Abstract
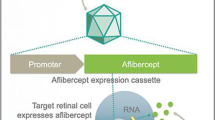
Gene therapy has shown great potential for the treatment of diseases that previously were either untreatable or treatable but not curable with conventional schemes. Recent progress in clinical gene therapy trials has emerged in various severe diseases, including primary immunodeficiencies, leukodystrophies, Leber’s congenital amaurosis, haemophilia, as well as retinal dystrophy. The clinical transformation and industrialization of gene therapy in Asia have been remarkable and continue making steady progress. A total of six gene therapy-based products have been approved worldwide, including two drugs from Asia. This review aims to highlight recent progress in gene therapy clinical trials and discuss the prospects for the future in China and wider Asia.
Similar content being viewed by others
Introduction
Gene therapy may be defined as a treatment in which genetic material is introduced into a cell, to enhance the effect of functional genes or modify malfunctioning genes. Gene therapy was originally conceived as a strategy to treat monogenic diseases, but it has expanded its application spectrum to many other conditions including cancer1, 2 and infectious diseases,3, 4 well beyond the primary immunodeficiencies.5, 6 Both ex vivo and in vivo strategies have been used in clinical trials (Figure 1). In 1990, the first gene therapy clinical trial, targeting adenosine deaminase deficiency-severe combined immune deficiency disorder (ADA-SCID), was approved by the US Federal Drug Administration. Unfortunately, in 1999, an 18-year-old man died from a severe immune response to the Ad5 vector used in a subsequent clinical trial.7 Fischer et al.10 reported the treatment of SCID-X1 with a Moloney murine leukaemia virus vector in 2003 and, although successful, 3 of 11 patients developed leukaemia.8, 9, 10 These setbacks caused concern and skepticism in gene therapy clinical trials but attitudes are changing gradually. The past two decades have witnessed rapid progress in this field and gene therapy is poised to become a promising approach through its potential to treat a disease at its genetic roots. It was encouraging that gene therapy was selected as one of the runners up to ‘Breakthrough of the year’in 2009 by Science magazine.11 Cancer immunotherapy for eradication of blood cancers using chimeric antigen receptor (CAR)-modified T cells finally achieved ‘Breakthrough of the year’ in 2013.12 These achievements not only depend on the development of gene therapy vector systems but also on the accumulation of clinical experience.
Many gene therapy technologies have been applied in clinical trials. Up to April 2017 (http://www.abedia.com/wiley/), 2463 gene therapy clinical trials had been completed, were ongoing or had been approved worldwide (Figure 2). The United States (64.4%) has conducted most of the trials, followed by Europe (23.7%) and Asia (6.1%). Most gene therapy trials target cancer (64.6%), followed by monogenetic diseases (10.5%), infectious diseases (7.4%) and cardiovascular diseases (7.2%). To date, six gene therapy-based products13, 14, 15, 16, 17, 18 have been approved around the world to target cancer, peripheral arterial disease, lipoprotein lipase deficiency, ADA-SCID, as well as spinal muscular atrophy (Table 1). It is worth mentioning that the approval of Spinraza, a 2′O-methoxyethyl phosphorothioate-modified antisense drug for treatment of patients with spinal muscular atrophy, by the US Federal Drug Administration was an important milestone in gene-based product development.18, 19
The status of gene therapy clinical trials worldwide up to April 2017. The statistical data were obtained from http://www.abedia.com/wiley/.
The United States has been at the forefront of the gene therapy research and accounts for 62.9% of the world with 1550 clinical trials. The United Kingdom and Germany undertook 8.9% and 3.7% of the total, respectively (Figure 3). China, similar to other countries, has also attached great important to gene therapy and approved the first gene therapy-based product for clinical use in 2003.13 Besides, Chinese scientists were the first to use cells modified using the clustered regularly interspaced short palindromic repeat (CRISPR)-Cas9 gene-editing technique in a clinical trial.20 These inspiring results suggest that China is becoming a leader in this field, particularly in the industrialization of gene therapy. This review aims to highlight recent progress in gene therapy clinical trials as well as the gene delivery vectors in China and wider Asia.
The proportion of gene therapy clinical trials in major countries worldwide up to April 2017. The statistical data were obtained from http://www.abedia.com/wiley/.
