Abstract
The long-term antihypertensive efficacy and safety of losartan/hydrochlorothiazide (HCTZ) combinations have not been appropriately evaluated in Japan. In this study, treated hypertensive patients taking angiotensin-receptor blocker (ARB) or angiotensin-converting enzyme inhibitor (ACEI) regimens not at blood pressure (BP) goals proposed by the Japanese Society of Hypertension (JSH) were switched to losartan/HCTZ combinations and followed for 1 year. Data analysis included 244 patients aged 64.5±10.7 years, 56% male, 27% with diabetes mellitus and 36% with dyslipidemia. Pre-switching BP 157±16/88±10 mm Hg promptly decreased and maintained a steady state, reaching 132±15/77±9 mm Hg (P<0.001) 1 year later. After 1 year of treatment, 50% of patients cleared the goals of the JSH guideline for systolic BP and 79% for diastolic BP. Patients with maximal doses of ARBs tended to show larger decreases in BP (159±11/90±10 to 128±10/75±8 mm Hg, P<0.001, n=32). Clinical and laboratory adverse events were reported for 29 patients (11%), but serious abnormalities were not observed. In particular, plasma levels of uric acid (UA) were well-maintained for 1 year, and significant decreases in UA were observed in patients with higher levels of UA (⩾7.0 mg dl−1). Losartan/HCTZ combinations showed strong and steady hypotensive abilities and acceptable safety and tolerability in patients currently not at BP goals with regimens including ARBs or ACEIs in Japan.
Similar content being viewed by others
Introduction
Guidelines for hypertension treatment, including those of the Japanese Society of Hypertension (JSH), have recommended strict blood pressure (BP) control, with the aim of improving protection against cardiovascular and renal accidents.1, 2 However, considerable numbers of hypertensive patients have not achieved the recommended goals of BP in Japan.3 The JSH guideline recommends angiotensin-receptor blockers (ARBs), angiotensin-converting enzyme inhibitors (ACEIs), Ca2+ channel blockers (CCB), β-blockers and diuretics as first-line drugs for hypertensive treatment.1 The guideline also recommends appropriate combinations of the drugs, in particular low-dose (quarter to half dose) diuretics are recommended as an important candidate for satisfactory BP control.1 However, the prescribing rate of diuretics was quite low (under 10%) in cases of monotherapy or combination therapy for hypertension in Japan.4 The principal reason for reluctance to prescribe thiazide diuretics is the metabolic side effects of the drugs. However, low-dose thiazide diuretics retain their hypotensive abilities with minimal side effects.5 Therefore, proper application of low-dose diuretics, particularly in combination therapies, is desirable in Japan to improve BP control.
A fixed dose combination of losartan (50 mg)/hydrochlorothiazide (HCTZ, 12.5 mg) (Preminent; Banyu/Merck, Tokyo, Japan) is the first combination of an ARB and a diuretic for hypertensive treatment in Japan, and is expected to be effective and safe from the pharmacological properties of both drugs. However, limited data were available on the combination drug in Japan, especially with regard to long-term treatment, large numbers of patients and its use in a clinical setting.6, 7, 8 We organized a study group mainly consisting of clinical physicians in Miyazaki Prefecture in Japan (Preminent Assigned League in Miyazaki by Primary care physicians: PALM-1 study group), and evaluated the efficacy and safety of the fixed combination of losartan/HCTZ for patients with essential hypertension for 1 year.
Methods
Study subjects
This study was conducted at 43 centers for the PALM-1 study group (Appendix). Patients with essential hypertension (20–79 years old) were considered for screening and potential recruitment into the trial. They had visited the attending clinics from February 2007 to March 2008 and had not reached BP goals with antihypertensive therapy regimens, including ARBs or ACEIs, but not diuretics, over 1 month. Patients were excluded from the study if there was any evidence of secondary hypertension, renal failure (serum creatinine ⩾2.0 mg dl−1), severe liver dysfunction and symptomatic heart failure (New York Heart Association functional class-III or IV for dyspnea at exertion). Patients with concomitant use of two or more ARBs and/or ACEIs and any type of diuretics were also excluded.
