Abstract
Salt intake is an important risk factor for hypertension. Because it has been reported that increased salt intake dulls the taste of salt, measuring the sense of taste might be a good way of identifying individuals who consume excessive salt. Using a recently developed simple salt taste test, we investigated the relationship between the taste of salt and blood pressure. The subjects in this cross-sectional study were 823 Japanese adults (479 women and 344 men) 40 years old or older. Following a taste test with salt-impregnated taste strips, the subjects were divided into two groups: normal (recognition threshold of salt at <1.0% concentration) and taste impaired (⩾1.0%). We determined hypertension from the measured blood pressure. In women, the multi-adjusted odds ratio (95% CI) of hypertension in the impaired group was 2.47 (1.53–3.99) compared with the normal group, whereas no significant difference was observed between the two male groups. When we excluded subjects with moderate and severe hypertension, similar findings were observed. A sub-analysis of couples living alone showed a higher prevalence of hypertension among men whose wives were in the impairment group (58.8%) than in the normal group (36.7%, P=0.10). In conclusion, the taste of salt is associated with blood pressure in Japanese women, but not in men. Because most family meals in Japan are prepared by women, educating women about salt reduction may contribute to the prevention of hypertension, not only among women but also among their husbands and family members.
Similar content being viewed by others
Introduction
Hypertension is a clear risk factor for cardiovascular disease.1 In 2001, 7.6 million premature deaths and 92 million disability-adjusted life years worldwide were attributed to high blood pressure.2 In Japan, the population-attributable fraction of hypertension for all-cause mortality is reported to be approximately 20%.3 The findings of the INTERSALT and INTERMAP studies indicated a positive association between salt intake and blood pressure in multiethnic populations,4, 5, 6, 7 and evidence from randomized controlled trials has shown that a low sodium diet reduces blood pressure.8, 9, 10 Although public health recommendations in most developed countries suggest reducing salt intake to 5–6 g day−1,11 the average salt intake in Japan is still higher than the recommendations (10.8 g day−1, according to a national health and nutrition survey in 200612).
In an attempt to modify lifestyles to include a reduction in salt intake, several health education tools, such as measurement of 24-h urinary sodium excretion and evaluation of diet with regard to salt content, have been developed. These methods are reliable, but they are not widely used in either clinical or community settings for practical reasons.13
Because evidence exists that increased salt intake dulls the taste of salt,14 measuring the taste of salt might be useful as a screening tool to identify individuals with elevated salt intake who are, therefore, at high risk for hypertension. In fact, the taste recognition threshold for salt is elevated in hypertensive patients.15, 16 A simple and convenient taste test using salt-impregnated taste strips has been developed recently.17, 18 To date, however, few epidemiological studies have taken advantage of this test to investigate the association of salt taste with blood pressure. It is logical to assume that the salt taste of the primary cook in a family is the key determinant of the entire household's salt intake, so it makes sense to investigate the relationship between that person's salt taste and the blood pressure of other members of the household.
With this in mind, our aim was to investigate the relationship between salt taste, using a recently developed simple test, and blood pressure in Japanese community-dwelling women and men.
Methods
Study population
The rural town of Kurabuchi in Takasaki City, Gunma prefecture, Japan, conducted annual health check-ups on residents aged 40 years or older (3175 residents in 2007), in accordance with the Japanese Health and Medical Services Law for the Elderly. In 2007, 579 women and 450 men attended the health examinations, at which time they were all invited to participate in a salt taste test. Of the women, 479 (83% of 579) accepted our invitation and gave informed consent for us to use the data collected. Together with the 344 (76% of 450) men who accepted, they constituted the subjects for this study. The characteristics of the study population are shown in Table 1. This study received ethics committee approval (Keio University School of Medicine, Tokyo, Japan).
