Abstract
Thrombin has a crucial role in cardiac remodeling through protease-activated receptor-1 activation in cardiac fibroblasts and cardiomyocytes. As heparin cofactor II (HCII) inhibits the action of tissue thrombin in the cardiovascular system, it is possible that HCII counteracts the development of cardiac remodeling. We investigated the relationships between plasma HCII activity and surrogate markers of cardiac geometry, including left atrial volume index (LAVI), relative wall thickness (RWT) and left ventricular mass index, and deceleration time (DcT) and the ratio of peak E velocity to early diastolic mitral annulus velocity (E/e' ratio) as surrogate markers of left ventricular diastolic dysfunction measured using echocardiography in 304 Japanese elderly individuals without systolic heart failure (169 men and 135 women; mean age: 65.4±11.8 years). Mean plasma HCII activity in all participants was 95.8±17.0% and there was no difference between the mean plasma HCII activities in males and females. Multiple regression analysis revealed that there were significant inverse relationships between plasma HCII activity and LAVI (coefficient: −0.2302, P<0.001), between HCII activity and RWT (coefficient: −0.0007, P<0.05), between HCII activity and DcT (coefficient: −0.5189, P<0.05) and between HCII activity and E/e' ratio (coefficient: −0.0558, P<0.01). Plasma HCII activity was independently and inversely associated with the development of cardiac remodeling, including cardiac concentric change, left atrial enlargement and left ventricular diastolic dysfunction. These findings suggest that cardiac tissue thrombin inactivation by HCII is a novel therapeutic target for cardiac remodeling and atherosclerosis.
Similar content being viewed by others
Introduction
Thrombin acts as a pivotal enzyme for generating fibrin clots and activates platelets, vascular endothelial cells, vascular smooth muscle cells, macrophages and fibroblasts to enhance procoagulation,1 chemoattraction,2 mitogenesis3 and proliferation4 of these cells. Thrombin exerts its physiological and pathological actions in these cells through the proteolytic processing of specific cell-surface receptors known as protease-activated receptors (PARs).5, 6 Nelken et al.7 demonstrated that PAR-1 was widely expressed in regions where macrophages, cardiomyocytes, cardiac fibroblasts, vascular smooth muscle cells and mesenchymal-appearing intimal cells are abundantly present. Thus, excessive PAR-1 activation promotes cardiovascular disorders, including cardiac remodeling, arterial thrombosis and atherosclerosis. From the point of view of PAR-1 modulation in cardiovascular remodeling, the use of antithrombin agents and antagonists of the thrombin receptor might be useful approaches for the treatment and prevention of these disorders. Antithrombin (AT), a major serine protease inhibitor (serpin), inhibits thrombin action at the intravascular lumen and it exerts its optimal AT actions by binding to heparan sulfate and heparan sulfate proteoglycans on the luminal surface of endothelial cells. In addition, heparin cofactor II (HCII), which is also a serpin, is a plasma glycoprotein with a molecular weight of 65.6 kDa that is synthesized by the liver and circulates in plasma at a concentration of 1.0 μmol l−1. HCII potently inhibits thrombin action by forming a bimolecular complex with dermatan sulfate proteoglycans under the endothelial layer in mammalians.8, 9 Although AT inhibits not only the thrombin action, but also the actions of several proteases involved in blood coagulation or fibrinolysis, HCII only inactivates thrombin and has no inhibitory effect on the action of any other proteases. As HCII can counteract the actions of thrombin at injured vascular walls, we, and others, have investigated and confirmed the protective role of HCII against atherosclerosis in clinical examinations and studies using HCII-deficient mice.9, 10, 11, 12, 13, 14, 15
As the development of vascular remodeling, including atherosclerosis, has been shown to be closely associated with cardiac remodeling in humans and experimental animal models, we hypothesized that HCII is involved in the process of not only atherosclerosis, but also cardiac remodeling. In order to clarify this issue, we investigated the relationships between plasma HCII activity and surrogate markers with respect to cardiac remodeling in elderly subjects with cardiovascular risk factors. We found that plasma HCII activity is inversely associated with cardiac remodeling in subjects without systolic heart failure (HF).