Number and phase of gene therapy clinical trial in Asia
Up to April 2017, 150 gene therapy clinical trials had been undertaken in Asia (Figure 4), which account for 6.1% of world trials (http://www.abedia.com/wiley/). China undertook the most (70 trials, 68 in mainland China and 2 in Taiwan), closely followed by Japan (42 trials) and South Korea (20 trials). More than two-thirds of gene therapy clinical trials performed in Asia are phase I or I/II. Phase II trials account for 20.6% of the total and phase II/III and III make up only 3.3% of all trials. Two phase IV clinical trials are ongoing at Sichuan University’s West China Hospital in Chengdu for the treatment of thyroid, and oral and maxillofacial malignant tumours, respectively. The two phase IV clinical trials are ‘Open-Label, Multi-Center, Randomized, Active-Controlled, Phase 4 Study of rAd-p53 Gene Mono-Therapy, With Concurrent Radioactive Iodine, or Combination With Surgery in Subjects With Advanced Malignant Thyroid Tumors’ and ‘Open-Label, Multi-Center, Randomized, Active-Controlled, Phase 4 Study of rAd-p53 Gene Mono-Therapy, With Concurrent Chemotherapy, or Combination With Surgery in Subjects With Advanced Oral and Maxillofacial Malignant Tumors.’
The proportion of gene therapy clinical trials in major countries from Asia up to April 2017. The statistical data were obtained from http://www.abedia.com/wiley/.
Vectors used for gene therapy in Asia
Vector performance has a critical role in gene therapy clinical trials. Effective strategies for clinical gene therapy are largely depending on the vectors, which are responsible for delivering functional genes to target cells or tissues (in vivo) or into autologous cells (ex vivo). In general, there are two approaches to deliver genes into a cell, that is, viral and non-viral. The most popular approach among the many vector systems used in Asia are adenovirus vectors (32%), followed by retrovirus (11.3%) and naked/plasmid DNA vectors (9.3%). Adeno-associated virus vectors make up only 4.7% of total vector systems, but they have demonstrated great clinical application value for in vivo gene delivery.21 It is worth noting that seven trials based on CRISPR-cas9 have been started in Asia from 2017, all of them conducted in China. Advances in vector manufacturing and characterization will improve the safety and efficiency of vector systems in clinical trials.
Diseases targeted by gene therapy in Asia
The majority of gene therapy clinical trials in Asia have addressed cancer (64.7%), cardiovascular diseases and inherited monogenic diseases (Figure 5). In addition, other gene therapy clinical trials have focused on infectious diseases, neurological diseases, as well as ocular diseases.
Diseases addressed by gene therapy clinical trials in Asia up to April 2017. The statistical data were obtained from http://www.abedia.com/wiley/
Cancer
Cancer gene therapy is one of the most active fields, with various cancers having been targeted to date, including haematological, lung, hepatocellular, nasopharyngeal, as well as head and neck cancers.22 The p53 gene is the most commonly mutated gene in human cancer and the most intensively studied tumour suppressor protein in cancer gene therapy.23 The world’s first gene therapy-based product (marketed as Gendicine) is a recombinant adenovirus vector encoding human p53 tumour suppressor gene (rAd-p53).13 It was approved by the State Food and Drug Administration of China in 2003 to treat head and neck squamous cell carcinoma and has been used for the treatment of solid tumours.24 Another gene therapy based product, Oncorine, which is the marketed name of H101 and aims at late-stage refractory nasopharyngeal cancer was approved by State Food and Drug Administration of China 2 years later,14 becoming the first oncolytic virus drug approved in the world. Initially, Oncorine was conceived as an oncolytic virus that would selectively replicate in p53-defective tumour cells. However, subsequent study demonstrated that loss of E1B-55K-mediated late viral RNA export, rather than p53, restricts Oncorine replication in primary cells.25, 26 H101, H102 and H103 make up the H100 series of recombinant oncolytic adenoviruses, and H102 and H103 are also ongoing clinical or preclinical trials in China.
Another gene commonly used in cancer gene therapy experiments is the herpesvirus thymidine kinase gene, which is often termed a suicide gene. Herpes simplex virus thymidine kinase has been used to convert the nontoxic pro-drug ganciclovir into the cytotoxic triphosphate ganciclovir.27, 28 Several clinical trials using adenovirus vectors (ADV-TK) have been completed or are ongoing in Asia. The results demonstrated that ADV-TK can be administered safely to cancer patients and showed therapeutic potential towards malignant tumours, including glioma, hepatocellular carcinoma and head and neck cancer.29, 30, 31
KH901 is a conditionally replicating oncolytic adenovirus, which reportedly selectively replicates in and lyses telomerase-positive tumour cells and expresses granulocyte macrophage colony-stimulating factor.32, 33 A phase I study investigated the therapeutic effect of KH901 in patients with recurrent head and neck cancer and showed that intratumoral administration of KH901 was feasible and well tolerated.34 OrienX010 is a recombinant human granulocyte macrophage colony-stimulating factor herpes simplex virus injection to treat solid tumours such as melanoma, liver cancer and lung cancer. A phase I trial evaluated the safety of the application of OrienX010 and follow-up clinical studies of this product are being planned.35
Endostatin is a broad-spectrum angiogenesis inhibitor and has been used for the treatment of tumours in gene therapy. EDS01 is a recombinant human endostatin adenovirus injection36 that has shown tumour suppressor effect in phase I clinical trials. This product is being tested in a phase II clinical trial at West China Hospital in Chengdu. Another antiangiogenic product is E10A (a recombinant human endostatin adenovirus), for which a phase II clinical trial has demonstrated safety and efficacy in patients with advanced head and neck squamous cell carcinoma or nasopharyngeal carcinoma.37 In addition, heat shock protein 70 (HSP70), Dickkopf-3 (Dkk-3/REIC) and NK4 genes have also been used in cancer gene therapy in Asia.
