Abstract
Marshall–Stickler syndrome represents a spectrum of inherited connective tissue disorders affecting the ocular, auditory, and skeletal systems. The syndrome is caused by mutations in the COL2A1, COL11A1, COL11A2, COL9A1, and COL9A2 genes. In this study, we examined four Turkish families with Marshall–Stickler syndrome using whole-exome sequencing and identified one COL2A1 mutation and three COL11A1 mutations. Two of the COL11A1 mutations were novel. Our findings expand our knowledge of the COL11A1 mutational spectrum that causes Marshall–Stickler syndrome.
Similar content being viewed by others
Marshall and Stickler syndromes are phenotypically overlapping connective tissue disorders characterized by ocular, auditory, skeletal, and orofacial abnormalities.1,2 Most patients develop eye manifestations, including myopia, vitreoretinal degeneration, retinal detachment, and cataracts. Additional features include cleft palate, micrognathia, flat midface, hearing loss, and skeletal abnormalities.3
Marshall and Stickler syndromes are clinically variable and genetically heterogeneous. Based on the causal genes, Stickler syndromes are classified into five different subtypes: type I (STL1; MIM 108300), type II (STL2; MIM 604841), type III (STL3; MIM 184840), type IV (STL4; MIM 614134), and type V (STL5; MIM 614284). STL1, STL2, and STL3 are autosomal dominant disorders caused by mutations in the COL2A1 (MIM 120140),4,5 COL11A1 (MIM 120280),6,7 and COL11A2 genes (MIM 120290),8,9 respectively. STL4 and STL5 are autosomal recessive disorders caused by mutations in COL9A1 (MIM 120210)10,11 and COL9A2 (MIM 120260),12 respectively. Marshall syndrome (MIM 154780) and STL2 have the same causal gene, COL11A1,13,14 and are considered to constitute an identical clinical spectrum.6
In this study, we conducted whole-exome sequencing and identified two novel and one recurrent COL11A1 splice-site mutations, and one recurrent COL2A1 mutation in four unrelated Turkish patients with the Marshall–Stickler syndrome spectrum.
The study protocol was approved by the Ethics Committee of RIKEN and participating institutions, and informed consent was obtained from all participants. The clinical manifestations are described below and summarized in Table 1. More detailed information is available in Supplementary Material.
Patient 1 from Family A was a baby boy who was referred to our genetics clinic because of his familial degenerative myopia, mild deafness, and mild hypermobility. He is the younger child of a non-consanguineous couple who had two children (Supplementary Figure S1). After birth, he presented with severe hypotonia and contractures of the hands. Physical examination at 1.5 years of age revealed that his weight was 12.6 kg (50–75th percentile), height 84 cm (75–90th percentile), and occipital frontal circumference (OFC) 48.2 cm (50th percentile). He had a mildly depressed nasal bridge, mild micrognathia, hypermobility of the finger joints, and phimosis (Figure 1a,b). Eye examination revealed degenerative myopia (−5.75/−5.25) and tigroid retinae. He had mild hearing loss (10 dB, mixed type).
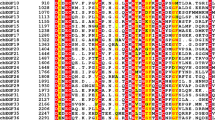
Physical appearance of the patients. (a, b) Case 1, age 1.5 years. Mild depression of the nasal bridge and micrognathia. (c) Case 2, age 1 month. Buphthalmic eyes, hypertelorism, bilateral epicanthus, flat face, depressed nasal bridge, short stubby nose, and micro-retrognathia. (d, e) Case 4, age 8.5 years. Proptotic eyes, flat face with mild frontal bossing, depressed nasal bridge, and short nose. (f, g) Case 3, age 9 months. Buphthalmic eyes, flat face with frontal bossing, midfacial hypoplasia, depressed nasal bridge, short nose with anteverted nares, long philtrum, and micro-retrognathia. (h–j) Case 3, age 9 years. (h, i) High-frontal area, big proptotic eyes, long palpebral fissures, depressed nasal bridge, short nose, long philtrum, irregular teeth order, micrognathia, and dry rough hairs. (j) Small hands with brachydactyly.