Methods
Subjects for cross-sectional study
We consecutively recruited 304 Japanese subjects (169 males and 135 females) who were outpatients with lifestyle-related diseases and subjects older than 35 years of age were recruited consecutively from the Department of Medicine and Bioregulatory Sciences and Department of Cardiovascular Medicine at Tokushima University Hospital, Tokushima, Japan between April 2007 and September 2009. All subjects underwent a standardized interview and a physical examination. Current smokers were defined as subjects who had smoked within the past year. Body mass index was calculated as an index of obesity. Blood pressure was measured twice and averaged. Hypertensive patients were defined as those with systolic blood pressure (SBP) ⩾140 mm Hg and/or diastolic blood pressure (DBP) ⩾90 mm Hg or those receiving antihypertensive agents. Pulse pressure was calculated as SBP−DBP. Patients who were diagnosed with white coat hypertension were not categorized as having hypertension. Hyperlipidemic patients were defined as those with low-density lipoprotein cholesterol ⩾140 mg −1dl and/or triglyceride level ⩾150 mg dl−1 or those receiving lipid-lowering agents. Patients were classified as diabetics by their use of insulin and/or oral hypoglycemic agents or by glycosylated hemoglobin A1c (HbA1c) >6.5%. In this study, the criteria for cardiovascular risk factor(s) included current smoking, hypertension, hyperlipidemia and diabetes mellitus. The exclusion criteria included subjects with overt left ventricular systolic dysfunction (ejection fraction <50%), history of previous episodes of congestive HF, moderate to severe valvular disease and atrial fibrillation, known malignancy, renal failure, liver dysfunction and malnutrition. Our study followed the institutional guidelines of the University of Tokushima and was approved by the Institutional Review Board. Prior informed consent was obtained from all patients according to the Declaration of Helsinki.
Biochemical analyses
Before noon, overnight fasting blood samples were collected from the antecubital vein and were assayed immediately for HbA1c and serum lipid parameters, including low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and triglyceride level. Serum levels of low-density lipoprotein cholesterol, high-density lipoprotein cholesterol and triglyceride level were measured using the enzymatic method. HbA1c was measured using high-performance liquid chromatography.
Measurements of plasma HCII and AT activities
Blood was drawn as described above, collected into a tube containing 1/10 volume of 3.8% sodium citrate and centrifuged at 2000 × g for 20 min. Plasma was stored at −80 °C until use. Plasma HCII and AT activities were measured as previously described.16
Echocardiography
The ultrasound instrument used in this study was a Toshiba Aplio 80 with a 2.5-MHz transducer (Toshiba Medical Corporation, Tokyo, Japan). Left atrial size was quantified as left atrial volume (LAV) because LAV is a more accurate estimate of left atrial size than M-mode or 2D left atrial diameters and is a better predictor of cardiovascular events.17, 18, 19 Left atrial (LA) dimensions were measured in three orthogonal planes: parasternal long axis, lateral and superoinferior (Figure 1).20 Those dimensions were recorded at the end phase of ventricular systole. As suggested by current guidelines,19 LAV was calculated by using the length diameter ellipsoid method computed at ventricular end-systole by the following equation: V=4π/3 × (parasternal long axis/2) × (lateral/2) × (superoinferior/2). Finally, left atrial volume index (LAVI) was indexed by body surface area. Left ventricular mass index (LVMI) was estimated using Devereux formula21 and was calculated as an index of body surface area. Relative wall thickness (RWT) was calculated as (septal wall thickness+posterior wall thickness in the end-diastolic phase)/(left ventricular end−diastolic diameter). Doppler echocardiographic assessment, including measurements of peak velocities of E and A waves and deceleration time (DcT), was carried out in all patients who underwent tissue Doppler imaging. Spectral pulsed wave Doppler tissue interrogation of longitudinal mitral annular velocity was recorded throughout the cardiac cycle at the septal annulus in the apical four-chamber view. The ratio of peak E velocity to early diastolic mitral annulus velocity (E/e' ratio) was calculated. Other routine echocardiographic examinations, including measurements of left ventricular fractional shortening (FS%) and ejection fraction, were also performed.
Representative images of measurement of LAV. PLAX was taken in the parasternal long-axis view. The LAT and SI dimensions were both taken from the apical four-chamber view using the inner edge-to-inner edge measurement. LAV was calculated by using the length diameter ellipsoid method, applying the following equation: V=4π/3 × (PLAX/2) × (LAT/2) × (SI/2). LAV, left atrial volume, PLAX, parasternal long axis, LAT, lateral, SI, superoinferior.
