Abstract
The detrimental effects of cigarette smoking on the kidney in healthy individuals without established renal diseases have not been established. We evaluated the effects of smoking on renal function and proteinuria in 35 288 apparently healthy participants who were not on antihypertensive and/or antidiabetic medication and who had undergone a health examination at the Health Promotion Center, Seoul National University Hospital from 1995 to 2006. Renal function was estimated using the simplified Modification of Diet in Renal Disease Study equation for estimated glomerular filtration rate (eGFR), and proteinuria was determined by the spot urine dipstick test. Adjusted eGFR was higher in current smokers (mean±s.e.m., 79.3±0.1 ml min−1) than in ex-smokers (77.3±0.2 ml min−1, P<0.001) and non-smokers (77.7±0.1 ml min−1, P<0.001). The adjusted eGFR of smokers who smoked >20 cigarettes per day were higher than that of individuals who smoked ⩽20 cigarettes per day (P<0.001). In participants with an eGFR of <50 ml min−1, current smoking (38.3±1.9 ml min−1) and past smoking (39.5±1.9 ml min−1) were associated with significantly lower eGFR values than non-smoking (45.1±1.2 ml min−1; P=0.007 and P=0.027, respectively). Current smoking was associated with a higher risk of proteinuria (urine dipstick for albuminuria ⩾1+) than non-smoking (odds ratio=1.380, P<0.001). In conclusion, cigarette smoking is associated with a higher eGFR in the general population, whereas it might reduce eGFR in a small subset of the population and increase the risk of proteinuria. These subsets should be better defined to prevent chronic kidney diseases related to smoking in the general population.
Similar content being viewed by others
Introduction
Chronic kidney disease (CKD) is a risk factor not only for end-stage renal disease but also for cardiovascular diseases,1 and has been documented to be associated with increased cardiovascular2 and all-cause mortality.1, 2, 3 The risk factors of CKD are of major concern, because the prevalence of CKD is rapidly increasing, especially in developing countries.4 This increased prevalence of CKD is matched by similar increases in the prevalence of risk factors for CKD, such as diabetes, hypertension, obesity and an age greater than 60 years.5
Smoking is a well-known risk factor for many serious diseases, including pulmonary, cardiovascular and neurologic diseases,6 and there is much experimental evidence to show that cigarette smoking induces renal damage.7, 8, 9 The detrimental effect of smoking on established renal diseases is relatively well documented, but its effects on the glomerular filtration rate (GFR) and the risk for proteinuria remain controversial, especially in the general population. Some reported that cigarette smoking was associated with a decreased GFR,10, 11, 12 whereas others concluded that GFR was significantly higher in current smokers than in non-smokers or ex-smokers.13, 14 On the other hand, Zhang et al.15 reported that GFR in smokers was not significantly different from that in non-smokers or ex-smokers.
In addition, cigarette smoking was shown to increase the risk of proteinuria (an established predictor of a decreased renal function) in the general population,16, 17, 18, 19 though not all studies agreed.15 The discrepancy between the reports on the effects of smoking on GFR and proteinuria is not clearly explained.
In this study, we examined the effects of cigarette smoking on renal function and albuminuria in 35 288 apparently healthy participants who were not on antihypertensive and/or antidiabetic medication, and we investigated whether the association between smoking status and GFR was modified by the renal functional status, sex, age, blood pressure (BP), fasting serum glucose, degree of obesity and albuminuria.
Methods
Participants
Between March 1995 and May 2006, 49 038 participants, aged over 20 years, underwent comprehensive health examinations, including cancer, diabetes and hypertension screening, at the Health Promotion Center, Seoul National University Hospital. A total of 13 750 participants with incomplete records or who were being treated for diabetes or hypertension at the time of the evaluation were excluded. Finally, a total of 35 288 participants were included in the analysis. The Seoul National University Hospital institutional review board approved the study protocol.
