Abstract
This study compares relationships between each of morning home blood pressure (BP), evening home BP and office BP with electrocardiographic (ECG) abnormalities among treated hypertensive Japanese patients. We defined ECG left ventricular hypertrophy (LVH) as Sokolow–Lyon voltage and/or Cornell voltage duration product. Abnormal T waves and ST segment depression were categorized based on the Minnesota code. Office BP was calculated as the mean of four readings taken during two visits. Morning and evening home BP were calculated as the mean of five readings measured once each morning and evening for 5 days, respectively. Multivariate analysis showed that ECG-LVH in 747 hypertensives (mean age: 72 years; women: 63%) was more closely associated with morning home BP than with either office or evening home BP. Even the first reading of morning home BP on day 1 was significantly associated with ECG-LVH independently of office BP. The association between home BP and ECG-LVH increased with the cumulative number of home BP measurements. The results for abnormal T waves were similar. Home and office BP did not significantly differ between patients with and without ST segment depression. Morning home BP was more closely associated with ECG-LVH and abnormal T waves than either office or evening home BP among treated hypertensive Japanese patients.
Similar content being viewed by others
Introduction
Echocardiography can diagnose anatomical heart diseases such as left ventricular hypertrophy (LVH) more accurately than electrocardiography (ECG). However, heart disease is often diagnose by ECG before echocardiography, because the procedure is simple, widely accessible, inexpensive and echocardiography for obese and elderly patients can be difficult.1, 2 LVH is a powerful predictor of cardiovascular morbidity and mortality.3 Abnormal T waves and ST segment depression develop among patients with severe LVH that might be reflected in the ischemic heart.4 Some studies have shown that hypertension for several years is associated with the development of ECG abnormalities that in turn are related to a higher left ventricular mass among patients without ischemic heart disease.5, 6, 7, 8 These abnormalities are also associated with hypertension9, 10, 11 and a poor prognosis.3, 4, 12
Measuring blood pressure (BP) at home (home BP) allows the collection of multiple measurements under controlled conditions, and it is more reliable than conventional (office) BP measurements, because bias arising from both observer and regression dilution is avoided and the white-coat effect is eliminated.13, 14 Cross-sectional and a prospective cohort studies have found that home BP measurement has stronger power for predicting target organ damage, morbidity and mortality than office BP measurement.11, 15, 16, 17, 18, 19 Tsunoda et al. found that the degree of LVH determined by echocardiography was more closely associated with home than with office BP values among 209 hypertensive Japanese patients.15 However, the relationship between home BP and LVH determined by ECG among treated patients in Japan is unclear. Niiranen et al. reported that the mean of morning and evening home BP measurements is more closely associated with LVH determined by ECG than by office BP among the general population in Finland.11 However, they assessed their findings using univariate analysis and did not consider confounding factors such as patients’ characteristics or drug information.11, 15
This study uses multivariate analysis to compare relationships between each of morning home, evening home and office BP with LVH, abnormal T waves and ST segment depression determined by ECG among treated hypertensive Japanese patients.
Methods
Patients
We examined data from patients who had enrolled in the Japan Home versus Office Blood Pressure Measurement Evaluation in the Elderly (J-HOME-Elderly) study that investigated the influence of proper control of home BP on cardiovascular events and mortality among elderly hypertensive Japanese patients undergoing antihypertensive treatment other than Ca-channel blockers. Eligibility for this study comprised men or women aged ⩾60 years who were diagnosed with hypertension by a physician and treated with antihypertensive drugs other than Ca-channel blockers. During December 2004, 8371 physicians randomly selected from all over Japan were invited to participate in this project. Of the 1553 who agreed to participate, 334 collected data for the study. By the end of November 2005, 1215 patients who provided written, informed consent to participate were enrolled in the study. Fifty-two patients who were < 60 years were excluded and 57 others were excluded as they had not received any antihypertensive treatment or had been treated with Ca-channel blockers. Another 15 were excluded because insufficient data about their BP values or their characteristics were provided. Therefore, population in the J-HOME-Elderly study was consisted of 1091 patients. In this analysis seventy-four patients with a history of ischemic heart disease, 24 with arrhythmia (including 4 treated with anti-arrhythmic agents), 4 with valvular disease and 4 treated with digitalis were further excluded, because these conditions might affect the wave on electrocardiograms. Of the remaining 985 patients, ECG data were accessible for 794 of them. Forty-five patients with left and right bundle branch block and two with pacemakers were also excluded. Thus, this study population comprised 747 patients. The characteristics of patients did not significantly differ between those included and excluded except for the proportion of heart diseases used as exclusion criteria (Table 1).
