Abstract
African Americans have an increased incidence of end-stage renal disease and are characterized as having reduced bioavailability of nitric oxide and salt-sensitivity. We propose that endothelial nitric oxide synthase (eNOS) knockout mice (eNOS−/−) are a suitable model of hypertension-associated renal injury as seen in African Americans. Therefore, the purpose of this study was to determine whether older eNOS−/− mice have hypertension-associated renal injury and if dietary salt modulates this injury. Six-month-old eNOS−/− mice were placed on 0.12%, 0.45% or 8% NaCl diet for 8 weeks and blood pressure measured weekly; kidneys were collected for pathology evaluation and scoring at the end of the 8-week period. Mice deficient of eNOS were hypertensive at baseline compared with control mice in all three groups (128±3 vs. 112±3, P<0.05). Blood pressure was significantly elevated from baseline in eNOS−/− on 0.45 and 8% salt diets (P<0.02). The composite renal pathology scores for eNOS−/− mice were significantly greater than wild-type mice, indicating high salt intake exacerbates the injury (P<0.001 vs. normal salt diet). eNOS−/− mice may be used as a model of salt-induced and hypertension-associated renal injury as seen in African Americans.
Similar content being viewed by others
Introduction
African Americans experience a 3–17-fold (depending on type and number of risk factors present) greater likelihood of developing end-stage renal disease as compared with other populations.1, 2, 3 One distinguishing characteristic of this population that might account for this disparity is reduced nitric oxide bioavailability.4, 5, 6 Nitric oxide deficiency within the kidney causes increased renal resistance and acceleration of renal injury.7, 8 Interestingly, African Americans are reported to have increased renal vascular resistance with accompanying decrease in renal blood flow.9, 10 The renal injury observed in this population includes glomerulosclerosis, tubular atrophy, arteriosclerosis and interstitial fibrosis.11
Also of interest is the finding that ∼75% of hypertensive African Americans are characterized as salt-sensitive,1, 2, 3 suggesting that salt may contribute to the disparate pathophysiology of tissue organ damage associated with hypertension in this population. We and others have shown that increased salt may be ‘toxic,’ contributing to cardiac and renal tissue injury under certain conditions;12, 13, 14 some of these conditions may include states of nitric oxide deficiency.12, 14 Recent evidence reveals that salt inhibits nitric oxide synthase (NOS) activity and expression;15, 16 increased extracellular sodium dose-dependently inhibits NOS activity in cultured endothelial cells.15 In addition, studies show that salt inhibits brain nNOS expression and increases sympathetic output in uninephrectomized male rats given 1% saline.16 Thus, available evidence indicates that nitric oxide deficiency has both a permissive as well as an initiator function in the injurious effects of salt. Therefore, in this study we used 8–9-month-old endothelial knockout mice (eNOS−/−) to (1) characterize hypertensive-associated renal injury in NO deficiency and (2) determine whether salt aggravates the renal injury associated with this model of hypertension.
Methods
Animals
Breeding pair stocks for eNOS knockout mice were obtained from Jackson Laboratory (Bar Harbor, ME, USA; stock # 002684) and Dr Paul Huang (Massachusetts General Hospital, Boston, MA, USA). Both were bred onto the background of the C57BL/6 wild-type (WT) control strain, thus the C57BL/6, purchased from Jackson Laboratory, served as the control mouse strain. All animals were maintained on regular rodent chow. Mice were entered into the study at 6 months of age. Systolic blood pressure was measured using the tail-cuff method (Visitech 2000, Visitech Systems, Apex, NC, USA).
Protocol
WT and eNOS knockout mice were divided into three treatment groups. Group I mice were placed on a low salt diet (0.12% NaCl; Harlan Teklad, Madison, WI, USA; cat. no. T7034), Group II mice were remained on a control regular salt diet (0.4% NaCl, LabDiet, Richmond, IN, USA; cat. no. 5001), and Group III mice were given a high salt diet (8% NaCl, Harlan Teklad, cat. no. TD92012); dietary interventions were for 8 weeks. Low and high salt diets were initiated in Groups I and III, respectively, once basal tail-cuff systolic blood pressures were obtained. Mice on control diets remained on this diet throughout the basal and experimental periods. Weekly blood pressures were taken throughout the 8-week study period. All experiments were performed following protocols that were approved by the Institutional Animal Care and Use Committee.
Tail-cuff blood pressure measurements
Mice tail-cuff blood pressures were measured using the BP2000 instrument (Visitech Systems). Mice were trained 1–2 weeks before beginning blood pressure measurements. The mice were kept in restrainers during measurements, and these were magnetically held in place on a heated (37 °C) platform. The cuff was gradually inflated, and systolic pressure was determined as that pressure when flow ceases as detected by a sensor.