Baseline measurements
Information on medication for diabetes or hypertension at the time of examination, smoking status, alcohol consumption and exercise was obtained using a structured self-reporting questionnaire, and validated by trained nurses. Smoking status was classified into three categories; smoker, ex-smoker and non-smoker. Participants who smoked at least one cigarette per day at the time of the health examination were classified as smokers. For smokers, daily numbers of cigarettes smoked were determined, and they were then divided into two subgroups: light smokers ⩽20 cigarettes per day and heavy smokers >20 cigarettes per day. Participants who reported that they did not smoke at the time of examination, but had smoked earlier were classified as ex-smokers. Non-smokers were defined as those who had never smoked. History of alcohol consumption was classified based on the average number of times per week they had consumed alcohol during the month before screening. Regular drinkers were defined as those who drank alcoholic beverages at least once a week. Regular exercise was defined as an exercise lasting more than 30 min, at least three times a week.
Height and weight were measured after an overnight fast, with participants wearing a lightweight gown. Body mass index (BMI) was calculated by dividing weight (kg) by height (m) squared. BP was measured using an automated BP-measuring device (Jawon, Pusan, Korea) after resting, for at least 20 min, in a sitting position. High BP was defined as a systolic BP⩾130 mm Hg or a diastolic BP⩾85 mm Hg. Blood samples were drawn after an overnight fast. Serum creatinine was measured using the Jaffe kinetic method (Toshiba 200FR Autoanalyzer, Japan). Within-run and total coefficients of variation for creatinine determinations were no greater than 3% during the study period. The test was conducted in a clinical laboratory, which was inspected and surveyed annually by the Korean Association of Quality Assurance for Clinical Laboratories.
Urine albumin was determined semiquantitatively by single spot urine dipstick analysis (URiSCAN Urine Strip; YD Diagnostics, Yong-In, Korea). Dipstick urinalysis was performed on midstream urine samples collected in the morning. Urine albumin amounts were reported as grades, that is, absent, trace, 1+, 2+, 3+ and 4+, and albuminuria was defined as grade 1+ or greater. GFRs were estimated using the simplified Modification of Diet in Renal Disease Study equation.20
Statistical analysis
All statistical analyses were carried out using SPSS version 13.0. Distributions of participant characteristics by smoking status and sex were compared by one-way analysis of variance for continuous variables, and by the χ2 test for categorical variables. The effects of smoking status on eGFR were evaluated by multivariate linear regression analysis after adjusting for potential confounders, which included age, sex, systolic BP, diastolic BP, BMI, fasting serum glucose and serum total cholesterol. The effects of smoking on discrete dependent variables, such as decreased eGFR (<60 ml min−1), albuminuria and high BP, were evaluated using multivariate logistic regression analysis. In addition, stratified analyses were performed with respect to eGFR (<50 or ⩾50 ml min−1), sex, age (⩽55 years or >55 years), BP (<130/85 or ⩾130/85 mm Hg), BMI (⩽25 or >25 kg/m2), fasting serum glucose (⩽100 or >100 mg per 100 ml) and albuminuria (a urine dipstick finding of negative/trace or ⩾1+) to examine the possible differential effects of smoking on eGFR. Probability levels of lower than 0.05 were considered statistically significant based on a two-sided test.
Results
The characteristics of the study participants are shown in Table 1. Of the 17 985 men, 8782 (48.8%) were smokers, 5821 (32.4%) were ex-smokers and 3382 (18.8%) were non-smokers. The proportions of smokers (904/17 303, 5.2%) and ex-smokers (495/17 303, 2.9%) among women were considerably lower. Age, BMI, glucose, regular exercise and lipid profiles showed a linear trend in both men and women across the smoking status.
Systolic BP was lower in smokers than in non-smokers and ex-smokers (125.3±18.5 vs 130.9±19.4 and 131.8±18.7 mm Hg, respectively, in men; 116.6±18.6 vs 126.7±20.3 and 120.8±21.0 mm Hg, respectively, in women). The pattern of association between diastolic BP and smoking status was similar to that between systolic BP and smoking status. The prevalence of high BP (systolic BP ⩾130 mm Hg or diastolic BP ⩾85 mm Hg) was lower in smokers than in non-smokers and in ex-smokers for both sexes (42.2 vs 54.5 and 57.0%, respectively, in men; 22.6 vs 42.7 and 29.4%, respectively, in women).
