Abstract
Following the introduction of angiotensin-converting enzyme (ACE) inhibitors in the treatment of hypertension and ischemic heart disease, there has been increasing interest in the bradykinin-mediated aspects of ACE inhibition. Several preclinical and clinical studies have been conducted using genetically engineered animals or pharmacological agonists and antagonists of the two receptors of bradykinin, B1R and B2R. The results have mostly indicated that the B1R, whose expression is induced by tissue damage, seem to have mostly noxious effects, whereas the constitutively expressed B2R, when activated, exert mostly beneficial actions. Accumulating evidence in the recent literature suggests that the B2R have an important role in the process of ischemic post-conditioning that limits the ischemia/reperfusion injury of the myocardium. In this article, we describe a series of experiments conducted on mice submitted to acute myocardial infarct and treated either with ACE inhibition (which produces potentiation of bradykinin resulting in non-selective B1R and B2R activation) or with a potent and highly selective B2R agonist. These data suggest that this latter pharmacological approach offers functional and structural benefits and is therefore a promising cardioprotective therapeutic modality against acute ischemic events.
Similar content being viewed by others
Introduction
The possible role of bradykinin (BK) in cardiovascular regulation has intrigued scientists for many years. A member of the kinin system discovered in the late 1920s, BK is a nonapeptide whose existence was first recognized by Roha e Silva et al.1 from its effects on intestinal smooth muscle. Since then, several other actions of BK were described, including vascular contraction and relaxation, participation in the process of inflammatory reactions, interaction with central and peripheral neural structures, stimulation of synthesis and release of various vasoactive substances, enhanced insulin-dependent glucose transport and utilization, etc.
Circulatory homeostasis is the result of a constant equilibrium between vasoconstrictors (e.g., pressor neurohormonal factors like angiotensin II, catecholamines, vasopressin, endothelin) and vasodilators (like kinins, prostaglandins, NO, etc.). Bradykinin, a tissue hormone that regulates the regional blood flows of vital organs, is an important member of the latter group.2 The role of BK in cardiovascular regulation under physiological and pathological conditions attracted the interest of clinicians with the advent of angiotensin-converting enzyme (ACE) inhibitors, which in the last two decades have become standard therapy for hypertension, ischemic heart disease and heart failure.3
In recent years the work of many investigators has produced a lot of new information regarding the role of kinins in the pathophysiology of hypertension and the prevention of its end-organ complications. Interest in the physiology and pharmacology of BK was prompted by the discoveries that the kininase II, which degrades BK is identical to the ACE;4 that the BK-potentiating factors isolated from a snake venom could act as antihypertensives in experimental hypertension;5 that renal prostaglandins synthesized locally were both stimulated by, and found to mediate the action of locally generated kinins;6, 7 that various types of hypertension were associated with, and probably affected by, changes in the renal kallikrein–kinin system;8 that cyclooxygenase inhibitors, which interrupt prostaglandin synthesis, could induce renal failure through their effects on kinins as well as on the renin–angiotensin system;9 and, most importantly, by the realization that part of the BP lowering and other effects of ACE inhibitors must be accounted for by potentiation of BK.10 Notably, the main adverse effects of ACE inhibition, that is, cough and angioedema, have also been attributed to amplified reactions to BK when its enzymatic degradation is impaired.11
The cardioprotective effects of ACE inhibition are well recognized, but have been mostly attributed to inhibition of the formation of angiotensin II, whose cardiotoxic (and nephrotoxic) properties were described long ago. The fact that angiotensin AT1 receptor blockade—which does not involve alteration in BK metabolism—can similarly prevent or minimize end-organ damage has initially focused attention on the angiotensin-mediated actions of both interventions. However, a growing body of evidence in recent years indicates that part of the cardioprotective benefits of ACE inhibition is attributable to the diminished degradation and hence accumulation of BK. The following mini-review will highlight some of the studies that show the role of the two BK receptors under conditions of cardiac ischemia and will concentrate on the growing experimental evidence indicating that selective activation of the B2 type receptor has cardioprotective properties.