CARs represent a promising cancer immunotherapy, based on genetic modification of autologous T cells targeting tumour-specific surface antigens.38, 39 It is highly effective at eradicating B-cell leukaemias and lymphomas that are resistant to standard therapies. In contrast, due to the hostile immunosuppressive microenvironment, CAR-T cells show limited therapeutic efficacy in solid tumours. The main challenges of CAR-T therapy for solid tumours are (1) poor infiltration of T lymphocytes into solid tumours, (2) the identification of proper tumour-associated antigens and (3) immunosuppressive environment within solid tumour.40, 41 June and colleagues1 reported a successful clinical trial treating chronic lymphoid leukaemia with a lentiviral vector expressing a CAR with specificity for the B-cell antigen CD19, coupled with CD137 and CD3-zeta signalling domains. Han and collegues42 conducted a clinical trial to assess the efficacy of CD33-directed CAR modified T cells (CART-33) for the treatment of refractory acute myeloid leukaemia. Although the patient died 13 weeks after the CART-33 infusion, the trial provided beneficial experience for further research. Recently, in a phase I clinical trial, Han and collegues43 reported the treatment of relapsed or refractory Hodgkin lymphoma with autologous T Cells expressing CD30 CARs. Of 18 patients, 7 achieved partial remission and 6 achieved stable disease. These results guarantee a large-scale patient recruitment for further research.44 Besides, they investigated CART cocktail immunotherapy targeting epidermal growth factor receptor and CD133 in a patient with advanced cholangiocarcinoma. The results suggested that CART cocktail immunotherapy may be feasible for the treatment of cholangiocarcinoma as well as other solid malignancies.45 Recently, Qian and colleagues46 investigated a CAR-T therapy targeting carcino-embryonic antigen-positive colorectal cancer patients with metastases and they observed efficacy in most patients.
Advances in gene-editing technologies also help expand the spectrum of diseases that can be targeted by gene therapy. Particularly worth mentioning is the development and application of CRISPR-Cas9 in preclinical and clinical trials.47, 48 Testing the CRISPR-Cas9 gene-editing technique in patients with lung cancer has received ethical approval at West China Hospital. Thus, Chinese scientists have been the first to inject people with cells modified using CRISPR-Cas9.
Cardiovascular diseases
Cardiovascular diseases such as critical limb ischaemia, ischaemic heart disease and intermittent claudication, always have poor prognosis and adversely influence patients’ quality of life. A large proportion of cardiovascular gene therapy trials have been designed to increase blood flow to ischaemic regions. The fibroblast growth factor, vascular endothelial growth factor and hepatocyte growth factor (HGF) have been most widely applied in Asia. A Phase I/IIa open-label clinical trial reported the potential therapeutic efficacy of DVC1-0101 in critical limb ischaemia patients.49 DVC1-0101 is a non-transmissible recombinant Sendai virus vector expressing human fibroblast growth factor-2. DVC1-0101-based gene therapy was effective and could significantly improve limb function as well as patients’ quality of life over a 6-month period.50 In addition, studies in animal models and a phase I clinical trial have demonstrated the safety and effectiveness of adenovirus-HGF in inducing angiogenesis.51, 52, 53, 54 A phase II clinical trial has been conducted in China to investigate the safety and efficiency of adenovirus-HGF for the treatment of ischaemic heart disease. Several other gene therapy-based products tested in clinical trials such as NL003/VM202RY (a DNA plasmid that contains human HGF coding sequence) and VMDA-3601 (a DNA plasmid that contains human vascular endothelial growth factor coding sequence) also showed promising results.
Monogenic diseases
Following US Federal Drug Administration approval of the first gene therapy trial to treat ADA-SCID in 1990, genetically modified autologous T lymphocytes transduced with the human ADA cDNA were successfully transferred in Japan in 1997.55 The patient’s immune function improved after periodic infusions. Given the risk of development of T-cell leukaemia due to insertional mutagenesis caused by the retroviral vector, autologous CD34+ cells were used to increase safety in a phase I trial. Haemophilia is another monogenetic disease, caused by dysfunction of the coagulation proteins factor VIII (haemophilia A) or factor IX (haemophilia B). As early as 1996, Chinese scientists reported the treatment of haemophilia B with autologous skin fibroblasts transduced with a human clotting factor IX cDNA.56 Other gene therapy trials aimed at monogenetic diseases such as granular corneal dystrophy, retinitis pigmentosa, familial lecithin–cholesterol acyltransferase deficiency, as well as chronic granulomatous disease are ongoing in Asia.