Patient 2 from Family B was a newborn girl who was referred to the genetics clinic because of her Pierre Robin sequence (the triad of micro-retrognathia, cleft palate, and glossoptosis). She was the only child of unrelated healthy parents (Supplementary Figure S1). The first physical examination at the age of 1 month revealed that her weight was 3,080 g (10–25th percentile), length 49 cm (10–25th percentile), and OFC 35 cm (10–25th percentile). She presented with a flat face with a depressed profile, buphthalmic eyes, hypertelorism, bilateral epicanthus, depressed nasal bridge, short stubby nose, and Pierre Robin sequence (Figure 1c). She also had axial hypotony and pectus excavatum. Echocardiography revealed atrial septal defect (ASD). Strabismus, myopia, and megalocornea (corneal diameter 11 mm/11 mm) were followed later with growth retardation and deafness, which needed ear tube insertion. Her height fell under the third percentile at age 4 years.
Patient 3 from Family C was a baby girl who was referred to us because of cleft palate, deafness, and facial dysmorphism. She was born as the second child of a Turkish family consisting of non-consanguineous parents and a healthy elder boy (Supplementary Figure S1). Cleft palate was recognized at birth, and deafness was observed at the age of 4 months. When she was first examined at the age of 9 months, she had a very flat face with frontal bossing, buphthalmic eyes, midfacial hypoplasia, flat nasal bridge, hypoplastic depressed short nose with anteverted nares, long philtrum, cleft palate, bifid uvula, small mouth and chin, and micro-retrognathia (Figure 1f,g). Audiological evaluation confirmed severe sensorineural deafness bilaterally. Eye examination revealed tigroid retinae, 10.5 mm corneal diameter, and 11 mmHg intraocular pressure. Her follow-up examination at the age of 9 years revealed that her weight was 21.5 kg (3rd–10th percentile), height 113 cm (<3rd percentile), and OFC 51 cm (2nd–50th percentile). Her main problems were large proptotic eyes, long palpebral fissures, degenerative high myopia (−22/−22), cone dystrophy (detected by electroretinography), retinal pigmentation, right cataract, deafness (wearing a hearing aid), high-frontal area, depressed nasal bridge, hypoplastic short nose, repaired cleft palate, irregular teeth order, long philtrum, micrognathia, short stature, small hands with brachydactyly, and dry rough hairs (Figure 1h–j).
Patient 4 from Family D was an 8.5-year-old boy who suffered from high myopia, deafness, short stature, and facial dysmorphism. His consanguineous parents and his elder brother were healthy (Supplementary Figure S1). The prenatal and postnatal course were uneventful. Physical examination at the age of 8.5 years revealed that his weight was 32.5 kg (75–90th percentile), height 122 cm (10th percentile), and OFC 57 cm (97th percentile). He had macrocephaly, flat face with midfacial hypoplasia, mild frontal bossing, depressed nasal bridge, short nose, anteverted nares, proptotic eyes, severe myopia (−17/−17), glaucoma with 14 mmHg intraocular pressure, bifid uvula, sensorineural deafness, and short hands with brachydactyly (Figure 1d,e).
Whole-exome sequencing was performed as previously described (Supplementary Methods, Supplementary Table S1).15–18 The identified variants were confirmed by Sanger sequencing. We identified three heterozygous variants in COL11A1 (NM_001854: c.1845+1G>A, c.2808+1G>C, c.3816+1G>A) and one heterozygous variant in COL2A1 (NM_001844: c.2710C>T) in the four unrelated patients, respectively. COL11A1 and COL2A1 mutations are known to cause Marshall–Stickler syndrome.4–7 No potential mutations in any known disease genes, including other disease genes of Stickler syndrome (COL11A2, COL9A1, and COL9A2), were identified.4,5 By Sanger sequencing, we confirmed the variants in the patients. We also verified that c.2808+1G>C, c.3816+1G>A and c.2710C>T are de novo variants due to their absence in the patients’ parents’ genomes (Supplementary Figure S2).
c.3816+1G>A13 and c.2710C>T19 are recurrent mutations in the Marshall–Stickler syndromes and have been annotated in The Human Gene Mutation Database (HGMD) as mutations (CS982120 and CM980396, respectively). By contrast, both c.1845+1G>A and c.2808+1G>C have not been deposited in any available public databases, including dbSNP, 1,000 genomes, ExAC, ESP6500, and HGMD. Similar to the known mutation c.3816+1G>A, both of the novel variants also located at splice donor sites of the intronic sequences of COL11A1 (intron 18, 36, and 50, respectively; Supplementary Figure S2). According to the GT–AG rule, the two novel variants would certainly disrupt the donor-site motifs. Several in silico splice-site prediction programs indicated that the donor splice sites around these variants disappeared or were weakened greatly, suggesting aberrant splicing (Supplementary Table S2). Thus, the two novel splice-site variants in our study would be pathogenic mutations. Until now, more than 20 splice-site mutations in COL11A1 related to Marshall-STL2 Stickler syndrome have been reported. Our results will further expand our knowledge of the mutational spectrum of the COL11A1 gene.