Bradykinin receptors
A large body of literature over the past several years has explored the physiopharmacology of BK and defined its two receptor types, B1R and B2R, which mediate its multiple hemodynamic and metabolic effects.12 In earlier years this was accomplished mainly via use of peptide analogs with agonistic and antagonistic properties. It has generally been accepted that all the physiologically significant hemodynamic and metabolic actions of bradykinin are exerted via activation of the constitutive B2R. Indeed, acute and chronic infusion of BK antibodies13 or selective B2R antagonists in animals14, 15 and humans16 was shown to partly reverse the antihypertensive effect of ACE inhibitors; to prevent the cardioprotective action of ACE inhibition in animals submitted to cardiac ischemia/reperfusion injury;17, 18 and to inhibit the amelioration of insulin-dependent glucose transport by ACE inhibitors.19, 20 On the contrary, the B1R is believed to be mostly unexpressed under normal conditions, but is highly inducible by lipopolysaccharides, bacterial toxins and inflammatory mediators resulting from tissue injury.21
More recently, advances in molecular biology permitted the cloning and characterization of these receptors and the creation of genetically engineered mice with deletion of the B2R22 or B1R.23 Several investigators have used B2R gene knockout mice to further explore the physiological actions of BK. Compared with their wildtype controls, these animals were shown by some investigators to have higher blood pressure at baseline24 although others did not confirm this finding.25, 26 However, everybody agrees that inactivation of the B2R makes animals particularly salt-sensitive, that is, prone to develop earlier and more severe hypertensive response to salt loading.24, 25, 26, 27 They were also found to have less efficient myocardial metabolism with increased propensity to ischemic myocardial injury28 and increased cardiac oxygen consumption.29
There is also evidence that kinins affect preferentially the cardiac and renal perfusion30 and influence the local redistribution of blood flow within these organs, favoring the subendocardial layers of the myocardium31 and the papillary region of the kidney,32 that is, the areas most vulnerable to ischemic tissue damage. It has repeatedly been shown that activation of the endogenenous kallikrein–kinin system by various means can protect the myocardium from ischemia/reperfusion injury. Indeed, the protective effects of ACE inhibitors in this setting can be partially abolished by B2R antagonists,17, 18, 33, 34 whereas gene treatment designed to enhance the expression of kinins was shown to attenuate the damage and subsequent remodeling after acute myocardial infarct (AMI).35
Another property of the kallikrein–kinin system contributing to its tissue-protective actions is its capacity to enhance the insulin-dependent glucose transport and metabolism,36, 37 which has been shown in both animal and human experiments.37, 38 Indeed, the well-recognized effect of ACE inhibition to improve insulin sensitivity is in part attributed to bradykinin,39 whereas kininogen-deficient rats were found to be resistant to insulin.40 This effect of ACE inhibition is also mediated by the B2R, because it is reversed by selective B2R antagonists;19, 20 but, unlike the vasodilatory effects of bradykinin, which are exerted via B2R-mediated activation of the prostaglandin-NO cascade (which can also be stimulated by the B1R, albeit via different mechanism),41 this metabolic activity appears to be a direct effect of the B2R.20, 42, 43 Indeed, B2R gene knockout mice show severe insulin resistance, despite compensatory upregulation of the B1R.42
Cardiovascular complications of hypertension and atherosclerosis are associated with elevation in plasma levels of biochemical markers of inflammation, such as the proinflammatory cytokines interleukin-6 and tumor necrosis factor-α (TNF-α), as well as the resulting stimulation of C-reactive protein.44, 45, 46 High sensitivity C-reactive protein is also significantly correlated with measures of arterial stiffness,47, 48 which may be partly due to angiotensin II49, 50 and partly to metabolic abnormalities, such as diabetes mellitus, with its advanced glycation endproducts, not necessarily correlated to BP. Indeed, ACE inhibition was shown to reverse arterial stiffness in diabetic normotensive patients.51
Unlike the B2Rs, which are constitutively expressed throughout and mediate the majority of the vascular and metabolic actions of kinins, as mentioned above, the B1Rs are generally absent from normal tissues, but are known to become induced by a variety of pathological conditions, including inflammation, the presence of toxins, cytokines or tissue trauma.21, 52 They were also found to become induced and upregulated by disturbances in circulatory homeostasis, such as induction of experimental hypertension by salt loading, renal artery clipping or exogenous Angiotensin II (Ang II) infusion41, 53 as well as by the normal aging process.54 But the most important stimulus causing overexpression of the B1R was found to be the disruption of the B2R, whether due to functional inactivation via a selective B2R antagonist or to deletion of B2R gene.41, 42, 55 In such cases, the B1R can take over some of the vasodilatory functions of the B1R, but not its metabolic (insulin-sensitizing) function. It was recently reported that in hearts from subjects with end stage cardiac failure, the expression of B1Rs was significantly increased both at the mRNA and the protein level56, 57 in contrast to the B2Rs, which were found to be significantly downregulated.58 A plausible explanation for these findings is that increases in expression and activity of the B1R may be partly triggered by inflammatory cytokines, such as TNF-α, whose levels increase in chronic heart failure59, 60, 61 and chronic tissue injury, but may also represent a compensatory reaction to diminished functional capacity of the B2R. At this time it is unclear whether the upregulation of the B1R under these circumstances may be beneficial by enhancing regional blood flow, thus contributing to tissue protection, or may actually have a detrimental effect by interacting with inflammatory mediators and further exacerbating the inflammatory process.
Nevertheless, the overall experience from basic and experimental studies to date supports the notion that any tissue-protective actions of BK are mostly exerted via activation of the B2R. Following is a brief review of the data indicating that B2R activation can protect the myocardium that has been exposed to ischemic injury, and therefore a highly selective B2R agonist can be cardioprotective, while avoiding the adverse consequences of B1R activation.