Neurological diseases
Metachromatic leukodystrophy is an autosomal recessive disease caused by a deficiency in the enzyme arylsulfatase A, whereby the enzyme activity in leukocytes is less than 10% of normal cells.57 Adrenoleukodystrophy is a disease linked to the X chromosome caused by a deficiency in adrenoleukodystrophy protein.58 Targeting of the haematopoietic compartment has shown promising results in the treatment of metachromatic leukodystrophy and adrenoleukodystrophy. In China, a phase I/II clinical trial using haematopoietic stem cells (HSCs) genetically modified with a lentivirus vector has been approved for the treatment of metachromatic leukodystrophy and adrenoleukodystrophy.
Parkinson’s disease is a common neurodegenerative disorder that mainly affects the motor system. Aminoacid decarboxylase is an important enzyme in the biosynthesis of dopamine, which functions as a neurotransmitter.59, 60 Children with defects in the aminoacid decarboxylase gene show compromised development, particularly in motor function.61 Tyrosine hydroxylase and cyclohydrolase 1 are also important enzymes in the synthesis of dopamine. Increasing the expression of dopamine-synthesizing enzymes is a promising strategy in gene therapy. ProSavin is a lentiviral vector encoding the dopamine biosynthetic enzymes tyrosine hydroxylase, aminoacid decarboxylase and cyclohydrolase 1. A phase I/II clinical trial has reported the safety of ProSavin and improvement in motor behaviour was observed in patients.62 In Asia, Wu and colleagues63 have reported the treatment of four children 4 to 6 years of age with Adeno-associated virus vector encoding human aminoacid decarboxylase gene, and all of the patients showed increased dopamine level and improvements in motor behaviour.
Infectious diseases
Various gene therapy approaches are being used for the treatment of infectious diseases in Asia, including HIV and hepatitis B. A phase I clinical trial using a prime-boost vaccine strategy to induce both humoral and cell-mediated immunity in HIV-infected patients is ongoing at Beijng Ditan Hospital of Capital Medical University Beijing in China. This vaccine is based on naked/plasmid DNA combined with modified vaccinia virus Ankara and is expected to increase the level of HIV-specific immune responses. In South Korea, a phase I clinical trial investigated the safety and efficacy of GX-12, a genetic vaccine including naked DNA with HIV-1 antigen genes and human interleukin-12 mutant as immune adjuvant in HIV-infected patients with highly active antiretroviral therapy. However, to date, with the exception of the Berlin patient case, no gene therapy approach has fully cured HIV-infected patients.64
HB-110 is a therapeutic DNA vaccine against chronic hepatitis B, including the HBV envelope proteins, core protein, polymerase and human interleukin-12.65 Its safety and immunogenicity have been evaluated in a phase I clinical study in South Korea. HB-110 was safe and well tolerated in chronic hepatitis B patients, but it induced weaker HBV-specific T-cell responses in Korean patients than in Caucasian patients, which may due to the higher level of immune tolerance in Asian patients.66
Challenges and future prospects
China started conducting gene therapy clinical trials in 1987, making up ~46.7% of the total trials in Asia, followed closely by Japan. China approved the first two gene therapy-based products, Gendicine and Oncorine, for clinical use in 2003 and 2005. However, since then, gene therapy seemed to reach a plateau in China, as well as wider Asia. The limited clinical benefits caused concern and skepticism regarding the further development and application of these gene therapy strategies. However, these attitudes are rapidly changing with the emergence of novel genetic technologies, particularly advances in gene-editing and the CAR-T field. However, major challenges must still be addressed to revitalize and promote the development of gene therapy. Lentiviral and Adeno-associated virus vectors should be further optimized to enable cell-type-specific uptake. Advances in vector design could also help to mitigate the risk of insertional mutagenesis in clinical trials. In addition, all vector types likely induce an immune response67 and further advances could also help vectors to circumvent the innate and adaptive immune system.
Gene therapy trials often address rare diseases, but better understanding of disease pathogenesis and the accumulation of clinical experience will help to promote the emergence of novel gene therapy strategies for common diseases. In addition, larger number of patients and longer follow-up periods will be required to validate existing clinical data.
Gene-editing technologies have provided powerful impetus in the further development of gene therapy strategies.68 Zinc finger nucleases were used to disrupt the gene that encodes CCR5 for the treatment of HIV-infected patients.3 The CRISPR-Cas9 system has been tested in animal disease models such as Duchenne muscular dystrophy and haemophilia B.69, 70,71,72 Recently, testing CRISPR-Cas9 in patients with lung cancer has received ethical approval at Sichuan University’s West China Hospital. The recent report entitled ‘Human Genome Editing: Science, Ethics, and Governance’, has provided a first set of guidelines for the application of genome editing in humans.73 Clinical studies of genome editing-based gene therapy will be performed in near future, and ethical and safety issues must be strictly evaluated.