Data collection
For the assessment of salt taste, we used a salt-impregnated taste strip, Salsave (Advantech Toyo Co., Tokyo, Japan), which has been validated using the whole-mouth method as a standard.17 The strips are impregnated with sodium chloride at concentrations of 0, 0.6, 0.8, 1.0, 1.2, 1.4 and 1.6%. The test-retest reliability of the strips was acceptable, and Spearman's rank correlation coefficient was 0.6 when 20 volunteer subjects were tested with a mean interval of 7 days. To determine the taste recognition threshold for salt, we used a modified version of the method developed by Maruyama18 and Nishimoto.17 The subjects were first asked to rinse their mouths with distilled water to neutralize oral conditions as much as possible. They were then asked to place a strip saturated with 0% sodium chloride on their tongue for three seconds to familiarize themselves with the taste of a blank strip. They then sequentially tasted the remaining taste strips in the same way, beginning with the lowest concentration. They were asked to report any taste and to say what it was. The concentration at which they identified the salt taste was taken as the recognition threshold. Subjects who could not recognize salt, even at the highest concentration level (1.6%), were assigned a recognition threshold of 1.6%. We prepared a manual for the procedure and trained a number of field staff. The trained staff were blinded to the subjects' medical conditions, including blood pressure.
The health examination included blood pressure measurements, blood tests and face-to-face interviews. Trained nurses took two blood pressure readings 60 s apart, using an automatic sphygmomanometer (Colin BP-103i, Tokyo, Japan) after each participant had been seated for 5 min at rest. The average of the two measurements was used for the analysis. Hypertension was defined as a systolic blood pressure (SBP) of 140 mm Hg or higher, a diastolic blood pressure (DBP) of 90 mm Hg or higher, the use of antihypertensive agents, or any combination of the above.
Total cholesterol and blood glucose were measured enzymatically from non-fasting blood samples in one laboratory (Harunaso Hospital, Gunma, Japan). Body mass index was calculated as weight (kg) divided by the square of height (m). Information on smoking, alcohol consumption, the presence of artificial teeth and living situation was obtained during interviews with trained nurses.
Statistical analysis
All statistical analyses were performed with Stata 9 software (Stata Corporation, College Station, TX, USA).
We applied stratification analysis by sex to assess the relationship between the taste of salt and hypertension, because a statistically significant interaction between the taste of salt and sex on hypertension was observed (P<0.05 for interaction by likelihood ratio test). For each taste recognition threshold for salt, a χ2 test and Student's t-test or one-way analysis of variance were used for comparisons of frequencies and mean values. Using a recognition threshold of 0.6% as the reference level, we applied logistic regression to obtain the age-adjusted odds ratios (OR) and 95% confidence interval (95% CI) for hypertension at each recognition threshold. Adjustment for age (continuous), body mass index (continuous), casual blood glucose (continuous), total cholesterol (continuous), the presence of artificial teeth (no, yes), smoking (none, <20, ⩾20 cigarettes per day) and alcohol consumption (none, <23, ⩾23 g of ethanol per day) was done by multivariate logistic regression. Trend tests were performed by allocating scores of 1, 2, 3, 4, 5 and 6 for each recognition threshold. Although smoking and alcohol consumption may modify taste,19 statistical methods such as stratification and a likelihood ratio test for interaction did not show any evidence that the association of the taste of salt with blood pressure varied according to smoking status or alcohol intake in this population. In addition, to examine the association of salt taste with milder stages of hypertension, we excluded subjects with moderate and severe hypertension (SBP⩾160 mm Hg or DBP⩾100 mm Hg, as defined by the Japanese Society of Hypertension guidelines for the management of hypertension (JSH2004)20). Subgroup analyses excluding subjects taking antihypertensive drugs or those of 70 years of age or older were also performed.
In Japan, women generally prepare meals for the family, so it is likely that their taste for salt influences the blood pressure of their family members, particularly their husbands. Indeed, it is probable that a woman's salt taste has a stronger influence on her husband's blood pressure than her own. We restricted the subjects to 77 couples living alone and investigated whether women's salt taste influenced their husbands' blood pressure as well as their own. Conveniently, because options for dining out are limited in this rural town, men usually eat at home. Therefore, this population seemed suitable for examining such an association.
Results
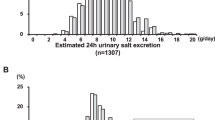
The salt taste test took about three minutes to perform per person. The percentage of the subjects with each taste recognition threshold for salt (0.6, 0.8, 1.0, 1.2, 1.4 and 1.6%) was, 62.2, 17.1, 6.9, 5.4, 3.3 and 5.1% among women, and 49.4, 18.3, 7.8, 6.7, 4.9 and 12.9% among men, respectively.
