Abstract
Although adrenomedullin (AM) is a potent hypotensive peptide that acts mainly as a vasodilative and proliferation inhibitory factor, there have been few hemodynamic studies on AM in humans, especially concerning arterial stiffness and hormonal effects. In addition, AM is a suppressive factor in insulin resistance, suggesting that the effects of AM in a state of insulin resistance are important. To evaluate the effects of AM in humans, 28 participants were intravenously administered AM (5 pmol min−1 kg−1) for 90 min. They also received a representative vasodilator drug, nicardipine, as a reference drug. Blood pressure, heart rate, pulse wave velocity (PWV) and blood flow were monitored throughout the experiment. Hormonal changes were also monitored by blood tests. The effects of AM were compared with those of nicardipine. In addition, the effects of AM were re-evaluated against insulin resistance state. AM and nicardipine produced the same level of hypotension, but AM showed a more potent ability to increase heart rate, blood flow and cardiac output and reduce PWV. AM and nicardipine similarly stimulated plasma noradrenaline and renin activity. However, in the state of insulin resistance, favorable effects of AM on aortic stiffness were blunted and differences between AM and nicardipine disappeared. Furthermore, there was a significant correlation between maximum changes in the PWV induced by AM and the homeostasis model assessment of insulin resistance index (r=0.58, P=0.001). Our results suggest that AM may improve arterial stiffness and act as a compensatory factor against arterial sclerosis. Moreover, decreased reactivity of AM may participate in the progression of arterial sclerosis in insulin resistance.
Similar content being viewed by others
Introduction
Adrenomedullin (AM) is a potent hypotensive peptide found ubiquitously in tissues and organs, especially in cardiovascular tissues, the kidneys, lungs and endocrine glands. AM has multiple functions in a wide range of tissues and acts mainly as a vasodilative and proliferation inhibitory factor.1 AM also has a role in the development of arterial sclerosis as an inflammatory modulator.2, 3 Recently, it was shown that endogenous AM has a protective effect against cardiovascular injury, possibly through the inhibition of oxidative stress.4 Morphologically, dense manifestation of AM has been detected in macrophages within plaques of atherosclerotic lesions.5 Shinomiya et al.6 reported an association between plasma AM concentration and carotid atherosclerosis in patients with stroke. Furthermore, we previously reported a relationship between plasma AM levels and pulse wave velocity (PWV), an indicator of arterial stiffness, in patients.7 In addition, AM may counteract insulin resistance development through an antioxidative stress factor.8, 9 Insulin resistance is well recognized as a major pathogenetic factor of arterial disorders, including hypertension and arterial sclerosis. Accumulating data suggest that AM acts as an important modulator against arterial sclerosis and organ damage.
Exogenous AM administration has been shown to have beneficial effects in various stages of cardiovascular disease. In normotensive and hypertensive subjects, short-term AM infusion produced hypotension through vasodilation and increased cardiac output.10, 11 AM also improved hemodynamics in heart failure patients. Specifically, AM administration reduced arterial pressure and cardiac filling pressure and also increased cardiac output and renal sodium excretion.12 However, the effect of AM on the arteries, especially large arteries, has not been determined in humans. A sustained increase in arterial stiffness, as demonstrated by increased PWV, is closely correlated with morbidity and mortality in cardiovascular events.13, 14, 15 In this study, we investigated the effect of AM on arterial stiffness in human subjects. In addition, because the effect of AM may be affected by insulin resistance, we evaluated the relationship between the effects of AM and insulin resistance state in these subjects.
Methods
Study subjects
Twenty-eight subjects that were normotensive (n=11), hypertensive (n=9) or diabetic (n=8) received AM. In addition, all subjects received nicardipine as a reference drug at least 1 week after AM. Subjects with one or more of the following conditions were excluded: (1) heart failure (ejection fraction <50%), (2) severe valvular diseases, (3) renal insufficiency (serum creatinine >1.0 mg per 100 ml), (4) peripheral artery diseases and (5) history of cardiovascular events. All subjects were completely free from any kind of drugs. The study was approved by the ethics committee of the institute, and all participants gave written informed consent.
Preparation of human AM
Chemically synthesized human AM was purchased from the Peptide Institute, Osaka, Japan. The homogeneity of human AM was confirmed by reverse-phase high-performance liquid chromatography and amino acid analysis. AM was dissolved in distilled water with 3.75% D-mannitol and 0.05% aminoacetic acid, then sterilized by passage through a 0.22-μm filter (Millipore, Bedford, MA, USA). The chemical nature and content of the human AM in vials were verified by reverse-phase high-performance liquid chromatography.
