Abstract
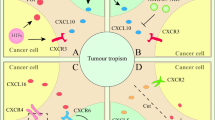
Mesenchymal stem cells (MSC) exhibit tropism for sites of tissue damage as well as the tumor microenvironment. Many of the same inflammatory mediators that are secreted by wounds are found in the tumor microenvironment and are thought to be involved in attracting MSC to these sites. Cell migration is dependent on a multitude of signals ranging from growth factors to chemokines secreted by injured cells and/or respondent immune cells. MSC are likely to have chemotactic properties similar to other immune cells that respond to injury and sites of inflammation. Thus, the well-described model of leukocyte migration can serve as a reasonable example to facilitate the identification of factors involved in MSC migration.Understanding the factors involved in regulating MSC migration to tumors is essential to ultimately develop novel clinical strategies aimed at using MSC as vehicles to deliver antitumor proteins or suppress MSC migration to reduce tumor growth. For example, radiation enhances inflammatory signaling in the tumor microenvironment and may be used to potentiate site-specific MSC migration. Alternatively, restricting the migration of the MSC to the tumor microenvironment may prevent competent tumor-stroma formation, thereby hindering the growth of the tumor. In this review, we will discuss the role of inflammatory signaling in attracting MSC to tumors.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Prockop DJ . Marrow stromal cells as stem cells for nonhematopoietic tissues. Science 1997; 276: 71–74.
Zappia E, Casazza S, Pedemonte E, Benvenuto F, Bonanni I, Gerdoni E et al. Mesenchymal stem cells ameliorate experimental autoimmune encephalomyelitis inducing T-cell anergy. Blood 2005; 106: 1755–1761.
Lopez Ponte A, Marais E, Gallay N, Langonné A, Delorme B, Hérault O et al. The in vitro migration capacity of human bone marrow mesenchymal stem cells: comparison of chemokine and growth factor chemotactic activities. Stem Cells 2007; 25: 1737–1745.
Li Y, Chen J, Wang L, Zhang L, Lu M, Chopp M . Intracerebral transplantation of bone marrow stromal cells in a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of parkinson's disease. Neurosci Lett 2001; 316: 67–70.
Niedzwiedzki T, Dabrowski Z, Miszta H, Pawlikowski M . Bone healing after bone marrow stromal cell transplantation to the bone defect. Biomaterials 1993; 14: 115–121.
Kawada H, Fujita J, Kinjo K, Matsuzaki Y, Tsuma M, Miyatake H et al. Nonhematopoietic mesenchymal stem cells can be mobilized and differentiate into cardiomyocytes after myocardial infarction. Blood 2004; 104: 3581–3587.
Dezawa M, Ishikawa H, Itokazu Y, Yoshihara T, Hoshino M, Takeda S et al. Bone marrow stromal cells generate muscle cells and repair muscle degeneration. Science 2005; 309: 314–317.
Dvorak HF . Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 1986; 315: 1650–1659.
Studeny M, Marini FC, Dembinski JL, Zompetta C, Cabreira-Hansen M, Bekele BN et al. Mesenchymal stem cells: potential precursors for tumor stroma and targeted-delivery vehicles for anticancer agents. J Natl Cancer Inst 2004; 96: 1593–1603.
Kanehira M, Xin H, Hoshino K, Maemondo M, Mizuguchi H, Hayakawa T et al. Targeted delivery of NK4 to multiple lung tumors by bone marrow-derived mesenchymal stem cells. Cancer Gene Ther 2007; 14: 894–903.
Hall B, Dembinski J, Sasser AK, Studeny M, Andreeff M, Marini F . Mesenchymal stem cells in cancer: tumor-associated fibroblasts and cell-based delivery vehicles. Int J Hematol 2007; 86: 8–16.
Nakamizo A, Marini F, Amano T, Khan A, Studeny M, Gumin J et al. Human bone marrow-derived mesenchymal stem cells in the treatment of gliomas. Cancer Res 2005; 65: 3307–3318.
Balkwill F . Cancer and the chemokine network. Nat Rev Cancer 2004; 4: 540–550.
Zernecke A, Weber KSC, Erwig LP, Kluth DC, Schröppel B, Rees AJ et al. Combinatorial model of chemokine involvement in glomerular monocyte recruitment: role of CXC chemokine receptor 2 in infiltration during nephrotoxic nephritis. J Immunol 2001; 166: 5755–5762.
Malek S, Kaplan E, Wang JF, Ke Q, Rana JS, Chen Y et al. Successful implantation of intravenously administered stem cells correlates with severity of inflammation in murine myocarditis. Pflug Arch Eur J Physiol 2006; 452: 268–275.