Home BP measurements
The patients recorded home BP measured once every morning while seated, within 1 h of waking and after 1–2 min of rest but before ingesting medications and breakfast, and once every evening just before bedtime for a period 5 days according to Japanese guidelines.14 Participating doctors distributed instructions regarding methods of measuring home BP to all of the patients before starting the study. We asked the doctors to provide data only from those patients who followed these instructions. Cuff oscillometry was applied using electronic upper arm-cuff devices. The Ministry of Health, Labour and Welfare, Japan has validated and approved all such devices in Japan.20 The actual models were not described by the doctors who participated in the study, but all devices used to measure BP were certified as conforming to the Association for the Advancement of Medical Instrumentation (AAMI) standards.21 The mean of all measurements recorded over the 5-day period was calculated for each patient and subsequently analyzed.
Office BP measurements
The BP values of the patients were consecutively measured twice while seated and after resting for 1–2 min during regular attendance at the participating institutions. Physicians (63.4%) or nurses (36.6%) used the auscultation method with a mercury (50.3%) or aneroid (4.9%) sphygmomanometer, or the cuff-oscillometric method with electronic arm-cuff devices (44.8%). The mean of four measurements at two clinic visits during the period of home measurements was defined as the office BP value for each patient and included in the analysis.
Electrocardiography
We collected copies of ECG data. Four technicians measured the QRS duration and amplitudes, which were then verified by an independent technician. We defined ECG-LVH as follows: Cornell voltage duration product ((RaVL+SV3) × QRS duration, in men; (RaVL+SV3+6) × QRS duration, in women) ⩾2440 mm × ms,22 or Sokolow–Lyon voltage (SV1+RV5/6) ⩾35 mm.23 Abnormal T waves and ST segment depression were categorized based on Minnesota Codes. Abnormal T waves were categorized based on Minnesota Codes 5-1-3 (Code 5-1, T amplitude negative ⩾5.0 mm in any of leads I, II, V1–V6 and aVL when R amplitude is ⩾5 mm, or aVF when QRS is mainly upright; code 5-2, T amplitude negative or diphasic (positive-negative or negative-positive type) with negative phase at least 1.0 mm but not as deep as 5.0 mm in any of leads I, II, V1–V6 and aVL when R amplitude is ⩾5 mm, or aVF when QRS is mainly upright; code 5-3, T amplitude zero (flat), or negative or diphasic (negative-positive type only) with <1.0 mm negative phase in lead I, II, V3–V6 and aVL when R amplitude is ⩾5 mm).24 ST segment depression was categorized based on Minnesota Codes 4-1-3 (Code 4-1, STJ depression ⩾1.0 mm and ST segment horizontal or downward sloping in any of leads I, II, V1–V6 and aVL or aVF; code 4-2, STJ depression ⩾0.5 mm and less than 1.0 mm and ST segment horizontal or downward sloping in any of leads I, II, V1–V6, aVL or aVF; code 4-3, no STJ depression as much as 0.5 mm, but ST segment downward sloping and a segment or T-wave nadir of ⩾0.5 mm below P-R baseline in any of leads I, II, V2–V6 or aVL).24 We also evaluated ECG strain, which was defined as the presence of typical strain when a downsloping convex ST segment with an inverted asymmetrical T wave with polarity opposite the QRS axis was present in leads V5 or V6.25
Data collection and statistical analysis
Information about patients’ characteristics and drug regimens were collected by a questionnaire administered by the attending physicians. Variables were compared using Student’s t-test, the χ2-test or logistic regression analysis as appropriate. In multivariate analysis, the model was adjusted for variables that were associated in the univariate analysis. If the model included evening home BP, it was additionally adjusted for ‘before’ or ‘after’ consuming alcoholic beverages and bathing because evening home BP was obviously affected by such activities in the evening.26, 27 Data are shown as mean±standard deviation (s.d.). A P-value of <0.05 was considered statistically significant. All data were statistically analyzed using the SAS package (version 9.1; SAS Institute, Cary, NC, USA).
