Abstract
Recent studies have reported a high prevalence of primary aldosteronism among patients with severe hypertension. However, the prevalence of this disease among normotensive and mildly hypertensive patients has not been determined. The aim of this study was to examine the prevalence of primary aldosteronism among prehypertensive and stage 1 hypertensive subjects. A total of 292 adult subjects with hypertension or prehypertension was screened for primary aldosteronism. Subjects with a plasma aldosterone concentration (ng per 100 ml) to plasma renin activity (ng ml–1 h–1) ratio (ARR) above 20 underwent confirmatory captopril suppression testing. A total of 54 subjects (18.5%) had an ARR above 20. A captopril suppression test was performed in 17 of 54 subjects with probable primary aldosteronism. The test confirmed the diagnosis of primary aldosteronism in 11 (64.7%) of 17 patients, giving a least prevalence of 3.8% for this disease. The 11 patients with primary aldosteronism had a mean±s.d. systolic blood pressure of 139±4 mm Hg, diastolic blood pressure of 95±10 mm Hg and serum potassium of 4.46±0.48 mEq l–1 at the time of screening test. The prevalence of primary aldosteronism as could be assessed in this study was at least 6.8% in prehypertensive patients, 3.3% in stage 1 hypertensive patients and 3.1% in stage 2 hypertensive patients. In conclusion, this study suggests a high prevalence of primary aldosteronism among prehypertensive and stage 1 hypertensive Japanese patients. Significant numbers of prehypertensive individuals may have subclinical forms of this disease.
Similar content being viewed by others
Introduction
Primary aldosteronism has historically been thought to be an uncommon cause of secondary hypertension, with prevalence rates of <0.5%. In addition, spontaneous hypokalemia has been considered obligatory for ordering diagnostic tests for primary aldosteronism. However, it is now recognized that significant numbers of patients with primary aldosteronism are not hypokalemic, and recent studies using the plasma aldosterone concentration (PAC) to plasma renin activity (PRA) ratio (ARR) as a screening test among both hypokalemic and normokalemic hypertensives have resulted in much higher prevalence estimates for this disease,1, 2, 3, 4 as high as 8–30% in severe and/or resistant hypertensive populations.5
Screening for primary aldosteronism is often indicated in individuals with moderate to severe hypertension and/or resistant hypertension, as the degree of hypertension with this disease is believed to usually be severe and may be resistant to usual pharmacological treatments. However, the clinical and biochemical features vary widely. Sporadic cases of normotensive primary aldosteronism have been rarely described,6, 7, 8, 9 and normotensive patients have been observed among individuals with familial hyperaldosteronism type-I (FH-I);10 however, the prevalence of this disease in normotensive and mild hypertensive populations has not been determined.6, 7, 11, 12 The purpose of this study was to examine the prevalence of primary aldosteronism in an unselected Japanese population with prehypertension and stage 1 hypertension at a health screening center.