The regenerative potential of stem cells such as HSCs can be critical for improved gene therapy strategies.74 Gene-modified HSCs can function as a long-term source of their gene-corrected progeny in patients. HSC gene therapy can avoid the risk of morbidity due to mismatched human leukocyte antigen between donors and recipients, particularly when no matched HSC donor is available in severe immunodeficiencies such as SCID-X1,75 ADA-SCID76 and Wiskott–Aldrich syndrome.5, 77
Conclusions
Gene therapy research in Asia is on the increase, however, much importance should be attached to narrowing the gap with the United States and Europe. In China, gene therapy-based products are considered as new drugs and the application and management of these products is conducted by State Food and Drug Administration of China. The approval process of phase I gene therapy clinical trials is very strict in China and could be optimized. Gene therapy is widely expected to provide treatments for previously intractable diseases. Although not exempt of setbacks, effective and informative results are being increasingly reported from gene therapy trials. The clinical transformation and industrialization of gene therapy in Asia are considerable and will progress further towards gene-editing tools as well as HSC-based strategies, which will increase precision and efficiency in gene therapy approaches.
References
Porter DL, Levine BL, Kalos M, Bagg A, June CH . Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med 2011; 365: 725–733.
Husain SR, Han J, Au P, Shannon K, Puri RK . Gene therapy for cancer: regulatory considerations for approval. Cancer Gene Ther 2015; 22: 554–563.
Tebas P, Stein D, Tang WW, Frank I, Wang SQ, Lee G et al. Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. N Engl J Med 2014; 370: 901–910.
Mitsuyasu RT, Merigan TC, Carr A, Zack JA, Winters MA, Workman C et al. Phase 2 gene therapy trial of an anti-HIV ribozyme in autologous CD34+ cells. Nat Med 2009; 15: 285–292.
Aiuti A, Biasco L, Scaramuzza S, Ferrua F, Cicalese MP, Baricordi C et al. Lentiviral hematopoietic stem cell gene therapy in patients with Wiskott-Aldrich syndrome. Science (New York, NY) 2013; 341: 1233151.
Stein S, Ott MG, Schultze-Strasser S, Jauch A, Burwinkel B, Kinner A et al. Genomic instability and myelodysplasia with monosomy 7 consequent to EVI1 activation after gene therapy for chronic granulomatous disease. Nat Med 2010; 16: 198–204.
Raper SE, Chirmule N, Lee FS, Wivel NA, Bagg A, Gao GP et al. Fatal systemic inflammatory response syndrome in a ornithine transcarbamylase deficient patient following adenoviral gene transfer. Mol Genet Metab 2003; 80: 148–158.
Hacein-Bey-Abina S, Von Kalle C, Schmidt M, McCormack MP, Wulffraat N, Leboulch P et al. LMO2-associated clonal T cell proliferation in two patients after gene therapy for SCID-X1. Science (New York, NY) 2003; 302: 415–419.
McCormack MP, Rabbitts TH . Activation of the T-cell oncogene LMO2 after gene therapy for X-linked severe combined immunodeficiency. N Engl J Med 2004; 350: 913–922.
Fischer A, Abina SH, Thrasher A, von Kalle C, Cavazzana-Calvo M . LMO2 and gene therapy for severe combined immunodeficiency. N Engl J Med 2004; 350: 2526–2527; author reply 2526-7.
Naldini L . Medicine. A comeback for gene therapy. Science (New York, NY) 2009; 326: 805–806.
Couzin-Frankel J . Breakthrough of the year 2013. Cancer immunotherapy. Science (New York, NY) 2013; 342: 1432–1433.
Peng Z . Current status of gendicine in China: recombinant human Ad-p53 agent for treatment of cancers. Hum Gene Ther 2005; 16: 1016–1027.
Liang M . Clinical development of oncolytic viruses in China. Curr Pharm Biotechnol 2012; 13: 1852–1857.
Yla-Herttuala S . Endgame: glybera finally recommended for approval as the first gene therapy drug in the European union. Mol Ther 2012; 20: 1831–1832.
Chervyakov YV, Staroverov IN, Vlasenko ON, Bozo IY, Isaev AA, Deev RV . [Five-year results of treating patients with chronic lower limb ischaemia by means of gene engineering]. Angiol Vasc Surg 2016; 22: 38–44.
Schimmer J, Breazzano S . Investor outlook: rising from the ashes; GSK's European approval of strimvelis for ADA-SCID. Hum Gene Ther Clin Dev 2016; 27: 57–61.
Adams L . Motor neuron disease: Nusinersen potentially effective in SMA. Nat Rev Neurol 2017; 13: 66.
Finkel RS, Chiriboga CA, Vajsar J, Day JW, Montes J, De Vivo DC et al. Treatment of infantile-onset spinal muscular atrophy with nusinersen: a phase 2, open-label, dose-escalation study. Lancet (Lond, Engl) 2016; 388: 3017–3026.