Results
Patients’ characteristics
The mean values for morning and evening home, and mean office systolic BP (SBP)/diastolic BP (DBP) were 134.0±14.1/78.0±9.4, 127.3±13.8/72.8±8.7 and 138.0±15.3/77.4±9.0 mm Hg, respectively, among the 827 patients (mean age: 71.5±6.5 years; women 63.0%). LVH, abnormal T waves and ST segment depression were identified in 15.5, 18.9 and 5.8% of the patients, respectively (Table 1).
ECG-LVH
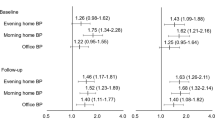
Values for morning home SBP and DBP, and office SBP were higher among patients with ECG-LVH than those without ECG-LVH. Patients with ECG-LVH had a lower body mass index (BMI) and were less likely to be obese (BMI ⩾25 kg m−2) (Table 2). Multivariate logistic regression analysis showed that ECG-LVH was more closely associated with values for morning home BP than with those for office or evening home BP (Table 3).
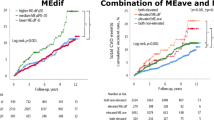
The association between ECG-LVH and the cumulative number of home BP measurements is shown in Figure 1. Morning home SBP values on day 1 were associated with ECG-LVH, independently of office SBP. The association between ECG-LVH and morning home SBP slightly increased with the cumulative number of morning home BP measurements, but the trend was not statistically significant. Conversely, the association between ECG-LVH and evening home SBP significantly increased with the cumulative number of evening home BP measurements. The trends for DBP were similar.
Adjusted ORs (95% CI) for LVH (present, 1; absent, 0) associated with cumulative home BP measurements. Models were adjusted for body mass index, office HR and office BP. If models included evening home BP, data were further adjusted for BP measurements before or after bathing and before or after consuming alcohol. OR, odds ratio; CI, confidence interval; LVH, left ventricular hypertrophy; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure.
Abnormal T waves
Morning home, evening home and office BP values were higher among patients with abnormal T waves than those without abnormal T waves. Patients with abnormal T waves were also older, more likely to have a history of ischemic heart disease and less likely to take antihypertensive drugs in the evening (Table 2). Multivariate logistic regression analysis showed that morning and evening home BP values were significantly and more closely associated with abnormal T waves than with office BP values. Morning home SBP values were also significantly and more closely associated with abnormal T waves than evening home SBP values (Table 3).
Both morning home SBP and DBP values on day 1 were associated with abnormal T waves independently of office BP. The association between abnormal T waves and morning home BP significantly increased with the cumulative number of morning home BP measurements. The trend for evening home BP was similar (Figure 2).
Adjusted ORs (95% CI) for abnormal T waves (present, 1; absent, 0) associated with cumulative home BP measurements. Models were adjusted for age, timing of taking medication in the evening and office BP. If models included evening home BP, data were further adjusted for BP measurements before or after bathing, and before or after consuming alcohol. OR, odds ratio; CI, confidence interval; SBP, systolic blood pressure; DBP, diastolic blood pressure.