Unadjusted eGFR was higher in smokers than in non-smokers and in ex-smokers for both sexes (79.7±12.3 vs 77.1±11.7 and 76.4±12.0 ml min−1, respectively, in men; 79.9±13.3 vs 77.9±13.0 and 79.2±14.6 ml min−1, respectively, in women). In men, the prevalence of a decreased eGFR (eGFR <60 ml min−1) was significantly lower in smokers than in non-smokers and in ex-smokers (3.1 vs 5.0 and 5.6%, respectively, in men); however, this association was not significant in women (3.7 vs 5.4 and 6.1%, respectively, in women). The prevalence of albuminuria in smokers, non-smokers and ex-smokers were 5.2, 4.6 and 4.1%, in men, and 4.4, 2.4 and 2.1%, in women, respectively, and there was significantly increased prevalence of albuminuria in smokers than in non-smokers and in ex-smokers (P=0.006 in men, P=0.001 in women).
The risk of a decreased eGFR (eGFR <60 ml min−1) was not significantly different between non-smokers and ex-smokers, as shown in Table 2. The odds ratio (OR) (95% confidence interval, CI) of heavy smokers who smoke more than 20 cigarettes per day was 0.733 (0.598–0.899) and that of light smokers who smoke 20 cigarettes per day or less was 0.763 (0.617–0.943). The dose–response relationship between a decreased GFR and the smoking status was observed only in men (P-value for trend=0.002).
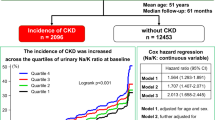
Multiple linear regression analysis using a general linear model showed that the means (±s.e.m.) of eGFRs of non-smokers, ex-smokers, light smokers and heavy smokers were 77.7±0.1, 77.3±0.2, 78.8±0.2 and 79.8±0.2 ml min−1, respectively, and that of the eGFRs of light and heavy smokers were significantly higher than those of non-smokers and ex-smokers (P<0.001 for each comparisons) as shown in Figure 1, and that the eGFR of heavy smokers was significantly higher than that of light smokers (P<0.001), after adjusting for age, sex, BMI, systolic and diastolic BP, fasting serum glucose and serum total cholesterol. However, the eGFRs of non-smokers and ex-smokers were not significantly different (P=0.108) in Figure 1.
The impacts of cigarette smoking on estimated glomerular filtration rates (eGFRs). Group means were compared by multiple linear regression analyses using a general linear model adjusted for age, sex, systolic and diastolic blood pressure, fasting serum glucose, serum total cholesterol and body mass index. Error bars represent standard errors. (1) Significantly different from non-smokers (P<0.001), (2) significantly different from ex-smokers (P<0.001), (3) significantly different from light smokers (P<0.001), (4) ⩽20 cigarettes per day and (5) >20 cigarettes per day.
Subgroup analyses were performed according to eGFR (<50 or ⩾50 ml min−1), sex, age (⩽55 years or >55 years), BP (<130/85 or ⩾130/85 mm Hg), fasting serum glucose (⩽100 or >100 mg per 100 ml), BMI (<25 or ⩾25 kg/m2) and the presence of albuminuria (a urine dipstick finding of negative/trace or ⩾1+). In the subgroup with an eGFR <50 ml min−1, the means (±s.e.m.) of the eGFRs of smokers, ex-smokers and non-smokers were 38.3±1.9, 39.5±1.9 and 45.1±1.2 ml min−1, respectively. The eGFRs of smokers and ex-smokers were significantly lower than those of non-smokers (P-value for smokers vs non-smokers=0.007 and P-value for ex-smokers vs non-smokers=0.027, Figure 2), but no significant difference was observed between the eGFRs of smokers and ex-smokers (P=0.651, Figure 2). The eGFRs of smokers were significantly higher than those of ex-smokers and non-smokers in all subgroups of age, BP, fasting serum glucose and BMI, whereas the eGFR was not significantly different across the smoking status in participants with albuminuria (data not shown).
The impact of cigarette smoking on estimated glomerular filtration rate (eGFR) according to renal function. Group means were compared by multiple linear regression analyses using a general linear model adjusted for age, sex, systolic and diastolic blood pressure, fasting serum glucose, serum total cholesterol and body mass index. Error bars represent standard errors. (1) Significantly different from non-smokers and (2) significantly different from ex-smokers.