B2R-mediated cardioprotection post ischemic injury
As mentioned above, the properties of BK under various conditions have been studied extensively with the use of BK analogs with various degrees of agonistic or antagonistic capacity and affinity for the B1R and B2R. Earlier studies used mostly agents with BK receptor blocking capacity. One of those, the selective B2R antagonist HOE-140 or icatibant, has been the agent most widely used in experimental animal and human studies and shown to partly reverse the antihypertensive action of ACE inhibitors15, 16 to prevent the cardioprotective action of ACE inhibition in animals submitted to cardiac ischemia/reperfusion injury17, 18 and to counteract the amelioration of insulin-dependent glucose transport and utilization that normally occurs with the use of ACE inhibitors.19, 20
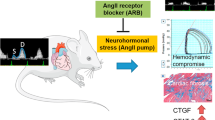
Acute myocardial ischemia causes neurohormonal activation associated with a sharp increase in vasopressor hormones, including the renin system. Ang II was shown long ago to be a cause of acute ischemic myocardial tissue damage leading to microfoci of necrosis and scarring.62 More recently, we have found that Ang II in vivo and in vitro stimulates gene overexpression of various vasoactive factors, including the B1R and B2R genes53 as well as a novel gene, the cardiomyopathy-associated 3, also known as myomaxin and recently renamed Xirp2.63, 64, 65 Although this gene's product remains unknown, its contribution to ischemic cardiomyopathy is crucial, as shown by studies in genetically engineered mice.65 Interestingly, concurrent inhibition of the AT1 receptor of Ang II with losartan can abolish the BK receptor upregulation.53 Furthermore, ACE itself can also upregulate the gene expression of both BK receptors by up to 11–22 fold, via a mechanism apparently unrelated to its enzymatic properties.66 It was reported that in myocardial tissues of rats submitted to acute myocardial infarct there was a significant upregulation of both B1R and B2R detectable within 6 h and reaching its peak at 24 h,57, 67, 68 with the B1R expression returning gradually to baseline in the next 3–6 days, whereas the B2R overexpression appears to last much longer. Thus, myocardial ischemia—whether due to Ang II-induced coronary constriction or to mechanical coronary obstruction—is associated with an upregulation of both BK receptors that would seem to be compensatory, but may also have noxious effects as well.
To further define the function of each BK receptor under ischemic conditions, we conducted a number of experiments in genetically engineered mice with deletion of either the B2R or the B1R gene. In B2R gene knockouts, the B1R becomes highly upregulated and assumes most of the hemodynamic properties of the B2R. It also becomes upregulated in response to experimental manipulations inducing hypertension, which do not affect B2R gene expression.41 In the absence of B2R, the B1R can still contribute to BP lowering by ACE inhibition, as it too can influence vasoactive components of the arachidonic acid cascade, although the effects of the two BK receptors on specific components of the prostaglandin/nitric oxide sequence are different.27 But, although the B2R gene knockout mice can still respond to BK with B1R-mediated vasodilation, they cannot respond to the insulin-sensitizing action of BK. Indeed, using the hyperinsulinemic euglycemic clamp technique, we found that B2R gene knockout mice become severely insulin-resistant, despite marked B1R upregulation,42 evidently because this effect is exerted directly by the B2R and not via the prostaglandin/NO cascade.
The B1R gene knockout mice seem to have a normal cardiovascular phenotype at rest, although they have evidence of hypoalgesia and abnormal responses to inflammatory mediators.23 They also have markedly overexpressed B2R genes. In a recent series of experiments, we induced AMI by ligation of the left anterior descending coronary artery in B1R or B2R gene knockout mice and wild-type controls and evaluated their cardiac function with or without ACE inhibition.69 Not surprisingly, wild-type mice had a significant decrease in left ventricular (LV) systolic capacity if untreated, whereas if treated with lisinopril they had a significantly lesser loss of LV function. The B1R gene knockouts, despite overexpression of the B2R, had a similar degree of decrease in LV systolic function whether treated with ACEI or not. However, the B2R gene knockouts with overexpressed B1R, not only had a significantly greater loss of LV systolic capacity than the other groups if left untreated, but also showed a further deterioration, rather than improvement, in LV function if treated with ACEI. These data indicated that potentiation of BK in the absence of B1R is insufficient to provide full cardioprotection, despite upregulated B2R; however, in the setting of absent B2R and upregulated B1R, the potentiation of BK actually seems to inflict further cardiac tissue damage.68 In view of the known proinflammatory and noxious B1R-mediated actions and the loss of the metabolic B2R-mediated properties that would enhance glucose utilization by the ischemic myocardium, it is not surprising that BK potentiation in the setting of absent B2R and upregulated B1R would exert an additional detrimental effect on the injured myocardium.
A growing body of literature in recent years has accumulated data regarding the process of ischemic post-conditioning, which minimizes the myocardial damage following ischemia/reperfusion injury.70 Although there have been some conflicting data regarding the role of the B1R in this setting, there is general agreement on the beneficial cardioprotective effects of B2R activation.28, 71, 72 These data provide conclusive evidence indicating that the B2R have a crucial role in this process of preserving myocardial tissue integrity and functional capacity to various degrees, depending on coexisting conditions and interventions.