Methods
A total of 292 consecutive adult subjects with hypertension or prehypertension visiting the Health Screening Center at KKR Hokuriku Hospital for a general health screening (annual health examination) was screened for primary aldosteronism. Subjects taking antihypertensive agents, and those with renal disease, hepatic failure or cardiac failure, were excluded from the study. The severity of hypertension was staged according to the Joint National Committee 7 criteria: prehypertension, 120 to 139/80 to 89 mm Hg; stage 1, 140 to 159/90 to 99 mm Hg; and stage 2, >160/100 mm Hg.13
The procedures used for the diagnosis of primary aldosteronism were in accordance with the guideline of the Japanese Society of Hypertension 2009 and Japanese Endocrine Society. Briefly, the subjects were advised to maintain an average dietary salt intake for the Japanese population (approximately over 11 g per day) before ARR testing and throughout the subsequent diagnostic screening for primary aldosteronism, and they were evaluated between 0800 and 1000 hours after an overnight fast. With subjects in the sitting position, blood pressure was measured with a properly calibrated and validated mercury sphygmomanometer by a healthcare professional. The subjects were seated quietly for at least 5 min in a chair with their feet on the floor, and an arm supported at heart level using an appropriate-sized cuff (cuff bladder encircling at least 80% of the arm). At least two measurements were made, and the mean value was calculated. The first and fifth Korotkoff sounds were used to designate systolic (SBP) and diastolic blood pressures (DBP). Written, informed consent was obtained from all participants. Blood was withdrawn from the antecubital vein to measure potassium, PAC and PRA after at least 2 h of upright posture (sitting, standing or walking), with patients seated at the time of blood collection. PAC (ng per 100 ml) and PRA (ng ml–1 h–1) were measured by radioimmunoassay using commercially available kits (SRL, Tokyo, Japan). In samples with PRA <0.2 ng ml–1 h–1, a PRA of 0.2 ng ml–1 h–1 was used for the calculation of ARR to avoid overinflating the ARR. An ARR >20 was regarded as being increased and suggestive of primary aldosteronism. In patients with an increased ARR, to confirm or exclude primary aldosteronism, the captopril suppression test was performed as an outpatient procedure after an overnight fast; blood samples for PAC and PRA were obtained 90 min after the patients received a 50-mg dose of captopril orally and rested in the supine position. The diagnosis was definite primary aldosteronism if the patients had a high ARR (>20) after the captopril suppression test.4
Patients with a confirmed diagnosis of primary aldosteronism underwent adrenal computed tomography scanning and adrenal venous sampling (AVS) by a highly experienced radiologist to differentiate unilateral from bilateral adrenal aldosterone overproduction. Adrenal vein cannulation was considered successful if the adrenal vein/inferior vena cava cortisol gradient was greater than two times. Unilateral aldosterone overproduction was defined when an aldosterone to cortisol ratio on one adrenal vein was greater than two times the ratio on the other adrenal vein and on the other side was less than the peripheral vein (‘contralateral suppression’), and less than two times with ratios more than the peripheral value on each adrenal vein for bilateral aldosterone overproduction.14 Patients with bilateral hyperaldosteronism were clinically diagnosed as having idiopathic hyperaldosteronism. In patients with unilateral hyperaldosteronism, adrenalectomy and pathological examination were performed, and follow-up data were collected after surgery.
No patients with definite primary aldosteronism underwent genetic testing for the presence of the CYP11B1-CYP11B2 hybrid gene responsible for the glucocorticoid-remediable form of primary aldosteronism because of the relative rarity of that subtype (∼1% of patients with primary aldosteronism).
ARR values are reported as medians (interquartile range), and other data for continuous variables are reported as means±s.d. Values were compared between the groups using Student's t-test, Welch's t-test or the Mann–Whitney U-test. The χ2-test or Fisher's exact test was used as appropriate for categorical variables. Observed differences were assumed to be statistically significant if P<0.05. As only a small proportion of the subjects with an increased ARR underwent a captopril suppression test, the true prevalence of primary aldosteronism cannot be determined from this study. Therefore, we calculated the least prevalence of primary aldosteronism as ‘the number of positive subjects in the captopril suppression test’ divided by ‘the total subjects in the screening test’ times 100.
Results
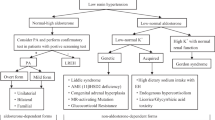
A total of 292 consecutive subjects (44 females, 248 males) visiting the Health Screening Center from July 2006 through June 2007 were studied (Table 1). The diagnostic flow chart for primary aldosteronism is shown in Table 2. Study subjects had a mean±s.d. age of 51.1±7.5 (range 33–72) years. Their SBP was 146±12 mm Hg, their DBP was 95±9 mm Hg, and their serum potassium was 4.27±0.34 mEq l–1. Overall, 44 subjects (15.1%) were categorized as having prehypertension, 152 subjects (52.1%) were categorized as having stage 1 hypertension and 96 subjects (32.9%) were categorized as having stage 2 hypertension.
