nicotinamide, Hcy and norepinephrine, but lower levels of plasma normetanephrine, a methylated norepinephrine derivative. Nicotinamide loading induced a significant increase in the levels of plasma N1-methylnicotinamide and norepinephrine, and a significant decrease in the levels of O-methylated epinephrine (metanephrine) and betaine, a major methyl donor, in both hypertensives and normotensives. Moreover, nicotinamide-loading significantly increased plasma Hcy levels, but decreased plasma normetanephrine levels in normotensives. The baseline levels of plasma epinephrine in hypertensives were similar to those of normotensives, but the post-nicotinamide-loading levels of plasma epinephrine in hypertensives were higher than those of normotensives. This study demonstrated that excess nicotinamide might deplete the labile methyl pool, increase Hcy generation and inhibit catecholamine degradation. It also revealed that hypertensives had an abnormal methylation pattern, characterized by elevated fasting plasma levels of unmethylated substrates, nicotinamide, Hcy and norepinephrine. Therefore, it seems likely that high nicotinamide intake may be involved in the pathogenesis of Hcy-related cardiovascular disease.
Similar content being viewed by others
Introduction
Niacin (vitamin B3, i.e. nicotinamide and its precursor nicotinic acid) is essential for the synthesis of nicotinamide adenine dinucleotide and nicotinamide adenine dinucleotide phosphate, coenzymes important in energy metabolism and redox reactions. Therefore, changes in niacin status have profound effects on the body.1 Excess niacin is known to be degraded mainly by homocysteine (Hcy)-producing methylation, which is catalyzed by S-adenosylmethionine (SAM)-dependent nicotinamide N-methyltransferase (NNMT; Figure 1).2 Thus, high niacin intake may lead to a depletion of labile methyl groups and an elevation of plasma Hcy,3 a phenomenon termed hyperhomocysteinemia, which is often seen in patients with cardiovascular disease (CVD).4
The linkage between nicotinamide degradation and catecholamine inactivation by the methionine cycle. The methylation of nicotinamide, norepinephrine and epinephrine is all S-adenosylmethionine (SAM)-dependent reactions, in which homocysteine is generated. The resultant homocysteine may be either remethylated back to methionine via betaine- or folate-dependent pathway, or converted to cystathionine (CTH). (1a), nicotinamide-N-methyltransferase; (1b), catechol-O-methyltransferase; (1c), phenylethanolamine N-methyltransferase; (2), S-adenosylhomocysteine hydrolase; (3), betaine-homocysteine-methyltransferase; (4), methionine synthase; (5), S-adenosylmethionine synthetase. SAH, S-adenosylhomocysteine; DMG, dimethylglycine; THF, tetrahydrofolate.
Catecholamines, primarily norepinephrine and epinephrine, mediate the cardiovascular effects of the sympathetic nervous system.5 CVD is frequently associated with increased circulating levels of catecholamines,6 which is generally attributed to sympathetic overactivity. However, although a decrease in the degradation of catecholamines is expected to contribute to the elevated circulating catecholamines, whether there are changes in the degradation (i.e. inactivation) of catecholamines, in CVD is unknown. Based on evidence that the inactivation of catecholamines is also mediated via SAM-dependent methylation (Figure 1),7 which may be influenced by niacin due to a competition for labile methyl groups, we postulated that high niacin intake may contribute to increased circulating levels of catecholamines and subsequent development of CVD. To test this hypothesis, we investigated the effect of nicotinamide loading on the body’s methylation status and methylation-mediated catecholamine degradation in both normotensives and hypertensives.
Methods
Participants
The study was approved by the local Ethics Committee. All the participants gave their written informed consent. Hypertension was defined as a systolic blood pressure ⩾140 mm Hg and/or a diastolic blood pressure ⩾90 mm Hg on three separate occasions. The participants’ sitting blood pressure was measured three times using a standard sphygmomanometer after 15 min of rest on each occasion. Twenty-seven hypertensives (including 21 untreated hypertensives) without definable cause (that is, essential hypertension), diabetes, renal dysfunction or cerebral ischemic disease and 19 age- and sex-matched healthy normotensives with a blood pressure of ⩽135/85 mm Hg participated in this study (see Supplementary Information for detailed characteristics of the participants). None of the participants received any dietary intervention before the study. The hypertensive participants who had taken antihypertensive medication discontinued use of the medication for at least 2 weeks before the onset of the study. All participants refrained from smoking, drinking alcohol and consuming caffeinated products for at least 3 days before the study.