Study protocol
The study was conducted in accordance with the principles of the declaration of Helsinki. The investigational protocol was approved by the ethics committee for human studies at the University of Miyazaki. Informed consent was obtained from all patients prior to recruitment.
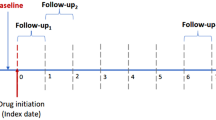
This was an open-label, multicenter study consisting of a 3-month screening/baseline period and 1-year treatment period. Under antihypertensive treatment with regimens including ARBs or ACEIs, at least two BP measurements were conducted within 3 months of the baseline period to confirm baseline BP measurements were over the recommended BP goals of the JSH. The BP goals were 130/85 mm Hg for patients aged less than 65 years, 140/90 mm Hg for those aged 65 years or more, 130/80 mm Hg for patients with diabetes and/or chronic kidney disease and/or history of myocardial infarction, and 140/90 mm Hg for patients with a history of stroke.1 After screening 311 patients, 266 entered the trial. Then only ARBs or ACEIs were switched to the fixed dose combination of losartan/HCTZ and patients were followed for 1 year. Changed prescriptions were kept for the initial 3 months and then, if needed, adjustments of antihypertensive drugs were allowed except for ARBs, ACEIs and diuretics. Symptoms, sitting BP, pulse rate and blood tests, including potassium, uric acid (UA), lipid profile, creatinine, glucose, hemoglobin-A1c (HbA1c, diabetic patients only), were evaluated every 3 months. Major complications were also evaluated. The criteria for diabetes and dyslipidemia were as follows: diabetes, using antiglycemic drugs or fasting blood glucose ⩾126 mg dl−1; dyslipidemia, using lipid-lowering drugs or total cholesterol ⩾220 mg dl−1 and/or high-density lipoprotein-cholesterol <40 mg dl−1, and/or triglyceride ⩾150 mg dl−1.
Statistical analysis
All data are expressed as mean±s.d. The significance of differences was evaluated by one-factor analysis of variance with repeated measures on the time course of variables followed by Bonferroni/Dunn post hoc comparison tests. Comparisons of parameters among subgroups were made by unpaired Dunnet's C-test or analysis of variance followed by Scheffe's post hoc comparison test. P-value <0.05 was the criterion for statistical significance.
Results
As indicated in Figure 1, 22 of the 266 enrolled patients dropped out within the first 3 months. The remaining 244 patients were considered as full analytical objects. Finally, 222 patients completed the entire trial and were used for evaluation of efficacy.
The baseline characteristics of the study population are summarized in Table 1. Patients’ age was 64.5±10.7 years, 56% were male and major complications included 27% of patients with diabetes, 36% with dyslipidemia and 18% with mild heart failure. Pre-prescribed ARBs or ACEIs were well distributed from among drugs on the market and, noteworthy, the average doses per day of the drugs were very close to the usual dosage of each drug (Table 1). ARBs or ACEIs were used as monotherapy for 93 patients (38%) and as combined therapy, mainly with CCB, for 151 patients (62%). Other pre-prescribed drugs were as follows and these drugs were not altered after introduction of the losartan/HCTZ combination: antiglycemic drugs for 38 of 266 patients (37 of 222), lipid-lowering drugs for 58 of 266 (53 of 222) and UA-lowering drugs for 14 of 266 (14 of 222).