A total of 54 subjects (18.5%) had an ARR above 20, and they were regarded as having probable primary aldosteronism. There were no statistically significant differences in age, SBP, DBP or serum potassium levels between subjects with and without probable primary aldosteronism. Compared with subjects without probable primary aldosteronism, subjects with probable primary aldosteronism had a higher PAC (12.0±4.4 (range 5.4–25.3) vs. 10.3±4.1 (range 2.5–31.8) ng per 100 ml, P<0.01), a lower PRA (0.42±0.20 (range 0.2–1.1) vs. 1.41±1.21 (range 0.3–11) ng ml–1 h–1, P<0.0001) and a higher ARR (27.2 (23.0–35.7) vs. 9.0 (6.2–13.3), P<0.0001) (Table 1).
A captopril suppression test was performed in 17 of the 54 subjects with an increased ARR, whereas the other 37 of 54 subjects did not visit our hospital for further examinations. In prehypertensive subjects, 50% of the positive subjects in the screening test underwent the captopril suppression test (Table 2). There were no statistically significant differences in age, SBP, DBP, serum potassium, PAC, PRA or ARR between the 54 subjects with an increased ARR and the 17 patients who underwent captopril suppression testing. The test confirmed the diagnosis of primary aldosteronism in 11 (64.7%; 3 females and 8 males) of 17 patients, giving a least prevalence of 3.8% for this disease (Table 2).
The 11 patients with primary aldosteronism had a mean±s.d. age of 53.1±6.5 years; their SBP was 139±4 mm Hg; their DBP was 95±10 mm Hg; their serum potassium was 4.46±0.48 mEq l–1; their PAC was 11.5±3.8 (range 7.8–22) ng per 100 ml; and their PRA was 0.32±0.09 (range 0.2–0.5) ng ml–1 h–1 at the time of the screening test (Table 3). Only three patients (27.3%) had an upright PAC that exceeded 12 ng per 100 ml; all patients had suppressed (<1.0 ng ml–1 h–1) PRA; and nine patients had frankly increased (>30) and two had high–normal (20–30) ARR. Subjects with and without confirmed primary aldosteronism were similar in age, SBP, DBP and serum potassium levels. The ARRs at the time of the screening test and after the captopril suppression test were significantly different between the two groups (screening: 35.7 (31.4–40.3) vs. 23.9 (21.1–26.8), P<0.05; and captopril suppression: 29.1 (23.9–33.2) vs. 10.6 (9.9–12.3), P<0.001) (Table 3).
The blood pressure measurements of the 11 patients with primary aldosteronism are shown in Table 4. Three patients were categorized as having prehypertension; five patients were categorized as having stage 1 hypertension; and three patients were categorized as having stage 2 hypertension. Although the true prevalence of primary aldosteronism cannot be determined from this study, the prevalence of primary aldosteronism as could be assessed in this study was at least 6.8% (3 of 44 subjects) in prehypertensive subjects, 3.3% in stage 1 hypertensive patients and 3.1% in stage 2 hypertensive patients (Table 2).
AVS was performed in 9 of 11 patients with confirmed primary aldosteronism for localization studies. Successful cannulation of the adrenal veins was achieved in eight (88.9%) of the nine who have so far undergone AVS; five (62.5%) patients demonstrated lateralization of aldosterone overproduction to one adrenal gland (two patients were prehypertensive, one was stage 1 hypertensive and two patients were stage 2 hypertensive), and three (37.5%) patients exhibited bilateral overproduction (one patient was prehypertensive and two were stage 1 hypertensive) and were clinically diagnosed as having idiopathic hyperaldosteronism (Tables 2 and 4). Adrenalectomy was performed in four of five patients with unilateral aldosterone overproduction, and the results of the pathological examinations of the removed adrenal glands were compatible with aldosterone-producing adenoma in three patients and nodular hyperplasia in one patient. Blood pressure decreased in all the four patients after adrenalectomy. Adrenal computed tomography was not useful to distinguish between unilateral and bilateral disease, as computed tomography detected no abnormal findings in the adrenal glands with unilateral hyperaldosteronism defined by AVS in four of five patients, and a bilateral adrenal mass was present in one patient with aldosterone-producing adenoma (Table 4).