Study protocol
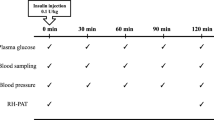
All experiments began at 0900 hours with subjects in a fasted state. Experiments were conducted in our outpatient office, which provided a quiet environment with a constant temperature. A 20-gauge cannula was inserted into the forearm vein for infusion of 0.9% saline. Saline was infused at a rate of 100 ml h−1 throughout the experiments (Figure 1). Baseline measurements were obtained after a 30-min equilibration period. Then AM (5 pmol min−1 kg−1) was intravenously administered at a rate of 5 ml h−1 for 1.5 h followed by saline infusion for 1.5 h. One week after AM infusion, the same subjects were infused with nicardipine (1–1.5 μg min−1 kg−1) as a reference drug. Blood pressure and pulse rate were monitored every 10 min by an automated hemodynamometer on a brachial cuff. Every 15 min, blood pressure, heart rate and PWV were measured using an automatic waveform analyzer (form PWV/ABI, BP-203RPE; Omron Colin, Komaki, Japan), as reported in our previous study.7 Carotid artery pulsation was measured using echo equipment at three time points, as indicated in Figure 1, and the elastic property16 was calculated. Using the Doppler echo method, blood flow in the common carotid artery and segmental renal artery were measured, as was cardiac output. In addition, blood samples were taken at three time points, namely, before, during and after AM infusion (Figure 1). Plasma total and mature AM were measured by specific immunoradiometric assay kits (Shionogi, Osaka, Japan). Plasma concentrations of other hormones were measured using a commercially available laboratory testing service (SRL, Hachioji, Japan).
Statistical analyses
All data were expressed as the mean±s.e.m. Comparisons of parameters between the two groups (AM vs. nicardipine) were carried out using paired Student's t-tests. Comparisons of the time course of parameters between the two groups were carried out by two-way repeated measures analysis of variances followed by Bonferroni/Dunn's multiple comparison tests. A value of P<0.05 was the criterion for statistical significance.
Results
Table 1 presents the baseline characteristics of the participants. AM and nicardipine achieved the same levels of systolic blood pressure reduction in all subjects, as shown in Figure 2. However, AM produced a stronger diastolic blood pressure reduction and heart rate increase when compared with nicardipine (Figures 2a and b). Most interestingly, AM caused a significantly larger reduction of PWV and elastic property of the carotid artery when compared with nicardipine (Figures 2c and d). These changes rapidly recovered after termination of AM or nicardipine administration, except for the prolonged decrease in systolic blood pressure induced by nicardipine. Table 2 summarizes the increase in blood flow and cardiac output after AM or nicardipine administration. Both reagents clearly increased blood flow, but AM was more potent than nicardipine. AM induced significantly larger increases in cardiac output when compared with nicardipine.
Changes in blood pressure (a), heart rate (b), pulse wave velocity (c) and elastic property of the carotid artery (d) during infusion of AM (closed symbols) or nicardipine (open symbols). Data are mean±s.e.m. *P<0.05, **P<0.01, ***P<0.0001 vs. each baseline; #P<0.05, ##P<0.01, ###P<0.0001 vs. nicardipine.
The responses of these parameters were similar among normotensive, hypertensive and diabetic groups of subjects (data not shown). Next, subjects were divided into three groups according to the homeostasis model assessment of insulin resistance (HOMA-IR) index, according to which the highest tertile (HOMA-IR⩾2.0) corresponds to an insulin-resistant state in Japan. HOMA-IR values for each group were as follows: low=0.31–1.39 (n=9), middle=1.43–1.78 (n=10) and high=2.00–6.96 (n=9). As shown in Figure 3, only the reduction in PWV induced by AM was blunted in subjects with the highest HOMA-IR, despite the nearly identical reduction in systolic blood pressure. In this group, the reductions in PWV were similar for AM and nicardipine treatments. This phenomenon was also confirmed by the significant correlation between maximum changes in PWV induced by AM and HOMA-IR (Figure 4). The difference in elastic property reduction between AM and nicardipine treatment was not significant in the high HOMA-IR group (Figure 3c).
Maximum changes in systolic blood pressure (SBP, panel a), pulse wave velocity (PWV, panel b) and elastic property of the carotid artery (Ep, panel c) during infusion of AM (closed column) or nicardipine (open column) in each of the three groups divided by HOMA-IR index. Groups divided by HOMA-IR index include low (n=9), middle (n=10) and high (n=9) index groups. Data are mean±s.e.m. *P<0.05, **P<0.01.