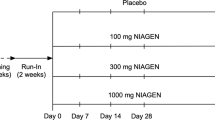
Study protocol
After an overnight fast, all participants rested quietly in bed throughout the test. Antecubital venous blood was collected into vacuum tubes containing one-tenth volume of 0.129 mol l−1 sodium citrate at 0630–0700 h Each participant was then orally administered 100-mg nicotinamide. A second venous blood sample was collected from each participant at 5-h post-nicotinamide loading. The plasma was separated from the blood samples by centrifugation at 1500 g for 10 min. Aliquots of plasma sample were placed directly in liquid nitrogen and then transferred to −80 °C for subsequent analyses. The plasma samples were analyzed in double-blind fashion.
Determination of nicotinamide, N1-methylnicotinamide, Hcy and betaine
High-performance liquid chromatography (HPLC) was used to measure plasma nicotinamide, N1-methylnicotinamide, Hcy and betaine levels. The HPLC system consisted of an LC-9A pump (Shimadzu, Kyoto, Japan), a Rheodyne 7725i sample injector with a 20-μl sample loop (Rheodyne LLC, Rohnert Park, CA, USA), a Hypersil ODS C18 column (Thermo, Bellefonte, PA, USA) with a Waters 470 fluorescence detector (Waters, Milford, MA, USA) for the analysis of plasma nicotinamide, N1-methylnicotinamide and Hcy, and a Supelcosil LC-SCX column (Supelco, Bellefonte, PA, USA) with a UV3000 detector (Thermo Separations Products, Fremont, CA, USA) for the detection of betaine. All chromatography was performed at room temperature. Nicotinamide and N1-methylnicotinamide were analyzed as previously described.8
HPLC analysis of plasma Hcy was performed according to Pfeiffer et al.9 A mixture of 50 μl of plasma, 25 μl of internal standard (10 μmol l−1 cystamine) and 25 μl of phosphate-buffered saline (pH 7.4) was incubated with 10 μl of 100 g l−1 tris (2-carboxyethyl) phosphine hydrochloride for 30 min at room temperature, to reduce and release protein-bound thiols, after which 90 μl of 100 g l−1 trichloroacetic acid containing 1 mmol l−1 EDTA was added for deproteinization. Then, after centrifugation (13 000 g for 10 min), 50 μl of the supernatant was transferred to another Eppendorf tube, containing 10 μl of 1.55 mol l−1 NaOH, 125 μl of 0.125 mol l−1 borate buffer containing 4 mmol l−1 EDTA (pH9.5) and 25 μl of 1 g l−1 4-fluoro-7-sulfobenzofurazan ammonium salt in the borate buffer. The sample was then incubated at 60 °C for 60 min, and then 15 μl of 85% H3PO4 was added. An aliquot of 20 μl was injected directly into the HPLC system for analysis. Hcy was quantified using fluorescence detection at 385 nm excitation wavelength and 515 nm emission wavelength, using 0.1 mol l−1 acetic acid–acetate buffer, pH4.62, containing 30 ml l−1 methanol as mobile phase at a flow rate of 0.8 ml min−1. Hcy standard solution was added to pooled plasma to obtain the desired final concentrations (0, 2, 4, 6, 8, 10, 12, 16 and 20 μmol l−1) for calibration.
HPLC determination of plasma betaine was performed using the method of Laryea et al.10 Briefly, the derivatizing solution was made by dissolving 66 mg (2.5 mmol) of 18-crown-6 and 1390 mg (50 mmol) of 4-bromophenacyl bromide in 100 ml of acetonitrile. Plasma sample or calibrator solution (50 μl) was added to 50 μl of 100-mmol l−1 KH2PO4. After the solution was vortex-mixed, 900 μl of derivatizing solution was added, and mixed again. The tubes were capped, vortex-mixed and heated to 80 °C for 60 min. After being cooled to room temperature, the mixture was vortexed, followed by centrifugation at 1000 g for 5 min. Then, 100 μl of the supernatant was taken and diluted up to 10-fold with chromatography grade acetonitrile. The derivatized sample (20 μl) was injected directly into the HPLC. The UV detector was set at 254 nm. The mobile phase contained 22-mmol l−1 choline in 900-ml l−1 acetonitrile and 100 ml l−1 distilled water, and was degassed in an ultrasonic bath before use. The flow rate was 1.2 ml min−1. The linearity of the method was determined by assaying betaine standards, ranging in concentration from 0 to 200 μmol l−1.