In the past it has been theorized that BK receptor agonists, especially those selective for the B2R, should be considered as means to improve myocardial metabolism in the setting of various cardiovascular disorders, but that the safe therapeutic window between potential beneficial and harmful effects of BK analogs should first be defined.73 As it is widely accepted that most physiologically important and beneficial effects of BK—including its vasodilatory properties and its insulin-sensitizing effects—are exerted through the constitutively expressed B2R, whereas the B1R that is inducible by factors released after tissue injury or inflammation may cause further harm, any BK analog considered for pharmacotherapy should be a BK agonist highly selective for the B2R. Indeed, a few years back it was reported that coronary artery ligation produced a larger size AMI in kininogen-deficient rats than in normal rats; however, if the former rats were treated for 24 h with infusion of a B2R agonist, the size of their AMI was the same as that of normal rats, suggesting improved myocardial blood flow in the borders of the ischemic area.74 By contrast, as mentioned earlier, infusion of a B2R antagonist has been shown to prevent or reverse the cardioprotective action of ACE inhibition.17, 18
Treatment with a selective B1R antagonist in the setting of AMI has no effects of its own; however, it was shown to reverse the cardioprotective action of the angiotensin AT1 receptor blocker irbesartan75 despite the fact that BK potentiation does not contribute to the vasodilatory/antihypertensive actions of AT1 receptor blockers. This finding was attributed to the cross-talk between AT1 and B1R genes. Indeed, there is emerging evidence that in addition to the widely investigated hemodynamic and metabolic actions of the ACE, Ang II and BK, they also have transcriptional regulatory properties and interactions that have not yet been fully appreciated: Ang II stimulates gene expression of the BK receptors, an action inhibited by the AT1 receptor blocker losartan,53 and ACE inhibitors have been reported to affect gene expression of BK receptors in the absence of ACE,76 whereas ACE itself can enter the nucleus of cells and stimulate gene expression of BK receptors.66, 77 Incidentally, there is a large body of literature exploring the molecular signaling interactions elicited by vasoactive factors and their possible implications on carcinogenesis.78 Such interactions further complicate the interpretation of results from pharmacological interventions altering the function of these vasoactive factors and the molecular mechanisms mediating these results. Nevertheless, the hemodynamic and histological results are indisputable, even when the underlying molecular mechanisms are unclear.
Recently Dr Gobeil and colleagues from Sherbrooke University, Canada, came up with a series of BK peptide analogs, of which one, the compound NG 291 (Hyp3, Thi5 NChg7 Thi8-BK) was a B2R agonist with the highest potency, selectivity and affinity for the B2R and the highest resistance to proteolytic enzymes.79 Using this agent, we conducted a series of experiments designed to evaluate the capacity of selective B2R activation to minimize ischemic myocardial damage. After inducing AMI via ligation of the left anterior descending coronary artery in mice, we initiated a continuous infusion of this agent for 1 week via osmotic minipump implanted subcutaneously in their scapular area. We then compared the functional LV capacity and the extent of cardiac tissue damage and remodeling, as well as the gene expression pattern of a number of factors related to myocardial tissue inflammation, perfusion and metabolism, between actively treated mice and control mice receiving the vehicle saline solution. We found that actively treated mice had a significantly attenuated decrease in systolic function compared with saline-treated mice, as shown by the better ejection fraction and better fractional shortening, as well as a lesser degree of cardiac remodeling and a closer to normal body weight to heart weight ratio. Despite the known vasodilatory effects of the B2R, systolic blood pressure at end-point was normal in the B2R agonist-treated mice, whereas it tended to be depressed in the saline-treated controls, evidently reflecting the diminished cardiac systolic capacity and decreased cardiac output. The infarct size tended to be smaller, though not significantly so, in actively treated mice, but there was a significant increase in markers of myocardial cell necrosis and apoptosis in the saline-treated group.80
Analysis of expression patterns of selected genes to factors related to tissue injury, inflammation and metabolism, was performed in cardiac tissues from the two MI groups, in comparison with cardiac tissues of sham-operated mice with or without B2R agonist treatment. The results indicated that acute myocardial ischemia induced significant upregulation of these genes (that is, the B1R, B2R, eNOS, TNF-α, PDk4 and cardiomyopathy-associated 3/Xirp2), whereas the B2R agonist itself produced no difference in pattern of gene expression in the myocardium of sham-operated mice, whose patterns were similar to the saline-treated sham-operated ones. However, the active treatment produced a profound attenuation of the upregulation of these genes in the actively treated MI mice to levels close to those of the sham-operated normal animals. As these factors are reported to regulate tissue perfusion, metabolism and apoptosis, we concluded that their tendency to normalization must reflect the beneficial influence of the experimental treatment.
These experiments prove that a continuous infusion for 1 week of a potent and highly selective B2R agonist of bradykinin initiated at the time of occurrence of an acute MI can diminish the extent of myocardial damage. This is shown by the significantly improved indices of left ventricular function and cardiac tissue remodeling, as well as the significantly attenuated pattern of inflammation-related tissue gene expression, which explains the structural and functional benefits of the treatment. With this approach, it is possible to take advantage of the beneficial effects of B2R activation, while avoiding the nefarious consequences of upregulation and stimulation of the B1R. In fact, this approach could also be utilized in other conditions of myocardial ischemia, for example, surgical procedures, where preservation of myocardial tissue may be enhanced by optimizing glucose metabolism. One intervention that has recently been re-introduced to this aim is the ‘GIK’ treatment, that is, a controlled glucose–insulin–potassium infusion81 that was shown to benefit diabetics with coronary artery disease undergoing cardiac surgery. A B2R agonist infused along with the GIK components would further enhance the benefits of this intervention by promoting optimal glucose utilization by cardiomyocytes, something particularly useful for patients with type II diabetes mellitus, who are already at higher risk of ischemic cardiac events and adverse long-term consequences of such events.