Cyranoski D . Chinese scientists to pioneer first human CRISPR trial. Nature 2016; 535: 476–477.
Kumar SR, Markusic DM, Biswas M, High KA, Herzog RW . Clinical development of gene therapy: results and lessons from recent successes. Mol Ther Methods Clin Dev 2016; 3: 16034.
Saadatpour Z, Bjorklund G, Chirumbolo S, Alimohammadi M, Ehsani H, Ebrahiminejad H et al. Molecular imaging and cancer gene therapy. Cancer Gene Ther; epub ahead of print 18 November 2016; doi:10.1038/cgt.2016.62.
Muller PA, Vousden KH . Mutant p53 in cancer: new functions and therapeutic opportunities. Cancer Cell 2014; 25: 304–317.
Li Y, Li B, Li CJ, Li LJ . Key points of basic theories and clinical practice in rAd-p53 (Gendicine) gene therapy for solid malignant tumors. Expert Opin Biol Ther 2015; 15: 437–454.
O'Shea CC, Soria C, Bagus B, McCormick F . Heat shock phenocopies E1B-55 K late functions and selectively sensitizes refractory tumor cells to ONYX-015 oncolytic viral therapy. Cancer Cell 2005; 8: 61–74.
O'Shea CC, Johnson L, Bagus B, Choi S, Nicholas C, Shen A et al. Late viral RNA export, rather than p53 inactivation, determines ONYX-015 tumor selectivity. Cancer Cell 2004; 6: 611–623.
Rojas-Martinez A, Manzanera AG, Sukin SW, Esteban-Maria J, Gonzalez-Guerrero JF, Gomez-Guerra L et al. Intraprostatic distribution and long-term follow-up after AdV-tk immunotherapy as neoadjuvant to surgery in patients with prostate cancer. Cancer Gene Ther 2013; 20: 642–649.
Karjoo Z, Chen X, Hatefi A . Progress and problems with the use of suicide genes for targeted cancer therapy. Adv Drug Deliv Rev 2016; 99 (Pt A): 113–128.
Li N, Zhou J, Weng D, Zhang C, Li L, Wang B et al. Adjuvant adenovirus-mediated delivery of herpes simplex virus thymidine kinase administration improves outcome of liver transplantation in patients with advanced hepatocellular carcinoma. Clin Cancer Res 2007; 13: 5847–5854.
Xu F, Li S, Li XL, Guo Y, Zou BY, Xu R et al. Phase I and biodistribution study of recombinant adenovirus vector-mediated herpes simplex virus thymidine kinase gene and ganciclovir administration in patients with head and neck cancer and other malignant tumors. Cancer Gene Ther 2009; 16: 723–730.
Ji N, Weng D, Liu C, Gu Z, Chen S, Guo Y et al. Adenovirus-mediated delivery of herpes simplex virus thymidine kinase administration improves outcome of recurrent high-grade glioma. Oncotarget 2016; 7: 4369–4378.
Mi Y, Li Y, Long Y . [Antitumor effects of radioiodine labeled KH901 on nude mice bearing hepatoma]. J Biomed Eng 2010; 27: 389–394.
Mi YX, Li YC, Long YH . Imaging of radioiodine-labeled KH901, a tumor-specific oncolytic recombinant adenovirus, in nude mice with human hepatocellular carcinoma. Nucl Med Commun 2010; 31: 405–410.
Chang J, Zhao X, Wu X, Guo Y, Guo H, Cao J et al. A phase I study of KH901, a conditionally replicating granulocyte-macrophage colony-stimulating factor: armed oncolytic adenovirus for the treatment of head and neck cancers. Cancer Biol Ther 2009; 8: 676–682.
Gao YD, Chen GL, Guo PD, Yang XL . [Study on the application effect of Once Vex(GM)(-)(CSF) and adriamycin in the interventional therapy of malignant tumor in clinical curative effect]. Zhonghua Yi Xue Za Zhi 2016; 96: 2173–2175.
Wang L, Yao B, Li Q, Mei K, Xu JR, Li HX et al. Gene therapy with recombinant adenovirus encoding endostatin encapsulated in cationic liposome in coxsackievirus and adenovirus receptor-deficient colon carcinoma murine models. Hum Gene Ther 2011; 22: 1061–1069.
Ye W, Liu R, Pan C, Jiang W, Zhang L, Guan Z et al. Multicenter randomized phase 2 clinical trial of a recombinant human endostatin adenovirus in patients with advanced head and neck carcinoma. Mol Ther 2014; 22: 1221–1229.
June CH, Riddell SR, Schumacher TN . Adoptive cellular therapy: a race to the finish line. Sci Transl Med 2015; 7: 280ps7.