Histology preparation
At the end of the diet regimen, the animals were anesthetized with pentobarbital or isofluorane for tissue perfusion. Phosphate-buffered saline (pH 7.4) was perfused through the heart to flush the blood from the tissues (an incision of the liver provided a route for blood drainage). Finally, 5 ml of 10% buffered formalin (Fisher) was perfused through the heart for fixation of tissues. The kidneys were harvested for weighing and routinely processed for histologic evaluation (Histotechniques, Powell, OH, USA). Kidney sections were stained with periodic acid-Schiff. Hearts were collected and weighed for calculation of heart to body weight ratios.
Pathology scoring
Sections of kidney from eNOS−/− and WT mice were analyzed by a veterinary pathologist without any identifying information. Renal injury was divided into five categories: glomerular damage, tubular damage, interstitial inflammation, perivascular inflammation and vascular changes. Each category was scored for distribution or extent of damage based on the following scale: (1) focal, (2) multifocal and (3) diffuse or global change. In addition, each category was scored for the degree or grade of injury present using the following scale: 0=no injury present, 1=mild, 2=moderate, 3=moderate and 4=severe. Glomeruli were evaluated for the presence of fibrosis, cellularity, sclerosis and thrombosis; interstitial injury included the presence of lymphocytes, neutrophils, plasma cells and macrophages; tubular damage was defined as the presence of protein casts; perivascular inflammatory injury was defined as the presence of inflammatory cells including lymphocytes, plasma cells, neutrophils and macrophages; and in blood vessels, vascular injury was defined as medial hypertrophy and/or intimal proliferation. For each category of renal injury, the sum of the injury scores for each histopathologic change observed was multiplied by the distribution score, resulting in a composite renal pathology score for each animal. Therefore, the renal pathology score represented the product of grade (intensity) and extent of injury.
Statistical analysis
Blood pressure time course data were analyzed by two-way analysis of variance (2-ANOVA), whereas blood pressure single point multiple group analysis was performed by one-way analysis of variance (1-ANOVA) followed by Duncan's multiple comparison. t-Test or rank sum (for non-parametric data) analysis was used for basal and end-point comparisons. An among-group pathology comparison was made using 1-ANOVA followed by Student's Newman–Keuls (parametric analysis) or Dunn's (non-parametric analysis) multiple comparison test.
Results
Blood pressure
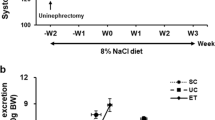
All animals remained relatively healthy as indicated by body weight increases over the duration of the study (Table 1). As shown in Figure 1, all three groups of eNOS−/− mice had significantly higher baseline systolic blood pressures as compared with WT control mice. This pressure difference persisted throughout the 8-week study period. Interestingly, systolic blood pressure in eNOS−/− mice on control and high salt diets was significantly higher than the starting baseline blood pressure at week 8 of the diets (0.45%: 129±4 vs. 145±4, P=0.004; 8%: 120±2 vs. 135±5, P=0.017) (Table 1); however, blood pressure was unchanged in eNOS−/− on a low salt diet. Blood pressure in WT was unchanged from baseline over the 8-week period in all three diet groups.
Heart and kidney weights
As cardiac hypertrophy is frequently associated with hypertension, we also examined the 8-month-old eNOS−/− transgenic mice for cardiac hypertrophy (assessed as tissue weight to body weight ratios). Indeed, we observed increased cardiac weight/body weight ratios in eNOS−/− relative to WT control mice in all three diet groups (Figure 2, top panel). Although salt had no effect on the increased heart weight associated with hypertension in the eNOS−/− mice, there was a dose-dependent effect of salt on cardiac weight in WT mice with high salt causing a significant increase in cardiac size relative to the low salt group (P<0.01 vs. low salt treatment; 1-ANOVA and Newman–Keuls). Dietary salt had no effect on kidney size in either eNOS−/− or WT (Figure 2, bottom panel).
Cardiac (top panel) and renal (bottom panel) hypertrophy in wild-type (WT) and eNOS knockout (eNOS−/−) mice following 8 weeks on low salt (0.12% NaCl), normal salt (0.45% NaCl) and high salt (8% NaCl) diets. Number of animals for each is displayed in parentheses. *P<0.002 vs. low salt and **P<0.01 vs. WT.