The characteristics of Marshall–Stickler syndrome spectrum caused by COL11A1 are different from those caused by COL2A1.14 The most important aspects of the differential diagnosis are that the patients with COL11A1 mutations more commonly had severe hearing impairment than those with COL2A1 mutations. In addition, the patients with COL11A1 mutations seldom had vitreoretinal degeneration and retinal detachment compared with the high incidence in those with COL2A1 mutations.14 However, in our study, Case 4 with COL2A1 mutation presented with severe hearing impairment; Cases 1 and 3 with COL11A1 mutations had retinal detachment and/or retinal degeneration to a certain extent. Additionally, Marshall–Stickler syndrome caused by COL11A1 is considered to have a higher incidence of midfacial hypoplasia than that caused by COL2A1.20 By contrast, Case 1, who carries a novel mutation in COL11A1, not only manifested very mild hearing loss and severe retinal detachment but also showed a nearly normal facial appearance. All of the clinical characteristics of Case 1 are compatible with the common phenotypes caused by COL2A1 but not COL11A1. The contradictory manifestations in our patients suggest a more complex genotype–phenotype association than previously reported. The highly overlapping phenotypes of STL1 and STL2 are reasonable because of the structural nature of the collagen molecules. COL2A1, COL11A1, and COL11A2 encode each of the three alpha chains. These alpha chains are finally assembled into one protein, type XI collagen characterized by triple helix.
Molecular genetic analysis is necessary for confirming the clinical diagnosis of patients with Marshall–Stickler syndrome spectrum due to the phenotypic variability. Candidate gene-based screening by Sanger sequencing is usually laborious and time-consuming, particularly when applied to the analysis of multiple large genes, such as COL11A1 and COL2A1, which have more than 50 exons. In this study, we used whole-exome sequencing to identify the causal mutations in different collagen genes. The method based on next-generation sequencing seems to be highly effective in the molecular diagnosis of Marshall–Stickler syndrome.
Additional infomation
Publisher's note:Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
References
Stickler GB, Belau PG, Farrell FJ, Jones JD, Pugh DG, Steinberg AG et al. Hereditary progressive arthro-ophthalmopathy. Mayo Clin Proc 1965; 40: 433–455.
Marshall D . Ectodermal dysplasia; report of kindred with ocular abnormalities and hearing defect. Am J Ophthalmol 1958; 45: 143–156.
Baraitser M . Marshall/Stickler syndrome. J Med Genet 1982; 19: 139–140.
Ahmad NN, Ala-Kokko L, Knowlton RG, Jimenez SA, Weaver EJ, Maguire JI et al. Stop codon in the procollagen II gene (COL2A1) in a family with the Stickler syndrome (arthro-ophthalmopathy). Proc Natl Acad Sci USA 1991; 88: 6624–6627.
Ahmad NN, McDonald-McGinn DM, Zackai EH, Knowlton RG, LaRossa D, DiMascio J et al. A second mutation in the type II procollagen gene (COL2AI) causing stickler syndrome (arthro-ophthalmopathy) is also a premature termination codon. Am J Hum Genet 1993; 52: 39–45.
Majava M, Hoornaert KP, Bartholdi D, Bouma MC, Bouman K, Carrera M et al. A report on 10 new patients with heterozygous mutations in the COL11A1 gene and a review of genotype-phenotype correlations in type XI collagenopathies. Am J Med Genet A 2007; 143A: 258–264.
Richards A, Yates JRW, Williams R, Payne SJ, Pope FM, Scott JD et al. A family with Stickler syndrome type 2 has a mutation in the COL11A1 gene resulting in the substitution of glycine 97 by valine in alpha 1 (XI) collagen. Hum Mol Genet 1996; 5: 1339–1343.
Vikkula M, Mariman EC, Lui VC, Zhidkova NI, Tiller GE, Goldring MB et al. Autosomal dominant and recessive osteochondrodysplasias associated with the COL11A2 locus. Cell 1995; 80: 431–437.