Brown CE, Alizadeh D, Starr R, Weng L, Wagner JR, Naranjo A et al. Regression of glioblastoma after chimeric antigen receptor T-cell therapy. N Engl J Med 2016; 375: 2561–2569.
Zhang H, Ye ZL, Yuan ZG, Luo ZQ, Jin HJ, Qian QJ . New strategies for the treatment of solid tumors with CAR-T cells. Int J Biol Sci 2016; 12: 718–729.
Beatty GL, O'Hara M . Chimeric antigen receptor-modified T cells for the treatment of solid tumors: defining the challenges and next steps. Pharmacol Ther 2016; 166: 30–39.
Wang QS, Wang Y, Lv HY, Han QW, Fan H, Guo B et al. Treatment of CD33-directed chimeric antigen receptor-modified T cells in one patient with relapsed and refractory acute myeloid leukemia. Mol Ther 2015; 23: 184–191.
Dai H, Zhang W, Li X, Han Q, Guo Y, Zhang Y et al. Tolerance and efficacy of autologous or donor-derived T cells expressing CD19 chimeric antigen receptors in adult B-ALL with extramedullary leukemia. Oncoimmunology 2015; 4: e1027469.
Wang Y, Zhang WY, Han QW, Liu Y, Dai HR, Guo YL et al. Effective response and delayed toxicities of refractory advanced diffuse large B-cell lymphoma treated by CD20-directed chimeric antigen receptor-modified T cells. Clin Immunol 2014; 155: 160–175.
Feng KC, Guo YL, Liu Y, Dai HR, Wang Y, Lv HY et al. Cocktail treatment with EGFR-specific and CD133-specific chimeric antigen receptor-modified T cells in a patient with advanced cholangiocarcinoma. J Hematol Oncol 2017; 10: 4.
Zhang C, Wang Z, Yang Z, Wang M, Li S, Li Y et al. Phase I escalating-dose trial of CAR-T therapy targeting CEA+ metastatic colorectal cancers. Mol Ther 2017; 25: 1248–1258.
Swiech L, Heidenreich M, Banerjee A, Habib N, Li Y, Trombetta J et al. In vivo interrogation of gene function in the mammalian brain using CRISPR-Cas9. Nat Biotechnol 2015; 33: 102–106.
Yin H, Xue W, Chen S, Bogorad RL, Benedetti E, Grompe M et al. Genome editing with Cas9 in adult mice corrects a disease mutation and phenotype. Nat Biotechnol 2014; 32: 551–553.
Yonemitsu Y, Matsumoto T, Itoh H, Okazaki J, Uchiyama M, Yoshida K et al. DVC1-0101 to treat peripheral arterial disease: a Phase I/IIa open-label dose-escalation clinical trial. Mol Ther 2013; 21: 707–714.
Matsumoto T, Tanaka M, Yoshiya K, Yoshiga R, Matsubara Y, Horiuchi-Yoshida K et al. Improved quality of life in patients with no-option critical limb ischemia undergoing gene therapy with DVC1-0101. Sci Rep 2016; 6: 30035.
Liu J, Wu P, Wang H, Wang Y, Du Y, Cheng W et al. Necroptosis induced by Ad-HGF activates endogenous C-Kit+ cardiac stem cells and promotes cardiomyocyte proliferation and angiogenesis in the infarcted aged heart. Cell Physiol Biochem 2016; 40: 847–860.
Yang ZJ, Zhang YR, Chen B, Zhang SL, Jia EZ, Wang LS et al. Phase I clinical trial on intracoronary administration of Ad-hHGF treating severe coronary artery disease. Mol Biol Rep 2009; 36: 1323–1329.
Liu J, Wu P, Wang Y, Du Y, N A, Liu S et al. Ad-HGF improves the cardiac remodeling of rat following myocardial infarction by upregulating autophagy and necroptosis and inhibiting apoptosis. Am J Transl Res 2016; 8: 4605–4627.
Yang ZJ, Chen B, Sheng Z, Zhang DG, Jia EZ, Wang W et al. Improvement of heart function in postinfarct heart failure swine models after hepatocyte growth factor gene transfer: comparison of low-, medium- and high-dose groups. Mol Biol Rep 2010; 37: 2075–2081.
Onodera M, Ariga T, Kawamura N, Kobayashi I, Ohtsu M, Yamada M et al. Successful peripheral T-lymphocyte-directed gene transfer for a patient with severe combined immune deficiency caused by adenosine deaminase deficiency. Blood 1998; 91: 30–36.
Qiu X, Lu D, Zhou J, Wang J, Yang J, Meng P et al. Implantation of autologous skin fibroblast genetically modified to secrete clotting factor IX partially corrects the hemorrhagic tendencies in two hemophilia B patients. Chinese Med J 1996; 109: 832–839.