Renal pathology
Figure 3 shows the representative renal histopathology observed in eNOS−/− mice on control (panels a–c) and high (panels d–f) salt diet. There was significant glomeruli injury consisting of thrombosis, fibrosis and necrosis observed in eNOS−/− fed the control salt diet (0.45%). In Figure 3a, an example of an enlarged and fibrotic glomerulus is shown.
Renal pathology in eNOS−/− mice fed control (0.45% NaCl) (a–c) and high (8% NaCl) salt diets (d–f) for 8 weeks. A thrombosed glomerulus (β) and interstitial inflammation (†) from an eNOS−/− mice fed the control salt diet are shown in (a). Moderate perivascular inflammation (§), intimal thickening and medial layer proliferation (‘onion-skin’ appearance, *) are evident in small blood vessels (b). Prominent intra-luminal tubular casts (arrows) in a control diet fed mouse are shown (c). Renal injury involving glomeruli, tubules and blood small vessels was more severe and extensive in eNOS−/− mice fed the high salt diet. Several thrombosed (β) and/or sclerotic (δ) glomeruli are shown in (d). Moderate-to-severe perivascular (§) and interstitial inflammation (†) are shown in (e) and (f), respectively. Intra-tubular protein casts (arrows) formation was extensive in eNOS−/− mice fed the high salt diet (f). Normal renal histology was observed in wild-type (WT) mice fed a control (0.45% NaCl) salt diet for 8 weeks (g–i). Normal (*) appearing glomeruli, tubules, interstitium and blood vessels are shown (g–i).
Interstitial inflammation was also a feature of the injury observed (see Figure 3b). Mild perivascular cellular infiltration (inflammation) was another prominent feature of the injury seen in eNOS knockout mice fed the control diet (Figure 3b). The walls of small renal arteries were often thickened and had an ‘onion-skin’ appearance, indicating moderate-to-severe medial thickening and smooth muscle cell proliferation.17, 18 The lumens of renal tubules were often distended by deeply eosinophilic protein casts (Figure 3c). Similar, albeit, more severe and extensive renal injury involving glomeruli, tubules and small blood vessels was observed in eNOS−/− mice fed the high salt diet (Figures 3d–f). The renal tubules in eNOS−/− mice on a high salt diet contained significantly more protein casts than eNOS−/− fed control salt diet (Figure 3f). In addition, there was extensive perivascular (Figure 3e) and interstitial inflammation observed throughout the kidneys of eNOS−/− mice fed a high salt diet (Figures 3e and f).
In contrast, there was no change in the histology of glomeruli, tubules, interstitium or blood vessels in WT mice fed control (0.45% NaCl) or low (0.12% NaCl) and high (8% NaCl) salt diets. Evidence of normal appearing glomeruli, tubules, interstitium and blood vessels is shown in Figures 3g–i.
Finally, the effect of dietary salt on the development of renal injury in WT and eNOS−/− mice is summarized in Table 2. Regardless of dietary salt level, pathology scores for glomerular injury and interstitial and perivascular inflammation were significantly higher in eNOS−/− mice than WT mice fed a similar dietary regimen. In eNOS−/− mice, pathology scores for each category of renal injury were highest in mice fed the high salt diet; interestingly, only tubular injury was statistically significant from that of eNOS−/− on control salt diet (Table 2; 8% diet: 2.46±0.65 vs. normal 0.45% diet 0.29±0.16; 1-ANOVA and Dunn's test, P<0.004). In contrast, dietary salt levels did not affect renal histology in WT mice.
Discussion
This study shows that knocking out eNOS promotes renal injury and that high salt exacerbates this renal injury in eNOS−/− knockout mice. This is an important observation and the first documentation of the effect of dietary salt on renal injury in this mouse model of hypertension. In addition, cardiac hypertrophy, as indicated by increased heart weight/body weight ratio, was associated with the hypertension seen in this model of hypertension. However, cardiac hypertrophy was not modulated by dietary salt in eNOS−/− mice, whereas there was a dose-dependent effect of salt on cardiac hypertrophy seen in WT mice.