Table 2 shows the association between the taste recognition threshold for salt and blood pressure. For both sexes, the prevalence of the use of hypertensive agents increased along with elevation of the recognition threshold. Among women, elevated recognition thresholds were related to an increased prevalence of hypertension (age-adjusted OR (95% CI) for each 1-unit increase in the recognition (1.26 1.10–1.44). The inclusion of several potential confounders in the models did not change the results substantially. Compared with a recognition threshold of 0.6%, the recognition threshold of 1.4% showed the highest OR for hypertension (multi-adjusted OR (95% CI)=6.64 (1.99–22.16)). Among men, however, no constant tendency was observed regarding the relationship between the recognition threshold and hypertension. We conducted the following three subgroup analyses: (1) excluding subjects with moderate and severe hypertension; (2) excluding subjects taking antihypertensive agents; and (3) excluding subjects 70 years old or older. These analyses produced results similar to those obtained for the full study population (data not shown).
Because no universally accepted cutoff point for the taste recognition threshold for salt in relation to hypertension has been established, we classified the subjects as normal (<1.0%) or taste impaired (⩾1.0%), as shown in Table 2. Among women, the multi-adjusted OR (95% CI) in the impairment group was 2.47 (1.53–3.99) for hypertension when compared with the normal group. Among the men, there was no significant relationship between the taste threshold categories and hypertension.
Table 3 summarizes the results of the secondary analysis of 77 couples living alone. As with the main analysis presented in Table 2, a relationship between the women's salt taste and their own blood pressure was demonstrated. For the women in the impairment group, the prevalence of hypertension in their husbands (58.8%) tended to be higher than in the husbands of women in the normal group (36.7%, P=0.10). Even after excluding subjects with moderate and severe hypertension, the association between women's salt taste and their husbands' blood pressure was similar (P=0.07).
Discussion
In this cross-sectional study of Japanese community-dwelling adults 40 years old or older, we found that an elevated taste recognition threshold for salt was associated with an increased prevalence of hypertension in women, but not in men. These associations did not change after adjusting for several potential confounders. Interestingly, our findings also suggest that a woman's salt taste might influence her husband's blood pressure.
Making people aware of their own taste of salt has been reported to be helpful in educating them to reduce their salt intake.21, 22 A simple taste test using salt-impregnated taste strips overcomes the disadvantages of the standard taste tests, such as the whole-mouth method, the micropipette method and the paper filter disk stimulation method in the following respects: the test is less time-consuming, administering it requires no special training and there is no need to prepare a testing solution, for example, salt solution.23 This makes it possible to use the test repeatedly in clinical and community settings; the effects of dietary salt restriction can be evaluated by the subjects' taste threshold for salt both before and after health education. This is useful because it has been reported that salt restriction improves the taste threshold.24 In addition, subjects are able to receive their test results on site and interpret them easily, without any special knowledge. Although no clear cutoff value for the taste recognition threshold for salt has been established, we proposed 1.0% based on our finding that the odds of hypertension were elevated in women at thresholds above 1.0%. This tentative cutoff point, however, should be examined in other populations to determine whether it is generally applicable. We found that the prevalence of hypertension did not increase when the taste recognition threshold was 1.6%. It is possible that the participants in this category included subjects who did not understand the procedure or who had a taste dysfunction caused by factors other than excessive salt intake.
The present study found no clear association between the taste threshold for salt and blood pressure among the male subjects, possibly because Japanese men are not accustomed to the act of tasting for culinary purposes because they rarely prepare meals in everyday life. This result is consistent with the findings of Minohara et al.25; in taste tests involving the dropping of solutions on the tongue, they found that hypertensive women had elevated taste recognition thresholds for salt, whereas men did not. On the other hand, in a study using salt-impregnated taste strips, Maruyama et al.18 reported an association between elevated taste recognition thresholds for salt and hypertension in men. Although some early studies performed in Western populations suggested a relationship between salt taste and blood pressure, the studies were performed in clinical settings and did not show the results stratified by sex.15, 16, 26, 27, 28 Therefore, it is difficult to compare those results with the results of our study. Because this was a cross-sectional study, prospective studies regarding the connection between the taste of salt and blood pressure are needed.