The time course of BP in all patients is illustrated in Figure 2. Baseline BP 157±16/88±10 mm Hg significantly decreased to 134±14/77±9 mm Hg at 3 months (P<0.001) (fixed prescription period), and then steady levels were maintained throughout the remaining treatment period. The respective goals of BP were cleared by 50% of the patients for systolic BP and 79% of the patients for diastolic BP in the final assessment 1 year later. Interestingly, 32 of 222 patients who were switched from the maximum dose of ARBs showed a similar to larger decrease in BP as compared with patients with low-to-medium dose of ARBs (Figure 3). There was a significant difference in the changes of BP from 3 months to 1 year between patients switched from low-to-medium dose of ARBs and maximum dose of ARBs (at 1 year: systolic BP, 23±19 vs. 31±13 mm Hg, P=0.005; diastolic BP, 10±11 vs. 15±10 mm Hg, P=0.027). As shown in Figure 4, similar and significant decreases in systolic and diastolic BP were achieved in all patients grouped based on pre-prescribed drugs at 1 year. Also there was no difference in BP changes among all ARBs and ACEI-receiving patients. The systolic and diastolic BPs at 0 and 12 month (changes of the BPs) for each drug were as follows: losartan, 154±17 to 135±10 mm Hg (−19±17 mm Hg, P<0.001) and 87±11 to 78±8 mm Hg (−9±10 mm Hg, P<0.001); candesartan, 156±14 to 131±14 mm Hg (−24±17 mm Hg, P<0.001) and 87±9 to 76±9 mm Hg (−11±10 mm Hg, P<0.001); valsartan, 160±16 to 134±13 mm Hg (−26±18 mm Hg, P<0.001) and 89±9 to 77±8 mm Hg (−12±10 mm Hg, P<0.001); telmisartan, 156±17 to 132±20 mm Hg (−24±15 mm Hg, P<0.001) and 85±12 to 75±11 mm Hg (−10±8 mm Hg, P<0.001); olmesartan, 153±18 to 129±14 mm Hg (−24±24 mm Hg, P<0.001) and 88±15 to 77±10 mm Hg (−11±15 mm Hg, P<0.001); and ACEIs, 159±16 to 133±19 mm Hg (−26±20 mm Hg, P<0.001) and 87±9 to 76±12 mm Hg (−11±12 mm Hg, P=0.001). There were very limited number of alterations in antihypertensive drugs after 3 months (8 of 222): two terminations of CCBs, one decrease of CCB, four introductions of low doses of CCBs for patients receiving low-to-medium dose of ARBs and one introduction of atenolol (12.5 mg) for a patient with maximum dose of ARBs.
To determine the difference in receptivity to losartan/HCTZ between specific backgrounds of the patients, we compared BP changes at 1 year for various subgroups. However, there was no difference among the subgroups and specific factors contributing to resistance against losartan/HCTZ were not detected. For example, if patients are grouped according presence (+) or absence (−) of diabetes (D) and obesity (O) (body mass index, ⩾25 kg m−2), decreases in systolic BP were 24±18 mm Hg (D+/O+, n=35), 23±17 mm Hg (D+/O−, n=27), 24±15 mm Hg (D−/O+, n=63) and 25±21 mm Hg (D−/O−, n=97). This indicates that the losartan/HCTZ combination is effective even for patients with diabetes and obesity.
Remarkable changes were not observed in metabolic parameters after 1 year of treatment with losartan/HCTZ. Figure 5 shows changes in UA levels in all patients (5.46±1.43 to 5.62±1.43 mg dl−1) and subgroups with high levels of UA at baseline and others. UA level was slightly increased in patients with relatively low levels of UA (UA < 7.0 mg dl−1, middle panel): 5.02±1.11 to 5.37±1.34 mg dl−1 (P<0.001). But, interestingly, UA level was significantly decreased in patients with high level of UA (UA ⩾ 7.0 mg dl−1, right panel): 7.66±0.57 to 6.88±1.16 mg dl−1 (P=0.004). Other changes (month 0 to 12) concerning parameters in blood tests are summarized in Table 2.