The older, 8-month-old, eNOS−/− mice on a low salt diet were clearly hypertensive compared with their WT counterparts at baseline and the systolic blood pressure did not change over the 2-month low salt diet intervention (Figure 1). However, over the 2-month time course on a high salt diet, blood pressure increased from 120±2 at baseline to 148±5 mm Hg by the end of the study, a 28 mm Hg increase (Figure 1, bottom panel; P<0.05). We observed a similar blood pressure increase in eNOS−/− mice on a normal salt diet in this strain (Figure 1, middle panel). The reason for the initial spike observed in the eNOS−/− groups on control and high salt diets 1 week after baseline measurements is not clear. There was a drop after the first week but blood pressure remained above baseline for the remainder of the study period in both the normal and high salt diet groups. It is not clear why blood pressure increased during the first week, although it is unlikely due to acclimation to the tail-cuff blood pressure measurement as all mice were exposed to a 1–2-week training period. The rise may have been due to some undetected environmental stressor. Leonard et al.19 have also reported similar time course effects of high dietary salt on blood pressure in eNOS−/− mice. They show an early peak at 2 weeks followed by a sustained increase throughout the remainder of the 6-week time period. The results from the normal salt group suggest that a normal salt diet may still be an inappropriately high salt diet in the absence of eNOS, perhaps eNOS−/− may represent a type of salt-sensitive model of hypertension. Such an interpretation is consistent with earlier reports implicating a role of nitric oxide in the development of salt-sensitive hypertension. Specifically, salt-sensitive rats have impaired nitric oxide and cGMP synthesis following a high salt diet compared with control rats, whereas inhibition of NOS conveys salt-sensitive hypertension.20, 21, 22, 23 Recent studies have shown that the mechanism of this salt effect on NO levels may be due to direct effects of sodium on endothelial cell NOS; Li et al.15 showed that extracellular sodium produces a dose-dependent inhibition of NOS activity in bovine endothelial cells. Other studies suggest that the resulting reduction in NO leads to an imbalance between NO and superoxide production.24
A major focus of this study was to determine whether renal injury is associated with the hypertension in eNOS−/− mice and determine whether high dietary salt exacerbates the hypertension-associated renal injury. The rationale was that this model could be useful in the study of hypertension-associated renal injury as seen in African Americans as African Americans are characterized by significantly reduced bioavailable NO.1, 25 In addition to impaired NO, African Americans have significant hypertension-associated renal injury6, 26, 27 and tend to be salt-sensitive.28 Characteristics of the renal pathology observed in African Americans includes increased renal vasoconstriction, perhaps due to the eNOS 894T and ACE deletion polymorphisms.8, 10 Histological examination of biopsied kidneys from hypertensive African Americans reveal focal glomerulosclerosis, contracted glomeruli, cortical fibrosis, tubular atrophy, interstitial inflammation and arteriosclerosis.11, 29, 30 Although early studies of eNOS−/− found no evidence of renal injury,31 subsequent studies using older mice reveal focal renal injury.32 Furthermore, renal injury usually associated with remnant kidney model of hypertension or diabetes is exacerbated in eNOS−/− mice.7, 33 In this study, we observe similar renal injury characteristics in this model as reported for African Americans, including glomerulosclerosis, fibrosis, interstitial inflammation and arteriosclerosis.
Because of the proclivity of African Americans for salt-sensitivity and the independent effect of salt on tissue injury, we also examined the effect of salt on blood pressure and renal injury in this NO-deficient model of hypertension. We observed that dietary salt significantly modulated the extent of tubular casts. Although not statistically significant, glomerular injury tended to increase as dietary salt intake increased. The inflammation seen in this model was not altered by dietary salt; however, it is interesting to note that perivascular inflammation tended to be greater under both low and high salt conditions. In addition, the renal pathological scores were unaffected by dietary interventions in the WT, normotensive control mice. These findings suggest that prolonged exposure to hypertension in this mouse model is associated with significant renal injury. Although a high salt diet aggravates the injury, a low salt diet may protect against hypertension and tissue injury associated with hypertension in the setting of NO deficiency. There was no evidence of renal hypertrophy in either control or eNOS−/− mice; unlike what has been reported for the L-NAME-induced hypertension model.34 Absence of kidney hypertrophy in similar aged eNOS−/− mice has been reported by others;33 indeed kidneys of eNOS−/− were found to be smaller than age-matched C57/129sv mice on regular salt diet. We observed a similar trend in eNOS−/− on regular salt diet compared with C57. This difference may simply be due to differences in the genetic background on which the mice were bred or it may reflect the degree of glomerulosclerosis and nephron loss. Hartner et al.35 showed strain differences in blood pressure and renal injury response to DOCA salt administration; C57 mice were more resistant to DOCA salt, exhibiting lower blood pressure, interstitial fibrosis and renal glomerulosclerosis than 129sv. However, kidney weights were comparable after the DOCA salt administration.