Current cigarette smoking was found to be associated with an increased risk of albuminuria, and the ORs (95% CI) of albuminuria of light and heavy smokers were 1.325 (1.079–1.627) and 1.425 (1.174–1.729), but this was not the case for ex-smokers (OR 0.947, 95% CI: 0.779–1.152), after adjusting for age, sex, systolic and diastolic BP, BMI, fasting serum glucose, serum total cholesterol, serum triglyceride and serum HDL cholesterol (Table 3). Systolic and diastolic BPs were lower in smokers than in non-smokers and ex-smokers in both sexes, as shown in Table 1. The ORs (95% CIs) for high BP were 0.908 (0.838–0.984) for ex-smokers, 0.636 (0.582–0.695) for light smokers and 0.600 (0.551–0.653) for heavy smokers. A lower risk of high BP was also observed in smokers of both sexes (OR 0.657, 95% CI: 0.593–0.728 in light smoking men, OR 0.605, 95% CI: 0.551–0.663 in heavy smoking men; OR 0.530, 95% CI: 0.431–0.652 in light smoking women, OR 0.546, 95% CI: 0.381–0.785 in heavy smoking women) in Table 4.
Discussion
In this study, it was observed that smokers had higher eGFR and a lower risk of an eGFR of <60 ml min−1 than did ex-smokers and non-smokers; however, in participants with a reduced renal function (eGFR <50 ml min−1), smokers had lower eGFR than did non-smokers. Furthermore, smokers were found to have a higher risk of albuminuria regardless of renal functional status.
Various results regarding the association between smoking status and eGFR exist. Several studies have concluded that cigarette smoking is associated with a higher GFR, which is consistent with our results.13, 14 However, other studies have shown contrary findings of smoking being associated with a greater risk of a decreased GFR.10, 11, 12 Moreover, smoking has also been reported to be associated with an increased eGFR (⩾90 ml min−1) and a decreased GFR (<60 ml min−1) in the same population.13, 16 These results suggest that the impact of cigarette smoking on renal function, which differs for specific subgroups in the general population, might depend on the renal functional status. We observed that eGFRs across different smoking statuses in participants with an eGFR of <50 ml min−1 differed from those in participants with an eGFR of ⩾50 ml min−1. In particular, the mean eGFRs of smokers and ex-smokers with an eGFR of <50 ml min−1 were lower than that of non-smokers after adjusting for potential confounders. These findings suggest that smoking is associated with a higher GFR and a reduced risk of a decreased GFR in the general population, but that it is associated with a lower GFR in a subset of the population. On the basis of our observation that high BP, impaired fasting glucose or albuminuria was not associated with a differential renal response to smoking, it could be that those with an underlying renal disease are not the specific subgroup that is susceptible to a reduction in eGFR because of cigarette smoking. A number of longitudinal, large community-based cohort studies have concluded that cigarette smoking was an independent risk factor of end-stage renal disease, but these studies did not examine the specific subgroups who were more susceptible to a detrimental renal response to cigarette smoking.11, 21 Several studies have suggested the existence of a gender-specific renal response to chronic smoke exposure.22, 23, 24 In this study, we failed to observe a detrimental effect of smoking on renal function in women, but this might have been because of a loss of statistical power owing to the low proportion of female smokers in our population.22
In addition, we also observed that cigarette smoking was associated with an increased risk of albuminuria, dose dependently. Our result regarding this association between smoking and an increased risk of albuminuria is consistent with earlier findings.16, 17, 18, 19 Moreover, the absence of a relationship between decreased eGFR and smoking in participants with albuminuria suggests that the mechanism of albuminuria and a decreased GFR because of cigarette smoking might be independent of each other. To elucidate the pathophysiological mechanisms responsible for reducing GFR among smokers with an eGFR of <50 ml min−1, we would have to define a population subset whose renal functions are detrimentally affected by smoking, which raises the possibility that genetic factors may be responsible for this sensitivity.25, 26
