Abstract
Huntington's disease (HD) is caused by an expansion of CAG triplets at the 5′ end of the HD gene, which encodes a pathologically elongated polyglutamine stretch near the N-terminus of huntingtin. HD is an incurable autosomal-dominant neurodegenerative disease characterized by movement disorder, as well as emotional distress and dementia. The newly discovered roles of the non-coding small RNAs in specific degradation or translational suppression of the targeted mRNAs suggest a potential therapeutic approach of post-transcriptional gene silencing that targets the underlying disease etiology rather than the downstream pathological consequences. From pre-clinical trials in different HD animal models to cells from HD patients, small RNA interference has been applied to ‘allele-non-specifically or allele-specifically’ silence the mutant HD transgene or endogenous mutant HD allele. Silencing the mutant HD transgene significantly inhibits neurodegeneration, improves motor control, and extends survival of HD mice. With future improvement of mutant allele selectivity (preserving the expression of the neuroprotective wild-type allele), target specificity, efficacy and safety, as well as optimization of delivery methods, small non-coding RNA-based therapeutic applications will be a promising approach to treat HD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
The Huntington's Disease Collaborative Research Group. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington's disease chromosomes. Cell 1993; 72: 971–983.
Harper SQ . Progress and challenges in RNA interference therapy for Huntington disease. Arch Neurol 2009; 66: 933–938.
Denovan-Wright EM, Davidson BL . RNAi: a potential therapy for the dominantly inherited nucleotide repeat diseases. Gene Therapy 2006; 13: 525–531.
Boudreau RL, Davidson BL . RNAi therapy for neurodegenerative diseases. Curr Top Dev Biol 2006; 75: 73–92.
Wang YL, Liu W, Wada E, Murata M, Wada K, Kanazawa I . Clinico-pathological rescue of a model mouse of Huntington's disease by siRNA. Neurosci Res 2005; 53: 241–249.
Franich NR, Fitzsimons HL, Fong DM, Klugmann M, During MJ, Young D . AAV vector-mediated RNAi of mutant huntingtin expression is neuroprotective in a novel genetic rat model of Huntington's disease. Mol Ther 2008; 16: 947–956.
McBride JL, Boudreau RL, Harper SQ, Staber PD, Monteys AM, Martins I et al. Artificial miRNAs mitigate shRNA-mediated toxicity in the brain: implications for the therapeutic development of RNAi. Proc Natl Acad Sci USA 2008; 105: 5868–5873.
Boudreau RL, McBride JL, Martins I, Shen S, Xing Y, Carter BJ et al. Nonallele-specific silencing of mutant and wild-type huntingtin demonstrates therapeutic efficacy in Huntington's disease mice. Mol Ther 2009; 17: 1053–1063.
DiFiglia M, Sena-Esteves M, Chase K, Sapp E, Pfister E, Sass M et al. Therapeutic silencing of mutant huntingtin with siRNA attenuates striatal and cortical neuropathology and behavioral deficits. Proc Natl Acad Sci USA 2007; 104: 17204–17209.
Rodriguez-Lebron E, Denovan-Wright EM, Nash K, Lewin AS, Mandel RJ . Intrastriatal rAAV-mediated delivery of anti-huntingtin shRNAs induces partial reversal of disease progression in R6/1 Huntington's disease transgenic mice. Mol Ther 2005; 12: 618–633.
Denovan-Wright EM, Rodriguez-Lebron E, Lewin AS, Mandel RJ . Unexpected off-targeting effects of anti-huntingtin ribozymes and siRNA in vivo. Neurobiol Dis 2008; 29: 446–455.
Machida Y, Okada T, Kurosawa M, Oyama F, Ozawa K, Nukina N . rAAV-mediated shRNA ameliorated neuropathology in Huntington disease model mouse. Biochem Biophys Res Commun 2006; 343: 190–197.
Drouet V, Perrin V, Hassig R, Dufour N, Auregan G, Alves S et al. Sustained effects of nonallele-specific Huntingtin silencing. Ann Neurol 2009; 65: 276–285.
Huang B, Schiefer J, Sass C, Landwehrmeyer GB, Kosinski CM, Kochanek S . High-capacity adenoviral vector-mediated reduction of huntingtin aggregate load in vitro and in vivo. Hum Gene Ther 2007; 18: 303–311.