Assays of norepinephrine, epinephrine, normetanephrine and metanephrine
Plasma concentrations of norepinephrine and epinephrine were measured using 2-Cat ELISA (norepinephrine/epinephrine) kits (Labor Diagnostika Nord, Nordhorn, Germany) following instructions from the manufacturer. Plasma levels of normetanephrine and metanephrine were determined using a MetCombi (methanephrine/normetanephrine) elisa kit (DRG International, Inc, Mountainside, NJ, USA) according to instructions provided by the manufacturer. The absorbance of each plate was measured at 450 nm using a Bio-Rad model 550-microplate reader (Bio-Rad Co, Hercules, CA, USA).
Reagents and solvents
Nicotinamide, Hcy, betaine, cystamine dihydrochloride, tris (2-carboxyethyl) phosphine hydrochloride, 4-fluoro-7-sulfobenzofurazan ammonium salt and 18-crown-6,4-bromophenacyl bromide were purchased from Sigma (St Louis, MO, USA). N1-methylnicotinamide was purchased from Takeda Chemical Industries (Osaka, Japan). Nicotinamide tablets (50 mg per tablet) were purchased from Lisheng Pharma (Tianjin, China).
Statistical analysis
The data are presented as means±s.e.m. Statistical differences in the data were evaluated by paired or unpaired Student's t-test, and were considered significant at P<0.05.
Results
Patterns of nicotinamide metabolism in normotensives and hypertensives
Nicotinamide is known to rapidly reach peak plasma concentrations after oral administration, and excess nicotinamide is degraded to N1-methylnicotinamide.1, 11 The present results showed that the plasma nicotinamide levels had virtually returned to baseline (fasting) 5 h after an oral 100-mg nicotinamide load in both normotensives and hypertensives (Figure 2a), whereas N1-methylnicotinamide remained at very high levels (about six times higher than the baseline values in both groups; Figure 2b). The mean plasma N1-methylnicotinamide levels either before or 5 h after nicotinamide loading in hypertensives were slightly higher than that of normotensives (143.1±9.8 vs. 133.2±11.6 nmol l−1 at baseline conditions and 787.3±49.2 vs. 712.0±46.9 nmol l−1 after nicotinamide loading), although the differences between the two groups were not statistically significant (Figure 2b). However, both the baseline and post-nicotinamide-loading plasma nicotinamide levels in hypertensives were significantly higher than those of normotensives (Figure 2a).
Nicotinamide loading-induced changes in plasma nicotinamide and N1-methylnicotinamide levels in normotensives and hypertensives. (a and b) show the fasting (baseline) and 5-h post-nicotinamide load plasma nicotinamide and N1-methylnicotinamide levels, respectively. ##P<0.01 vs. baseline (paired Student's t-test); *P<0.05 and **P<0.01 vs. normotensives (unpaired Student's t-test).
Effects of nicotinamide loading on plasma Hcy and betaine in normotensives and hypertensives
The baseline plasma Hcy levels in hypertensives were significantly higher than those of normotensives (Figure 3a). The plasma Hcy levels were increased in both normotensives and hypertensives 5 h after nicotinamide loading (P<0.05 and P=0.14, respectively; Figure 3a). The baseline levels of plasma betaine, a major labile methyl donor,12 were slightly lower in hypertensives than in normotensives, but there was no statistically significant difference. In parallel with the observed increase in plasma N1-methylnicotinamide, plasma betaine levels in both hypertensives and normotensives were significantly decreased after nicotinamide loading (Figure 3b).
Effects of nicotinamide on plasma Hcy and betaine levels in normotensives and hypertensives. (a and b) show the fasting (baseline) and 5-h post-nicotinamide load plasma Hcy and betaine levels, respectively. #P<0.05 and ##P<0.01 vs. baseline (paired Student's t-test); *P<0.05 and **P<0.01 vs. normotensives (unpaired Student's t-test).