We observed that cigarette smoking was associated with lower BP and decreased risk for high BP after adjustment for sex, age, BMI, regular alcohol intake, eGFR, albuminuria and fasting serum glucose. Although cigarette smoking induces acute increase of BP and pulse rate in humans through adrenergic mechanisms,7 chronic cigarette smoking has been reported to be associated with lower systolic and diastolic BP in a cross-sectional epidemiological study of the general population27, 28, 29, 30, 31 and with less increase of BP in chronic smokers after a follow-up of 5 years.30, 32 A longitudinal study documented that being a never smoker was an independent risk factor for higher increase in BP over 7 years.33 Our observation of the association between smoking and higher GFR and lower BP was consistent with earlier reports. It is difficult to explain the discrepancies between acute response to cigarette smoking, possibly mediated by adrenergic mechanisms, and the results of epidemiological studies. The mechanism of decrease in BP and that of increase in GFR by cigarette smoking might be closely related to each other. Moreover, decrease in vascular resistance might also be involved. The possible difference in renal hemodynamic response to cigarette smoking between non-smokers and habitual smokers has been proposed. In smokers, in contrast with non-smokers, effective renal plasma flow and GFR remained unchanged, whereas urinary cyclic GMP rose by 87±43%, and the changes in effective renal plasma flow induced by nicotine were positively correlated with changes in urinary cyclic GMP.16 As an increase in urinary cyclic GMP has been suggested to be a marker of renal vasodilation, repeated exposure to these vasodilatory compounds might cause chronic glomerular hyperfiltration in habitual smokers.13 Therefore, it is possible that, although cigarette smoking causes a decrease in vascular resistance resulting in lower BP and higher GFR in the general population, chronic smoking lowers GFR through unknown mechanism(s) in a small subset of the population. Although acute smoking caused a decrease in GFR and an increase in the mean arterial pressure in healthy normotensive volunteers, acute smoking did not cause a significant change in GFR and BP in patients with IgA nephropathy.8 These results suggest a differential hemodynamic or renal response to smoking according to the pathophysiological conditions of participants. It is necessary to characterize these susceptible participants by longitudinal studies on large cohorts. As it was reported that chronic cigarette smokers were hyperinsulinemic,34 and that physiological and supraphysiological doses of insulin increased GFR in normal participants,35 further studies are needed to evaluate the possibility that hyperinsulinemia caused by chronic smoking increases GFR in normal participants.
Our study was conducted on a relatively large number of participants who had undergone a thorough health check up at a single center. As GFR is influenced by a wide spectrum of factors, a considerable sample size is required to obtain sufficient statistical power to evaluate the effect of smoking on GFR in various subgroups. Furthermore, in this study, all participants were evaluated at a single medical center using the same evaluation protocols. It is particularly important for the measurement of creatinine, which is prone to inter-laboratory variations.
Our study was retrospective and cross-sectional in nature, and its participants were of a single ethnic origin, which might limit the generalization of our results. In addition, we admit that insufficient information was available on behavioral factors, such as alcohol consumption and salt intake.
In conclusion, this study showed that cigarette smoking was associated with a lower risk of a decreased GFR and a higher risk of proteinuria in the general population, but that in a population with a reduced renal function (eGFR <50 ml min−1), smoking was associated with a reduction in eGFR. Prospective studies, including genotype analysis, are needed to characterize those who are susceptible to chronic smoke exposure.
References
Wen CP, Cheng TYD, Tsai MK, Chang YC, Chan HT, Tsai SP, Chiang PH, Hsu CC, Sung PK, Hsu YH, Wen SF . All-cause mortality attributable to chronic kidney disease: a prospective cohort study based on 462,293 adults in Taiwan. Lancet 2008; 371: 2173–2182.
Astor BC, Hallan SI, Miller III ER, Yeung E, Coresh J . Glomerular filtration rate, albuminuria, and risk of cardiovascular and all cause mortality in the US population. Am J Epidemiol 2008; 167: 1226–1234.
Maaravi Y, Bursztyn M, Hammerman-Rozenberg R, Stessman J . Glomerular filtration rate estimation and mortality in an elderly population. Q J Med 2007; 100: 441–449.
Weiner DE . Causes and consequences of chronic kidney disease: implications for managed health care. J Manag Care Pharm 2007; 13 (Suppl): S1–S9.
Vassalotti JA, Stevens LA, Levey AS . Testing for chronic kidney disease: a position statement from the National Kidney Foundation. Am J Kidney Dis 2007; 50: 169–180.
Das SK . Harmful health effects of cigarette smoking. Mol Cell Biochem 2003; 253: 159–165.