Adverse events were observed in 29 of 266 patients (10.9%) who received the losartan/HCTZ combination, including accidental events, and 16 (5.4%) discontinued the losartan/HCTZ combination, while the remaining 13 patients continued receiving the drug. Among the 16 patients who discontinued, 13 events (4.9%) were considered possibly, probably or definitely drug-related. Laboratory abnormalities were observed for 13 patients. The 13 drug-related adverse events included three cases of hypokalemia, two patients who complained of skin rash, one patient who suffered photosensitive dermatoses, worsening of diabetes in one patient and excessive BP depression in six patients. Four patients of 266 discontinued the losartan/HCTZ combination because of patient circumstances or requests, without adverse events. No death occurred during the study.
Discussion
Only 42% of hypertensive patients reached the guideline BP goals in the J-HOME (Japan Home versus Office Blood Pressure Measurement Evaluation) study.3 Mori et al.4 reported that hypertensive patients attaining BP under 140/90 mm Hg by monotherapy were limited to 34.0% with ARBs and 40.3% with CCBs. Additionally, strict BP goals (130/80 mm Hg) are recommended for hypertensive patients with diabetes, chronic kidney disease and old myocardial infarction.1 Addition of low-dose diuretics is recommended as a key combination therapy for better BP control in the JSH guideline.1 However, the prescription rate of diuretics remains low in Japan, for example, 9.3% in the J-HOME study.9 Additionally, combination therapy with diuretics seems to contribute to organ protection. Many large-scale clinical trials have shown organ-protective effects of losartan, and, importantly, the majority of patients in these trials concomitantly used diuretics, for example, 72% in the LIFE (Losartan Intervention For Endpoint) trial and 84% in the RENAAL (Reduction of Endpoints in NIDDM with the Angiotensin-II Antagonist Losartan) trial.10, 11 Therefore, an acceptable and safe way to introduce low doses of diuretics for hypertension therapy is desirable in Japan.
The losartan/HCTZ combination is composed of losartan, which displays superior activity under the activated renin–angiotensin system12 and a thiazide-diuretic that activates renin–angiotensin system through a diuretic effect,13 so this combination is expected to be efficient in BP lowering by the synergistic effect of both the drugs. In this study, BP was decreased by 23±17/11±10 mm Hg at 3 months and 24±18/11±11 mm Hg at 12 months after switching from ARBs or ACEIs alone to the losartan/HCTZ combination for patients who did not reach the BP goal with regimens including ARBs or ACEIs. Similar decreases in BP were observed with all types of pre-prescribed ARBs and ACEIs (Figure 4), and thus these strong and steady decreases in BP seem to depend on the HCTZ ‘add-on’ effect. Salt intake of the Japanese is relatively high,14 and thus excess salt may suppress the renin–angiotensin system and disturb the ability of ARBs or ACEIs. In particular, this possibility seems high for patients whose BP was not satisfactorily suppressed by ARBs or ACEIs. Alternatively, HTCZ probably works well in that situation, and this possibility is indirectly supported by evidence that patients pre-using the maximum dose of ARBs showed larger decreases in BP than those using the low-to-medium dose of ARBs following introduction of the losartan/HCTZ combination (Figures 2 and 3). Also this synergistic effect is effective in a comprehensive range of patients; over 90% of patients showed meaningful reductions in diastolic BP (⩾10 mm Hg) and 79% of patients reached the BP goals of the JSH guideline, and thus specific cases of diabetes or obesity resistant against losartan/HCTZ combination were not detected.
Diuretics such as HCTZ have been avoided in Japan for fear of their negative effects on metabolic parameters.4 In particular, hypokalemia and increase in UA are associated with HCTZ. In combination with losartan, hypokalemia may be canceled by the anti-aldosterone effect of ARBs and UA elevation may be enfeebled by the UA-decreasing ability of losartan. Losartan has a unique effect of stimulating UA excretion in urine by suppressing UA transporters URAT1 and URATv1, with a resulting decrease in the serum levels of UA.15, 16 In this study, these expectations were well achieved and potassium and UA levels were kept within normal ranges. Additionally, a significant decrease in UA was observed for patients with high levels of UA (Figure 5). Except for losartan, clinical doses of ARBs do not have suppressive properties on the UA transporters.17 This property of losartan should be profitable in combination with HCTZ.