Winner M, Koong AC, Rendon BE, Zundel W, Mitchell RA . Amplification of tumor hypoxic responses by macrophage migration inhibitory factor-dependent hypoxia-inducible factor stabilization. Cancer Res 2007; 67: 186–193.
Ye J, Gao Z, Yin J, He Q . Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am J Physiol Endocrinol Metab 2007; 293: E1118–E1128.
Pold M, Zhu LX, Sharma S, Burdick MD, Lin Y, Lee PP et al. Cyclooxygenase-2-dependent expression of angiogenic CXC chemokines ENA-78/CXC ligand (CXCL) 5 and interleukin-8/CXCL8 in human non-small cell lung cancer. Cancer Res 2004; 64: 1853–1860.
Ubogu EE, Callahan MK, Tucky BH, Ransohoff RM . Determinants of CCL5-driven mononuclear cell migration across the blood-brain barrier. Implications for therapeutically modulating neuroinflammation. J Neuroimmunol 2006; 179: 132–144.
Gregory JL, Morand EF, McKeown SJ, Ralph JA, Hall P, Yang YH et al. Macrophage migration inhibitory factor induces macrophage recruitment via CC chemokine ligand 2. J Immunol 2006; 177: 8072–8079.
Montecucco F, Bianchi G, Bertolotto M, Viviani G, Dallegri F, Ottonello L . Insulin primes human neutrophils for CCL3-induced migration: crucial role for JNK 1/2. Ann N Y Acad Sci 2006; 1090: 399–407.
Lehman N, Di Fulvio M, McCray N, Campos I, Tabatabaian F, Gomez-Cambronero J . Phagocyte cell migration is mediated by phospholipases PLD1 and PLD2. Blood 2006; 108: 3564–3572.
Laconi E . The evolving concept of tumor microenvironments. BioEssays 2007; 29: 738–744.
Guo HT, Cai CQ, Schroeder RA, Kuo PC . Nitric oxide is necessary for CC-class chemokine expression in endotoxin-stimulated ANA-1 murine macrophages. Immunol Lett 2002; 80: 21–26.
Takahashi F, Takahashi K, Maeda K, Tominaga S, Fukuchi Y . Osteopontin is induced by nitric oxide in RAW 264.7 cells. IUBMB Life 2000; 49: 217–221.
Chamberlain G, Fox J, Ashton B, Middleton J . Concise review: mesenchymal stem cells: their phenotype, differentiation capacity, immunological features, and potential for homing. Stem Cells 2007; 25: 2739–2749.
Ringe J, Strassburg S, Neumann K, Endres M, Notter M, Burmester G-R . Towards in situ tissue repair: human mesenchymal stem cells express chemokine receptors CXCR1, CXCR2 and CCR2, and migrate upon stimulation with CXCL8 but not CCL2. J Cell Biochem 2007; 101: 135–146.
Allen SJ, Crown SE, Handel TM . Chemokine: Receptor structure, interactions, and antagonism. Annu Rev Immunol 2007; 25: 787–820.
Viola A, Luster AD . Chemokines and their receptors: drug targets in immunity and inflammation. Annu Rev Pharmacol Toxicol 2008; 48: 171–197.
Luster AD, Alon R, von Andrian UH . Immune cell migration in inflammation: present and future therapeutic targets. Nat Immunol 2005; 6: 1182–1190.
Becker MD, O'Rourke LM, Blackman WS, Planck SR, Rosenbaum JT . Reduced leukocyte migration, but normal rolling and arrest, in interleukin-8 receptor homologue knockout mice. Invest Ophthalmol Vis Sci 2000; 41: 1812–1817.
Sekido N, Mukaida N, Harada A, Nakanishi I, Watanabe Y, Matsushima K . Prevention of lung reperfusion injury in rabbits by a monoclonal antibody against interleukin-8. Nature 1993; 365: 654–657.
Leemans JC, te Velde AA, Florquin S, Bennink RJ, de Bruin K, van Lier RA et al. The epidermal growth factor-seven transmembrane (EGF-TM7) receptor CD97 is required for neutrophil migration and host defense. J Immunol 2004; 172: 1125–1131.
Galle J, Sittig D, Hanisch I, Wobus M, Wandel E, Loeffler M et al. Individual cell-based models of tumor-environment interactions: multiple effects of CD97 on tumor invasion. Am J Pathol 2006; 169: 1802–1811.
Zabel BA, Zuniga L, Ohyama T, Allen SJ, Cichy J, Handel TM et al. Chemoattractants, extracellular proteases, and the integrated host defense response. Exp Hematol 2006; 34: 1021–1032.
Pisterna GV, Siragusa M . CD44 presence in inflamed pulp tissue. J Endodontics 2007; 33: 1203–1207.