Zhang Y, Friedlander RM . Silencing Huntington's disease (HD) gene with RNAi. In: Erdmann VA and Barciszewski J (eds). RNA Technologies and Their Applications. Springer: Berlin, 2010, pp 131–160.
van Bilsen PH, Jaspers L, Lombardi MS, Odekerken JC, Burright EN, Kaemmerer WF . Identification and allele-specific silencing of the mutant huntingtin allele in Huntington's disease patient-derived fibroblasts. Hum Gene Ther 2008; 19: 710–719.
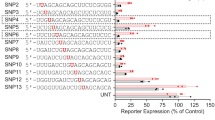
Zhang Y, Engelman J, Friedlander RM . Allele-specific silencing of mutant Huntington's disease gene. J Neurochem 2009; 108: 82–90.
Hu J, Matsui M, Corey DR . Allele-selective inhibition of mutant huntingtin by peptide nucleic acid-peptide conjugates, locked nucleic acid, and small interfering RNA. Ann NY Acad Sci 2009; 1175: 24–31.
Liu W, Kennington LA, Rosas HD, Hersch S, Cha JH, Zamore PD et al. Linking SNPs to CAG repeat length in Huntington's disease patients. Nat Methods 2008; 5: 951–953.
Palfi S, Brouillet E, Jarraya B, Bloch J, Jan C, Shin M et al. Expression of mutated huntingtin fragment in the putamen is sufficient to produce abnormal movement in non-human primates. Mol Ther 2007; 15: 1444–1451.
Lombardi MS, Jaspers L, Spronkmans C, Gellera C, Taroni F, Di Maria E et al. A majority of Huntington's disease patients may be treatable by individualized allele-specific RNA interference. Exp Neurol 2009; 217: 312–319.
de Mezer M, Wojciechowska M, Napierala M, Sobczak K, Krzyzosiak WJ . Mutant CAG repeats of huntingtin transcript fold into hairpins, form nuclear foci and are targets for RNA interference. Nucleic Acids Res 2011; 39: 3852–3863.
Hu J, Matsui M, Gagnon KT, Schwartz JC, Gabillet S, Arar K et al. Allele-specific silencing of mutant huntingtin and ataxin-3 genes by targeting expanded CAG repeats in mRNAs. Nat Biotechnol 2009; 27: 478–484.
Gagnon KT, Pendergraff HM, Deleavey GF, Swayze EE, Potier P, Randolph J et al. Allele-selective inhibition of mutant huntingtin expression with antisense oligonucleotides targeting the expanded CAG repeat. Biochemistry 2010; 49: 10166–10178.
Hu J, Liu J, Corey DR . Allele-selective inhibition of huntingtin expression by switching to an miRNA-like RNAi mechanism. Chem Biol 2010; 17: 1183–1188.
Fiszer A, Mykowska A, Krzyzosiak WJ . Inhibition of mutant huntingtin expression by RNA duplex targeting expanded CAG repeats. Nucleic Acids Res 2011; 39: 5578–5585.
Harper SQ, Staber PD, He X, Eliason SL, Martins IH, Mao Q et al. RNA interference improves motor and neuropathological abnormalities in a Huntington's disease mouse model. Proc Natl Acad Sci USA 2005; 102: 5820–5825.
Schilling G, Becher MW, Sharp AH, Jinnah HA, Duan K, Kotzuk JA et al. Intranuclear inclusions and neuritic aggregates in transgenic mice expressing a mutant N-terminal fragment of huntingtin. Hum Mol Genet 1999; 8: 397–407.
Mangiarini L, Sathasivam K, Seller M, Cozens B, Harper A, Hetherington C et al. Exon 1 of the HD gene with an expanded CAG repeat is sufficient to cause a progressive neurological phenotype in transgenic mice. Cell 1996; 87: 493–506.
Kotliarova S, Jana NR, Sakamoto N, Kurosawa M, Miyazaki H, Nekooki M et al. Decreased expression of hypothalamic neuropeptides in Huntington disease transgenic mice with expanded polyglutamine-EGFP fluorescent aggregates. J Neurochem 2005; 93: 641–653.
Senut MC, Suhr ST, Kaspar B, Gage FH . Intraneuronal aggregate formation and cell death after viral expression of expanded polyglutamine tracts in the adult rat brain. J Neurosci 2000; 20: 219–229.
de Almeida LP, Ross CA, Zala D, Aebischer P, Deglon N . Lentiviral-mediated delivery of mutant huntingtin in the striatum of rats induces a selective neuropathology modulated by polyglutamine repeat size, huntingtin expression levels, and protein length. J Neurosci 2002; 22: 3473–3483.