Another concern with HCTZ is worsening of glucose metabolism. A recent cohort study in Taiwan showed that diuretic or β-blocker monotherapy increased the risk of new-onset diabetes, but combination therapies composed of diuretics or β-blocker with ACEI or ARB did not. Conversely, there was a decrease in the risk of new-onset diabetes.18 In this study, blood glucose and HbA1c levels were stable in patients with diabetes (Table 2), as was glucose level in all patients, and so the losartan/HCTZ combination appears to be safe for glucose metabolism. However, the sensitivity of glucose metabolism under diuretics use could be changed by gene variation,19 and thus there may be small numbers of susceptible patients. In fact, one patient dropped out because of worsening of diabetes in this study. Therefore, careful monitoring of glucose metabolism is required.
Fixed dose combination drugs decrease the number of pills taken and may contribute to better adherence. Patients on a fixed-combination regimen showed better persistence after 1 year of antihypertensive treatment, namely 58% for combination therapy with ACEI plus diuretics in two pills, and 70% for one-pill fixed combination.20 In this study, a limited number of patients, 44 of 266 (16.5%), dropped out despite the clinical setting, so this fixed combination could be beneficial in clinical use.
In summary, a fixed dose combination of losartan/HCTZ for 1 year of treatment in a clinical setting resulted in sufficient and steady BP decrease in a majority of Japanese hypertensive patients who had not been controlled with a regimen including ARBs or ACEIs. Also this combination showed acceptable safety and tolerability. A fixed dose combination of losartan/HCTZ is an available tool to introduce low-dose diuretics for treatment of uncontrolled hypertension in Japan.
References
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M, Imai Y, Imaizumi T, Ito S, Iwao H, Kario K, Kawano Y, Kim-Mitsuyama S, Kimura G, Matsubara H, Matsuura H, Naruse M, Saito I, Shimada K, Shimamoto K, Suzuki H, Takishita S, Tanahashi N, Tsuchihashi T, Uchiyama M, Ueda S, Ueshima H, Umemura S, Ishimitsu T, Rakugi H, on behalf of The Japanese Society of Hypertension Committee. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32: 3–107.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O’Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B, Management of Arterial Hypertension of the European Society of Hypertension; European Society of Cardiology. 2007 Guidelines for the Management of Arterial Hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
Ohkubo T, Obara T, Funahashi J, Kikuya M, Asayama K, Metoki H, Oikawa T, Takahashi H, Hashimoto J, Totsune K, Imai Y, J-HOME Study Group. Control of blood pressure as measured at home and office, and comparison with physicians’ assessment of control among treated hypertensive patients in Japan: first report of the Japan Home versus Office Blood Pressure Measurement Evaluation (J-HOME) study. Hypertens Res 2004; 27: 755–763.
Mori H, Ukai H, Yamamoto H, Saitou S, Hirao K, Yamauchi M, Umemura S . Current status of antihypertensive prescription and associated blood pressure control in Japan. Hypertens Res 2006; 29: 143–151.
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 2002; 288: 2981–2997.
Shimosawa T, Gohchi K, Yatomi Y, Fujita T . Effectiveness of add-on low-dose diuretics in combination therapy for hypertension: losartan/hydrochlorothiazide vs candesartan/amlodipine. Hypertens Res 2007; 30: 831–837.
Saruta T, Ogihara T, Matsuoka H, Suzuki H, Toki M, Hirayama Y, Nonaka K, Takahashi K . Antihypertensive efficacy and safety of fixed-dose combination therapy with losartan plus hydrochlorothiazide in Japanese patients with essential hypertension. Hypertens Res 2007; 30: 729–739.
Minami J, Abe C, Akashiba A, Takahashi T, Kameda T, Ishimitsu T, Matsuoka H . Long-term efficacy of combination therapy with losartan and low-dose hydrochlorothiazide in patients with uncontrolled hypertension. Int Heart J 2007; 48: 177–186.