Earlier examination of renal histology of 14-week-old eNOS−/− mice revealed no obvious histological differences from that of WT.36 The effect of sustained hypertension on renal injury in eNOS−/− mice, however, has been less well characterized. In this study, we show that there is significant renal injury at 8 months of age in mice lacking the eNOS gene. In eNOS-deficient mice on normal rat chow, we observed enlarged and collapsed glomeruli, fibrotic glomeruli, tubular casts, interstitial and perivascular inflammation and less frequently or prominently, arterial wall thickening; similar abnormalities also have been reported by others.32 Chronic nitric oxide inhibition models of hypertension exhibit a similar degree of renal injury with the major features being enlarged and collapsed glomeruli.37, 38 Other histological findings in NO inhibition models of hypertension include capillary thrombi and sclerosis, arteriolar fibrosis and vessel wall thickening proliferation providing an onion-skin appearance to the arteriole walls.17, 18 Thus, this mouse model of hypertension appears to be comparable to the pharmacologic NO inhibition in other models.
As with renal injury, cardiac hypertrophy in eNOS−/− mice is variably reported. Several groups failed to detect cardiac hypertrophy in eNOS−/− mice;31, 36, 39, 40 however, we report significant cardiac hypertrophy in our eNOS−/− mice. We used two eNOS−/− stocks, obtained from Jackson Laboratory and Dr Paul Huang31; (Boston, MA, USA), and did not detect any difference in blood pressure or hypertrophy response between the two breeding stocks. The reason for this apparent discrepancy in cardiac hypertrophy reporting is not known but the use of younger aged animals or background strain differences may explain the failure to observe cardiac hypertrophy in earlier studies. In this study, we used 6-month-old mice bred on a C57 background; consequently, the mice were 8 months old at the time of measurement, an age comparable to middle age in humans. Babikat and colleagues also studied 6–8-month-old eNOS−/− with comparable systolic blood pressures as in our study, and found modest but statistically insignificant hypertrophy at this age. However, the mice used in that study were bred on a mixed background (C57/129sv). This discrepancy cannot be simply explained by differences in control dietary salt levels, as Babikat and colleagues used chow containing 0.6% NaCl and a chow containing 0.45% NaCl was used in our study. However, it is important to note that Yang et al.41 have reported left ventricular hypertrophy in 12-week-old eNOS−/− mice also bred on a mixed background of C57/129sv, a finding consistent with our study. It is not clear why the presence of cardiac hypertrophy is so variable in this model; however, despite this variability, these studies, taken together, suggest that sustained hypertension in eNOS−/− can produce cardiac hypertrophy.
We also examined the effect of low and high salt diets on cardiac hypertrophy. We found a dose-dependent effect of salt on cardiac hypertrophy in the WT; however, we did not find such an effect in the eNOS−/− mice. The ‘toxic’ effect of salt on organ damage independent of blood pressure has been reported earlier.42, 43, 44, 45, 46 This effect of salt on cardiac mass is seen in animals and humans.44, 47, 48, 49, 50 Thus, our cardiac hypertrophy response to salt in the WT is consistent with earlier findings of hypertrophy in the absence of hypertension. The dose-dependent effect of salt on cardiac hypertrophy in WT suggests that eNOS mediates the hypertrophic effect of salt. Endothelial NOS expression has been shown to be increased with high salt diet.51, 52 The increased eNOS may become uncoupled, leading to more superoxide production as compared with NO; the increased oxidative stress then contributes to the development of cardiac hypertrophy.52 On the other hand, the failure to see an effect of salt in eNOS−/− may be explained as a result of maximal cardiac hypertrophy expressed in eNOS−/− mice in the absence of a high salt diet. Thus, cardiac hypertrophy cannot be further increased with high salt. The existing hypertrophy before increased dietary salt may be mediated by the lack of eNOS. Evidence to support this interpretation include the finding that salt decreases eNOS expression in heart, kidney and aorta.53, 54 Of particular interest is the finding that blockade of endothelin prevents the hypertensive effect of high salt in obese rats but did not prevent the hypertrophy or accompanying decrease in eNOS expression.54 Thus, reduced eNOS may promote salt-induced hypertrophy. In both scenarios, the mechanism of salt-induced tissue injury may be mediated through oxidative stress.12, 24, 55
There was no evidence of renal hypertrophy in either control or eNOS−/− mice, in contrast to what has been reported for the L-NAME-induced hypertension model.34 The absence of kidney hypertrophy in similar aged eNOS−/− mice has been reported by others;33 indeed kidneys of eNOS−/− were found to be smaller than age-matched C57/129sv mice on regular salt diet. We observed a similar trend in eNOS−/− on regular salt diet compared with C57. This difference may simply be due to differences in the genetic background on which the mice were bred. Hartner et al.35 showed strain differences in blood pressure and renal injury response to DOCA salt administration; C57 mice were more resistant to DOCA salt, exhibiting lower blood pressure, interstitial fibrosis and renal glomerulosclerosis than 129sv. However, kidney weights were comparable after the DOCA salt administration.