Effects of nicotinamide loading on methylation-mediated catecholamine degradation in normotensives and hypertensives
The baseline plasma norepinephrine levels were significantly higher, whereas the baseline plasma normetanephrine levels were significantly lower in hypertensives than in normotensives (Figure 4a and b). After nicotinamide loading, the plasma norepinephrine levels were increased in both groups, and there were statistically significant differences between the baseline and 5-h post-load values in each group (Figure 4a). The post-load plasma normetanephrine levels were not significantly changed in hypertensives, although they were significantly decreased in normotensives, making the post-loading mean plasma normetanephrine value in normotensives statistically similar to that of hypertensives (Figure 4b). There was no significant difference in the baseline plasma epinephrine and metanephrine levels between the two groups (both P>0.05). Nicotinamide loading induced a slight increase in the plasma epinephrine levels in hypertensives, whereas a slight decrease was seen in normotensives. There was a statistically significant difference in the post-nicotinamide loading plasma epinephrine levels between the two groups (Figure 4c). Moreover, the post-nicotinamide-loading plasma metanephrine levels were significantly decreased in both groups (Figure 4d).
Nicotinamide loading-induced changes in plasma catecholamines and their methylated metabolites in normotensives and hypertensives. (a–d) show the fasting (baseline) and 5-h post-nicotinamide load plasma levels of norepinephrine, normetanephrine, epinephrine and metanephrine, respectively. #P<0.05 and ##P<0.01 vs. baseline (paired Student's t-test); *P<0.05 vs. normotensives (unpaired Student's t-test).
Discussion
In the present study, we found that the hypertensives had higher levels of fasting plasma nicotinamide associated with higher levels of Hcy and norepinephrine, and lower levels of normetanephrine, a methylated derivative of norepinephrine, than normotensives. All methylation reactions of exogenous and endogenous substrates require SAM as the donor of methyl groups. Thus, the increased-fasting plasma nicotinamide levels in hypertensives may be induced by either an increase in niacin intake or a decrease in its methylation-mediated degradation due to other substrate-induced SAM depletion, or both. If the increased nicotinamide levels in hypertensives are induced by other substrate-induced SAM depletion, the fasting levels of plasma N1-methylnicotinamide, the methylated product of nicotinamide, should be decreased due to a lack of methyl groups. However, our results showed that the baseline plasma levels of N1-methylnicotinamide in hypertensives were the same, or even somewhat higher than those of normotensives and not lower as expected. Therefore, the contribution of other substrate(s) to the increased fasting nicotinamide levels, if there is any, is assumed to be very limited in these hypertensives. It has been reported that excessive niacin consumption is very common nowadays;13 thus, it is likely that increased niacin intake may largely account for the higher fasting nicotinamide levels observed in the hypertensives of this study.
Hyperhomocysteinemia is known to be strongly associated with CVD.2, 4 Usually, mild-to-moderate hyperhomocysteinemia is attributed to folate and vitamin B12 deficiency, for these two vitamins participate in the remethylation of Hcy to methionine (Figure 1). However, more recent conclusive evidence indicates that folate and vitamin B12 supplementation does not prevent cardiovascular events.14 Thus, it seems that other mechanisms may be involved in the pathogenesis of Hcy-related CVD. As Hcy generation is linked to the methylation of exogenous and endogenous substrates (Figure 1), the development of Hcy-related CVD may involve the metabolism of exogenous/endogenous methyl-accepting (consuming) substrates. Indeed, the present study found that nicotinamide load significantly increased the levels of plasma Hcy and decreased the levels of plasma betaine, a major labile methyl donor,12 in normotensives. This finding, together with the observations that hypertensives had higher fasting plasma Hcy and nicotinamide levels, suggests that frequent high nicotinamide intake may be a risk factor for hyperhomocysteinemia.
Both excess nicotinamide1 and circulating norepinephrine7 have previously been shown to be degraded through methylation, primarily in the liver. The findings that in normotensives, nicotinamide load significantly increased plasma concentrations of norepinephrine and Hcy while decreasing the levels of normetanephrine and betaine, suggest that excess nicotinamide may deplete liver methyl pool. The observations of higher fasting plasma concentrations of nicotinamide, Hcy and norepinephrine, but lower plasma normetanephrine in hypertensives suggest that the liver methyl-pool may already be in a depleted state, which could limit the conversion of norepinephrine to normetanephrine. This may explain why, in hypertensives, nicotinamide load caused a significant increase in plasma norepinephrine levels without significantly changing plasma normetanephrine levels. Moreover, as plasma metanephrine comes predominantly from the adrenal medulla (>90%),7 the post-nicotinamide-loading decrease in plasma metanephrine seen in both groups suggests that excess nicotinamide may also deplete the methyl pool of the adrenal medulla. Therefore, nicotinamide status may be an important factor in determining the inactivation of catecholamines.