Chaulet H, Desgranges C, Renault MA, Dupuch F, Ezan G, Peiretti F et al. Extracellular nucleotides induce arterial smooth muscle cell migration via osteopontin. Circ Res 2001; 89: 772–778.
Jiang D, Liang J, Noble PW . Hyaluronan in tissue injury and repair. Annu Rev Cell Dev Biol 2007; 23: 435–461.
Simpson MA, Wilson CM, McCarthy JB . Inhibition of prostate tumor cell hyaluronan synthesis impairs subcutaneous growth and vascularization in immunocompromised mice. Am J Pathol 2002; 161: 849–857.
Herrera MB, Bussolati B, Bruno S, Morando L, Mauriello-Romanazzi G, Sanavio F et al. Exogenous mesenchymal stem cells localize to the kidney by means of CD44 following acute tubular injury. Kidney Int 2007; 72: 430–441.
Wright DE, Bowman EP, Wagers AJ, Butcher EC, Weissman IL . Hematopoietic stem cells are uniquely selective in their migratory response to chemokines. J Exp Med 2002; 195: 1145–1154.
Sutton A, Friand V, Brule-Donneger S, Chaigneau T, Ziol M, Sainte-Catherine O et al. Stromal cell-derived factor-1/chemokine (C-X-C motif) ligand 12 stimulates human hepatoma cell growth, migration, and invasion. Mol Cancer Res 2007; 5: 21–33.
Ip JE, Wu Y, Huang J, Zhang L, Pratt RE, Dzau VJ . Mesenchymal stem cells use integrin beta1 not CXC chemokine receptor 4 for myocardial migration and engraftment. Mol Biol Cell 2007; 18: 2873–2882.
Schwabe RF, Bataller R, Brenner DA . Human hepatic stellate cells express CCR5 and RANTES to induce proliferation and migration. Am J Physiol Gastrointest Liver Physiol 2003; 285: G949–G958.
Novo E, Cannito S, Zamara E, Valfrè di Bonzo L, Caligiuri A, Cravanzola C et al. Proangiogenic cytokines as hypoxia-dependent factors stimulating migration of human hepatic stellate cells. Am J Pathol 2007; 170: 1942–1953.
Lévesque JP, Hendy J, Takamatsu Y, Simmons PJ, Bendall LJ . Disruption of the CXCR4/CXCL12 chemotactic interaction during hematopoietic stem cell mobilization induced by gcsf or cyclophosphamide. J Clin Invest 2003; 111: 187–196.
Shi M, Li J, Liao L, Chen B, Li B, Chen L et al. Regulation of CXCR4 expression in human mesenchymal stem cells by cytokine treatment: Role in homing efficiency in NOD/SCID mice. Haematologica 2007; 92: 897–904.
Segers VFM, VanRiet I, Andries LJ, Lemmens K, Demolder MJ, De Becker AJ et al. Mesenchymal stem cell adhesion to cardiac microvascular endothelium: activators and mechanisms. Am J Physiol Heart Circ Physiol 2006; 290: H1370–H1377.
Li Y, Yu X, Lin S, Li X, Zhang S, Song YH . Insulin-like growth factor 1 enhances the migratory capacity of mesenchymal stem cells. Biochem Biophys Res Commun 2007; 356: 780–784.
Mira E, Lacalle RA, González MA, Gómez-Moutón C, Abad JL, Bernad A et al. A role for chemokine receptor transactivation in growth factor signaling. EMBO Rep 2001; 2: 151–156.
Schmidt A, Ladage D, Schinkothe T, Klausmann U, Ulrichs C, Klinz FJ et al. Basic fibroblast growth factor controls migration in human mesenchymal stem cells. Stem Cells 2006; 24: 1750–1758.
Dwyer RM, Potter-Beirne SM, Harrington KA, Lowery AJ, Hennessy E, Murphy JM et al. Monocyte chemotactic protein-1 secreted by primary breast tumors stimulates migration of mesenchymal stem cells. Clin Cancer Res 2007; 13: 5020–5027.
Wang L, Li Y, Chen J, Gautam SC, Zhang Z, Lu M et al. Ischemic cerebral tissue and MCP-1 enhance rat bone marrow stromal cell migration in interface culture. Exp Hematol 2002; 30: 831–836.
Ball SG, Shuttleworth CA, Kielty CM . Vascular endothelial growth factor can signal through platelet-derived growth factor receptors. J Cell Biol 2007; 177: 489–500.
Honczarenko M, Le Y, Swierkowski M, Ghiran I, Glodek AM, Silberstein LE . Human bone marrow stromal cells express a distinct set of biologically functional chemokine receptors. Stem Cells 2006; 24: 1030–1041.