Murai K, Obara T, Ohkubo T, Metoki H, Oikawa T, Inoue R, Komai R, Horikawa T, Asayama K, Kikuya M, Totsune K, Hashimoto J, Imai Y, J-Home Study Group. Current usage of diuretics among hypertensive patients in Japan: the Japan Home versus Office Blood Pressure Measurement Evaluation (J-HOME) study. Hypertens Res 2006; 29: 857–863.
Dahlöf B, Devereux RB, Kjeldsen SE, Julius S, Beevers G, de Faire U, Fyhrquist F, Ibsen H, Kristiansson K, Lederballe-Pedersen O, Lindholm LH, Nieminen MS, Omvik P, Oparil S, Wedel H, LIFE Study Group. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002; 359: 995–1003.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S, RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345: 861–869.
Wong PC, Price WA, Chiu AT, Duncia JV, Carini DJ, Wexler RR, Johnson AL, Timmermans PB . Nonpeptide angiotensin II receptor antagonists. VIII. Characterization of functional antagonism displayed by DuP 753, an orally active antihypertensive agent. J Pharmacol Exp Ther 1990; 252: 719–725.
Lijnen P, Fagard R, Staessen J, Amery A . Effect of chronic diuretic treatment on the plasma renin–angiotensin–aldosterone system in essential hypertension. Br J Clin Pharmacol 1981; 12: 387–392.
Brown IJ, Tzoulaki I, Candeias V, Elliott P . Salt intakes around the world: implications for public health. Int J Epidemiol 2009; 38: 791–813.
Enomoto A, Kimura H, Chairoungdua A, Shigeta Y, Jutabha P, Cha SH, Hosoyamada M, Takeda M, Sekine T, Igarashi T, Matsuo H, Kikuchi Y, Oda T, Ichida K, Hosoya T, Shimokata K, Niwa T, Kanai Y, Endou H . Molecular identification of a renal urate anion exchanger that regulates blood urate levels. Nature 2002; 417: 447–452.
Anzai N, Ichida K, Jutabha P, Kimura T, Babu E, Jin CJ, Srivastava S, Kitamura K, Hisatome I, Endou H, Sakurai H . Plasma urate level is directly regulated by a voltage-driven urate efflux transporter URATv1 (SLC2A9) in humans. J Biol Chem 2008; 283: 26834–26838.
Iwanaga T, Sato M, Maeda T, Ogihara T, Tamai I . Concentration-dependent mode of interaction of angiotensin II receptor blockers with uric acid transporter. J Pharmacol Exp Ther 2007; 320: 211–217.
Liou YS, Ma T, Tien L, Lin CM, Jong GP . The relationship between antihypertensive combination therapies comprising diuretics and/or beta-blockers and the risk of new-onset diabetes: a retrospective longitudinal cohort study. Hypertens Res 2009; 32: 496–499.
Bozkurt O, de Boer A, Grobbee DE, de Leeuw PW, Kroon AA, Schiffers P, Klungel OH . Variation in renin–angiotensin system and salt-sensitivity genes and the risk of diabetes mellitus associated with the use of thiazide diuretics. Am J Hypertens 2009; 22: 545–551.
Dezii CM . A retrospective study of persistence with single-pill combination therapy vs concurrent two-pill therapy in patients with hypertension. Manag Care 2000; 9 (Suppl): 2–6.