Statistical analysis
Statistical analyses were performed using the StatView statistical package (StatView 5.0; SAS Institute, Japan Ltd., Tokyo, Japan). Continuous variables were averaged and values were expressed as the mean±s.d. or as a percentage for categorical parameters. Male gender and the presence of hypertension, diabetes mellitus, hyperlipidemia and current smoking status were coded as dummy variables. The degrees of association between independent variables including sex, age, body mass index, SBP, serum lipid parameters, HbA1c, plasma AT and HCII activities, history of current smoking, hypertension, diabetes mellitus and hyperlipidemia were determined by means of multiple regression analysis.
Results
Characteristics of subjects
The physical and laboratory characteristics of the subjects enrolled in this study are shown in Table 1. The high-density lipoprotein cholesterol levels and plasma AT activity were higher in females than in males. On the other hand, males showed higher levels of serum creatinine and more were current smokers. The mean plasma HCII activity in all of the participants was 95.8±17.0% and there was no difference between the mean plasma HCII activity in males and females. In addition, there were no significant gender differences in the age and body mass index, SBP, pulse pressure, low-density lipoprotein cholesterol, triglyceride level and HbA1c values. No significant gender differences were observed between the prevalences of hypertension, diabetes mellitus and hyperlipidemia and the use of medications for cardiovascular treatment in males and females.
Echocardiographic measurements
Table 1 also shows the results of the echocardiographic examinations. Although the left atrial dimension index (LADI) in females was significantly larger than that in males, there was no statistically significant gender difference in LAVI. Males manifested higher LVMI values than females. In contrast, the left ventricular systolic functions indicated by FS% and ejection fraction were both slightly higher in females than in males. Although there was no gender difference in the value of E/A, DcT and E/e' ratio were significantly larger in females than in males.
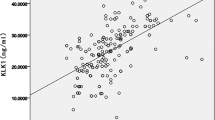
HCII is an independent and negative determinant of left atrial size
Age and sex-adjusted scatter plots between HCII and LADI and between HCII and LAVI indicated significant linear associations (Figure 2). Multiple regression analysis showed that age was a positive contributor for an increase in LADI and LAVI (Table 2). Conversely, HCII was found to be an independent and negative contributor for an increase in LADI and LAVI (Table 2). The significance of the relationship between HCII and LA size markers was more accurate in LAVI than in LADI (Figure 2 and Table 2).
Plasma HCII activity is inversely associated with concentric left ventricular remodeling
As increased RWT was recognized as a concentric change of the cardiac left ventricle, we evaluated the independent determinants for increasing RWT using simple and multiple regression analyses. Age and sex-adjusted scatter plots between HCII and RWT demonstrated a significant linear relationship as shown in Figure 2. Although age and body mass index were independent contributors for an increase in RWT, HCII was the sole negative contributor for an increase in RWT (Table 3). Although male gender, pulse pressure and the presence of hypertension were independent contributors for increase in LVMI, plasma HCII activity did not have any significant association with LVMI (Figure 2 and Table 3). Taken together, these results suggest that reduced plasma HCII activity is associated with the phenotype of cardiac concentric remodeling without increased LVMI.
Plasma HCII activity is inversely associated with left ventricular diastolic dysfunction
As not only left ventricular systolic dysfunction, but also left ventricular diastolic dysfunction were shown to be closely associated with all-cause mortality in the general population,22 we evaluated the relationship between plasma HCII activity and left ventricular diastolic function. Although age, SBP and the presence of hypertension were independent contributors for decrease in E/A ratio, plasma HCII activity did not have any significant association with E/A ratio (Figure2 and Table 4). On the other hand, significant linear associations were found in age and sex-adjusted scatter plots between HCII and DcT, and between HCII and E/e' value as shown in Figure 2. We then evaluated the independent determinants of DcT and E/e' ratio and found that HCII was an independent and negative contributor for increases in DcT and E/e' value (Table 4). These results indicated that HCII is the sole protective factor against left ventricular diastolic dysfunction.