Discussion
This study suggests a high prevalence of primary aldosteronism among an unselected Japanese population of prehypertensive and stage 1 hypertensive patients. The true prevalence of primary aldosteronism among prehypertensive or hypertensive individuals in our region cannot be precisely determined from this study, as only a small proportion of the subjects suspected as having primary aldosteronism underwent a captopril suppression test as a confirmatory test. Nevertheless, at least 6.8% of prehypertensive subjects (3 of 44 subjects) was confirmed as having a diagnosis of primary aldosteronism on the captopril suppression test and demonstrated lateralization of aldosterone overproduction on AVS; this rate of diagnosis of primary aldosteronism is rather high.
Nonhypertensive primary aldosteronism has been thought to be exceedingly rare. As far as we are aware, only 18 reports of sporadic cases have been documented in the English literature;8, 9, 15, 16 many cases were middle-aged Eurasian (especially Japanese) women, which suggests that genetic and sex-related protective factors have a function in the response to excessive aldosterone, and that this disease may have a higher prevalence in the nonhypertensive Japanese population. Many normotensive patients with excessive aldosterone production have also been observed among individuals with FH-I, and female patients with FH-I were relatively protected against the development of early-onset or severe hypertension.10 It is therefore likely that there are nonhypertensive patients with all forms of primary aldosteronism, whether familial or sporadic. Screening for primary aldosteronism is primarily limited to patients presenting with moderate to severe hypertension,17 because many recent studies have reported a much higher prevalence of this disease in severe and/or resistant hypertensive patients.1, 5, 18, 19, 20 In contrast, screening for primary aldosteronism in nonhypertensive or mild hypertensive populations has been described in only a few reports.6, 7, 11, 12 Therefore, the prevalence of this disease in normotensive or stage 1 hypertensive patients has not yet been determined. The prevalence of normotensive primary aldosteronism is probably underestimated, because screening for primary aldosteronism has been almost never performed in normotensive patients without hypokalemia or an adrenal mass.
Several possible causes of the nonhypertensive form of primary aldosteronism must be considered. Vantyghem et al.8 reported that blood pressure fell markedly after aldosterone-producing adenoma surgery in their nonhypertensive patients, suggesting that hyperaldosteronism had induced relative hypertension; however, the blood pressure remained at nonhypertensive levels due to very low spontaneous baseline levels. Another major explanation is that some of the study participants had mild, subclinical hyperaldosteronism because they were in the early phase of this disease, and hypertension may develop later and be detected on follow-up.21, 22 Estrogens may modulate the renin–angiotensin system and also have vasodilating actions on peripheral blood vessels and contribute to normalization of blood pressure,23 because 70% of previously reported normotensive primary aldosteronism patients were women.9 Rigorous sodium depletion may lower their blood pressure and could explain their normotensive status. However, patients in this study were advised to maintain an average dietary salt intake for a Japanese population (>11 g per day), which is much higher than that in several foreign countries.
This study had several limitations. First, a captopril suppression test was performed in only 17 of the 54 subjects with probable primary aldosteronism after screening showed an ARR >20. As it was impossible to calculate the exact prevalence rate including these ‘dropouts’, only the least prevalence rate could be reported. However, the prevalence rate was underestimated by this calculation; the prevalence of primary aldosteronism was at least 6.8% in prehypertensive patients and 3.3% in stage 1 hypertensive patients, indicating primary aldosteronism might not be uncommon in these patients. Second, the diagnosis of primary aldosteronism was based on only captopril suppression testing in this study, but several authors reported that the captopril suppression test is dependent on the sodium intake and less reliable than the saline load or fludrocortisone suppression test as a confirmatory test. Although we did not check 24-h urinary sodium measurements or spot urine samples to calculate a sodium/creatinine index, the study subjects were advised to maintain an average dietary salt intake for the Japanese population (>11 g per day). Such a large salt intake is sufficient for confirmative captopril suppression tests, because both the captopril suppression test and the saline infusion test have been shown to be accurate for confirming primary aldosteronism due to aldosterone-producing adenoma at a salt intake of >7.6 g per day.24 The captopril suppression test has been described as reliable, specific and safer for the diagnosis of primary aldosteronism, may be as good as tests of sodium suppression in confirming the diagnosis of primary aldosteronism,24, 25, 26, 27, 28 and has been recommended as a confirmatory test for the diagnosis of primary aldosteronism by the Japanese Society of Hypertension 2009 and Japanese Endocrine Society. Moreover, in this study, 8 (72.7%) of 11 patients with primary aldosteronism demonstrated lateralization of aldosterone overproduction on AVS, and the diagnosis of primary aldosteronism is highly likely in such patients.