Acknowledgements
This study was supported by foundation for multicenter clinical study of Japan Heart Foundation.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix
Appendix
Members of the PALM-1 study group: Takao Ayabe (Ayabe Iin), Susumu Chiyotanda (Chiyoda Hospital), Tanenao Eto (Miyazaki Prefectural Health Foundation), Takuma Etoh (Etoh Clinic), Shuji Fukuoka (Fukuoka Clinic), Yoshiomi Hamada (Takao Hamada Iin), Akihiko Higa (Higa Naika Ichouka), Yoshinari Ichiki (Ichiki Naika Geka Iin), Naoto Ishikawa (Ishikawa Clinic), Sumito Kariya (Kariya Iin), Toshiro Kariya (Kariya Geka Ichouka), Johji Kato (Frontier Science Research Center, University of Miyazaki), Toshihiro Kita, Kazuo Kitamura (Department Of Internal Medicine, Circulatory and Body Fluid Regulation, Faculty of Medicine, University of Miyazaki), Kenji Kodama (Kodama Naika Clinic), Hideyuki Komidori (Komidori Naika Clinic), Kouichi Kondo (Kondo Naika Clinic), Munetoshi Kuroki (Kuroki Naika Iin), Kazunobu Maeda (Maeda Iin), Masakazu Maeno (Maeno Clinic), Fumiaki Matsuoka (Matsuoka Naika Iin), Toshio Mimata (Mimata Hospital), Koji Miyamoto (Ikedadai Clinic), Junichi Miyata (Miyata Naika Iin), Kazuhito Morisako (Morisako Ichouka Naika), Hozumi Nagakura (Nagakura Iin), Toshiro Nagoshi (Nagoshi Naika), Masafumi Nakashima (Nakashima Iin), Hiromi Niina (Niina Naika Junkankika), Toshifumi Nobe (Nobe Iin), Katsuhiro Nozaki (Nozakihigashi Hospital), Toshitaka Ohkubo (Ohkubo Clinic), Teruhiko Oogi (Oogi Iin), Tatsumi Oshikawa (Oshikawa Hospital), Akira Sasaki (Sasaki Naika), Kouji Sasaki (Sasaki Iin), Takehiko Shida (Shida Naika Ichouka Iin), Toru Shimokubo (Sakoda Hospital), Sadahiko Sonoda (Nojiri Central Hospital), Toshifumi Taguchi (Taguchi Junkankika Naika Clinic), Noboru Tamaki (Tamaki Clinic), Johji Tanaka (Kubobaru Tanaka Iin), Tetsuo Tanaka (Wakaba Clinic), Tomohiko Uemura (Miyazakihigashi Hospital), Toshihide Unoki (Unoki Junkankika Naika Iin), Masanori Yamashita (Yamashita Iin), Seiichi Yamawaki (Yamawaki Naika Shounika Iin), Naoto Yokota (Yokota Naika), Hiroaki Yuchi (Yuchi Naika Ichouka Clinic).
Rights and permissions
About this article
Cite this article
Kita, T., Yokota, N., Ichiki, Y. et al. One-year effectiveness and safety of open-label losartan/hydrochlorothiazide combination therapy in Japanese patients with hypertension uncontrolled with ARBs or ACE inhibitors. Hypertens Res 33, 320–325 (2010). https://doi.org/10.1038/hr.2009.230
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.230
Keywords
This article is cited by
-
Clinical efficacy of various anti-hypertensive regimens in hypertensive women of Punjab; a longitudinal cohort study
BMC Women's Health (2020)
-
Mechanism of the blood pressure-lowering effect of sodium-glucose cotransporter 2 inhibitors in obese patients with type 2 diabetes
BMC Pharmacology and Toxicology (2017)
-
Significance of estimated salt excretion as a possible predictor of the efficacy of concomitant angiotensin receptor blocker (ARB) and low-dose thiazide in patients with ARB resistance
Hypertension Research (2013)
-
Comparison of medium-dose losartan/hydrochlorothiazide and maximal-dose angiotensin II receptor blockers in the treatment of Japanese patients with uncontrolled hypertension: the Kobe-CONNECT Study
Hypertension Research (2012)
-
Antihypertensive effect of a fixed-dose combination of losartan /hydrochlorothiazide in patients with uncontrolled hypertension: a multicenter study
Clinical and Experimental Nephrology (2012)