To promote a reduction in salt intake, health education programs dealing with the household as a basic unit for intervention have been attempted. Yokota et al.29 conducted a community-based blood pressure control program in which they evaluated the salt concentration of soybean soup in each household. Our findings may support the household intervention strategy, where the main cook of the family is the key target for intervention. Because the results of the INTERSALT study suggest that maintaining low salt intake leads to no or minimal increase in blood pressure with age,6, 30 success in persuading the main cook in a family to reduce the salt content of meals could contribute to not only lowering the family members' current blood pressure, but also preventing the development of hypertension. This knowledge may motivate Japanese women to reduce the use of salt in their meals.
When interpreting the results of this study, some methodological issues should be discussed. First, outcome misclassification may have occurred because we adopted casual blood pressure due to the feasibility of screening for hypertension in the health check-up setting. Home blood pressure and ambulatory blood pressure are more closely associated with cardiovascular mortality and stroke morbidity than conventional blood pressure31 and can be used to detect white coat hypertension and masked hypertension.32 We assumed outcome misclassification to be non-differential with respect to exposure status. Thus, our results are likely to underestimate the relationship between salt taste and blood pressure because they are biased toward the null. Second, although we adjusted for several potential confounders, there is a possibility of residual confounding by factors known to influence blood pressure, for example, several dietary factors such as vegetable proteins, polyunsaturated fatty acids, phosphorus and iron.5, 7, 33, 34, 35 Finally, although earlier research has provided evidence that increased salt intake dulls the taste of salt,14 epidemiological evidence of the association between the salt taste and salt intake is limited. Additional studies are needed.
In conclusion, salt taste impairment was associated with an increased prevalence of hypertension in Japanese women 40 years old or older, but not in men. For women, measuring the taste threshold for salt seems to be a promising screening tool to detect individuals at high risk for hypertension caused by excessive salt intake. Furthermore, health education on salt restriction aimed at Japanese women, generally the main cook in the family, may contribute to hypertension prevention not only among the women themselves, but also among their family members.
Conflict of interest
The authors declare no conflict of interest.
References
Hozawa A, Okamura T, Murakami Y, Kadowaki T, Nakamura K, Hayakawa T, Kita Y, Nakamura Y, Abbot RD, Okarama A, Ueshima H, the NIPPON DATA80 Research Group. Joint impact of smoking and hypertension on cardiovascular disease and all-cause mortality in Japan: NIPPON DATA80, a 19-year follow-up. Hypertens Res 2007; 30: 1169–1175.
Lawes CM, Vander Hoorn S, Rodgers A . Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371: 1513–1518.
Murakami Y, Hozawa A, Okamura T, Ueshima H, the Evidence for Cardiovascular Prevention From Observational Cohorts in Japan Research Group (EPOCH-JAPAN ). Relation of blood pressure and all-cause mortality in 180 000 Japanese participants. Pooled analysis of 13 cohort studies. Hypertension 2008; 51: 1483–1492.
Zhao L, Stamler J, Yan LL, Zhou B, Wu Y, Liu K, Daviglus ML, Dennis BH, Elliott P, Ueshima H, Yang J, Zhu L, Guo D, for the INTERMAP Research Group. Blood pressure differences between northern and southern Chinese: role of dietary factors: the International Study on Macronutrients and Blood Pressure. Hypertension 2004; 43: 1332–1337.
Ueshima H, Stamler J, Elliott P, Chan Q, Brown IJ, Carnethon MR, Daviglus ML, He K, Moag-Stahlberg A, Rodriguez BL, Steffen LM, Van Horn L, Yarnell J, Zhou B, for the INTERMAP Research Group. Food omega-3 fatty acid intake of individuals (total, linolenic acid, long-chain) and their blood pressure: INTERMAP study. Hypertension 2007; 50: 313–319.
Intersalt Cooperative Research Group. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 h urinary sodium and potassium excretion. BMJ 1988; 297: 319–328.
Elliott P, Stamler J, Dyer AR, Appel L, Dennis B, Kesteloot H, Ueshima H, Okayama A, Chan Q, Garside DB, Zhou B, for the INTERMAP Cooperative Research Group. Association between protein intake and blood pressure: the INTERMAP Study. Arch Intern Med 2006; 166: 79–87.