It is well documented that CVD is associated with both elevated Hcy4 and circulating norepinephrine6 levels, and oxidative stress, a key pathogenic factor,15, 16, 17 all of which can be induced by excess nicotinamide. In fact, nicotinamide and its precursor nicotinic acid have long been known to induce glucose intolerance, insulin resistance and liver injury.1, 3, 18 Recently, our studies found that excess nicotinamide may induce oxidative stress, and suggested that obesity and type 2 diabetes, two major risk factors for CVD, may involve increased niacin consumption.8, 13, 19 The present study further demonstrated that excess nicotinamide may contribute to increased circulating catecholamines, as well as increasing plasma Hcy levels.
Whether nicotinamide induces clinical outcomes is expected to be related to the dose and the duration of nicotinamide exposure. NNMT, which is a key enzyme in the degradation of nicotinamide, is not only highly expressed in the liver, but also widely expressed in extrahepatic tissues, including adipose tissue,20 skeletal muscle,21 stomach,22 colon,23 kidney,24 thyroid25 and brain.26 It is obvious that nicotinamide methylation may occur not only in the liver, but also in those extrahepatic tissues. After being absorbed from the stomach and the intestine, niacin is transported to the liver, where excessive niacin is degraded first by hepatic NNMT. Thus, it is conceivable that excessive niacin may first deplete the hepatic methyl pool, and then the methyl pool of extrahepatic tissues if there is an increase in circulating nicotinamide levels. Supporting this suggestion, Riederer et al.20 found that niacin supplements can enhance NNMT activity in mouse adipose tissue, and demonstrated that human adipose tissue is a significant source of Hcy. The present results also suggested that there was a decrease in methylation-mediated degradation of epinephrine in the adrenal medulla after nicotinamide loading, as discussed above. Interestingly, many cancers have been reported to have an enhanced expression of NNMT.22, 23, 24, 25 As NNMT activity is positively related to nicotinamide levels, as demonstrated by Riederer et al,20 it is likely that elevated NNMT expression in cancers may therefore be related to excessive niacin intake.
Modern lifestyle, a major factor in CVD, is characterized by (1) stressors, which may lead to sympathetic overactivity and more catecholamine release, followed by subsequent cardiovascular damage;5, 27 (2) high niacin intake due to an increased use of meat and niacin-fortified grain products;13 and (3) sweat gland inactivity (anaphoresis) due to less physical activity, which may decrease excessive niacin elimination, as niacin can be effectively eliminated from the body through the sweating pathway.8 The latter two factors may contribute to chronic nicotinamide overload (i.e. nicotinamide toxicosis) and subsequent methyl depletion, oxidative stress, insulin resistance and liver injury. The combination of excess niacin and high-fat diets may induce abnormal lipid metabolism and fatty liver.28 Moderate levels of oxidative stress are known to enhance protein degradation, which can increase the release of asymmetric dimethylarginine (ADMA), an endogenous inhibitor of nitric oxide (NO) synthase, an enzyme that converts L-arginine into NO, a potent vasodilator.29 ADMA is formed by post-translational methylation of arginine residues in polypeptides, which is catalyzed by protein arginine N-methyltransferases. Therefore, elevated ADMA levels, which are frequently associated with hyperhomocysteinemia and CVD, may reflect the degradation of methylated arginine-containing proteins.29 Although this hypothesis remains untested, we suspect that an increase in ADMA levels may also occur in excessive nicotinamide-induced oxidative stress. Thus, the adverse effect of excessive nicotinamide on the cardiovascular system may also involve a decrease in the production of NO, due to the inhibition of endothelial NO synthase expressed in the vascular endothelium. Moreover, nicotinamide is a known potent inhibitor of sirtuins, which are enzymes that modulate diverse biologic processes. Emerging evidence indicates that sirtuins have a significant role in many biological processes, including longevity, obesity, fatty liver disease and cardiovascular health (see Kelly30 for review). Thus, it is expected that chronic nicotinamide overload-related clinical outcomes may also involve an inhibition of sirtuins. Investigating changes of sirtuins in response to long-term nicotinamide exposure may be of clinical significance. Therefore, it is likely that the development of CVD may be a consequence of the combined effects of the above factors. To that end, we propose a hypothesis for the etiology of CVD, as shown in Figure 5. It should be pointed out that other exogenous methyl-consuming substrates are expected to have a synergistic effect in inducing methyl depletion.