Slow EJ, van Raamsdonk J, Rogers D, Coleman SH, Graham RK, Deng Y et al. Selective striatal neuronal loss in a YAC128 mouse model of Huntington disease. Hum Mol Genet 2003; 12: 1555–1567.
Gray M, Shirasaki DI, Cepeda C, Andre VM, Wilburn B, Lu XH et al. Full-length human mutant huntingtin with a stable polyglutamine repeat can elicit progressive and selective neuropathogenesis in BACHD mice. J Neurosci 2008; 28: 6182–6195.
Spampanato J, Gu X, Yang XW, Mody I . Progressive synaptic pathology of motor cortical neurons in a BAC transgenic mouse model of Huntington's disease. Neuroscience 2008; 157: 606–620.
Hodgson JG, Agopyan N, Gutekunst CA, Leavitt BR, LePiane F, Singaraja R et al. A YAC mouse model for Huntington's disease with full-length mutant huntingtin, cytoplasmic toxicity, and selective striatal neurodegeneration. Neuron 1999; 23: 181–192.
Schwarz DS, Ding H, Kennington L, Moore JT, Schelter J, Burchard J et al. Designing siRNA that distinguish between genes that differ by a single nucleotide. PLoS Genet 2006; 2: e140.
Warby SC, Montpetit A, Hayden AR, Carroll JB, Butland SL, Visscher H et al. CAG expansion in the Huntington disease gene is associated with a specific and targetable predisposing haplogroup. Am J Hum Genet 2009; 84: 351–366.
Ambrose CM, Duyao MP, Barnes G, Bates GP, Lin CS, Srinidhi J et al. Structure and expression of the Huntington's disease gene: evidence against simple inactivation due to an expanded CAG repeat. Somat Cell Mol Genet 1994; 20: 27–38.
Almqvist E, Spence N, Nichol K, Andrew SE, Vesa J, Peltonen L et al. Ancestral differences in the distribution of the delta 2642 glutamic acid polymorphism is associated with varying CAG repeat lengths on normal chromosomes: insights into the genetic evolution of Huntington disease. Hum Mol Genet 1995; 4: 207–214.
Rubinsztein DC, Leggo J, Goodburn S, Barton DE, Ferguson-Smith MA . Haplotype analysis of the delta 2642 and (CAG)n polymorphisms in the Huntington's disease (HD) gene provides an explanation for an apparent ‘founder’ HD haplotype. Hum Mol Genet 1995; 4: 203–206.
Novelletto A, Persichetti F, Sabbadini G, Mandich P, Bellone E, Ajmar F et al. Polymorphism analysis of the huntingtin gene in Italian families affected with Huntington disease. Hum Mol Genet 1994; 3: 1129–1132.
Vuillaume I, Vermersch P, Destee A, Petit H, Sablonniere B . Genetic polymorphisms adjacent to the CAG repeat influence clinical features at onset in Huntington's disease. J Neurol Neurosurg Psychiatry 1998; 64: 758–762.
Sobczak K, de Mezer M, Michlewski G, Krol J, Krzyzosiak WJ . RNA structure of trinucleotide repeats associated with human neurological diseases. Nucleic Acids Res 2003; 31: 5469–5482.
Gacy AM, Goellner G, Juranic N, Macura S, McMurray CT . Trinucleotide repeats that expand in human disease form hairpin structures in vitro. Cell 1995; 81: 533–540.
Broda M, Kierzek E, Gdaniec Z, Kulinski T, Kierzek R . Thermodynamic stability of RNA structures formed by CNG trinucleotide repeats. Implication for prediction of RNA structure. Biochemistry 2005; 44: 10873–10882.
Sobczak K, Michlewski G, de Mezer M, Kierzek E, Krol J, Olejniczak M et al. Structural diversity of triplet repeat RNAs. J Biol Chem 2010; 285: 12755–12764.
Michlewski G, Krzyzosiak WJ . Molecular architecture of CAG repeats in human disease related transcripts. J Mol Biol 2004; 340: 665–679.
Krol J, Fiszer A, Mykowska A, Sobczak K, de Mezer M, Krzyzosiak WJ . Ribonuclease dicer cleaves triplet repeat hairpins into shorter repeats that silence specific targets. Mol Cell 2007; 25: 575–586.
Napierala M, Krzyzosiak WJ . CUG repeats present in myotonin kinase RNA form metastable "slippery" hairpins. J Biol Chem 1997; 272: 31079–31085.