ST segment depression
Morning home and office SBP values tended to be higher among patients with ST segment depression, than those without ST segment depression, although the differences did not reach significance (Table 2). Patients with ST segment depression were less likely to consume alcohol and more likely to take antihypertensive drugs in the morning.
ECG strain
Only 19 (2.5%) patients had ECG strain and they also had higher morning and evening home SBP in univariate analysis. Multivariate analysis showed that evening home SBP and morning home DBP were significantly associated with ECG strain, independently of office BP (data not shown).
Discussion
This study found that morning home BP was more closely associated with ECG-LVH and abnormal T waves than office BP. Others have shown that target organ damage due to hypertension is more closely associated with home than with office BP.11, 15, 16, 17, 18, 19 Home BP is usually measured under highly controlled conditions compared to office BP. Home BP was measured in this study according to Japanese guidelines,14 which generates highly reproducible and reliable BP information. This is because the white-coat effect is eliminated and regression dilution bias, observer bias and environmental influences are excluded, which is difficult to achieve in the clinic or office setting. We postulate that these characteristics of home BP measurements explain the closer association between ECG abnormalities and home BP than with office BP. Only 2.5% of patients in this study had ECG strain. Therefore, further study is needed to evaluate the association of home BP values with ECG strain.
We found that the association between home BP and ECG-LVH or abnormal T waves increased with the cumulative number of BP measurements, indicating that the association between home BP and ECG abnormalities partly depends upon the number of measurements. Others have also reported similar results.11, 17 Although Niiranen et al.11 reported that the correlation between the mean of morning and evening home BPs and ECG-LVH increases slightly with the number of home BP measurements, they did not assess the relationship between ECG-LVH and individual morning and evening home BP values. We found that morning home SBP on day 1, but not evening home SBP, was closely associated with ECG-LVH and abnormal T waves independently of office SBP, even for fewer home BP measurements. The Ohasama study found that even the first morning and evening home BP values were more powerful predictors of stroke than the mean of two office BP values.28 The advantages of home BP might be due to the stability of the measurement environment.
Morning home BP was independently and more closely associated with ECG-LVH and abnormal T waves than evening home BP in this study. Kawabe and Saito26 reported that BP is significantly lower when measured after than before bathing, and that evening home BP is lower when measured after compared to before consuming alcohol.27 Therefore, the recent guidelines of the Japanese Society of Hypertension recommend that the effects of bathing and consuming alcohol should be considered when evaluating evening home BP,14 but, even after such adjustment, ECG abnormalities were still more closely associated with morning than with evening home BP. Measurement conditions and other factors such as physical activity during the daytime might have more influence on evening than morning home BP. We found that morning home BP was associated with ECG abnormalities independently of office and evening home BP, which might arise because patients with ECG abnormalities could not control their BP over a 24-h period, especially in the morning. We suspected that patients with uncontrolled morning hypertension under antihypertensive therapy had masked hypertension associated with hypertensive target organ damage.29, 30 Therefore, our findings indicate that morning home BP reflects the risk of cardiovascular events more accurately than either office or evening home BP in hypertensive patients undergoing appropriate treatment.
The limitations of this study are as follows. First, the patients in this study were taking antihypertensive medication other than Ca-channel blockers and some patients without ECG data had a higher BP, indicating some potential selection bias. Second, home BP measurements were not externally controlled, so compliance with the rules of home BP measurements was uncertain. However, the patients received instructions regarding methods of home BP measurements from participating doctors before starting the study. Therefore, the conditions of home BP measurements might be quite stable. We adjusted the multivariate analysis for evening bathing and the consumption of alcoholic beverages in the evening. Kawabe et al.27 showed that a depressor effect of nighttime bathing persists for 60 min thereafter. Furthermore, although the effects of alcohol differ according to the amount consumed,31 we could not adjust either the amount of consumed alcoholic beverages or the interval after bathing, because data about these parameters were not collected. Evening home BP might also be affected by the time and composition of evening meals. However, we simply asked the patients to measure evening home BP immediately before going to bed according to the Japanese guidelines,32 and we did not collect data about the time and composition of evening meals. Therefore, the adjustment might be insufficient. Third, office BP was measured after 1–2 min of rest, which was shorter than the period recommended in the guidelines.14 Therefore, office BP might be inaccurate. However, because this study was based on the environment of daily practice, these results might represent the reality of the daily clinical setting in Japan.