Whelton PK, Appel LJ, Espeland MA, Applegate WB, Ettinger Jr WH, Kostis JB, Kumanyika S, Lacy CR, Johnson KC, Folmar S, Cutler JA, for the TONE Collaborative Research Group. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). JAMA 1998; 279: 839–846.
The Trials of Hypertension Prevention Collaboration Research Group. The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the trials of hypertension prevention, Phase I. JAMA 1992; 267: 1213–1220.
Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller III ER, Simons-Morton DG, Karanja N, Lin PH, for the DASH-Sodium Collaborative Research Group. Effects on blood pressure of reduced dietary sodium and the dietary approaches to stop hypertension (DASH) diet. N Engl J Med 2001; 344: 3–10.
He FJ, MacGregor GA . Effect of modest salt reduction on blood pressure: a meta-analysis of randomized trials. Implications for public health. J Hum Hypertens 2002; 16: 761–770.
Health and Welfare Statistics Association. Kokumin eisei no douko. J Health Welf Stat 2008; 55: 459 (in Japanese).
Kawano Y, Tsuchihashi T, Matsuura H, Ando K, Fujita T, Ueshima H . Report of the Working Group for Dietary Salt Reduction of the Japanese Society of Hypertension: (2) Assessment of salt intake in the management of hypertension. Hypertens Res 2007; 30: 887–893.
Mattes RD . The taste for salt in humans. Am J Clin Nutr 1997; 65: 692S–697S.
Barylko-Pikielna N, Zawadzka L, Niegowska J, Cybulska I, Sznajderman M . Taste perception of sodium chloride in suprathreshold concentration related to essential hypertension. J Hypertens 1985; 3: S449–S452.
Fallis N, Lasagna L, Tetreulat L . Gustatory thresholds in patients with hypertension. Nature 1962; 196: 74–75.
Nishimoto K, Hirota R, Egawa M, Furuta S . Clinical evaluation of taste dysfunction using a salt-impregnated taste strip. ORL J Otorhinolaryngol Relat Spec 1996; 58: 258–261.
Maruyama C, Murata M, Tomiyama J, Kumamoto E, Matsuo S, Nunokawa N, Murakami T, Aizawa C . Study of salty teste in healthy subjects and hypertensive patients (first report). Jpn J Nutr 1990; 48: 121–126 (in Japanese with English abstract).
Maruyama C, Amagai K, Higashi C, Matsuzawa M, Okuwaki I, Kichimi C, Ahara S, Murakami T, Aizawa C . A study of salt teste in healthy subjects and patients with hypertension (second report). Jpn J Nutr 1990; 48: 267–271 (in Japanese with English abstract).
Japanese Society of Hypertension. Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2004). Hypertens Res 2006; 29 Suppl: S1–S105.
Iso H, Yokota K, Shimamoto T, Sankai T, Imano H, Koike K, Harada M, Wakabayashi Y, Inagawa M, Ohki M, Komachi Y . A randomized controlled trail of intensive and usual community-based education for blood pressure control. Nippon Koshu Eisei Zasshi 1994; 41: 1015–1026 (in Japanese with English abstract).
Iso H, Shimamoto T, Naito Y, Sato S, Kitamura A, Iida M, Konishi M, Jacobs Jr DR, Komachi Y . Effects of a long-term hypertension control program on stroke incidence and prevalence in a rural community in northeastern Japan. Stroke 1998; 29: 1510–1518.
Mueller C, Kallert S, Renner B, Stiassny K, Temmel AF, Hummel T, Kobal G . Quantitative assessment of gustatory function in a clinical context using impregnated ‘taste strips’. Rhinology 2003; 41: 2–6.
Beauchamp GK, Bertino M, Burke D, Engelman K . Experimental sodium depletion and salt taste in normal human volunteers. Am J Clin Nutr 1990; 51: 881–889.
Minohara M, Ito Y, Otani M, Sasaki R, Aoki K . A study on taste-sensitivity in healthy adults—with reference to blood pressure. Nippon Koshu Eisei Zasshi 1988; 35: 133–138 (in Japanese with English abstract).
Zumkley H, Vetter H, Mandelkow T, Spieker C . Taste sensitivity for sodium chloride in hypotensive, normotensive and hypertensive subjects. Nephron 1987; 47 (Suppl 1): 132–134.