Discussion
Enlarged LAD reflects left atrial pressure and volume overload in response to cardiac dysfunction associated with cardiovascular diseases, including atrial fibrillation.23, 24 There is accumulating evidence that the association between cardiovascular disease and LAV/body surface area (LAVI) is stronger than that observed with LAD/body surface area (LADI) after adjustment for age and gender in subjects with sinus rhythm.17, 23, 24, 25 Therefore, we assessed the relationships between plasma HCII activity and the LA size parameters. We found a significant inverse correlation between plasma HCII activity and LAVI, as well as LADI even after adjustment for other confounding cardiovascular risk factors, suggesting that HCII independently counteracts LA enlargement. Enlarged LAV has been shown to be associated with inflammation and atherosclerosis.26, 27 As cuff-tube placement around the femoral artery caused increases in the gene expression levels of inflammatory cytokines and chemokines, such as interleukin-1β and -6 and monocyte chemoattractant protein-1 in HCII-deficient mice compared with the levels in wild-type mice,14 there is a possibility that HCII prevents LA enlargement partly through its anti-inflammatory potency leading to attenuation of left atrial remodeling. As LAV is an indicator of the burden of diastolic dysfunction, even in patients without atrial fibrillation or significant valvular heart disease,28 our results indicated that plasma HCII activity could be involved in the pathogenesis of left ventricular diastolic dysfunction. Therefore, we estimated association between plasma HCII activity and left ventricular (LV) diastolic function in humans and observed the significant relationship between plasma HCII activity and ventricular diastolic dysfunction indicated by the DcT and E/e' ratio. As it is well known that prolonged DcT indicates abnormal LV relaxation in patients with early diastolic abnormality,29 a significant inverse relationship between plasma HCII activity and DcT suggests that HCII has potency to counteract abnormal LV relaxation in subjects without systolic LV dysfunction. Diastolic tissue Doppler velocities reflect myocardial relaxation and, in combination with conventional Doppler measurements, the ratios (transmitral early diastolic velocity/mitral annular early diastolic velocity (E/e' ratio)) have been used to non-invasively estimate LV filling pressure, as well as pulmonary capillary wedge pressure.30, 31, 32 As pulmonary capillary wedge pressure is a prognostic indicator in patients with HF, E/e' value is a similarly powerful predictor of prognosis in patients with various cardiac diseases.33 In the present study, plasma HCII activity was independently and inversely associated with the value of E/e', suggesting that HCII preserves compliance of the left ventricular wall.
Warfarin is a synthetic thrombin inhibitor and is frequently used for the prevention of cardiogenic thrombosis. AT is also an endogenous thrombin inhibitor in the intravascular lumen. As warfarin has never been documented to have a pharmacological effect on anticardiac remodeling and as the present study has shown that AT was not associated with any cardiac remodeling phenotype, thrombin inactivation at the intravascular lumen and/or intracardiac chamber might be unable to attenuate cardiac remodeling. Conversely, as HCII is thought to inhibit thrombin action by forming a bimolecular complex with dermatan sulfate proteoglycans that are deposited at vascular smooth muscle cells and fibroblasts, HCII may also exert tissue thrombin inactivation in cardiomyocytes and/or cardiac fibroblasts in concert with binding to the deposited dermatan sulfate.
PAR-1 is expressed in the heart by cardiomyocytes and cardiac fibroblasts34, 35 and a recent study demonstrated that PAR-1 expression was increased in the hearts of patients with ischemic and idiopathic dilated cardiomyopathy.36 PAR-1 expression is increased in the LV of a mouse model for chronic HF37 and Pawlinski et al.38 demonstrated that PAR-1 overexpression by cardiomyocytes induced cardiac hypertrophy in MHC-PAR-1 mice. These hypertrophic changes of cardiomyocytes by PAR-1 activation may be partly explained by the mechanism of cleavage of PAR-1 resulting in activation of Gq, G12/13 and Gi, as well as downstream signaling pathways, including the MAPK pathways ERK 1/2 and ERK5.39, 40 Therefore, activation of PAR-1 in the heart promotes hypertrophic growth and/or influences the survival of cardiomyocytes.34 These findings are consistent with the assumption that PAR-1 activation in the heart, including cardiomyocytes and cardiac fibroblasts, accelerates cardiac remodeling, leading to reduced elasticity of the left ventricular wall. From these previous observations, we hypothesized that HCII counteracts cardiac remodeling through inactivation of the tissue thrombin–PAR-1 pathway. As there is a possibility that activation and expression of (pro) thrombin and its major receptor PAR-1 axis is modulated according to the condition of cardiac stress in each subject, it is difficult to clarify the exact interplay between HCII and PAR-1 activation in such subjects. However, our results suggest that reduced plasma HCII activity is one of several major causes of LA enlargement and LV diastolic dysfunction regardless of PAR-1 expression levels.