Proposed hypothesis for the pathogenesis of cardiovascular disease. The development of cardiovascular disease may be a result of combined effects of risk factors, including sympathetic nervous overactivity, high niacin and fat intake and decreased sweat gland activity (see text for details). Elevated plasma homocysteine levels may be an indicator of aberrant methylation status. Met, methionine; SAH, S-adenosylhomocysteine; SAM, S-adenosylmethionine; DMG, N,N-dimethylglycine; THF, tetrahydrofolate; ROS, reactive oxygen species; IR, insulin resistance; ADMA, asymmetric dimethylarginine; NO, nitric oxide; NOS, nitric oxide synthase; The up hollow arrow indicates increase; the down hollow arrow indicates decrease.
In conclusion, the present study demonstrated that excess nicotinamide may inhibit the degradation of catecholamines due to its depletion of the methyl donor pool, and revealed that hypertensives had an abnormal methylation pattern, characterized by elevated fasting plasma levels of unmethylated substrates, including nicotinamide, Hcy and norepinephrine. These findings, taken together with those of previous studies on nicotinamide toxicity, suggest that frequent high-nicotinamide intake may have a role in the development of Hcy-related CVD.
References
Institute of Medicine. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. National Academy Press: Washington, DC, 1998, pp 123–149.
Carmel R, Jacobsen DW . Homocysteine in Health and Disease. Cambridge University Press: Cambridge UK, 2001.
McCarty MF . Co-administration of equimolar doses of betaine may alleviate the hepatotoxic risk associated with niacin therapy. Med Hypotheses 2000; 55: 189–194.
McCully KS . Homocysteine and vascular disease. Nat Med 1996; 2: 386–389.
Malpas SC . Sympathetic nervous system overactivity and its role in the development of cardiovascular disease. Physiol Rev 2010; 90: 513–557.
Goldstein DS . Plasma catecholamines in clinical studies of cardiovascular diseases. Acta Physiol Scand Suppl 1984; 527: 39–41.
Eisenhofer G, Kopin IJ, Goldstein DS . Catecholamine metabolism: a contemporary view with implications for physiology and medicine. Pharmacol Rev 2004; 56: 331–349.
Zhou SS, Li D, Sun WP, Guo M, Lun YZ, Zhou YM, Xiao FC, Jing LX, Sun SX, Zhang LB, Luo N, Bian FN, Zou W, Dong LB, Zhao ZG, Li SF, Gong XJ, Yu ZG, Sun CB, Zheng CL, Jiang DJ, Li ZN . Nicotinamide overload may play a role in the development of type 2 diabetes. World J Gastroenterol 2009; 15: 5674–5684.
Pfeiffer CM, Huff DL, Gunter EW . Rapid and accurate HPLC assay for plasma total homocysteine and cysteine in a clinical laboratory setting. Clin Chem 1999; 45: 290–292.
Laryea MD, Steinhagen F, Pawliczek S, Wendel U . Simple method for the routine determination of betaine and N,N-dimethylglycine in blood and urine. Clin Chem 1998; 44: 1937–1941.
Bechgaard H, Jespersen S . GI absorption of niacin in humans. J Pharm Sci 1977; 66: 871–872.
Ueland PM, Holm PI, Hustad S . Betaine: a key modulator of one-carbon metabolism and homocysteine status. Clin Chem Lab Med 2005; 43: 1069–1075.
Zhou SS, Li D, Zhou YM, Sun WP, Liu QG . B-vitamin consumption and the prevalence of diabetes and obesity among the US adults: population based ecological study. BMC Public Health 2010; 10: 746.
Ebbing M, Ueland PM . Prevention: B vitamins and CVD–failure to find a simple solution. Nat Rev Cardiol 2010; 7: 608–609.
Touyz RM . Reactive oxygen species, vascular oxidative stress, and redox signaling in hypertension: what is the clinical significance? Hypertension 2004; 44: 248–252.
