Abstract
In general, treatment with most angiotensin receptor blockers (ARBs) increases plasma angiotensin II (Ang II) level because of a lack of negative feedback on renin activity. Olmesartan is a potential ARB inducing activation of angiotensin-converting enzyme 2 (ACE2) that hydrolyzes Ang II to Ang 1–7, and has shown a beneficial effect on ventricular remodeling. Indeed, a previous study reported that olmesartan treatment resulted in decreased plasma levels of Ang II and aldosterone. However, there has not yet been a study showing the relationship of chronic effects of olmesartan on Ang II and the left ventricular mass index (LVMI) in comparison with those of other ARB.
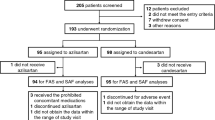
A total of 50 stable outpatients with essential hypertension who had received candesartan for more than 1 year were randomized into two groups: control group (n=25): continuous candesartan treatment at a stable dose; and olmesartan group (n=25): candesartan (8 mg day−1) was changed to olmesartan given at a dose of 20 mg day−1. There was no difference in the baseline characteristics between the two groups. In the control group, there were no significant changes in blood pressure, LVMI or biomarkers during 12 months of study. In the olmesartan group, blood pressure did not change and plasma levels of Ang II decreased during 12 months of study, whereas LVMI was significantly decreased after 12 months (135±36 vs. 123±29 g m−2; P<0.01).
These findings indicate that replacing candesartan with olmesartan decreased LVMI in association with a sustained decrease of plasma Ang II over a 12-month period without changing blood pressure or plasma aldosterone in patients with essential hypertension.
Similar content being viewed by others
Main
Angiotensin receptor blockers (ARBs) are widely used for the management of hypertension and chronic heart failure (CHF). In general, treatment with ARBs increases the plasma angiotensin II (Ang II) level because of a lack of negative feedback on renin activity or competition of Ang II with AT1 receptor. Indeed, several types of ARBs have been shown to increase both plasma renin activity and plasma Ang II concentrations in hypertensive patients.1, 2, 3 In contrast, Ichikawa et al.4 reported that long-term treatment of hypertensive patients with olmesartan resulted in a reduction of the plasma Ang II level. The exact mechanism underlying the failure of olmesartan to increase the plasma Ang II levels remains uncertain.
Angiotensin-converting enzyme 2 (ACE2), a homolog of the ACE enzyme5, 6 expressed primarily in the vascular endothelium, removes a single amino acid from the carboxy-terminus of Ang II to generate Ang 1–7. Previous studies suggested that the ACE2–Ang 1–7 axis has an important role in hypertensive disease and CHF.7, 8, 9 Takeda et al.10 reported that treatment with candesartan increased ACE2 mRNA level and decreased angiotensinogen mRNA level in the heart. Recently, it was shown that olmesartan increased ACE2 expression during the remodeling of the heart after myocardial infarction,11 and olmesartan improved left ventricular remodeling with an increase in cardiac ACE2 expression in stroke-prone spontaneously hypertensive rats.12 The ACE2 is a membrane-associated carboxy-peptidase that is highly expressed in the heart and kidney13 and hydrolyzes Ang II to Ang 1–7, which inhibits the ACE C-domain and bradykinin by acting as an ACE inhibitor.14 Therefore, olmesartan may be a potential ARB with an activating effect on ACE2 and an inhibitory effect on ACE.
We previously reported that plasma Ang II level was significantly increased in patients with CHF after chronic treatment with candesartan.15 Therefore, we hypothesize that there is a difference in chronic effect on Ang II between candesartan and olmesartan in patients with essential hypertension. In this study, we compared the chronic effects of olmesartan on Ang II in comparison with those of candesartan, as well as the long-term effects of olmesartan on left ventricular mass index (LVMI) in comparison with those of candesartan. This study evaluated the long-term effects of olmesartan, after replacement of candesartan, on plasma levels of Ang II and aldosterone (ALD) and on left LVMI in patients with essential hypertension.