This study showed that morning home BP was independently and more closely associated with ECG-LVH and abnormal T waves than either office BP or evening BP among elderly Japanese patients undergoing antihypertensive treatment. Further prospective studies are required to assess whether home BP predicts the regression of these ECG abnormalities.
References
Levy D, Anderson KM, Savage DD, Kannel WB, Christiansen JC, Castelli WP . Echocardiographically detected left ventricular hypertrophy: prevalence risk factors the Framingham heart study. Ann Intern Med 1988; 108: 7–13.
Gardin JM, Siscovick D, Anton-Culver H, Lynch JC, Smith VE, Klopfenstein HS, Bommer WJ, Fried L, O’Leary D, Manolio TA . Sex age disease affect echocardiographic left ventricular mass systolic function in the free-living elderly the cardiovascular health study. Circulation 1995; 91: 1739–1748.
Ishikawa J, Ishikawa S, Kabutoya T, Gotoh T, Kayaba K, Schwartz JE, Pickering TG, Shimada K, Kario K, Jichi Medical School Cohort Study Investigators Group. Cornell product left ventricular hypertrophy in electrocardiogram and the risk of stroke in a general population. Hypertension 2009; 53: 28–34.
Thiry PS, Rosenberg RM, Abbott JA . A mechanism for the electrocardiogram response to left ventricular hypertrophy and acute ischemia. Circ Res 1975; 36: 92–104.
Mancia G, Bombelli M, Facchetti R, Madotto F, Corrao G, Trevano FQ, Giannattasio C, Grassi G, Sega R . Long-term risk of diabetes, hypertension and left ventricular hypertrophy associated with the metabolic syndrome in a general population. J Hypertens 2008; 26: 1602–1611.
Kawamura T, Yamamoto R, Wakai K, Ichihara Y, Mizuno Y, Kojima M, Aoki R, Tamakoshi A, Ohno Y . Newly developed ST-T abnormalities on the electrocardiogram and chronologic changes in cardiovascular risk factors. Am J Cardiol 1996; 77: 823–827.
Ichihara Y, Sugino M, Hattori R, Anno T, Mizuno Y, Yokoi M, Kondo T, Hirai M, Kawamura T . Relation of electrocardiographic left ventricular hypertrophy with and without T-wave changes to systemic blood pressure, body mass, and serum lipids and blood glucose levels in Japanese men. Am J Cardiol 1997; 80: 730–735.
Okin PM, Devereux RB, Fabsitz RR, Lee ET, Galloway JM, Howard BV, Strong Heart Study. Quantitative assessment of electrocardiographic strain predicts increased left ventricular mass: the strong heart study. J Am Coll Cardiol 2002; 40: 1395–1400.
De Bacquer D, Martins Pereira LS, De Backer G, De Henauw S, Kornitzer M . Prevalences and correlates of ECG abnormalities in the adult Belgian population. J Electrocardiol 1995; 28: 1–11.
Okin PM, Devereux RB, Jern S, Kjeldsen SE, Julius S, Dahlof B . Baseline characteristics in relation to electrocardiographic left ventricular hypertrophy in hypertensive patients: the Losartan intervention for endpoint reduction (LIFE) in hypertension study. The Life Study Investigators. Hypertension 2000; 36: 766–773.