The results of the present clinical study were further corroborated by a study using our HCII-deficient mice.41 In that study, infusion of angiotensin II prominently accelerated cardiac remodeling, including concentric LV changes, enlargement of LAV and exaggeration of cardiac fibrosis in HCII-deficient mice when compared with littermate wild-type mice.41 The study using HCII-deficient mice demonstrated that HCII protects against angiotensin II-induced cardiac remodeling through the suppression of the NAD(P)H oxidase–TGF-β1 pathway.41 Therefore, we speculate that HCII is also capable of attenuating oxidative stress in the human heart, as well as in the murine heart through suppression of the NAD(P)H oxidase–TGF-β1 pathway.
As LV hypertrophy causes LA enlargement and the LA enlargement may impair LV function, it is important to clarify whether HCII primarily influences LA or LV remodeling. Although further examinations are needed to clarify this issue, results of our animal studies using HCII-deficient mice indicate that abnormal changes, including angiotensin II-induced LV concentric change and LA enlargement with acceleration of cardiac fibrosis, seem to occur simultaneously after starting angiotensin II infusion (data not shown in reference 41), and it is therefore possible that HCII directly and independently influences LA enlargement and LV dysfunction.
The results of the present clinical study cannot be extended to the general population because we only enrolled patients with cardiovascular risk factors and we previously reported that subjects without cardiovascular risk factors had higher levels of plasma HCII activity than those in subjects with one or more cardiovascular risk factor.11 Thus, large-scale investigations and cohort studies are required to assess and clarify the prognostic value of plasma HCII activity for cardiac remodeling in the general population. In addition, it is crucial to compare plasma HCII activities in subjects with and without LV systolic dysfunction for understanding the pathophysiological roles of HCII in cardiac remodeling. Therefore, further examinations focusing on the relationship between HCII and systolic HF are needed. In summary, plasma HCII activity is independently and inversely associated with the development of cardiac remodeling including concentric cardiac changes, LA enlargement and LV diastolic dysfunction. These results suggest that the inactivation of thrombin in cardiac tissue by HCII might be a novel and valuable therapeutic approach to prevent cardiac remodeling and atherosclerosis.
References
Narayanan S . Multifunctional roles of thrombin. Ann Clin Lab Sci 1999; 29: 275–280.
Bar-Shavit R, Kahn A, Wilner GD, Fenton II JW . Monocyte chemotaxis: stimulation by specific exosite region in thrombin. Science 1983; 220: 728–731.
Chen LB, Buchanan JM . Mitogenic activity of blood components. I. Thrombin and prothrombin. Proc Natl Acad Sci USA 1975; 72: 131–135.
McNamara CA, Sarembock IJ, Gimple LW, Fenton II JW, Coughlin SR, Owens GK . Thrombin stimulates proliferation of cultured rat aortic smooth muscle cells by a proteolytically activated receptor. J Clin Invest 1993; 91: 94–98.
Derian CK, Damiano BP, D'Andrea MR, Andrade-Gordon P . Thrombin regulation of cell function through protease-activated receptors: implications for therapeutic intervention. Biochemistry (Mosc) 2002; 67: 56–64.
Hirano K . The roles of proteinase-activated receptors in the vascular physiology and pathophysiology. Arterioscler Thromb Vasc Biol 2007; 27: 27–36.
Nelken NA, Soifer SJ, O'Keefe J, Vu TK, Charo IF, Coughlin SR . Thrombin receptor expression in normal and atherosclerotic human arteries. J Clin Invest 1992; 90: 1614–1621.
Tollefsen DM . Insight into the mechanism of action of heparin cofactor II. Thromb Haemost 1995; 74: 1209–1214.
He L, Vicente CP, Westrick RJ, Eitzman DT, Tollefsen DM . Heparin cofactor II inhibits arterial thrombosis after endothelial injury. J Clin Invest 2002; 109: 213–219.