Cryer PE, Haymond MW, Santiago JV, Shah SD . Norepinephrine and epinephrine release and adrenergic mediation of smoking-associated hemodynamic and metabolic events. N Engl J Med 1976; 295: 573–577.
Ritz E, Benck U, Franek E, Keller C, Seyfarth M, Clorius J . Effects of smoking on renal hemodynamics in healthy volunteers and in patients with glomerular disease. J Am Soc Nephrol 1998; 9: 1798–1804.
Gambaro G, Verlato F, Budakovic A, Casara D, Saladini G, Del Prete D, Bertaglia G, Masiero M, Checchetto S, Baggio B . Renal impairment in chronic cigarette smokers. J Am Soc Nephrol 1998; 9: 562–567.
Hallan S, de Mutsert R, Carlsen S, Dekker FW, Aasarød K, Holmen J . Obesity, smoking, and physical inactivity as risk factors for CKD: are men more vulnerable? Am J Kidney Dis 2006; 47: 396–405.
Shankar A, Klein R, Klein BEK . The association among smoking, heavy drinking, and chronic kidney disease. Am J Epidemiol 2006; 164: 263–271.
Yamagata K, Ishida K, Sairenchi T, Takahashi H, Ohba S, Shiigai T, Narita M, Koyama A . Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int 2007; 71: 159–166.
Halimi JM, Philippon C, Mimran A . Contrasting renal effects of nicotine in smokers and non-smokers. Nephrol Dial Transplant 1998; 13: 940–944.
Noborisaka Y, Honda R, Ishizaki M, Nakata M, Yamada Y . Alcohol and cigarette consumption, renal function and blood pressure in middle-aged healthy men. J Hum Hypertens 2007; 21: 966–968.
Zhang L, Zhang P, Wang F, Zuo L, Zhou Y, Shi Y, Li G, Jiao S, Liu Z, Liang W, Wang H . Prevalence and factors associated with CKD: a population study from Beijing. Am J Kidney Dis 2008; 51: 373–384.
Halimi JM, Giraudeau B, Vol S, Cacès E, Nivet H, Lebranchu Y, Tichet J . Effects of current smoking and smoking discontinuation on renal function and proteinuria in the general population. Kidney Int 2000; 58: 1285–1292.
Pinto-Sietsma SJ, Mulder J, Janssen WMT, Hillege HL, de Zeeuw D, de Jong PE . Smoking is related to albuminuria and abnormal renal function in nondiabetic persons. Ann Intern Med 2000; 133: 585–591.
De Cosmo S, Lamacchia O, Rauseo A, Viti R, Gesualdo L, Pilotti A, Trischitta V, Cignarelli M . Cigarette smoking is associated with low glomerular filtration rate in male patients with type 2 diabetes. Diabetes Care 2006; 29: 2467–2470.
Ishizaka N, Ishizaka Y, Toda E, Shimomura H, Koike K, Seki G, Nagai R, Yamakado M . Association between cigarette smoking and chronic kidney disease in Japanese men. Hypertens Res 2008; 31: 485–492.
Van Biesen W, De Bacquer D, Verbeke F, Delanghe J, Lameire N, Vanholder R . The glomerular filtration rate in an apparently healthy population and its relation with cardiovascular mortality during 10 years. Eur Heart J 2007; 28: 478–483.
Stengel B, Tarver-Carr ME, Powe NR, Eberhardt MS, Brancati FL . Lifestyle factors, obesity and the risk of chronic kidney disease. Epidemiology 2003; 14: 479–487.
Orth SR, Stockmann A, Contradt C, Ritz E, Ferro M, Kreusser W, Piccoli G, Rambausek M, Roccatello D, Schäfer K, Sieberth HG, Wanner C, Watschinger B, Zucchelli P . Smoking as a risk factor for end-stage renal failure in men with primary renal disease. Kidney Int 1998; 54: 926–931.
Tozawa M, Iseki K, Iseki C, Oshiro S, Ikemiya Y, Takishita S . Influence of smoking and obesity on the development of proteinuria. Kidney Int 2002; 62: 956–962.