In summary, prolonged hypertension in eNOS-deficient mice is associated with renal injury that is aggravated by a high salt diet. The renal injury hallmark characteristics were similar to that observed in hypertensive African Americans. This renal pathology response to a high salt diet is associated with an increase in systolic blood pressure. Therefore, these observations suggest that this model may be useful for studying hypertension-associated renal injury that is observed in African Americans.
Conflict of interest
The authors declare no conflict of interest.
References
Rostand SG, Kirk KA, Rutsky EA, Pate BA . Racial differences in the incidence of treatment for end-stage renal disease. N Engl J Med 1982; 306: 1276–1279.
Dustan H . Does keloid pathogenesis hold the key to understanding Black/White differences in hypertension severity? Hypertension 1995; 26: 858–862.
McClellan W, Tuttle E, Issa A . Racial differences in the incidence of hypertensive end-stage renal disease (ESRD) are not entirely explained by differences in the prevalence of hypertension. Am J Kidney Dis 1988; 12: 285–290.
Cardillo C, Kilcoyne CM, Cannon 3rd RO, Panza JA . Attenuation of cyclic nucleotide-mediated smooth muscle relaxation in blacks as a cause of racial differences in vasodilator function. Circulation 1999; 99: 90–95.
Jones DW, Chambless LE, Folsom AR, Heiss G, Hutchinson RG, Sharrett AR, Szklo M, Taylor Jr HA . Risk factors for coronary heart disease in African Americans: the atherosclerosis risk in communities study, 1987–1997. Arch Intern Med 2002; 162: 2565–2571.
Stein CM, Lang CC, Nelson R, Brown M, Wood AJ . Vasodilation in black Americans: attenuated nitric oxide-mediated responses. Clin Pharmacol Ther 1997; 62: 436–443.
Nakayama T, Sato W, Kosugi T, Zhang L, Campbell-Thompson M, Yoshimura A, Croker BP, Johnson RJ, Nakagawa T . Endothelial injury due to eNOS deficiency accelerates the progression of chronic renal disease in the mouse. Am J Physiol Renal Physiol 2009; 296: F317–F327.
Stafford-Smith M, Podgoreanu M, Swaminathan M, Phillips-Bute B, Mathew JP, Hauser EH, Winn MP, Milano C, Nielsen DM, Smith M, Morris R, Newman MF, Schwinn DA . Association of genetic polymorphisms with risk of renal injury after coronary bypass graft surgery. Am J Kidney Dis 2005; 45: 519–530.
Campese VM, Parise M, Karubian F, Bigazzi R . Abnormal renal hemodynamics in black salt-sensitive patients with hypertension. Hypertension 1991; 18: 805–812.
Frohlich ED, Messerli FH, Dunn FG, Oigman W, Ventura HO, Sundgaard-Riise K . Greater renal vascular involvement in the black patient with essential hypertension. A comparison of systemic and renal hemodynamics in black and white patients. Miner Electrolyte Metab 1984; 10: 173–177.
Obialo CI, Hewan-Lowe K . Rapid progression to end-stage renal disease in young hypertensive African Americans with proteinuria. J Natl Med Assoc 1998; 90: 649–655.
Trolliet MR, Rudd MA, Loscalzo J . Oxidative stress and renal dysfunction in salt-sensitive hypertension. Kidney Blood Press Res 2001; 24: 116–123.
Boero R, Pignataro A, Quarello F . Salt intake and kidney disease. J Nephrol 2002; 15: 225–229.
Jones-Burton C, Mishra SI, Fink JC, Brown J, Gossa W, Bakris GL, Weir MR . An in-depth review of the evidence linking dietary salt intake and progression of chronic kidney disease. Am J Nephrol 2006; 26: 268–275.
Li J, White J, Guo L, Zhao X, Wang J, Smart EJ, Li XA . Salt inactivates endothelial nitric oxide synthase in endothelial cells. J Nutr 2009; 139: 447–451.
Campese VM, Mozayeni P, Ye S, Gumbard M . High salt intake inhibits nitric oxide synthase expression and aggravates hypertension in rats with chronic renal failure. J Nephrol 2002; 15: 407–413.
Benter IF, Yousif MH, Anim JT, Cojocel C, Diz DI . Angiotensin-(1–7) prevents development of severe hypertension and end-organ damage in spontaneously hypertensive rats treated with L-NAME. Am J Physiol Heart Circ Physiol 2006; 290: H684–H691.