Papaharalambus CA, Griendling KK . Basic mechanisms of oxidative stress and reactive oxygen species in cardiovascular injury. Trends Cardiovasc Med 2007; 17: 48–54.
Fearon IM, Faux SP . Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol 2009; 47: 372–381.
Greenbaum CJ, Kahn SE, Palmer JP . Nicotinamide's effects on glucose metabolism in subjects at risk for IDDM. Diabetes 1996; 45: 1631–1634.
Li D, Sun WP, Zhou YM, Liu QG, Zhou SS, Luo N, Bian FN, Zhao ZG, Guo M . Chronic niacin overload may be involved in the increased prevalence of obesity in US children. World J Gastroenterol 2010; 16: 2378–2387.
Riederer M, Erwa W, Zimmermann R, Frank S, Zechner R . Adipose tissue as a source of nicotinamide N-methyltransferase and homocysteine. Atherosclerosis 2009; 204: 412–417.
Kim HC, Mofarrahi M, Vassilakopoulos T, Maltais F, Sigala I, Debigare R, Bellenis I, Hussain SN . Expression and functional significance of nicotinamide N-methyl transferase in skeletal muscles of patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2010; 181: 797–805.
Jang JS, Cho HY, Lee YJ, Ha WS, Kim HW . The differential proteome profile of stomach cancer: identification of the biomarker candidates. Oncol Res 2004; 14: 491–499.
Roessler M, Rollinger W, Palme S, Hagmann ML, Berndt P, Engel AM, Schneidinger B, Pfeffer M, Andres H, Karl J, Bodenmüller H, Rüschoff J, Henkel T, Rohr G, Rossol S, Rösch W, Langen H, Zolg W, Tacke M . Identification of nicotinamide N-methyltransferase as a novel serum tumor marker for colorectal cancer. Clin Cancer Res 2005; 11: 6550–6557.
Sartini D, Muzzonigro G, Milanese G, Pierella F, Rossi V, Emanuelli M . Identification of nicotinamide N-methyltransferase as a novel tumor marker for renal clear cell carcinoma. J Urol 2006; 176: 2248–2254.
Xu J, Moatamed F, Caldwell JS, Walker JR, Kraiem Z, Taki K, Brent GA, Hershman JM . Enhanced expression of nicotinamide N-methyltransferase in human papillary thyroid carcinoma cells. J Clin Endocrinol Metab 2003; 88: 4990–4996.
Parsons RB, Smith SW, Waring RH, Williams AC, Ramsden DB . High expression of nicotinamide N-methyltransferase in patients with idiopathic Parkinson's disease. Neurosci Lett 2003; 342: 13–16.
Black PH, Garbutt LD . Stress, inflammation and cardiovascular disease. J Psychosom Res 2002; 52: 1–23.
Rikans LL, Arata D, Cederquist DC . Fatty livers produced in albino rats by excess niacin in high fat diets. I. Alterations in enzyme and coenzyme systems induced by supplementing 40% fat diets with 0.1% of niacin. J Nutr 1964; 82: 83–87.
Kielstein JT, Fliser D, Veldink H . Asymmetric dimethylarginine and symmetric dimethylarginine: axis of evil or useful alliance? Semin Dial 2009; 22: 346–350.
Kelly GS . A review of the sirtuin system, its clinical implications, and the potential role of dietary activators like resveratrol: part 2. Altern Med Rev 2010; 15: 313–328.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (30570665); the Foundation of Dalian Technology Bureau (2008E13SF182); and the Foundation of Key Laboratory of Education Department of Liaoning Province (2009S005).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Sun, WP., Li, D., Lun, YZ. et al. Excess nicotinamide inhibits methylation-mediated degradation of catecholamines in normotensives and hypertensives. Hypertens Res 35, 180–185 (2012). https://doi.org/10.1038/hr.2011.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2011.151
Keywords
This article is cited by
-
Relationship between dietary niacin intake and diabetes mellitus in the National Health and Nutrition Examination Survey (NHANES) 2003–2018
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)
-
Diverse therapeutic efficacies and more diverse mechanisms of nicotinamide
Metabolomics (2019)
-
Management of nicotinamide N-methyltransferase overexpression: inhibit the enzyme or reduce nicotinamide intake?
Diabetologia (2015)
-
The skin function: a factor of anti-metabolic syndrome
Diabetology & Metabolic Syndrome (2012)