Conclusions
In this review, we describe the results of a recently conducted series of experiments on wild-type or genetically engineered mice with deleted B1R or B2R, submitted to acute MI and treated with an ACE inhibitor or with a highly selective B2R agonist bradykinin analog. Overall, the results of these studies offer additional support to the notion that unselective potentiation of bradykinin may lead to mixed results, as activation of the B1R appears to have predominantly noxious effects, whereas selective activation of the B2R has predominantly beneficial effects in terms of both functional and structural cardioprotective actions. We therefore conclude that treatment with a potent and highly selective B2R agonist, initiated immediately after the occurrence of an acute ischemic event, should be further explored as a potential therapeutic option in these circumstances; indeed the data so far offer ‘proof of concept’ for the value of this pharmacological approach, but further studies are needed to ascertain the safety and long-term efficacy of this intervention.
References
Rocha e Silva M, Beraldo WT, Rosenfeld G . Bradykinin a hypotensive and smooth muscle stimulating factor released from plasma globulin by snake venoms and by trypsin. Am J Physiol 1949; 156: 261–273.
Carretero OA, Scicli AG . Local hormonal factors (intracrine, autocrine, and paracrine) in hypertension. Hypertension 1991; 18: I58–169.
Gavras H . Angiotensin-converting enzyme inhibition and the heart. Hypertension 1994; 23: 813–818.
Yang HY, Erdos EG, Levin Y . A dipeptidyl carboxypeptidase that converts angiotensin I and inactivates bradykinin. Biochim Biophys Acta 1970; 214: 374–376.
Krieger EM, Salgado HC, Assan CJ, Greene LLJ, Ferreira SH . Potential screening test for detection of overactivity of renin-angiontensin system. Lancet 1971; 1: 269–271.
McGiff JC, Itskovitz HD, Terragno A, Wong PYK . Modulation and mediation of the action of the renal kallikrein-kinin system by prostaglandins. Fed Proc 1976; 5: 175–180.
Nasjletti A, Malik KU . Relationships between the kallikrein-kinin and prostaglandin systems. Life Sci 1979; 25: 99–110.
Mills IH . Renal kallikrein and regulation of blood pressure in man. In: Erdos DG (ed). Bradykinin, Kallidin and Kallikrein. Springer Verlag, New York, 1979. pp 549–567.
Romero JC, Dunlop CL, Strong CG . The effect of indomethacin and other anti-inflammatory drugs on the renin-angiotensin system. J Clin Invest 1976; 58: 282–288.
Gavras I . Bradykinin-mediated effects of ACE inhibition. Kidney Int 1992; 42: 1020–1029.
Adam A, Cugno M, Molinaro G, Perez M, Lepage Y, Agostoni A . Aminopeptidase P in individuals with a history of angio-oedema on ACE inhibitors. Lancet 2002; 359: 2088–2089.
Regoli D, Barabe J . Pharmacology of bradykinin and related kinins. Pharmacol Rev 1980; 32: 1–46.
Carretero OA, Miyazaki S, Scicli AG . Role of kinins in the acute antihypertensive effect of converting enzyme inhibitor captopril. Hypertension 1981; 3: 18–22.
Benetos A, Gavras H, Stewart JM, Vavrek RJ, Hatinoglou S, Gavras I . Vasodepressor role of endogenous bradykinin assessed by a bradykinin antagonist. Hypertension 1986; 8: 971–974.
Wirth K, Hock FJ, Albus U, St Henke GA, Breipohl G, Konig W, Knolle J, Scholkens BA . Hoe 140 a new potent and long acting bradykinin-antagonist: in vivo studies. Br J Pharmacol 1991; 106: 774–777.
Gainer JV, Morrow JD, Loveland A, King DJ, Brown NJ . Effect of bradykinin-receptor blockade on the response to angiotensin-converting-enzyme inhibitor in normotensive and hypertensive subjects. N Engl J Med 1998; 339: 1285–1292.
Hartman JC, Wall TM, Hullinger TG, Shebuski RJ . Reduction of myocardial infarct size in rabbits by ramiprilat: reversal by the bradykinin antagonist HOE 140. J Cardiovasc Pharmacol 1993; 21: 996–1003.
Liu YH, Yang XP, Sharov VG, Sigmon DH, Sabbath HN, Carretero OA . Paracrine systems in the cardioprotective effect of angiotensin-converting enzyme inhibitors on myocardial ischemia/reperfusion injury in rats. Hypertension 1996; 27: 7–13.
Tomiyama H, Kushiro T, Abeta H, Ishii T, Takahashi A, Furukawa L, Asagami T, Hino T, Saito F, Otsuka Y, Kurumatani H, Kobayashi F, Kanmatsuse K, Kajiwara N . Kinins contribute to the improvement of insulin sensitivity during treatment with angiotensin converting enzyme inhibitor. Hypertension 1994; 23: 450–455.
Kohlman Jr O, Neves Fde A, Ginoza M, Tavares A, Cezaretti ML, Zanella MT, Ribeiro AB, Gavras I, Gavras H . Role of bradykinin in insulin sensitivity and blood pressure regulation during hyperinsulinemia. Hypertension 1995; 25: 1003–1007.