Table 3 summarizes the changes in humoral factors. AM administration produced significant increases in total AM (approximately 2.5-fold) and mature AM (approximately 7-fold) as well as an approximately 40% increase in the second messenger cAMP. AM and nicardipine produced the same degree of increase in noradrenaline and renin activity. There was no significant difference among the HOMA-IR groups for all humoral factor alterations (data not shown). Finally, AM and nicardipine had no effect on insulin and glucose levels.
Discussion
In this study, we confirmed the hemodynamic effects of AM as a vasodilative agent in humans. AM increased heart rate and cardiac output and decreased blood pressure. In addition, AM increased blood flow in carotid and renal arteries. These effects were similar to those of the common vasodilator nicardipine. However, AM produced greater increases in cardiac output and heart rate when compared with nicardipine (Table 2). The ventricular myocardium has abundant AM-binding sites; therefore, AM increases cardiac cAMP.17, 18 This cAMP-dependent mechanism mediates the positive inotropic action of β-adrenergic stimulants. AM also enhances angiotensin-II-induced improvement of systolic function, resulting in a further increase in left ventricular ejection fraction.19 In addition, a cAMP-independent mechanism for the positive inotropic action of AM has been reported.20 These data suggest that increased cardiac output, and probably heart rate, may be attributable not only to the decrease in cardiac afterload but also to the direct positive inotropic action of AM.
PWV is a convenient indicator of arterial stiffness and is applicable in the casual and prognostic estimation of risk for cardiovascular events. We used brachial ankle PWV (baPWV) in this study. As shown for authentic PWV, baPWV correlates well with blood pressure and aging,21 and increased baPWV is associated with cardiovascular diseases and risk factors.22 More importantly, high baPWV values predict poor prognosis in subjects.23 Conversely, improvement of PWV by antihypertensive therapy may reduce the incidence of cardiovascular events.15 Strong expression of AM is found ubiquitously in blood vessels where AM functions as a vasodilator, coordinating with other vasodilators, such as nitric oxide, to regulate vascular tonus.1 AM is suggested to be a significant modulator of arterial stiffness, decreasing blood pressure and vascular wall tension and preventing future wall remodeling. In this study, AM had a greater effect on aortic stiffness, as assessed by baPWV or elastic property, when compared with a common vasodilator Ca2+ channel blocker (Figure 2). This feature may contribute to a vascular protective or compensatory function of AM against vascular deterioration and resulting vascular events.
baPWV is mainly altered by blood pressure, but other factors, such as increased heart rate, cardiac output and sympathetic nerve activity, may also increase baPWV. Indeed, the effect of nifedipine on baPWV was reduced by increased sympathetic activity.24 Although decreases in systolic blood pressure were well matched in nicardipine and AM treatments, AM showed greater baPWV reduction despite larger increments in heart rate and cardiac output when compared with nicardipine (Figure 2 and Table 2). The increases in catecholamines and renin activity were equivalent in both treatments (Table 3). These alterations probably reduced or inhibited the decrease in baPWV in nicardipine treatment. Alternatively, it is conceivable that AM has greater potency against negative alterations to increase baPWV when compared with nicardipine.
AM and nicardipine produced a larger blood pressure reduction in hypertensive participants when compared with normotensive or diabetic participants, which is a common feature of hypotensive reagents (data not shown). However, other hemodynamic effects of AM and nicardipine evaluated within each treatment were essentially the same for each subgroup of participants. We evaluated potentially influential factors in the effects of AM, and we found that only the insulin resistance interfered with the effects of AM. Insulin resistance is an aggravating factor in vascular function and is an underlying cause of cardiovascular diseases. Insulin resistance also influences the sensitivity or efficacy of many drugs and bioactive substances. More importantly, increased arterial stiffness is commonly found in representative insulin resistance states, namely, metabolic syndrome and diabetes.25, 26, 27 As shown in Figures 3 and 4, favorable effects of AM on arterial stiffness were blunted in a state of insulin resistance. AM is thought to function as a suppressive factor against insulin resistance.8, 9 As such, plasma concentration of AM was progressively increased in patients with impaired glucose tolerance, diabetes and diabetes with nephropathy.28 In addition, an increase in AM was related to multiple metabolic factors.28 AM and insulin resistance may conflict with each other. Specifically, decreased reactivity of AM may contribute to increased arterial stiffness during insulin resistance, and this alteration may accelerate the progression of arterial sclerosis in insulin resistance. However, this intervention is only a temporary treatment, so further studies are required to clarify the relationship between AM and insulin resistance.