Niiranen TJ, Jula AM, Kantola IM, Karanko H, Reunanen A . Home-measured blood pressure is more strongly associated with electrocardiographic left ventricular hypertrophy than is clinic blood pressure: the Finn-HOME study. J Hum Hypertens 2007; 21: 788–794.
De Bacquer D, De Backer G, Kornitzer M, Blackburn H . Prognostic value of ECG findings for total, cardiovascular disease, and coronary heart disease death in men and women. Heart 1998; 80: 570–577.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Bertomeu V, Clement D, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O’Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B . 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H . Japanese Society of Hypertension Committee: Japanese Society of Hypertension guidelines for the management of hypertension (JSH2009). Hypertens Res 2009; 32: 1–107.
Tsunoda S, Kawano Y, Horio T, Okuda N, Takishita S . Relationship between home blood pressure and longitudinal changes in target organ damage in treated hypertensive patients. Hypertens Res 2002; 25: 167–173.
Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM . Cardiovascular prognosis of ‘masked hypertension’ detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA 2004; 291: 1342–1349.
Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, Hashimoto J, Totsune K, Satoh H, Imai Y . How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens 2004; 22: 1099–1104.
Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, Mancia G . Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation 2005; 111: 1777–1783.
Stergiou GS, Argyraki KK, Moyssakis I, Mastorantonakis SE, Achimastos AD, Karamanos VG, Roussias LG . Home blood pressure is as reliable as ambulatory blood pressure in predicting target-organ damage in hypertension. Am J Hypertens 2007; 20: 616–621.
Shirasaki O, Terada H, Niwano K, Nakanishi T, Kanai M, Miyawaki Y, Souma T, Tanaka T, Kusunoki T . The Japan home-health apparatus industrial association: investigation of home-use electronic sphygmomanometers. Blood Press Monit 2001; 6: 303–307.
Association for the Advancement of Medical Instrumentation: American National Standard for Electronic or Automated Sphygmomanometers. AAMI Analysis and Review: Washington, DC, 1987.
Casale PN, Devereux RB, Kligfield P, Eisenberg RR, Miller DH, Chaudhary BS, Phillips MC . Electrocardiographic detection of left ventricular hypertrophy: development and prospective validation of improved criteria. J Am Coll Cardiol 1985; 6: 572–580.
Sokolow M, Lyon TP . The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 1949; 37: 161–186.
Blackburn H, Keys A, Simonson E, Rautaharju P, Punsar S . The electrocardiogram in population studies. A classification system. Circulation 1960; 21: 1160–1175.
Okin PM, Oikarinen L, Viitasalo M, Toivonen L, Kjeldsen SE, Nieminen MS, Edelman JM, Dahlöf B, Devereux RB . LIFE Study investigators prognostic value of changes in the electrocardiographic strain pattern during antihypertensive treatment: the Losartan intervention for end-point reduction in hypertension study (LIFE). Circulation 2009; 119: 1883–1891.
Kawabe H, Saito I . Influence of nighttime bathing on evening home blood pressure measurements: how long should the interval be after bathing? Hypertens Res 2006; 29: 129–133.
Kawabe H, Saito I, Saruta T . Effects of nighttime alcohol intake on evening and next morning home blood pressure in Japanese normotensives. Clin Exp Hypertens 2007; 29: 43–49.
Asayama K, Ohkubo T, Hara A, Hirose T, Yasui D, Obara T, Metoki H, Inoue R, Kikuya M, Totsune K, Hoshi H, Satoh H, Imai Y . Repeated evening home blood pressure measurement improves prognostic significance for stroke: a 12-year follow-up of the Ohasama study. Blood Press Monit 2009; 14: 93–98.
Hara A, Ohkubo T, Kikuya M, Shintani Y, Obara T, Metoki H, Inoue R, Asayama K, Hashimoto T, Harasawa T, Aono Y, Otani H, Tanaka K, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y . Detection of carotid atherosclerosis in individuals with masked hypertension and white-coat hypertension by self-measured blood pressure at home: the Ohasama study. J Hypertens 2007; 25: 321–327.