Brunner HG, van Beersum SE, Warman ML, Olsen BR, Ropers HH, Mariman EC . A Stickler syndrome gene is linked to chromosome 6 near the COL11A2 gene. Hum Mol Genet 1994; 3: 1561–1564.
Van Camp G, Snoeckx RL, Hilgert N, van den Ende J, Fukuoka H, Wagatsuma M et al. A new autosomal recessive form of Stickler syndrome is caused by a mutation in the COL9A1 gene. Am J Hum Genet 2006; 79: 449–457.
Nikopoulos K, Schrauwen I, Simon M, Collin RWJ, Veckeneer M, Keymolen K et al. Autosomal recessive Stickler syndrome in two families is caused by mutations in the COL9A1 gene. Invest Ophthalmol Vis Sci 2011; 52: 4774–4779.
Baker S, Booth C, Fillman C, Shapiro M, Blair MP, Hyland JC et al. A loss of function mutation in the COL9A2 gene causes autosomal recessive Stickler syndrome. Am J Med Genet A 2011; 155A: 1668–1672.
Griffith AJ, Sprunger LK, Sirko-Osadsa DA, Tiller GE, Meisler MH, Warman ML . Marshall syndrome associated with a splicing defect at the COL11A1 locus. Am J Hum Genet 1998; 62: 816–823.
Annunen S, Körkkö J, Czarny M, Warman ML, Brunner HG, Kääriäinen H et al. Splicing mutations of 54-bp exons in the COL11A1 gene cause Marshall syndrome, but other mutations cause overlapping Marshall/Stickler phenotypes. Am J Hum Genet 1999; 65: 974–983.
Guo L, Elcioglu NH, Iida A, Demirkol YK, Aras S, Matsumoto N et al. Novel and recurrent XYLT1 mutations in two Turkish families with Desbuquois dysplasia, type 2. J Hum Genet 2016; 62: 447–451.
Guo L, Girisha KM, Iida A, Hebbar M, Shukla A, Shah H et al. Identification of a novel LRRK1 mutation in a family with osteosclerotic metaphyseal dysplasia. J Hum Genet 2016; 62: 437–441.
Wang Z, Horemuzova E, Iida A, Guo L, Liu Y, Matsumoto N et al. Axial spondylometaphyseal dysplasia is also caused by NEK1 mutations. J Hum Genet 2017; 62: 503–506.
Guo L, Elcioglu NH, Mizumoto S, Wang Z, Noyan B, Albayrak HM et al. Identification of biallelic EXTL3 mutations in a novel type of spondylo-epi-metaphyseal dysplasia. J Hum Genet 2017; 62: 797–801.
Ballo R, Beighton PH, Ramesar RS . Stickler-like syndrome due to a dominant negative mutation in the COL2A1 gene. Am J Med Genet 1998; 80: 6–11.
Poulson AV, Hooymans JM, Richards AJ, Bearcroft P, Murthy R, Baguley DM et al. Clinical features of type 2 Stickler syndrome. J Med Genet 2004; 41: e107–e107.
Data Citations
Ikegawa, Shiro HGV Database http://dx.doi.org/10.6084/m9.figshare.hgv.1639 (2017)
Ikegawa, Shiro HGV Database http://dx.doi.org/10.6084/m9.figshare.hgv.1642 (2017)
Ikegawa, Shiro HGV Database http://dx.doi.org/10.6084/m9.figshare.hgv.1645 (2017)
Ikegawa, Shiro HGV Database http://dx.doi.org/10.6084/m9.figshare.hgv.1648 (2017)
Acknowledgements
We thank the patients and their families for their participation in the study. This study was supported in part by research grants from the Japan Agency for Medical Research and Development (AMED) (contract No. 14525125), the Japan Society for the Promotion of Science (WAKATE B, No. 17K16710) and RIKEN-MOST.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information for this article can be found on the Human Genome Variation website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Guo, L., Elcioglu, N., Wang, Z. et al. Novel and recurrent COL11A1 and COL2A1 mutations in the Marshall–Stickler syndrome spectrum. Hum Genome Var 4, 17040 (2017). https://doi.org/10.1038/hgv.2017.40
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/hgv.2017.40
This article is cited by
-
Dysosteosclerosis is also caused by TNFRSF11A mutation
Journal of Human Genetics (2018)