Plasma concentration of total AM was increased approximately 2.4-fold above the control value after AM administration (Table 3). This level of AM concentration has been found in renal failure or heart failure patients,29 so the level of AM used was pathophysiological, not pharmacological. AM administration also increased cAMP, which is a second messenger of AM, approximately 1.4-fold above the control value. Similar changes in AM and cAMP have been reported in previous studies.10, 11, 12 AM and nicardipine also produced similar hormonal alterations, namely, stimulated sympathetic activity and renin release, which was also observed in another study.10, 11 The only difference between the effects of AM and nicardipine in our study was on aldosterone release. AM tended to inhibit aldosterone release despite increased renin activity, although this difference was not significant (P=0.051, Table 3). AM did not change aldosterone levels in healthy volunteers or patients with essential hypertension,10, 11 but AM suppressed increased aldosterone levels in patients with heart failure.12 Furthermore, AM may have renin-independent suppressive potency for aldosterone release, and this feature should be elucidated in future studies.
In conclusion, exogenous AM and Ca2+ channel blocker nicardipine caused similar vasodilations in humans, accompanied with resemble interactions with the renin–angiotensin and sympathetic nervous systems. However, AM had a greater potency in its cardiac inotropic action when compared with nicardipine. AM also more effectively decreased arterial stiffness, but the effect was weakened to a similar level as for nicardipine in a state of insulin resistance. Our results support the hypothesis that AM may modulate vasoactive substances and vascular tonus and also have a role in pathophysiological conditions, such as an insulin resistance state.
References
Eto T, Kato J, Kitamura K . Regulation of production and secretion of adrenomedullin in the cardiovascular system. Regl Pept 2002; 112: 61–69.
Elsasser TH, Kahl S . Adrenomedullin has multiple roles in disease stress: development and remission of the inflammatory response. Microsc Res Tech 2002; 57: 120–129.
Wong LY, Cheung BM, Li Y-Y, Tang F . Adrenomedullin is both proinflammatory and anti-inflammatory: its effects on gene expression and secretion of cytokines and macrophage migration inhibitory factor in NR8383 macrophage cell line. Endocrinology 2005; 146: 1321–1327.
Shimosawa T, Shibagaki Y, Ishibashi K, Kitamura K, Kangawa K, Kato S, Ando K, Fujita T . Adrenomedullin, an endogenous peptide, counteracts cardiovascular damage. Circulation 2002; 105: 106–111.
Marutsuka K, Hatakeyama K, Sato Y, Yamashita A, Sumiyoshi A, Asada Y . Immunohistological localization and possible functions of adrenomedullin. Hypertens Res 2003; 26 (Suppl): S33–S40.
Shinomiya K, Ohmori K, Ohyama H, Hosomi N, Takahashi T, Osaka K, Kohno M . Association of plasma adrenomedullin with carotid atherosclerosis in chronic ischemic stroke. Peptides 2001; 22: 1873–1880.
Kita T, Kitamura K, Hashida S, Morishita K, Eto T . Plasma adrenomedullin is closely correlated with pulse wave velocity in middle-aged and elderly patients. Hypertens Res 2003; 26: 887–893.
Shimosawa T, Ogihara T, Matsui H, Asano T, Ando K, Fujita T . Deficiency of adrenomedullin induces insulin resistance by increasing oxidative stress. Hypertension 2003; 41: 1080–1085.
Xing G, Shimosawa T, Ogihara T, Matsui H, Itakura K, Qingyou X, Asano T, Ando K, Fujita T . Angiotensin II-induced insulin resistance is enhanced in adrenomedullin-deficient mice. Endocrinology 2004; 145: 3647–3651.
Lainchbury JG, Troughton RW, Lewis LK, Yandle TG, Richards AM, Nicholls MG . Hemodynamic, hormonal, and renal effects of short-term adrenomedullin infusion in healthy volunteers. J Clin Endocrinol Metab 2000; 85: 1016–1020.
Troughton RW, Levis LK, Yandle TG, Richards AM, Nicholls MG . Hemodynamic, hormone, and urinary effects of adrenomedullin infusion in essential hypertension. Hypertension 2000; 36: 588–593.
Nagaya N, Satoh T, Nishikimi T, Uematsu M, Furuichi S, Sakamaki F, Oya H, Kyotani S, Nakanishi N, Goto Y, Masuda Y, Miyatake K, Kangawa K . Hemodynamic, renal, and hormonal effects of adrenomedullin infusion in patients with congestive heart failure. Circulation 2000; 101: 498–503.
Blacher J, Asmar R, Djane S, London GM, Safar ME . Aortic pulse wave velocity as a marker of cardiovascular risk in hypertensive patients. Hypertension 1999; 32: 570–574.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Guerin AP, Blacher J, Pannier B, Marchais SJ, Safar ME, London GM . Impact of aortic stiffness attenuation on survival of patients in end-stage renal failure. Circulation 2001; 103: 987–992.