In summary, this study suggested that primary aldosteronism was not uncommon in prehypertensive and stage 1 hypertensive Japanese patients. Given that recent evidence suggests that primary aldosteronism is a common condition, significant numbers of prehypertensive individuals may have subclinical forms of this disease.
References
Young WF . Primary aldosteronism: renaissance of a syndrome. Clin Endocrinol 2007; 66: 607–618.
Calhoun DA . Is there an unrecognized epidemic of primary aldosteronism? Hypertension 2007; 50: 447–453.
Loh KC, Koay ES, Khaw MC, Emmanuel SC, Young Jr WF . Prevalence of primary aldosteronism among Asian hypertensive patients in Singapore. J Clin Endocrinol Metab 2000; 85: 2854–2859.
Omura M, Saito J, Yamaguchi K, Kakuta Y, Nishikawa T . Prospective study on the prevalence of secondary hypertension among hypertensive patients visiting a general outpatient clinic in Japan. Hypertens Res 2004; 27: 193–202.
Calhoun DA, Nishizaka MK, Zaman MA, Thakkar RB, Weissmann P . Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension 2002; 40: 892–896.
Mosso L, Carvajal C, Gonzalez A, Barraza A, Avila F, Montero J, Huete A, Gederlini A, Fardella CE . Primary aldosteronism and hypertensive disease. Hypertension 2003; 42: 161–165.
Fardella CE, Mosso L, Gomez-Sanchez C, Cortes P, Soto J, Gomez L, Pinto M, Huete A, Oestreicher E, Foradori A, Montero J . Primary hyperaldosteronism in essential hypertensives: prevalence, biochemical profile, and molecular biology. J Clin Endocrinol Metab 2000; 85: 1863–1867.
Vantyghem M-C, Ronci N, Provost F, Ghulam A, Lefebvre J, Jeunemaitre X, Tabarin A . Aldosterone-producing adenoma without hypertension: a report of two cases. Eur J Endocrinol 1999; 141: 279–285.
Medeau V, Moreau F, Trinquart L, Clemessy M, Wemeau J-L, Vantyghem M-C, Plouin P-F, Reznik Y . Clinical and biochemical characteristics of normotensive patients with primary aldosteronism: a comparison with hypertensive cases. Clin Endocrinol 2008; 69: 20–28.
Stowasser M, Bachmann AW, Huggard PR, Rossetti TR, Gordon RD . Severity of hypertension in familial hyperaldosteronism type I: relationship to gender and degree of biochemical disturbance. J Clin Endocrinol Metab 2000; 85: 2160–2166.
Williams JS, Williams GH, Raji A, Jeunemaitre X, Brown NJ, Hopkins PN, Conlin PR . Prevalence of primary hyperaldosteronism in mild to moderate hypertension without hypokalaemia. J Hum Hypertens 2006; 20: 129–136.
Nishizaka MK, Calhoun DA . Primary aldosteronism: diagnostic and therapeutic considerations. Curr Cardiol Rep 2005; 7: 412–417.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ . The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Rossi GP, Sacchetto A, Chiesura-Corona M, Toni RD, Gallina M, Feltrin P, Pessina AC . Identification of the etiology of aldosteronism with adrenal vein sampling in patients with equivocal computed tomography and magnetic resonance findings: results in 104 consecutive cases. J Clin Endocrinol Metab 2001; 86: 1083–1090.
Matsunaga M, Hara A, Song TS, Hashimoto M, Tamori S, Ogawa K, Morimoto K, Pak CH, Kawai C, Yoshida O . Asymptomatic normotensive primary aldosteronism. Case report. Hypertension 1983; 5: 240–243.