Methods
A total of 50 stable outpatients with essential hypertension who had received candesartan for more than 1 year were randomized to two groups using the envelope method: control group (n=25): continuous candesartan treatment at a stable dose; and olmesartan group (n=25): candesartan (8 mg day−1) was changed to olmesartan given at a dose of 20 mg day−1, which is a comparable antihypertensive dose. Patients with renal insufficiency (serum creatinine 1.5 mg 100 ml−1), angina pectoris or moderate to severe CHF (New York Heart Association functional class (NYHA) III or IV) were excluded from this study. Patients who received ACE inhibitors and other ARBs were excluded. Although the use of other drugs was allowed, the doses of these agents were not changed during the study period. The general condition of each patient had been stable for more than 6 months before the study.
In the outpatient clinic, resting heart rate was determined from electrocardiogram and blood pressure measurements and data were independently confirmed by attending physicians. Blood samples were collected from the antecubital vein after rest in a seated position for at least 20 min at baseline, after 3 months, after 6 months and after 12 months. Echocardiography was performed at baseline and after 12 months by the same sonographer. Left ventricular ejection fraction (LVEF) was measured by echocardiography at the same time. The LVMI value was calculated from M-mode echocardiograms according to the formula derived by Devereux et al.16
Blood samples were assessed for plasma renin concentration (PRC), plasma levels of Ang II, ALD and brain natriuretic peptide (BNP). The attending physicians were blinded to the neurohumoral and echocardiographic data. Informed consent was obtained from all patients before participation in the study, after the approval of the protocol by the Committee on Human Investigation at our institution.
Measurement of neurohumoral factors
Blood samples were collected from the antecubital vein after rest in a seated position for at least 20 min. Blood sampling was performed in the afternoon. Blood was centrifuged at 3000 r.p.m. for 15 min at 4 °C, and the plasma thus obtained was stored at −30 °C until assay. The plasma levels of PRC, Ang II and ALD were measured using commercial radioimmunoassay kits as previously reported.15, 17 Samples for the assay of plasma BNP concentrations were transferred to chilled disposable tubes containing aprotinin (500 kallikrein inactivator units ml−1). The blood samples were immediately placed on ice and centrifuged at 4 °C, and then the plasma was frozen in aliquots and stored at −30 °C until assay. Plasma BNP concentrations were measured by a immunoradiometric assay specific for human BNP using a commercial kit (Shionogi, Osaka, Japan) as previously reported.18
Statistical analysis
All results are expressed as the mean±s.d. Univariate analysis was performed using Student's t-test. Categorical data were compared against a chi-squared distribution. Comparisons between groups were performed by analysis of variance with Fisher's test for continuous variables. A P-value <0.05 was regarded as significant.
Results
Table 1 lists the characteristics of the subjects. The study subjects were 50 patients with essential hypertension. There was no difference in baseline characteristics, including LVEF and LVMI and plasma levels of PRC, Ang II, ALD and BNP between the two groups (Table 1). A total of 17 patients had CHF (NYHA class I or II) and there was no difference in the incidence of CHF complication between the two groups. Concomitant therapy other than candesartan was maintained for at least 12 months and there was no difference in baseline medication between the two groups.
There were no significant changes in either the control or olmesartan groups with regard to blood pressure or heart rate over the 12-month observation period (Table 2). In the control group, plasma levels of PRC, Ang II, ALD and BNP did not change during 12 months of observation. In the olmesartan group, plasma Ang II level was significantly decreased after 3 months and the decrease in Ang II was sustained during 12 months (161±350 pg ml−1 at baseline, 66±120 pg ml−1 at 3 months, 68±101 pg ml−1 at 6 months, 32±47 pg ml−1 at 12 months; Figure 1) and plasma ALD level was slightly decreased after 3 months but there were no significant differences over the 12-month period (108±131 pg ml−1 at baseline, 89±75 pg ml−1 at 3 months, 90±95 pg ml−1 at 6 months and 92±94 pg ml−1 at 12 months; Figure 2). In the olmesartan group, plasma levels of BNP did not change during 12 months but LVMI was significantly decreased after 12 months (135±36 vs. 123±29 g m−2; P<0.01; Figure 3). There was a significant positive correlation between the changes of LVMI (LVMI at baseline−LVMI after 12 months) and the delta changes in plasma Ang II (Ang II at baseline−Ang II after 12 months) in the olmesartan group (r=0.521, P=0.0076; Figure 4).