Regoli DC, Marceau F, Lavigne J . Induction of B1-receptors for kinins in the rabbit by a bacterial lipopolysaccharide. Eur J Pharmacol 1981; 71: 105–115.
Borkowski JA, Ransom RW, Seabrook GR, Trumbauer M, Chen H, Hill RG, Strader CD, Hess JF . Journal title: targeted disruption of a B2 bradykinin receptor gene in mice eliminates bradykinin action in smooth muscle and neurons. J Biol Chem 1995; 270: 13706–13710.
Pesquero JB, Araujo RC, Heppenstall PA, Stucky CL, Silva Jr JA, Walter T, Oliveria SM, Pesquero JL, Paiva ACM, Calixto JB, Lewin GR, Bader M . Hypoalgesia and altered inflammatory responses in mice lacking kinin B1 receptors. Proc Natl Acad Sci USA 2000; 97: 8140–8145.
Madeddu P, Varoni MV, Palomba D, Emanueli C, Demontis MP, Glorioso N, Dessi-Fulgheri P, Sarzani R, Anania V . Cardiovascular phenotype of a mouse strain with disruption of bradykinin B2-receptor gene. Circulation 1997; 96: 3570–3578.
Alfie ME, Yang XP, Hess F, Carretero OA . Salt-sensitive hypertension in bradykinin B2 receptor knockout mice. Biochem Biophys Res Commun 1996; 224: 625–630.
Cervenka L, Harrison-Bernard LM, Dipp S, Primrose G, Imig D, El-Dahr SS . Early onset salt-sensitive hypertension in bradykinin B(2) receptor null mice. Hypertension 1999; 34: 176–180.
Duka I, Kintsurashvili E, Gavras I, Johns C, Bresnahan M, Gavras H . Vasoactive potential of the B1 bradykinin receptor in normotension and hypertension. Circ Res 2001; 88: 275–281.
Yang XP, Liu YH, Scicli GM, Webb CR, Carretero OA . Role of kinins in the cardioprotective effect of preconditioning: study of myocardial ischemia/reperfusion injury in B2 kinin receptor knockout mice and kininogen-deficient rats. Hypertension 1997; 30: 735–740.
Loke KE, Curran CM, Messina EJ, Laycock SK, Shesely EG, Carretero OA, Hintze TH . Role of nitric oxide in the control of cardiac oxygen consumption in B(2)-kinin receptor knockout mice. Hypertension 1999; 34: 563–567.
Wang YX, Gavras I, Wierzba T, Lammek B, Gavras H . Inhibition of nitric oxide, bradykinin, and prostaglandins in normal rats. Hypertension 1992; 19: II255–II261.
Ruocco NA, Bergelson BA, Yu TK, Gavras I, Gavras H . Augmentation of coronary blood flow by ACE inhibition: role of angiotensin and bradykinin. Clin Exp Hypertens 1995; 17: 1059–1072.
Scicli AG, Carretero OA . Renal kallikrein-kinin system. Kidney Int 1986; 29: 120–130.
Martorana PA, Kettenbach B, Breipohl G, Linz W, Scholkens BA . Reduction of infarct size by local angiotensin-converting enzyme inhibition is abolished by a bradykinin antagonist. Eur J Pharmacol 1990; 182: 395–396.
Linz W, Wiemer G, Gohlke P, Unger T, Scholkens BA . Contribution of kinins to the cardiovascular actions of angiotensin-converting enzyme inhibitors. Pharmacol Rev 1995; 47: 25–49.
Agata J, Chao L, Chao J . Kallikrein gene delivery improves cardiac reserve and attenuates remodeling after myocardial infarction. Hypertension 2002; 40: 653–659.
Isami S, Kishikawa H, Araki E, Uehara M, Kaneko K, Shirotani T, Todaka M, Ura S, Motoyoshi S, Matsumoto K, Miyamura N, Shichiri M . Bradykinin enhances GLUT4 translocation through the increase of insulin receptor tyrosine kinase in primary adipocytes: evidence that bradykinin stimulates the insulin signalling pathway. Diabetologia 1996; 39: 412–420.
Henriksen EJ, Jacob S, Fogt DL, Dietze GJ . Effect of chronic bradykinin administration on insulin action in an animal model of insulin resistance. Am J Physiol 1998; 275: R40–R45.
Dietze GJ, Wicklmayr M, Rett K, Jacob S, Henriksen EJ . Potential role of bradykinin in forearm muscle metabolism in humans. Diabetes 1996; 45 (Suppl 1): S110–S114.
Henriksen EJ, Jacob S, Augustin HJ, Dietze GJ . Glucose transport activity in insulin-resistant rat muscle. Effects of angiotensin-converting enzyme inhibitors and bradykinin antagonism. Diabetes 1996; 45 (Suppl 1): S125–S128.
Damas J, Bourdon V, Lefebvre PJ . Insulin sensitivity, clearance and release in kininogen-deficient rats. Exp Physiol 1999; 84: 549–557.
Duka I, Kintsurashvili E, Gavras I, Johns C, Bresnahan M, Gavras H . Vasoactive potential of the B1 bradykinin receptor in normotension and hypertension. Circ Res 2001; 88: 275–281.