Fujihara CK, Sena CR, Malheiros DM, Mattar AL, Zatz R . Short-term nitric oxide inhibition induces progressive nephropathy after regression of initial renal injury. Am J Physiol Renal Physiol 2006; 290: F632–F640.
Leonard AM, Chafe LL, Montani JP, Van Vliet BN . Increased salt-sensitivity in endothelial nitric oxide synthase-knockout mice. Am J Hypertens 2006; 19: 1264–1269.
Chen PY, Sanders PW . L-arginine abrogates salt-sensitive hypertension in Dahl/Rapp rats. J Clin Invest 1991; 88: 1559–1567.
Simchon S, Manger W, Blumberg G, Brensilver J, Cortell S . Impaired renal vasodilation and urinary cGMP excretion in Dahl salt-sensitive rats. Hypertension 1996; 27: 653–657.
Rudd MA, Trolliet M, Hope S, Scribner AW, Daumerie G, Toolan G, Cloutier T, Loscalzo J . Salt-induced hypertension in Dahl salt-resistant and salt-sensitive rats with NOS II inhibition. Am J Physiol 1999; 277: H732–H739.
Mattson DL, Higgins DJ . Influence of dietary sodium intake on renal medullary nitric oxide synthase. Hypertension 1996; 27: 688–692.
Majid DS, Kopkan L . Nitric oxide and superoxide interactions in the kidney and their implication in the development of salt-sensitive hypertension. Clin Exp Pharmacol Physiol 2007; 34: 946–952.
Cardillo C, Kilcoyne CM, Cannon 3rd RO, Panza JA . Racial differences in nitric oxide-mediated vasodilator response to mental stress in the forearm circulation. Hypertension 1998; 31: 1235–1239.
Shulman N, Ford C, Hall W, Blaufox M, Simon D, Langford H, Schneider K . Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the Hypertension Detection and Follow-up Program. Hypertension 1989; 13 (Suppl I): I80–I93.
Jones DS, Andrawis NS, Abernethy DR . Impaired endothelial-dependent forearm vascular relaxation in black Americans. Clin Pharmacol Ther 1999; 65: 408–412.
Weinberger MH, Miller JZ, Luft FC, Grim CE, Finberg NS . Definitions and characteristics of sodium sensitivity and blood pressure resistance. Hypertension 1986; 8: II-127–II-134.
Marcantoni C, Ma LJ, Federspiel C, Fogo AB . Hypertensive nephrosclerosis in African Americans versus Caucasians. Kidney Int 2002; 62: 172–180.
Pat B, Hughson MD, Nicol JL, Hoy WE, Gobe GC . A comparison of pathomolecular markers of fibrosis and morphology in kidney from autopsies of African Americans and whites. Virchows Arch 2007; 450: 41–50.
Huang PL, Huang Z, Mashimo H, Bloch KD, Moskowitz MA, Bevan JA, Fishman MC . Hypertension in mice lacking the gene for endothelial nitric oxide synthase. Nature 1995; 377: 239–242.
Forbes MS, Thornhill BA, Park MH, Chevalier RL . Lack of endothelial nitric-oxide synthase leads to progressive focal renal injury. Am J Pathol 2007; 170: 87–99.
Nakagawa T, Sato W, Glushakova O, Heinig M, Clarke T, Campbell-Thompson M, Yuzawa Y, Atkinson MA, Johnson RJ, Croker B . Diabetic endothelial nitric oxide synthase knockout mice develop advanced diabetic nephropathy. J Am Soc Nephrol 2007; 18: 539–550.
Vaskonen T, Mervaala E, Krogerus L, Teravainen TL, Laakso J, Karppanen H, Vapaatalo H . Cardiovascular effects of chronic inhibition of nitric oxide synthesis and dietary salt in spontaneously hypertensive rats. Hypertens Res 1997; 20: 183–192.
Hartner A, Cordasic N, Klanke B, Veelken R, Hilgers KF . Strain differences in the development of hypertension and glomerular lesions induced by deoxycorticosterone acetate salt in mice. Nephrol Dial Transplant 2003; 18: 1999–2004.
Shesely EG, Maeda N, Kim HS, Desai KM, Krege JH, Laubach VE, Sherman PA, Sessa WC, Smithies O . Elevated blood pressures in mice lacking endothelial nitric oxide synthase. Proc Natl Acad Sci USA 1996; 93: 13176–13181.
Ribeiro MO, Antunes E, de Nucci G, Lovisolo SM, Zatz R . Chronic inhibition of nitric oxide synthesis. A new model of arterial hypertension. Hypertension 1992; 20: 298–303.