Takamori N, Azuma H, Kato M, Hashizume S, Aihara K, Akaike M, Tamura K, Matsumoto T . High plasma heparin cofactor II activity is associated with reduced incidence of in-stent restenosis after percutaneous coronary intervention. Circulation 2004; 109: 481–486.
Aihara K, Azuma H, Takamori N, Kanagawa Y, Akaike M, Fujimura M, Yoshida T, Hashizume S, Kato M, Yamaguchi H, Kato S, Ikeda Y, Arase T, Kondo A, Matsumoto T . Heparin cofactor II is a novel protective factor against carotid atherosclerosis in elderly individuals. Circulation 2004; 109: 2761–2765.
Tollefsen DM . Heparin cofactor II modulates the response to vascular injury. Arterioscler Thromb Vasc Biol 2007; 27: 454–460.
Vicente CP, He L, Tollefsen DM . Accelerated atherogenesis and neointima formation in heparin cofactor II deficient mice. Blood 2007; 110: 4261–4267.
Aihara K, Azuma H, Akaike M, Ikeda Y, Sata M, Takamori N, Yagi S, Iwase T, Sumitomo Y, Kawano H, Yamada T, Fukuda T, Matsumoto T, Sekine K, Sato T, Nakamichi Y, Yamamoto Y, Yoshimura K, Watanabe T, Nakamura T, Oomizu A, Tsukada M, Hayashi H, Sudo T, Kato S . Strain-dependent embryonic lethality and exaggerated vascular remodeling in heparin cofactor II-deficient mice. J Clin Invest 2007; 117: 1514–1526.
Aihara K, Azuma H, Akaike M, Sata M, Matsumoto T . Heparin cofactor II as a novel vascular protective factor against atherosclerosis. J Atheroscler Thromb 2009; 16: 523–531.
Aihara K, Azuma H, Akaike M, Kurobe H, Takamori N, Ikeda Y, Sumitomo Y, Yoshida S, Yagi S, Iwase T, Ishikawa K, Sata M, Kitagawa T, Matsumoto T . Heparin cofactor II is an independent protective factor against peripheral arterial disease in elderly subjects with cardiovascular risk factors. J Atheroscler Thromb 2009; 16: 127–134.
Tsang TS, Abhayaratna WP, Barnes ME, Miyasaka Y, Gersh BJ, Bailey KR, Cha SS, Seward JB . Prediction of cardiovascular outcomes with left atrial size: is volume superior to area or diameter? J Am Coll Cardiol 2006; 47: 1018–1023.
Lester SJ, Ryan EW, Schiller NB, Foster E . Best method in clinical practice and in research studies to determine left atrial size. Am J Cardiol 1999; 84: 829–832.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ . Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Aurigemma GP, Gottdiener JS, Arnold AM, Chinali M, Hill JC, Kitzman D . Left atrial volume and geometry in healthy aging: the Cardiovascular Health Study. Circ Cardiovasc Imaging 2009; 2: 282–289.
Devereux RB, Reichek N . Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977; 55: 613–618.
Redfield MM, Jacobsen SJ, Burnett Jr JC, Mahoney DW, Bailey KR, Rodeheffer RJ . Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003; 289: 194–202.
Pritchett AM, Jacobsen SJ, Mahoney DW, Rodeheffer RJ, Bailey KR, Redfield MM . Left atrial volume as an index of left atrial size: a population-based study. J Am Coll Cardiol 2003; 41: 1036–1043.
Tsang TS, Barnes ME, Bailey KR, Leibson CL, Montgomery SC, Takemoto Y, Diamond PM, Marra MA, Gersh BJ, Wiebers DO, Petty GW, Seward JB . Left atrial volume: important risk marker of incident atrial fibrillation in 1655 older men and women. Mayo Clin Proc 2001; 76: 467–475.
Lim TK, Dwivedi G, Hayat S, Majumdar S, Senior R . Independent value of left atrial volume index for the prediction of mortality in patients with suspected heart failure referred from the community. Heart 2009; 95: 1172–1178.
Rao AK, Djamali A, Korcarz CE, Aeschlimann SE, Wolff MR, Stein JH . Left atrial volume is associated with inflammation and atherosclerosis in patients with kidney disease. Echocardiography 2008; 25: 264–269.