Duka I, Shenouda S, Johns C, Kintsurashvili E, Gavras I, Gavras H . Role of the B(2) receptor of bradykinin in insulin sensitivity. Hypertension 2001; 38: 1355–1360.
Gavras I, Gavras H . Metabolic effects of angiotensin-converting enzyme inhibition. The role of bradykinin. Curr Opin Endocrinol Diabetes 2002; 9: 323–328.
Chae CU, Lee RT, Rifai N, Ridker PM . Blood pressure and inflammation in apparently healthy men. Hypertension 2001; 38: 399–403.
Pai JK, Pischon T, Ma J, Manson JE, Hankinson SE, Joshipura K, Curhan GC, Rifai N, Cannuscio CC, Stampfer MJ, Rimm EB . Inflammatory markers and the risk of coronary heart disease in men and women. N Engl J Med 2004; 351: 2599–2610.
Bautista LE, Vera LM, Arenas IA, Gamarra G . Independent association between inflammatory markers (C-reactive protein, interleukin-6, and TNF-alpha) and essential hypertension. J Hum Hypertens 2005; 19: 149–154.
Yasmin, McEniery CM, Wallace S, Mackenzie IS, Cockcroft JR, Wilkinson IB . C-reactive protein is associated with arterial stiffness in apparently healthy individuals. Arterioscler Thromb Vasc Biol 2004; 24: 969–974.
Mattace-Raso FU, van der Cammen TJ, van der Meer IM, Schalekamp MA, Asmar R, Hofman A, Witteman JC . C-reactive protein and arterial stiffness in older adults: the Rotterdam Study. Atherosclerosis 2004; 176: 111–116.
Bassuk SS, Rifai N, Ridker PM . High-sensitivity C-reactive protein: clinical importance. Curr Probl Cardiol 2004; 29: 439–493.
Mahmud A, Feely J . Arterial stiffness is related to systemic inflammation in essential hypertension. Hypertension 2005; 46: 1118–1122.
Manolis AJ, Iraklianou S, Pittaras A, Zaris M, Tsioufis K, Psaltiras G, Psomali D, Foussas S, Gavras I, Gavras H . Arterial compliance changes in diabetic normotensive patients after angiotensin-converting enzyme inhibition therapy. Am J Hypertens 2005; 18: 18–22.
Marceau F, Hess JF, Bachvarov DR . The B1 receptors for kinins. Pharmacol Rev 1998; 50: 357–386.
Kintsurashvili E, Duka I, Gavras I, Johns C, Farmakiotis D, Gavras H . Effects of ANG II on bradykinin receptor gene expression in cardiomyocytes and vascular smooth muscle cells. Am J Physiol Heart Circ Physiol 2001; 281: H1778–H1783.
Kintsurashvili E, Duka A, Ignjacev I, Pattakos G, Gavras I, Gavras H . Age-related changes of bradykinin B1 and B2 receptors in rat heart. Am J Physiol Heart Circ Physiol 2005; 289: H202–H205.
Duka I, Duka A, Kintsurashvili E, Johns C, Gavras I, Gavras H . Mechanisms mediating the vasoactive effects of the B1 receptors of bradykinin. Hypertension 2003; 42: 1021–1025.
Liesmaa I, Kuoppala A, Shiota N, Kokkonen JO, Kostner K, Mayranpaa M, Kovanen PT, Lindstedt KA . Increased expression of bradykinin type-1 receptors in endothelium of intramyocardial coronary vessels in human failing hearts. Am J Physiol Heart Circ Physiol 2005; 288: H2317–H2322.
Tschope C, Heringer-Walther S, Walther T . Regulation of the kinin receptors after induction of myocardial infarction: a mini-review. Braz J Med Biol Res 2000; 33: 701–708.
Kuoppala A, Shiota N, Lindstedt KA, Rysa J, Leskinen HK, Luodonpaa M, Liesmaa I, Ruskoaho H, Kaaja R, Kovanen PT, Kokkonen JO . Expression of bradykinin receptors in the left ventricles of rats with pressure overload hypertrophy and heart failure. J Hypertens 2003; 21: 1729–1736.
Levine B, Kalman J, Mayer L, Fillit HM, Packer M . Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N Engl J Med 1990; 323: 236–241.
Ikonomidis I, Andreotti F, Economou E, Stefanadis C, Toutouzas P, Nihoyannopoulos P . Increased proinflammatory cytokines in patients with chronic stable angina and their reduction by aspirin. Circulation 1999; 100: 793–798.
Deliargyris EN, Raymond RJ, Theoharides TC, Boucher WS, Tate DA, Dehmer GJ . Sites of interleukin-6 release in patients with acute coronary syndromes and in patients with congestive heart failure. Am J Cardiol 2000; 86: 913–918.
Gavras H, Brown JJ, Lever AF, Macadam RF, Robertson JIS . Acute renal failure, tubular necrosis and myocardial infarction induced in the rabbit by intravenous angiotensin II. Lancet 1971; II: 19–22.
Schwartz F, Duka A, Duka I, Cui J, Gavras H . Novel targets of angiotensin II regulation in mouse heart identified by serial analysis of gene expression. Am J Physiol Hrt Circ Physiol 2004; 287: H1957–H1966.