(a) Changes in left ventricular mass index (LVMI) before and after 12 months. (b) Delta changes in LVMI before and after 12 months. Closed columns represent patients who received olmesartan replaced by candesartan; open columns represent patients who continued receiving candesartan. *P<0.01 vs. the baseline value.
Discussion
In this study, (1) we evaluated the long-term effects of replacing candesartan with olmesartan on plasma levels of PRC, ALD, Ang II, ALD and BNP in patients with essential hypertension, (2) we also estimated the long-term effects of replacing candesartan with olmesartan on LVMI. Interestingly, despite significant changes in blood pressure and heart rate over the12-month observation period in both groups, LVMI was significantly decreased in the olmesartan group only (Figure 3). In addition, the significant decrease in LVMI was associated with a decrease of Ang II (Figure 4) but not with changes in PRC, ALD or BNP level.
Whether the effects of several ARBs on ACE2 expression are same remains uncertain10, 11, 12 especially in hypertensive patients. The present finding that the plasma Ang II level was decreased after replacement of candesartan with olmesartan without any changes in PRC suggests that the effect of olmesartan on ACE2 expression is more stimulating than that of candesartan. Ang 1–7 is an endogenous ligand for the G protein-coupled receptor Mas19 and may have a beneficial effect on left ventricular remodeling. As experimental studies showed that olmesartan increased plasma Ang 1–7 levels through an increase in ACE2 expression, plasma Ang 1–7 level may be increased in association with the decrease in Ang II after replacement of candesartan with olmesartan. However, we could not measure the plasma levels of Ang 1–7 in this study. As the treatment with candesartan increases ACE2 mRNA in Dahl salt-sensitive hypertensive rats10 and local renin-angiotensin-aldosterone system (RAS) is independent of systemic RAS, further studies are needed to clarify this issue in a large number of patients.
Long-term treatment with ACE inhibitors or ARBs does not necessarily induce significant decreases in plasma ALD levels (ALD breakthrough).20, 21, 22 ALD breakthrough generally occurs in about half of the cases within 12 months.23, 24 Recently, ALD breakthrough was observed in 23% of hypertensive patients during candesartan treatment.25 The elevation of Ang II after treatment with ARBs may contribute to ALD breakthrough due to the activation of AT type 2 receptor in the adrenal gland.26 The finding that plasma ALD level was slightly decreased over the 12-month observation period in association with the significant decrease in Ang II may support findings in previous experimental study,26 but the decrease in ALD was not statistically significant, suggesting that multiple mechanisms may contribute to ALD breakthrough in patients with hypertension.
Although the significant decrease in LVMI, an important surrogate marker,27 was observed in the olmesartan group, plasma level of BNP, a biomarker of hemodynamic overload did not change during 12 months. Therefore, hemodynamic changes, including blood pressure, may not contribute to the decrease in LVMI. In this study, 17 patients had CHF (NYHA class I or II). In patients with CHF, high plasma levels of PRC, Ang II, ALD and BNP were associated with poor prognosis.17, 18, 28, 29 Most biomarkers, except Ang II, did not change after replacement of candesartan with olmesartan. A high plasma Ang II level is a prognostic predictor in asymptomatic CHF patients28 and in mild-to-moderate CHF patients.29 Recently, it was reported that there may be differential effects of various ARBs on prognosis in patients with CHF.30 Taken together with the improvement of LVMI, olmesartan may have a beneficial effect on surrogate markers for cardiac events in hypertensive patients with CHF.
This study has several limitations. First, we could not measure plasma level of Ang 1–7. Although we took blood samples after patients rested for at least 20 min in a seated position in this study and the attending physicians and sonographers were blinded to the neurohumoral data, the variability of biomarkers such as Ang II may have influenced the results. In addition, LVMI was slightly higher in the olmesartan group, which may have been reflected in the results. Further studies are needed to clarify this issue in a large number of patients.
Conclusions
At effective antihypertensive doses of candesartan and olmesartan, olmesartan significantly decreased the plasma Ang II level over the 12-month observation period. Furthermore, long-term olmesartan therapy decreased LVMI in patients with essential hypertension.
References
Grossman E, Peleg E, Carroll J, Shamiss A, Rosenthal T . Hemodynamic and humoral effects of the angiotensin II antagonist losartan in essential hypertension. Am J Hypertens 1994; 7: 1041–1044.