Boyd JH, Divangahi M, Yahiaoui L, Gvozdic D, Qureshi S, Petrof BJ . Toll-like receptors differentially regulate CC and CXC chemokines in skeletal muscle via NF-kappaB and calcineurin. Infect Immun 2006; 74: 6829–6838.
West AP, Koblansky AA, Ghosh S . Recognition and signaling by toll-like receptors. Annu Rev Cell Dev Biol 2006; 22: 409–437.
Tomchuck SL, Zwezdaryk KJ, Coffelt SB, Waterman RS, Danka ES, Scandurro AB . Toll-like receptors on human mesenchymal stem cells drive their migration and immunomodulating responses. Stem Cells 2007; 26: 99–107.
Hamada H, Kobune M, Nakamura K, Kawano Y, Kato K, Honmou O et al. Mesenchymal stem cells (MSC) as therapeutic cytoreagents for gene therapy. Cancer Sci 2005; 96: 149–156.
Foxman EF, Kunkel EJ, Butcher EC . Integrating conflicting chemotactic signals: the role of memory in leukocyte navigation. J Cell Biol 1999; 147: 577–587.
Tabatabai G, Frank B, Mohle R, Weller M, Wick W . Irradiation and hypoxia promote homing of haematopoietic progenitor cells towards gliomas by TGF-beta-dependent HIF-1alpha-mediated induction of CXCL12. Brain 2006; 129 (Pt 9): 2426–2435.
Heissig B, Rafii S, Akiyama H, Ohki Y, Sato Y, Rafael T et al. Low-dose irradiation promotes tissue revascularization through VEGF release from mast cells and MMP-9-mediated progenitor cell mobilization. J Exp Med 2005; 202: 739–750.
Rabbany SY, Heissig B, Hattori K, Rafii S . Molecular pathways regulating mobilization of marrow-derived stem cells for tissue revascularization. Trends Mol Med 2003; 9: 109–117.
Schichor C, Birnbaum T, Etminan N, Schnell O, Grau S, Miebach S et al. Vascular endothelial growth factor A contributes to glioma-induced migration of human marrow stromal cells (hMSC). Exp Neurol 2006; 199: 301–310.
Kim SK, Kim SU, Park IH, Bang JH, Aboody KS, Wang KC et al. Human neural stem cells target experimental intracranial medulloblastoma and deliver a therapeutic gene leading to tumor regression. Clin Cancer Res 2006; 12: 5550–5556.
Evans CH, Robbins PD, Ghivizzani SC, Wasko MC, Tomaino MM, Kang R et al. Gene transfer to human joints: progress toward a gene therapy of arthritis. Proc Natl Acad Sci USA 2005; 102: 8698–8703.
Fiedler J, Röderer G, Günther KP, Brenner RE . BMP-2, BMP-4, and PDGF-bb stimulate chemotactic migration of primary human mesenchymal progenitor cells. J Cell Biochem 2002; 87: 305–312.
Forte G, Minieri M, Cossa P, Antenucci D, Sala M, Gnocchi V et al. Hepatocyte growth factor effects on mesenchymal stem cells: proliferation, migration, and differentiation. Stem Cells 2006; 24: 23–33.
Acknowledgements
This work was supported in part by grants from the National Cancer Institute (CA-1094551 and CA-116199 for FCM, CA-55164, CA-16672, and CA-49639 for MA) and by the Paul and Mary Haas Chair in Genetics (MA). ES, AK and FCM are supported in part by grants from the Susan G Komen Breast Cancer Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Spaeth, E., Klopp, A., Dembinski, J. et al. Inflammation and tumor microenvironments: defining the migratory itinerary of mesenchymal stem cells. Gene Ther 15, 730–738 (2008). https://doi.org/10.1038/gt.2008.39
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gt.2008.39
Keywords
This article is cited by
-
Adiponectin affects the migration ability of bone marrow-derived mesenchymal stem cells via the regulation of hypoxia inducible factor 1α
Cell Communication and Signaling (2023)
-
Pretreatment of UC-MSCs with IFN-α2 improves treatment of liver fibrosis by recruiting neutrophils
Journal of Translational Medicine (2023)
-
Side population cells derived from hUCMSCs and hPMSCs could inhibit the malignant behaviors of Tn+ colorectal cancer cells from modifying their O-glycosylation status
Stem Cell Research & Therapy (2023)
-
Dual-functional extracellular vesicles enable synergistic treatment via m6A reader YTHDF1-targeting epigenetic regulation and chemotherapy
Nano Research (2023)
-
Targeting the tumor stroma for cancer therapy
Molecular Cancer (2022)