Schechter PJ, Horwitz D, Henkin RI . Salt preference in patients with untreated and treated essential hypertension. Am J Med Sci 1974; 267: 320–326.
Isezuo SA, Saidu Y, Anas S, Tambuwal BU, Bilbis LS . Salt taste perception and relationship with blood pressure in type 2 diabetics. J Hum Hypertens 2008; 22: 432–434.
Yokota K, Harada M, Wakabayashi Y, Inagawa E, Oshima M, Toriumi S, Hirose K, Shiina Y, Yamagishi K, Cui R, Ikeda A, Yao M, Noda H, Tanigawa T, Tanaka S, Kurokawa M, Imano H, Kiyama M, Kitamura A, Sato S, Shimamoto T, Iso H . Evaluation of a community-based health education program for salt reduction through media campaigns. Nippon Koshu Eisei Zasshi 2006; 53: 543–553 (in Japanese with English abstract).
Mancilha-Carvalho JJ, de Oliveira R, Esposito RJ . Blood pressure and electrolyte excretion in the Yanomamo Indians, an isolated population. J Hum Hypertens 1989; 3: 309–314.
Ohkubo T . Prognostic significance of variability in ambulatory and home blood pressure from the Ohasama study. J Epidemiol 2007; 17: 109–113.
Hozawa A, Ohkubo T, Kikuya M, Yamaguchi J, Ohmori K, Fujiwara T, Hashimoto J, Matsubara M, Kitaoka H, Nagai K, Tsuji I, Satoh H, Hisamichi S, Imai Y . Blood pressure control assessed by home, ambulatory and conventional blood pressure measurements in the Japanese general population: the Ohasama study. Hypertens Res 2002; 25: 57–63.
Elliott P, Kesteloot H, Appel LJ, Dyer AR, Ueshima H, Chan Q, Brown IJ, Zhao L, Stamler J, for the INTERMAP Cooperative Research Group. Dietary phosphorus and blood pressure: international study of macro- and micro-nutrients and blood pressure. Hypertension 2008; 51: 669–675.
Miura K, Stamler J, Nakagawa H, Ueshima H, Chan Q, Brown IJ, Tzoulaki I, Saitoh S, Dyer AR, Daviglus ML, Kesteloot H, Okayama A, Curb JD, Rodriguez BL, Elmer PJ, Steffen LM, Robertson C, Zhao L, for the International Study of Macro-Micronutrients and Blood Pressure Research Group. Relationship of dietary linoleic acid to blood pressure: the International Study of Macro-Micronutrients and Blood Pressure Study. Hypertension 2008; 52: 408–414.
Tzoulaki I, Brown IJ, Chan Q, Van Horn L, Ueshima H, Zhao L, Stamler J, Elliott P, for the International Collabotarive Research Group on Macro/Micronutrients and Blood Pressure. Relation of iron and red meat intake to blood pressure: cross sectional epidemiological study. BMJ 2008; 337: a258.
Acknowledgements
We are grateful to all staff members of the Kurabuchi project. We additionally thank Michiko Okamoto, Noriko Ijuin, Kaoru Uchida and Mutsuko Yamada for their support. This study was supported by a Grand-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology, Japan (No. 19390166).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Michikawa, T., Nishiwaki, Y., Okamura, T. et al. The taste of salt measured by a simple test and blood pressure in Japanese women and men. Hypertens Res 32, 399–403 (2009). https://doi.org/10.1038/hr.2009.31
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.31
Keywords
This article is cited by
-
Selective deletion of endothelial mineralocorticoid receptor protects from vascular dysfunction in sodium-restricted female mice
Biology of Sex Differences (2020)
-
Relationship of household salt intake level with long-term all-cause and cardiovascular disease mortality in Japan: NIPPON DATA80
Hypertension Research (2020)
-
Female Sex, a Major Risk Factor for Salt-Sensitive Hypertension
Current Hypertension Reports (2020)
-
Factors associated with gustatory threshold for salty taste in peritoneal dialysis patients
Renal Replacement Therapy (2019)
-
Hypertension as a Metabolic Disorder and the Novel Role of the Gut
Current Hypertension Reports (2019)