Saura D, Marin F, Climent V, Gonzalez J, Roldan V, Hernandez-Romero D, Oliva MJ, Sabater M, de la Morena G, Lip GY, Valdes M . Left atrial remodelling in hypertrophic cardiomyopathy: relation with exercise capacity and biochemical markers of tissue strain and remodelling. Int J Clin Pract 2009; 63: 1465–1471.
Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D . Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 1999; 33: 1948–1955.
Oh JK, Hatle L, Tajik AJ, Little WC . Diastolic heart failure can be diagnosed by comprehensive two-dimensional and Doppler echocardiography. J Am Coll Cardiol 2006; 47: 500–506.
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA . Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 1997; 30: 1527–1533.
Sohn DW, Chung WY, Chai IH, Zo JH, Lee MM, Park YB, Choi YS, Lee YW . Mitral annulus velocity in the noninvasive estimation of left ventricular peak dP/dt. Am J Cardiol 2001; 87: 933–936.
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ . Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 2000; 102: 1788–1794.
Yamamoto T, Oki T, Yamada H, Tanaka H, Ishimoto T, Wakatsuki T, Tabata T, Ito S . Prognostic value of the atrial systolic mitral annular motion velocity in patients with left ventricular systolic dysfunction. J Am Soc Echocardiogr 2003; 16: 333–339.
Sabri A, Muske G, Zhang H, Pak E, Darrow A, Andrade-Gordon P, Steinberg SF . Signaling properties and functions of two distinct cardiomyocyte protease-activated receptors. Circ Res 2000; 86: 1054–1061.
Sabri A, Short J, Guo J, Steinberg SF . Protease-activated receptor-1-mediated DNA synthesis in cardiac fibroblast is via epidermal growth factor receptor transactivation: distinct PAR-1 signaling pathways in cardiac fibroblasts and cardiomyocytes. Circ Res 2002; 91: 532–539.
Moshal KS, Tyagi N, Moss V, Henderson B, Steed M, Ovechkin A, Aru GM, Tyagi SC . Early induction of matrix metalloproteinase-9 transduces signaling in human heart end stage failure. J Cell Mol Med 2005; 9: 704–713.
Moshal KS, Tyagi N, Henderson B, Ovechkin AV, Tyagi SC . Protease-activated receptor and endothelial-myocyte uncoupling in chronic heart failure. Am J Physiol Heart Circ Physiol 2005; 288: H2770–H2777.
Pawlinski R, Tencati M, Hampton CR, Shishido T, Bullard TA, Casey LM, Andrade-Gordon P, Kotzsch M, Spring D, Luther T, Abe J, Pohlman TH, Verrier ED, Blaxall BC, Mackman N . Protease-activated receptor-1 contributes to cardiac remodeling and hypertrophy. Circulation 2007; 116: 2298–2306.
Coughlin SR . Thrombin signalling and protease-activated receptors. Nature 2000; 407: 258–264.
Marinissen MJ, Servitja JM, Offermanns S, Simon MI, Gutkind JS . Thrombin protease-activated receptor-1 signals through Gq- and G13-initiated MAPK cascades regulating c-Jun expression to induce cell transformation. J Biol Chem 2003; 278: 46814–46825.
Sumitomo-Ueda Y, Aihara K, Ise T, Yoshida S, Ikeda Y, Uemoto R, Yagi S, Iwase T, Ishikawa K, Hirata Y, Akaike M, Sata M, Kato S, Matsumoto T . Heparin cofactor II protects against angiotensin II-induced cardiac remodeling via attenuation of oxidative stress in mice. Hypertension 2010; 56: 430–436.
Acknowledgements
We thank Kazue Ishikawa and Ryoko Uemoto for providing technical assistance. This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Science, Sports and Culture of Japan, a grant from the Mitsui Life Social Welfare Foundation, a grant from the Takeda Science Foundation, and a Grant for a Study Group on Aseptic Femoral Neck Necrosis from the Ministry of Health, Labour, and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ise, T., Aihara, Ki., Sumitomo-Ueda, Y. et al. Plasma heparin cofactor II activity is inversely associated with left atrial volume and diastolic dysfunction in humans with cardiovascular risk factors. Hypertens Res 34, 225–231 (2011). https://doi.org/10.1038/hr.2010.211
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.211