Hara A, Ohkubo T, Kondo T, Kikuya M, Aono Y, Hanawa S, Shioda K, Miyamoto S, Obara T, Metoki H, Inoue R, Asayama K, Hirose T, Totsune K, Hoshi H, Izumi S, Satoh H, Imai Y . Detection of silent cerebrovascular lesions in individuals with ‘masked’ and ‘white-coat’ hypertension by home blood pressure measurement: the Ohasama study. J Hypertens 2009; 27: 1049–1055.
Nakashita M, Ohkubo T, Hara A, Metoki H, Kikuya M, Hirose T, Tsubota-Utsugi M, Asayama K, Inoue R, Kanno A, Obara T, Hoshi H, Totsune K, Satoh H, Imai Y . Influence of alcohol intake on circadian blood pressure variation in Japanese men: the Ohasama study. Am J Hypertens 2009; 22: 1171–1176.
Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, Miyakawa M, Fukiyama K, Japanese Society of Hypertension. Japanese society of hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res 2003; 26: 771–782.
Acknowledgements
This work was supported by Grants for Scientific Research (Nos. 1854042 and 207477) from the Ministry of Education, Culture, Sports, Science and Technology, by Junkanki-Byou-Itaku-Kenkyuhi (H19-Kou-8) from the National Cardiovascular Center, and by Nouvelle Place Inc., Japan.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
The study was designed and conducted, and will be interpreted by the investigators independently of sponsors. This study was conducted by the J-HOME-Elderly Study Group.
Members of the J-HOME-Elderly Study Group
Management committee: Yutaka Imai (Principal investigator), Takayoshi Ohkubo, Taku Obara, Masahiro Kikuya, Kei Asayama, Hirohito Metoki and Kazuhito Totsune.
Coordinating and data management committee: Taku Obara, Taku Shibamiya, Takahiro Shinki, Urara Ikeda, Makoto Yoshida and Kazuki Ishikura.
Participating practitioners: (Hokkaido) H Fujii, N. Miura, T. Sasanami, I Takagi, Y Takagi. (Aomori) M Fukushi. (Iwate) Y Kawamorita, T Yoshida. (Miyagi) K Asayama, K Ito, S Kataoka, K Matsuo, H Metoki, Y Otake, S Sasaki, S Sato, Y Shishido, Y Tanno, H Unakami. (Akita) H Kimura, N Sakusabe, T Wada. (Yamagata) S Nagai. (Fukushima) K Hangai, K Machii, Y Miyazaki, T Sato, T Yabuki. (Ibaraki) M Inoue, M Noritake, M Seki, Y Shimada, K Yasui. (Tochigi) T Noshiro, T Owada. (Gunma) S Aoki, J Hoshino, T Kobayashi, T Koitabashi, M Nakano, I Naruse. (Saitama) H Aoki, K Hayashida, K Kogure, Y Nashida, A Nitta, H Saito, T Sugiura, N Yagi. (Chiba) S Kato, Y Kodama, G Kudo, T Sakai, N Sekiya, K Suzuki, K Yamauchi. (Tokyo) M Akaike, T Arai, T Arino, J Asakawa, K Fukuda, K Hashimoto, S Hayashi, M Hojo, H Ichiba, T Irie, K Iseki, S Kukidome, K Kuwaki, M Miyazaki, H Mizotani, S Nakajima, T Noda, K Obayashi, K Oguchi, K Oh, H Okazaki, N Serizawa, H Takano, T Teruya, M Uchiyama, S Yatagai, S Yokoyama, F Yukawa. (Kanagawa) M Hasegawa, E Imai, K Minamisawa, M Miyake, M Miyamoto, F