Raij L . Nitric oxide in hypertension. Relationship with renal injury and left ventricular hypertrophy. Hypertension 1998; 31: 189–193.
Godecke A, Decking UK, Ding Z, Hirchenhain J, Bidmon HJ, Godecke S, Schrader J . Coronary hemodynamics in endothelial NO synthase knockout mice. Circ Res 1998; 82: 186–194.
Bubikat A, De Windt LJ, Zetsche B, Fabritz L, Sickler H, Eckardt D, Godecke A, Baba HA, Kuhn M . Local atrial natriuretic peptide signaling prevents hypertensive cardiac hypertrophy in endothelial nitric-oxide synthase-deficient mice. J Biol Chem 2005; 280: 21594–21599.
Yang XP, Liu YH, Shesely EG, Bulagannawar M, Liu F, Carretero OA . Endothelial nitric oxide gene knockout mice: cardiac phenotypes and the effect of angiotensin-converting enzyme inhibitor on myocardial ischemia/reperfusion injury. Hypertension 1999; 34: 24–30.
Mervaala EM, Laakso J, Vapaatalo H, Karppanen H . Effects of enalapril and hydrochlorothiazide on the salt-induced cardiac and renal hypertrophy in normotensive rats. Naunyn Schmiedebergs Arch Pharmacol 1994; 350: 416–425.
Antonios TF, MacGregor GA . Salt intake. potential deleterious effects excluding blood pressure. J Hum Hypertens 1995; 9: 511–515.
Coca A, De la Sierra A . Salt sensitivity and left ventricular hypertrophy. Adv Exp Med Biol 1997; 432: 91–101.
Weir MR . Salt intake and hypertensive renal injury in African-Americans. A therapeutic perspective. Am J Hypertens 1995; 8: 635–644.
Yu HC, Burrell LM, Black MJ, Wu LL, Dilley RJ, Cooper ME, Johnston CI . Salt induces myocardial and renal fibrosis in normotensive and hypertensive rats. Circulation 1998; 98: 2621–2628.
Campese VM . Salt sensitivity in hypertension. Renal and cardiovascular implications. Hypertension 1994; 23: 531–550.
Yuan BX, Leenen FH . Dietary sodium intake and left ventricular hypertrophy in normotensive rats. Am J Physiol 1991; 261: H1397–H1401.
Frohlich ED, Chien Y, Sesoko S, Pegram BL . Relationship between dietary sodium intake, hemodynamics, and cardiac mass in SHR and WKY rats. Am J Physiol 1993; 264: R30–R34.
Schmieder RE, Messerli FH, Garavaglia GE, Nunez BD . Dietary salt intake. A determinant of cardiac involvement in essential hypertension. Circulation 1988; 78: 951–956.
Herrera M, Garvin JL . A high-salt diet stimulates thick ascending limb eNOS expression by raising medullary osmolality and increasing release of endothelin-1. Am J Physiol Renal Physiol 2005; 288: F58–F64.
Hirai T, Okumura K, Nishimoto Y, Shumiya T, Murakami R, Takahashi R, Asai T, Murakami H, Numaguchi Y, Matsui H, Murohara T . Upregulation of renal eNOS by high-sodium diet facilitates hypertension in doxorubicin-treated rats through enhanced oxidative stress. Toxicology 2006; 225: 81–89.
Ni Z, Vaziri ND . Effect of salt loading on nitric oxide synthase expression in normotensive rats. Am J Hypertens 2001; 14: 155–163.
Radin MJ, Holycross BJ, Hoepf TM, McCune SA . Salt-induced cardiac hypertrophy is independent of blood pressure and endothelin in obese, heart failure-prone SHHF rats. Clin Exp Hypertens 2008; 30: 541–552.
Tian N, Thrasher KD, Gundy PD, Hughson MD, Manning Jr RD . Antioxidant treatment prevents renal damage and dysfunction and reduces arterial pressure in salt-sensitive hypertension. Hypertension 2005; 45: 934–939.
Acknowledgements
This work was supported in part by the National Heart, Lung and Blood Institute Grant P50 HL55993-01 (to JL, MP) and UH1 HL59868 (to LB, SY and MP).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Daumerie, G., Bridges, L., Yancey, S. et al. The effect of salt on renal damage in eNOS-deficient mice. Hypertens Res 33, 170–176 (2010). https://doi.org/10.1038/hr.2009.197
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.197
Keywords
This article is cited by
-
Physiological stress increases renal injury in eNOS-knockout mice
Hypertension Research (2012)