Duka A, Schwartz F, Duka I, Johns C, Melista E, Gavras I, Gavras H . A novel Gene (Cmya3) induced in the heart by angiotensin II-dependent but not salt-dependent hypertension in mice. Am J Hypertens 2006; 19: 275–281.
McCalmon SA, Desjardins DM, Ahmad S, Davidoff KS, Mathew M, Kielbasa OM, Sato K, Ohashi K, Walsh K, Gavras H, Naya FJ . Modulation of AngiotensinII-mediated cardiac remodeling by the MEF2A target gene Xirp2. Circ Research 2010; 106: 952–960.
Ignjacev-Lazich I, Kintsurashvili E, Johns C, Vitseva O, Duka A, Shenouda S, Gavras I, Gavras H . Angiotensin-converting enzyme regulates bradykinin receptor gene expression. Am J Physiol Heart Circ Physiol 2005; 289: H1814–H1820.
Tschope C, Koch M, Spillmann F, Heringer-Walther S, Mochmann HC, Stauss H, Bader M, Unger T, Schultheiss HP, Walther T . Upregulation of the cardiac bradykinin B2 receptors after myocardial infarction. Immunopharmacology 1999; 44: 111–117.
Tschope C, Heringer-Walther S, Koch M, Spillmann F, Wendorf M, Leitner E, Schultheiss HP, Walther T . Upregulation of bradykinin B1-receptor expression after myocardial infarction. Br J Pharmacol 2000; 129: 1537–1538.
Duka A, Kintsurashvili E, Duka I, Ona D, Hopkins TA, Bader M, Gavras I, Gavras H . Angiotensin-converting enzyme inhibition after experimental myocardial infarct: role of the kinin B1 and B2 receptors. Hypertension 2008; 51: 1352–1357. 2008.
Zhao ZQ, Vinten-Johansen J . Postconditioning: reduction of reperfusion-induced injury. Cardiovasc Res 2006; 70: 200–211.
Yin H, Chao J, Bader M, Chao L . Differential role of kinin B1 and B2 receptors in ischemia-induced apoptosis and ventricular remodeling. Peptides 2007; 28: 1383–1389.
Xi L, Das A, Zhao ZQ, Merino VF, Bader M, Kukreja RC . Loss of myocardial ischemic postconditioning in adenosine A1 and bradykinin B2 receptors gene knockout mice. Circulation 2008; 118: S32–S37.
Heitsch H . The therapeutic potential of bradykinin B2 receptor agonists in the treatment of cardiovascular disease. Expert Opin Investig Drugs 2003; 12: 759–770.
Ito H, Hayashi I, Izumi T, Majima M . Bradykinin inhibits development of myocardial infarction through B2 receptor signalling by increment of regional blood flow around the ischaemic lesions in rats. Br J Pharmacol 2003; 138: 225–233.
Tschope C, Spillmann F, Altmann C, Koch M, Westermann D, Dhayat S, Bascands JL, Gera L, Hoffmann S, Schultheiss HP, Walthner T . The bradykinin B1 receptor contributes to the cardioprotective effects of AT1 blockage after experimental myocardial infarction. Cardiovasc Res 2004; 61: 559–569.
Ignjatovic T, Tan F, Brovkovych V, Skidgel RA, Erdos EG . Novel mode of action of angiotensin I converting enzyme inhibitors: direct activation of bradykinin B1 Receptor. J Biol Chem 2002; 227: 16847–16852.
Lucero HA, Kintsurashvili E, Marketou ME, Gavras H . Cell signaling, internalization and nuclear localization of the angiotensin converting enzyme in smooth muscle cells and endothelial cells. J Biol Chem 2010; 285: 5555–5568.
Rosenthal T, Gavras I . Angiotensin inhibition and malignancies: a review. J Hum Hypertens 2009; 23: 623–635.
Belanger S, Bovenzi V, Cote J, Neugebauer W, Amblard M, Martinez J, Lammek B, Savard M, Gobeil Jr F . Structure-activity relationships of novel peptide agonists of the human bradykinin B2 receptor. Peptides 2009; 30: 777–787.
Marketou M, Kintsurashvili E, Papanicolaou KN, Lucero HA, Gavras I, Gavras H . Cardioprotective effects of a selective B2 receptor agonist of bradykinin post acute myocardial infarct. Am J Hypertens 2010; 23: 562–568.
Lazar HL, Chipkin S, Philippides G, Bao Y, Apstein C . Glucose-insulin-potassium solutions improve outcomes in diabetics who have coronary artery operations. Ann Thorac Surg 2000; 70: 145–150.
Acknowledgements
This work was supported in part by NIH Grant R01 HL 58807.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Manolis, A., Marketou, M., Gavras, I. et al. Cardioprotective properties of bradykinin: role of the B2 receptor. Hypertens Res 33, 772–777 (2010). https://doi.org/10.1038/hr.2010.82
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.82
Keywords
This article is cited by
-
The Enigma of Prodromes in Hereditary Angioedema (HAE)
Clinical Reviews in Allergy & Immunology (2021)
-
Pharmacological Attenuation of Myocardial Reperfusion Injury in a Closed-Chest Porcine Model: a Systematic Review
Journal of Cardiovascular Translational Research (2014)