Nonaka, K Toyoda, M Ushiyama, H Yamamoto. (Yamanashi) M Nagasaka. (Nagano) N Kojima, M Shimotori, F Soga, K Uchiba. (Niigata) K Fujita, N Furukawa, A Katagiri, T Kobayashi, K Kurokawa, Y Nakayama, S Takahashi, S Takahashi, S Takahashi, S Takano, K Uchiyama, Y Yamaguchi, K Yonekura. (Toyama) T Takahashi. (Ishikawa) N Oya. (Fukui) T Fujita, Y Koshino. (Gifu) K Aoyama, Y Baba, H Kobayashi, K Takai, R Tanaka. (Shizuoka) S Goto, M Hayakawa, A Ishida, T Ishii, T Mikami, S Nakamura, K Sano, Y Takahira, K Tamakoshi. (Aichi) Y Fujii, A Koyama, Y Koyama, T Mokuno, J Shirai, Y Tanaka, H Tatsura, E Yamada. (Mie) K Amano, T Asakawa, M Kusagawa, A Ochi, T Tanaka, Y Uchida. (Shiga) Y Kondo, T Okuda. (Kyoto) T Isaji, Y Katsuma, Y Kawanishi, S Kikkawa, Y Okada, K Sokai, K Takeshita. (Osaka) H Hashimura, R Izutani, T Kashiwai, N Kitagawa, T Kitagawa, Y Kubota, M Miyataka, J Nakamura, K Tamai, N Tsuji, J Ueno, T Uenoyama, Y Yoshida. (Hyogo) T Okano, H Oya. (Nara) H Hagihara, H Suzuki, Y Takeda, N Taketani. (Wakayama) N Hirabayashi, S Kushi. (Shimane) K Kodama, H Minami, T Sasaki, K Yamada, H Yashige. (Okayama) J Hayashi, Y Niitsu, K Osada, F Otsuka, R Sato, K Shiraga, K Shirahige, T Yoshimoto. (Hiroshima) K Kishizuchi, J Oiwa, J Oku, F Okuno, T Onaka, N Sasaki, S Sasaki, H Sugihara, T Sunahori, M Tanabe, K Watanabe, A Yamamoto, Y Yamashina, H Yoshimoto. (Yamaguchi) K Harada, Y Harada, K Iwasaki, T Kishida, O Koutoku, A Matsui, T Noda, T Okatani. (Tokushima) M Ono, S Ueta. (Kagawa) T Fukui, M Hattori, S Miyazaki, T Nakatsu. (Ehime) H Kadota, Y Kaneto, H Miyoshi, K Nakayama, K Yoshida. (Kochi) T Nakayama. (Fukuoka) N Fujino, T Hayakawa, K Hayashi, J Hirano, M Kikuchi, S Mori, K Nagasawa, Y Urabe, K Utsunomiya. (Saga) S Mitsuoka. (Nagasaki) T Mori. (Kumamoto) H Noda. (Oita) H Ikemoto, K Okita, O Yoshiga. (Miyazaki) T Aoki, Y Endo, H Nakao. (Kagoshima) K Arimura, A Kano. (Okinawa) Y Nakamura.
Rights and permissions
About this article
Cite this article
Shibamiya, T., Obara, T., Ohkubo, T. et al. Electrocardiographic abnormalities and home blood pressure in treated elderly hypertensive patients: Japan home versus office blood pressure measurement evaluation in the elderly (J-HOME-Elderly) study. Hypertens Res 33, 670–677 (2010). https://doi.org/10.1038/hr.2010.55
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.55
Keywords
This article is cited by
-
Left ventricular hypertrophy by electrocardiogram as a predictor of success in home blood pressure control: HOMED-BP study
Hypertension Research (2017)
-
Clinical significance of home blood pressure and its possible practical application
Clinical and Experimental Nephrology (2014)
-
The Japanese Society of Hypertension Guidelines for Self-monitoring of Blood Pressure at Home (Second Edition)
Hypertension Research (2012)