Bauer IH, Reams GP, Wu Z, Lau-Sieckman A . Effects of losartan on the renin-angiotensin-aldosterone axis in essential hypertension. J Hum Hypertens 1995; 9: 237–243.
Gavras I, Gavras H . Effects of eprosartan vs. enalapril in hypertensive patients on the renin-angiotensin-aldosterone system and safety parameters: results from a 26-week, double-blind, multicentre study Eprosartan Multinational Study Group. Curr Med Res Opin 1999; 15: 15–24.
Ichikawa S, Takayama Y . Long-term effects of olmesartan, an Ang II receptor antagonist, on blood pressure and the renin-angiotensin-aldosterone system in hypertensive patients. Hypertens Res 2001; 24: 641–646.
Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, Donovan M, Woolf B, Robison K, Jeyaseelan R, Breitbart RE, Acton S . A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1–9. Circ Res 2000; 87: E1–E9.
Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ . A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem 2000; 275: 33238–33243.
Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, Oliveira-dos-Santos AJ, da Costa J, Zhang L, Pei Y, Scholey J, Ferrario CM, Manoukian AS, Chappell MC, Backx PH, Yagil Y, Penninger JM . Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature 2002; 417: 822–828.
Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, Diz DI, Gallagher PE . Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation 2005; 111: 2605–2610.
Varagic J, Trask AJ, Jessup JA, Chappell MC, Ferrario CM . New angiotensins. J Mol Med 2008; 86: 663–671.
Takeda Y, Zhu A, Yoneda T, Usukura M, Takata H, Yamagishi M . Effects of aldosterone and angiotensin II receptor blockade on cardiac angiotensinogen and angiotensin-converting enzyme 2 expression in Dahl salt-sensitive hypertensive rats. Am J Hypertens 2007; 20: 1119–1124.
Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM . Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension 2004; 43: 970–976.
Agata J, Ura N, Yoshida H, Shinshi Y, Sasaki H, Hyakkoku M, Taniguchi S, Shimamoto K . Olmesartan is an angiotensin II receptor blocker with an inhibitory effect on angiotensin-converting enzyme. Hypertens Res 2006; 29: 865–874.
Gembardt F, Sterner-Kock A, Imboden H, Spalteholz M, Reibitz F, Schultheiss HP, Siems WE, Walther T . Organ-specific distribution of ACE2 mRNA and correlating peptidase activity in rodents. Peptides 2005; 26: 1270–1277.
Benter IF, Ferrario CM, Morris M, Diz DI . Antihypertensive actions of angiotensin-(1–7) in spontaneously hypertensive rats. Am J Physiol 1995; 269 (1 Pt 2): H313–H319.
Tsutamoto T, Wada A, Maeda K, Mabuchi N, Hayashi M, Tsutsui T, Ohnishi M, Sawaki M, Fujii M, Matsumoto T, Kinoshita M . Angiotensin II type 1 receptor antagonist decreases plasma levels of tumor necrosis factor alpha, interleukin-6 and soluble adhesion molecules in patients with chronic heart failure. J Am Coll Cardiol 2000; 35: 714–721.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N . Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
Tsutamoto T, Sakai H, Tanaka T, Fujii M, Yamamoto T, Wada A, Ohnishi M, Horie M . Comparison of active renin concentration and plasma renin activity as a prognostic predictor in patients with heart failure. Circ J 2007; 71: 915–921.
Tsutamoto T, Wada A, Maeda K, Hisanaga T, Maeda Y, Fukai D, Ohnishi M, Sugimoto Y, Kinoshita M . Attenuation of compensation of endogenous cardiac natriuretic peptide system in chronic heart failure: prognostic role of plasma brain natriuretic peptide concentration in patients with chronic symptomatic left ventricular dysfunction. Circulation 1997; 96: 509–516.
Santos RA, Simoes e Silva AC, Maric C, Silva DM, Machado RP, de Buhr I, Heringer-Walther S, Pinheiro SV, Lopes MT, Bader M, Mendes EP, Lemos VS, Campagnole-Santos MJ, Schultheiss HP, Speth R, Walther T . Angiotensin-(1–7) is an endogenous ligand for the G protein-coupled receptor Mas. Proc Natl Acad Sci USA 2003; 100: 8258–8263.