Braasch DA, Liu Y, Corey DR . Antisense inhibition of gene expression in cells by oligonucleotides incorporating locked nucleic acids: effect of mRNA target sequence and chimera design. Nucleic Acids Res 2002; 30: 5160–5167.
Dias N, Dheur S, Nielsen PE, Gryaznov S, Van Aerschot A, Herdewijn P et al. Antisense PNA tridecamers targeted to the coding region of Ha-ras mRNA arrest polypeptide chain elongation. J Mol Biol 1999; 294: 403–416.
Jackson AL, Bartz SR, Schelter J, Kobayashi SV, Burchard J, Mao M et al. Expression profiling reveals off-target gene regulation by RNAi. Nat Biotechnol 2003; 21: 635–637.
Qiu S, Adema CM, Lane T . A computational study of off-target effects of RNA interference. Nucleic Acids Res 2005; 33: 1834–1847.
Lin X, Ruan X, Anderson MG, McDowell JA, Kroeger PE, Fesik SW et al. siRNA-mediated off-target gene silencing triggered by a 7 nt complementation. Nucleic Acids Res 2005; 33: 4527–4535.
Jackson AL, Burchard J, Schelter J, Chau BN, Cleary M, Lim L et al. Widespread siRNA “off-target” transcript silencing mediated by seed region sequence complementarity. RNA 2006; 12: 1179–1187.
Birmingham A, Anderson EM, Reynolds A, Ilsley-Tyree D, Leake D, Fedorov Y et al. 3′ UTR seed matches, but not overall identity, are associated with RNAi off-targets. Nat Methods 2006; 3: 199–204.
Doench JG, Sharp PA . Specificity of microRNA target selection in translational repression. Genes Dev 2004; 18: 504–511.
Haley B, Zamore PD . Kinetic analysis of the RNAi enzyme complex. Nat Struct Mol Biol 2004; 11: 599–606.
Schwarz DS, Hutvagner G, Du T, Xu Z, Aronin N, Zamore PD . Asymmetry in the assembly of the RNAi enzyme complex. Cell 2003; 115: 199–208.
Khvorova A, Reynolds A, Jayasena SD . Functional siRNAs and miRNAs exhibit strand bias. Cell 2003; 115: 209–216.
Reynolds A, Leake D, Boese Q, Scaringe S, Marshall WS, Khvorova A . Rational siRNA design for RNA interference. Nat Biotechnol 2004; 22: 326–330.
Grimson A, Farh KK, Johnston WK, Garrett-Engele P, Lim LP, Bartel DP . MicroRNA targeting specificity in mammals: determinants beyond seed pairing. Mol Cell 2007; 27: 91–105.
Burger C, Gorbatyuk OS, Velardo MJ, Peden CS, Williams P, Zolotukhin S et al. Recombinant AAV viral vectors pseudotyped with viral capsids from serotypes 1, 2, and 5 display differential efficiency and cell tropism after delivery to different regions of the central nervous system. Mol Ther 2004; 10: 302–317.
Paterna JC, Feldon J, Bueler H . Transduction profiles of recombinant adeno-associated virus vectors derived from serotypes 2 and 5 in the nigrostriatal system of rats. J Virol 2004; 78: 6808–6817.
Taymans JM, Vandenberghe LH, Haute CV, Thiry I, Deroose CM, Mortelmans L et al. Comparative analysis of adeno-associated viral vector serotypes 1, 2, 5, 7, and 8 in mouse brain. Hum Gene Ther 2007; 18: 195–206.
Davidson BL, Stein CS, Heth JA, Martins I, Kotin RM, Derksen TA et al. Recombinant adeno-associated virus type 2, 4, and 5 vectors: transduction of variant cell types and regions in the mammalian central nervous system. Proc Natl Acad Sci USA 2000; 97: 3428–3432.
Grimm D, Streetz KL, Jopling CL, Storm TA, Pandey K, Davis CR et al. Fatality in mice due to oversaturation of cellular microRNA/short hairpin RNA pathways. Nature 2006; 441: 537–541.
Bumcrot D, Manoharan M, Koteliansky V, Sah DW . RNAi therapeutics: a potential new class of pharmaceutical drugs. Nat Chem Biol 2006; 2: 711–719.
Allerson CR, Sioufi N, Jarres R, Prakash TP, Naik N, Berdeja A et al. Fully 2′-modified oligonucleotide duplexes with improved in vitro potency and stability compared to unmodified small interfering RNA. J Med Chem 2005; 48: 901–904.