Shiroto H, Ando H, Ebitani I, Hara M, Numazawa K, Kawamura S, Sasaki H . Normotensive primary aldosteronism. Am J Med 1980; 69: 603–606.
Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, Young WF, Montori VM . Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 2008; 93: 3266–3281.
Rossi GP, Bernini G, Caliumi C, Desideri G, Fabris B, Ferri C, Ganzaroli C, Giacchetti G, Letizia C, Maccario M, Mallamaci F, Mannelli M, Mattarello M-J, Moretti A, Palumbo G, Parenti G, Porteri E, Semplicini A, Rizzoni D, Rossi E, Boscaro M, Pessina AC, Mantero F . PAPY Study Investigators. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol 2006; 48: 2293–2300.
Umpierrez GE, Cantey P, Smiley D, Palacio A, Temponi D, Luster K, Chapman A . Primary aldosteronism in diabetic subjects with resistant hypertension. Diabetes Care 2007; 30: 1699–1703.
Strauch B, Zelinka T, Hampf M, Bernhardt R, Widimsky Jr J . Prevalence of primary hyperaldosteronism in moderate to severe hypertension in the central Europe region. J Hum Hypertens 2003; 17: 349–352.
Vasan RS, Evans JC, Larson MG, Wilson PW, Meigs JB, Rifai N, Benjamin EJ, Levy D . Serum aldosterone and the incidence of hypertension in nonhypertensive persons. N Engl J Med 2004; 351: 33–41.
Dluhy RG, Williams GH . Aldosterone—villain or bystander? N Engl J Med 2004; 351: 8–10.
Ojeda NB, Grigore D, Robertson EB, Alexander BT . Estrogen protects against increased blood pressure in postpubertal female growth restricted offspring. Hypertension 2007; 50: 679–685.
Rossi GP, Belfiore A, Bernini G, Desideri G, Fabris B, Ferri C, Giacchetti G, Letizia C, Maccario M, Mallamaci F, Mannelli M, Palumbo G, Rizzoni D, Rossi E, Agabiti-Rosei E, Pessina AC, Mantero F . PAPY Study Investigators. Comparison of the captopril and the saline infusion test for excluding aldosterone-producing adenoma. Hypertension 2007; 50: 424–431.
Agharazii M, Douville P, Grose JH, Lebel M . Captopril suppression versus salt loading in confirming primary aldosteronism. Hypertension 2001; 37: 1440–1443.
Castro OL, Yu X, Kem DC . Diagnostic value of the post-captopril test in primary aldosteronism. Hypertension 2002; 39: 935–938.
Naomi S, Iwaoka T, Umeda T, Inoue J, Hamasaki S, Miura F, Fujii Y, Sato T . Clinical evaluation of the captopril screening test for primary aldosteronism. Jpn Heart J 1985; 26: 549–556.
Iwaoka T, Umeda T, Naomi S, Inoue J, Sasaki M, Yamauchi J, Sato T . The usefulness of the captopril test as a simultaneous screening for primary aldosteronism and renovascular hypertension. Am J Hypertens 1993; 6: 899–906.
Acknowledgements
YT was supported, in part, by a Japanese Ministry of Health, Labor and Welfare grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ito, Y., Takeda, R., Karashima, S. et al. Prevalence of primary aldosteronism among prehypertensive and stage 1 hypertensive subjects. Hypertens Res 34, 98–102 (2011). https://doi.org/10.1038/hr.2010.166
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.166
Keywords
This article is cited by
-
Diagnosis and management of primary hyperaldosteronism in patients with hypertension: a practical approach endorsed by the British and Irish Hypertension Society
Journal of Human Hypertension (2023)
-
Frequently asked questions and answers (if any) in patients with adrenal incidentaloma
Journal of Endocrinological Investigation (2021)
-
Primary aldosteronism is a public health issue: challenges and opportunities
Journal of Human Hypertension (2020)
-
Comparison of eplerenone and spironolactone for the treatment of primary aldosteronism
Hypertension Research (2016)
-
Primary aldosteronism and salt
Pflügers Archiv - European Journal of Physiology (2015)