Briganti EM, Branley P, Chadban SJ, Shaw JE, McNeil JJ, Welborn TA, Atkins RC . Smoking is associated with renal impairment and proteinuria in the normal population: the AusDiab Kidney Study. Am J Kidney Dis 2002; 40: 704–712.
Wang XL, Sim AS, Badenhop RF, McCredie RM, Wilcken DE . A smoking-dependent risk of coronary artery disease associated with a polymorphism of the endothelial nitric oxide synthase gene. Nat Med 1996; 2: 41–45.
Perna A, Iordache BE, Bettinaglio P, Ruggenenti P, Noris M, Galbusera A, Caprioli J, Rubis N, Gritti D, Fassi A, Remuzzi G, DD ACE genotype and smoking cluster with high-normal albuminuria: a cross sectional analysis in 1209 normo-albuminuric type 2 diabetics enrolled in the BErgamo NEphrologic DIabetes Complication Trial (BENEDICT). J Am Soc Nephrol 2001; 12: 154A.
Green MS, Jucha E, Luz Y . Blood pressure in smokers and nonsmokers: epidemiologic findings. Am Heart J 1986; 111: 932–940.
Teshima K, Imamura H, Uchida K, Miyamoto N, Masuda Y, Kobata D . Cigarette smoking, blood pressure and serum lipids in Japanese men aged 20–39 years. J Physiol Anthropol 2001; 20: 43–45.
Imamura H, Uchida K, Kobata D . Relationship of cigarette smoking with blood pressure, serum lipids and lipoproteins in young Japanese women. Clin Exp Pharmacol Physiol 2000; 27: 364–369.
Okubo Y, Miyamoto T, Suwazono Y, Kobayashi E, Nogawa K . An association between smoking habits and blood pressure in normotensive Japanese men. J Hum Hypertens 2002; 16: 91–96.
Criqui MH, Mebane I, Wallace RB, Heiss G, Holdbrook MJ . Multivariate correlates of adult blood pressures in nine North American populations: the Lipid Research Clinics Prevalence Study. Prev Med 1982; 11: 391–402.
Okubo Y, Suwazono Y, Kobayashi E, Nogawa K . An association between smoking habits and blood pressure in normotensive Japanese men: a 5-year follow-up study. Drug Alcohol Depend 2004; 73: 167–174.
Metcalf P, Scragg R, Jackson R . Blood pressure changes over 7 years in a large workforce cohort in New Zealand. N Z Med J 2006; 119: U2311.
Facchini FS, Hollenbeck CB, Jeppesen J, Chen YD, Reaven GM . Insulin resistance and cigarette smoking. Lancet 1992; 339: 1128–1130.
ter Maaten JC, Bakker SJ, Serné EH, ter Wee PM, Donker AJ, Gans RO . Insulin's acute effects on glomerular filtration rate correlate with insulin sensitivity whereas insulin's acute effects on proximal tubular sodium reabsorption correlate with salt sensitivity in normal subjects. Nephrol Dial Transplant 1999; 14: 2357–2363.
Acknowledgements
This study was supported by the SNUH Research Fund (Grant No. 03-2001-062-0).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoon, HJ., Park, M., Yoon, H. et al. The differential effect of cigarette smoking on glomerular filtration rate and proteinuria in an apparently healthy population. Hypertens Res 32, 214–219 (2009). https://doi.org/10.1038/hr.2008.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2008.37
Keywords
This article is cited by
-
Competitive interaction between smoking and chronic obstructive pulmonary disease for explaining renal function reduction in hypertensive patients
Internal and Emergency Medicine (2023)
-
Association of Single Measurement of dipstick proteinuria with physical performance of military males: the CHIEF study
BMC Nephrology (2020)
-
The role of cigarette smoking on new-onset of chronic kidney disease in a Japanese population without prior chronic kidney disease: Iki epidemiological study of atherosclerosis and chronic kidney disease (ISSA-CKD)
Clinical and Experimental Nephrology (2020)
-
Effects of smoking and its cessation on creatinine- and cystatin C-based estimated glomerular filtration rates and albuminuria in male patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry
Hypertension Research (2016)
-
The effects of continuing and discontinuing smoking on the development of chronic kidney disease (CKD) in the healthy middle-aged working population in Japan
Environmental Health and Preventive Medicine (2013)