Hoshika S, Minakawa N, Matsuda A . Synthesis and physical and physiological properties of 4′-thioRNA: application to post-modification of RNA aptamer toward NF-kappaB. Nucleic Acids Res 2004; 32: 3815–3825.
Dande P, Prakash TP, Sioufi N, Gaus H, Jarres R, Berdeja A et al. Improving RNA interference in mammalian cells by 4′-thio-modified small interfering RNA (siRNA): effect on siRNA activity and nuclease stability when used in combination with 2′-O-alkyl modifications. J Med Chem 2006; 49: 1624–1634.
Czauderna F, Fechtner M, Dames S, Aygun H, Klippel A, Pronk GJ et al. Structural variations and stabilising modifications of synthetic siRNAs in mammalian cells. Nucleic Acids Res 2003; 31: 2705–2716.
Jackson AL, Burchard J, Leake D, Reynolds A, Schelter J, Guo J et al. Position-specific chemical modification of siRNAs reduces “off-target” transcript silencing. RNA 2006; 12: 1197–1205.
Amarzguioui M, Holen T, Babaie E, Prydz H . Tolerance for mutations and chemical modifications in a siRNA. Nucleic Acids Res 2003; 31: 589–595.
Tonges L, Lingor P, Egle R, Dietz GP, Fahr A, Bahr M . Stearylated octaarginine and artificial virus-like particles for transfection of siRNA into primary rat neurons. RNA 2006; 12: 1431–1438.
Futaki S, Ohashi W, Suzuki T, Niwa M, Tanaka S, Ueda K et al. Stearylated arginine-rich peptides: a new class of transfection systems. Bioconjug Chem 2001; 12: 1005–1011.
Crombez L, Charnet A, Morris MC, Aldrian-Herrada G, Heitz F, Divita G . A non-covalent peptide-based strategy for siRNA delivery. Biochem Soc Trans 2007; 35: 44–46.
Simeoni F, Morris MC, Heitz F, Divita G . Peptide-based strategy for siRNA delivery into mammalian cells. Methods Mol Biol 2005; 309: 251–260.
Chu TC, Twu KY, Ellington AD, Levy M . Aptamer mediated siRNA delivery. Nucleic Acids Res 2006; 34: e73.
Kumar P, Wu H, McBride JL, Jung KE, Kim MH, Davidson BL et al. Transvascular delivery of small interfering RNA to the central nervous system. Nature 2007; 448: 39–43.
Jankowski MP, McIlwrath SL, Jing X, Cornuet PK, Salerno KM, Koerber HR et al. Sox11 transcription factor modulates peripheral nerve regeneration in adult mice. Brain Res 2009; 1256: 43–54.
Davidson TJ, Harel S, Arboleda VA, Prunell GF, Shelanski ML, Greene LA et al. Highly efficient small interfering RNA delivery to primary mammalian neurons induces MicroRNA-like effects before mRNA degradation. J Neurosci 2004; 24: 10040–10046.
Muratovska A, Eccles MR . Conjugate for efficient delivery of short interfering RNA (siRNA) into mammalian cells. FEBS Lett 2004; 558: 63–68.
Schwartz EI . Potential application of RNAi for understanding and therapy of neurodegenerative diseases. Front Biosci 2009; 14: 297–320.
Seyhan AA . RNAi: a potential new class of therapeutic for human genetic disease. Hum Genet 2011; 130: 583–605.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, Y., Friedlander, R. Using non-coding small RNAs to develop therapies for Huntington's disease. Gene Ther 18, 1139–1149 (2011). https://doi.org/10.1038/gt.2011.170
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2011.170
Keywords
This article is cited by
-
Bone scaffolds loaded with siRNA-Semaphorin4d for the treatment of osteoporosis related bone defects
Scientific Reports (2016)
-
Causes and Consequences of MicroRNA Dysregulation in Neurodegenerative Diseases
Molecular Neurobiology (2015)
-
Transcription, Epigenetics and Ameliorative Strategies in Huntington’s Disease: a Genome-Wide Perspective
Molecular Neurobiology (2015)
-
Novel siRNA delivery strategy: a new “strand” in CNS translational medicine?
Cellular and Molecular Life Sciences (2014)
-
Mechanisms of RNA-induced toxicity in CAG repeat disorders
Cell Death & Disease (2013)