Staessen J, Lijnen P, Fagard R, Verschueren LJ, Amery A . Rise in plasma concentration of aldosterone during long-term angiotensin II suppression. J Endocrinol 1981; 91: 457–465.
Struthers AD . Aldosterone escape during angiotensin-converting enzyme inhibitor therapy in chronic heart failure. J Card Fail 1996; 2: 47–54.
McKelvie RS, Yusuf S, Pericak D, Avezum A, Burns RJ, Probstfield J, Tsuyuki RT, White M, Rouleau J, Latini R, Maggioni A, Young J, Pogue J . Comparison of candesartan, enalapril, and their combination in congestive heart failure: randomized evaluation of strategies for left ventricular dysfunction (RESOLVD) pilot study. The RESOLVD Pilot Study Investigators. Circulation 1999; 100: 1056–1064.
Sato A, Saruta T . Aldosterone escape during angiotensin-converting enzyme inhibitor therapy in essential hypertensive patients with left ventricular hypertrophy. J Int Med Res 2001; 29: 13–21.
Horita Y, Taura K, Taguchi T, Furusu A, Kohno S . Aldosterone breakthrough during therapy with angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers in proteinuric patients with immunoglobulin A nephropathy. Nephrology (Carlton) 2006; 11: 462–466.
Yoneda T, Takeda Y, Usukura M, Oda N, Takata H, Yamamoto Y, Karashima S, Yamagishi M . Aldosterone breakthrough during angiotensin II receptor blockade in hypertensive patients with diabetes mellitus. Am J Hypertens 2007; 20: 1329–1333.
Naruse M, Tanabe A, Sato A, Takagi S, Tsuchiya K, Imaki T, Takano K . Aldosterone breakthrough during angiotensin II receptor antagonist therapy in stroke-prone spontaneously hypertensive rats. Hypertension 2002; 40: 28–33.
Ruilope LM, Schmieder RE . Left ventricular hypertrophy and clinical outcomes in hypertensive patients. Am J Hypertens 2008; 21: 500–508.
Tsutamoto T, Wada A, Maeda K, Hisanaga T, Mabuchi N, Hayashi M, Ohnishi M, Sawaki M, Fujii M, Horie H, Sugimoto Y, Kinoshita M . Plasma brain natriuretic peptide level as a biochemical marker of morbidity and mortality in patients with asymptomatic or minimally symptomatic left ventricular dysfunction. Comparison with plasma angiotensin II and endothelin-1. Eur Heart J 1999; 20: 1799–1807.
Roig E, Perez-Villa F, Morales M, Jimenez W, Orus J, Heras M, Sanz G . Clinical implications of increased plasma angiotensin II despite ACE inhibitor therapy in patients with congestive heart failure. Eur Heart J 2000; 21: 53–57.
Hudson M, Humphries K, Tu JV, Behlouli H, Sheppard R, Pilote L . Angiotensin II receptor blockers for the treatment of heart failure: a class effect? Pharmacotherapy 2007; 27: 526–534.
Acknowledgements
We thank R Watanabe for excellent technical assistance. We also thank D Mrozek for assistance in writing the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsutamoto, T., Nishiyama, K., Yamaji, M. et al. Comparison of the long-term effects of candesartan and olmesartan on plasma angiotensin II and left ventricular mass index in patients with hypertension. Hypertens Res 33, 118–122 (2010). https://doi.org/10.1038/hr.2009.192
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.192
Keywords
This article is cited by
-
Aldosterone breakthrough from a pharmacological perspective
Hypertension Research (2022)
-
Effects of Angiotensin II Receptor Blockers on Ventricular Hypertrophy in Hypertrophic Cardiomyopathy: A Meta-Analysis of Randomized Controlled Trials
Cardiovascular Drugs and Therapy (2022)
-
High-dose nitrate therapy recovers the expression of subtypes α1 and β-adrenoceptors and Ang II receptors of the renal cortex in rats with myocardial infarction-induced heart failures
BMC Cardiovascular Disorders (2020)
-
Effects of a changeover from other angiotensin II receptor blockers to olmesartan on left ventricular hypertrophy in heart failure patients
Heart and Vessels (2017)
-
Olmesartan reduces inflammatory biomarkers in patients with stable coronary artery disease undergoing percutaneous coronary intervention: results from the OLIVUS trial
Heart and Vessels (2014)