Sessa M, Lorioli L, Fumagalli F, Acquati S, Redaelli D, Baldoli C et al. Lentiviral haemopoietic stem-cell gene therapy in early-onset metachromatic leukodystrophy: an ad-hoc analysis of a non-randomised, open-label, phase 1/2 trial. Lancet (Lond, Engl) 2016; 388: 476–487.
Cartier N, Hacein-Bey-Abina S, Bartholomae CC, Veres G, Schmidt M, Kutschera I et al. Hematopoietic stem cell gene therapy with a lentiviral vector in X-linked adrenoleukodystrophy. Science (New York, NY) 2009; 326: 818–823.
Mittermeyer G, Christine CW, Rosenbluth KH, Baker SL, Starr P, Larson P et al. Long-term evaluation of a phase 1 study of AADC gene therapy for Parkinson's disease. Hum Gene Ther 2012; 23: 377–381.
Valdes P, Schneider BL . Gene therapy: a promising approach for neuroprotection in Parkinson's disease? Front Neuroanat 2016; 10: 123.
Kalia LV, Lang AE . Parkinson's disease. Lancet (Lond, Engl) 2015; 386: 896–912.
Palfi S, Gurruchaga JM, Ralph GS, Lepetit H, Lavisse S, Buttery PC et al. Long-term safety and tolerability of ProSavin, a lentiviral vector-based gene therapy for Parkinson's disease: a dose escalation, open-label, phase 1/2 trial. Lancet (Lond, Engl) 2014; 383: 1138–1146.
Hwu WL, Muramatsu S, Tseng SH, Tzen KY, Lee NC, Chien YH et al. Gene therapy for aromatic L-amino acid decarboxylase deficiency. Sci Transl Med 2012; 4: 134ra61.
Johnston R . Gene therapy to cure HIV: where to from here? AIDS Patient Care STDs 2016; 30: 531–533.
Kim CY, Kang ES, Kim SB, Kim HE, Choi JH, Lee DS et al. Increased in vivo immunological potency of HB-110, a novel therapeutic HBV DNA vaccine, by electroporation. Exp Mol Med 2008; 40: 669–676.
Yoon SK, Seo YB, Im SJ, Bae SH, Song MJ, You CR et al. Safety and immunogenicity of therapeutic DNA vaccine with antiviral drug in chronic HBV patients and its immunogenicity in mice. Liver Int 2015; 35: 805–815.
Razi Soofiyani S, Baradaran B, Lotfipour F, Kazemi T, Mohammadnejad L . Gene therapy, early promises, subsequent problems, and recent breakthroughs. Adv Pharm Bull 2013; 3: 249–255.
Naldini L . Gene therapy returns to centre stage. Nature 2015; 526: 351–360.
Tabebordbar M, Zhu K, Cheng JK, Chew WL, Widrick JJ, Yan WX et al. In vivo gene editing in dystrophic mouse muscle and muscle stem cells. Science (New York, NY) 2016; 351: 407–411.
Long C, Amoasii L, Mireault AA, McAnally JR, Li H, Sanchez-Ortiz E et al. Postnatal genome editing partially restores dystrophin expression in a mouse model of muscular dystrophy. Science (New York, NY) 2016; 351: 400–403.
Nelson CE, Hakim CH, Ousterout DG, Thakore PI, Moreb EA, Castellanos Rivera RM et al. In vivo genome editing improves muscle function in a mouse model of Duchenne muscular dystrophy. Science (New York, NY) 2016; 351: 403–407.
Guan Y, Ma Y, Li Q, Sun Z, Ma L, Wu L et al. CRISPR/Cas9-mediated somatic correction of a novel coagulator factor IX gene mutation ameliorates hemophilia in mouse. EMBO Mol Med 2016; 8: 477–488.
Sciences NAo Medicine NAo National Academies of Sciences E, Medicine Human Genome Editing: Science, Ethics, and Governance. The National Academies Press: Washington, DC, 2017.
Williams DA . Broadening the indications for hematopoietic stem cell genetic therapies. Cell Stem Cell 2013; 13: 263–264.
Hacein-Bey-Abina S, Pai SY, Gaspar HB, Armant M, Berry CC, Blanche S et al. A modified gamma-retrovirus vector for X-linked severe combined immunodeficiency. N Engl J Med 2014; 371: 1407–1417.
Cicalese MP, Aiuti A . Clinical applications of gene therapy for primary immunodeficiencies. Hum Gene Ther 2015; 26: 210–219.
Boztug K, Schmidt M, Schwarzer A, Banerjee PP, Diez IA, Dewey RA et al. Stem-cell gene therapy for the Wiskott-Aldrich syndrome. N Engl J Med 2010; 363: 1918–1927.
Acknowledgements
We acknowledge National Natural Science Foundation of China for funding through project number 81472195.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Deng, HX., Wang, Y., Ding, Qr. et al. Gene therapy research in Asia. Gene Ther 24, 572–577 (2017). https://doi.org/10.1038/gt.2017.62
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2017.62