Blankenhorn DH, Chin HP, Conover DJ, Nessim SA . Ultrasound observation on pulsation in human carotid artery lesions. Ultrasound Med Biol 1988; 14: 583–587.
Owji AA, Smith DM, Coppock HA, Morgan DG, Bhogal R, Ghatel MA, Bloom SR . An abundant and specific binding site for the novel vasodilator adrenomedullin in the rat. Endocrinology 1995; 136: 2127–2134.
Ihara T, Ikeda U, Tate Y, Ishibashi S, Shimada K . Positive inotropic effects of adrenomedullin on rat papillary muscle. Eur J Pharmacol 2000; 390: 167–172.
Luodonpää M, Leskinen H, Ilves M, Vuolteenaho O, Ruskoaho H . Adrenomedullin modulates hemodynamic and cardiac effects of angiotensin II in conscious rats. Am J Physiol 2004; 286: R1085–R1092.
Szokodi I, Kinnunen P, Tavi P, Weckstrom M, Toth M, Ruskoaho H . Evidence for cAMP-independent mechanisms mediating the effects of adrenomedullin, a new inotropic peptide. Circulation 1998; 97: 1062–1070.
Tomiyama H, Yamashina A, Arai T, Hirose K, Koji Y, Chikamori T, Hori S, Yamamoto Y, Doba N, Hinohara S . Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement—a survey of 12517 subjects. Atherosclerosis 2003; 166: 303–309.
Yamashina A, Tomiyama H, Arai T, Hirose H, Koji Y, Hirayama Y, Yamamoto Y, Hori S . Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens Res 2003; 26: 615–622.
Kitahara T, Ono K, Tsuchida A, Kawai H, Shinohara M, Ishii Y, Koyanagi H, Noguchi T, Matsumoto T, Sekihara T, Watanabe Y, Kanai H, Ishida H, Nojima Y . Impact of brachial-ankle pulse wave velocity and ankle-brachial blood pressure index on mortality in hemodialysis patients. Am J Kidney Dis 2005; 46: 688–696.
Munakata M, Nagasaki A, Nunokawa T, Sakuma T, Kato H, Yoshinaga K, Toyota T . Effects of valsartan and nifedipine coat-core on systemic arterial stiffness in hypertensive patients. Am J Hypertens 2004; 17: 1050–1055.
Ghiadoni L, Penno G, Giannarelli C, Plantinga Y, Bernardini M, Pucci L, Miccoli R, Taddei S, Salvetti A, Del Prato S . Metabolic syndrome and vascular alterations in normotensive subjects at risk of diabetes mellitus. Hypertension 2008; 51: 440–445.
Kovaite M, Petrulioniene Z, Ryliskyte L, Badariene J, Dzenkeviciute V, Cypiene A, Laucevicius A, Polena S, Gintautas J . Systemic assessment of arterial wall structure and function in metabolic syndrome. Proc West Pharmacol Soc 2007; 50: 123–130.
El Feghali R, Topouchian J, Pannier B, Asmar R . Ageing and blood pressure modulate the relationship between metabolic syndrome and aortic stiffness in never-treated essential hypertensive patients. A comparative study. Diabetes Metab 2007; 33: 183–188.
Lim SC, Morgenthaler NG, Subramanian T, Wu YS, Goh SK, Sum CF . The relationship between adrenomedullin, metabolic factors, and vascular function in individuals with type 2 diabetes. Diabetes Care 2007; 30: 1513–1519.
Nishikimi T . Adrenomedullin in cardiovascular disease. Adv Pharmacol 1998; 42: 599–603.
Acknowledgements
This study was supported in part by Health and Labor Science Research Grants for Translational Research from the Ministry of Health, Labor and Welfare, Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Previous presentation of this article: Partial data concerning nicardipine administration were presented in a previous paper (Hypertens Res 2005; 28: 959–964).
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kita, T., Suzuki, Y. & Kitamura, K. Hemodynamic and hormonal effects of exogenous adrenomedullin administration in humans and relationship to insulin resistance. Hypertens Res 33, 314–319 (2010). https://doi.org/10.1038/hr.2009.236
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.236
Keywords
This article is cited by
-
Translational studies of adrenomedullin and related peptides regarding cardiovascular diseases
Hypertension Research (2022)
-
Plasma adrenomedullin level in children with obesity: relationship to left ventricular function
World Journal of Pediatrics (2018)
-
Adrenomedullin Therapy in Patients with Refractory Ulcerative Colitis: A Case Series
Digestive Diseases and Sciences (2016)