Abstract
Purpose: Approximately 5–10% of patients who undergo genetic testing of BRCA1 and BRCA2 receive a variant of unknown significance (VUS) result. The ambiguous nature of a VUS may increase difficulty in patient understanding and decision making regarding risk reduction and surveillance options, including cancer risk-reducing surgeries. VUS reclassification to benign or deleterious may occur in time; however, clinical decisions may need to be made expeditiously, and some patients may pursue irreversible treatments before VUS reclassification.
Methods: We reviewed the surgical decisions of 107 women postdisclosure of a BRCA VUS result counseled at our institute between 1998 and 2009.
Conclusion: Among women receiving a BRCA VUS result at our center, 11 of 107 (10.3%) pursued cancer risk-reducing mastectomy and 22 of 107 (20.6%) pursued cancer risk-reducing bilateral salpingo-oophorectomy. Reclassification of VUS occurred up to 9 years after testing, and 5 of 22 (22.7%) women followed up for 8 or more years continue to have a VUS result. We discuss considerations for providers of genetic services to discuss with patients who receive a VUS result.
Similar content being viewed by others
Main
Hereditary breast and ovarian cancer associated with mutations in BRCA1 (OMIM# +113705) or BRCA2 (OMIM# *600185) account for 5–10% of all breast cancers; carriers of pathogenic mutations in BRCA1 or BRCA2 are at 40–73% lifetime risk of breast cancer and 11–41% lifetime risk of ovarian cancer.1–3 There are available recommendations for when to offer genetic counseling and consider genetic testing of BRCA1 and BRCA2, the genes most commonly associated with hereditary breast and ovarian cancer.4–6 The proportion of individuals who receive a variant of unknown significance (VUS) result from comprehensive BRCA1 and BRCA2 analysis historically varied widely by population with an overall VUS result rate of 7–15%,7 compared with Hispanic populations with VUS rates of up to 22%8 and African American populations with VUS rates of up to 46%.9 However, in more recent years with further testing and VUS reclassification, VUS detection rates in these populations decreased to approximately 5–10%.10
Many factors contribute to evaluating the clinical significance of a BRCA1 or BRCA2 variant, as addressed in practice guidelines of the National Society of Genetic Counselors11 (NSGC) (Table 1), and several models have been proposed to characterize these variants.12,13 However, in practice, it is often not possible to confidently establish the significance of a variant for the purpose of timely clinical decision making. The inherent ambiguity of risk conferred by a VUS result increases the complexity of cancer risk assessment and clinical recommendations. Implications of a VUS, therefore, must be carefully communicated and updates on VUS reclassification should be relayed to the patient. If the VUS is reclassified as deleterious, this provides support for clinical management recommendations, such as breast magnetic resonance imaging screening, beginning surveillance earlier, and cancer risk-reducing surgery.14,15 If the VUS is reclassified as a benign polymorphism, a patient may still be at increased risk of breast and ovarian cancer for the indications that motivated the initial testing (e.g., family history).
Previous studies have assessed patient comprehension, medical management outcomes, and psychosocial effects of deleterious mutations in BRCA1 and BRCA2, but less data are available in the case of a VUS result. Although the explanation of a VUS result can affect a patient's perception of cancer risk and risk reduction decision making, studies indicate that other variables may also play a role. For example, one woman who pursued risk-reducing bilateral mastectomy after VUS result disclosure cited both the ambiguity of the result and a persistent fear of cancer.16 Although misunderstanding of a VUS raises concern for false reassurance and less motivation to pursue surveillance options, multiple studies have not supported evidence for this concern.17–19 One study revealed that women who received a VUS result experienced higher levels of anxiety and depression at 1 and 6 months postdisclosure and higher levels of distress compared with women with no mutation.20 Other studies revealed that many women who undergo testing hope for a mutation-positive result to explain the etiology of their cancers and can experience frustration in the event of a VUS.21,22
At least one study has investigated associations between patient perceptions of VUS results and life impacts, including risk-reducing surgery outcomes.23 Subjective interpretation of the meaning of the VUS result was associated with prophylactic surgery outcomes, and participants attributed the decisions to pursue surgery to VUS disclosure instead of personal and family history of cancer. This small study of 24 women implied that despite correct recall that a VUS result was communicated to have an unknown association with cancer; women may subjectively interpret the result as pathogenic and pursue cancer risk-reducing surgery that may not be as beneficial as expected. Interpretation as pathogenic may serve as a coping mechanism to fulfill a need for a reason for cancer occurrence and may provide reasoning to err on the side of caution in determining the course of action for surveillance and prevention.23
Although not explicitly addressed in any of the aforementioned studies, the possibility of VUS reclassification may complicate the decision to pursue aggressive prevention treatments immediately because reclassification can occur months to years after disclosure. We describe herein our experience with cancer risk-reducing surgical decisions in patients who have received a BRCA VUS result, including those with results later reclassified as deleterious or benign.
METHODS
The University of Washington Medical Center (UWMC) Medical Genetics Clinic is a tertiary care facility that specializes in genetic disorders, including hereditary cancers. The clinic consists of nine medical genetics physicians and four board-certified genetic counselors and serves more than 1900 patients/year. Data are prospectively collected for purposes of quality improvement/assurance, including the number of patients seen for inherited cancer syndromes, genetic tests ordered through UWMC, and test results. Patients who received a BRCA VUS result, reclassification of the VUS as pathogenic or benign, and cancer risk-reducing surgery decisions documented in the electronic medical records were reviewed to assess compliance with NSGC practice standards and adequacy of VUS genetic counseling. Those patients with a VUS and an accompanying pathogenic mutation were excluded from further analysis as their decision making was likely influenced by the known deleterious mutation. Men were also excluded. For those individuals with multiple VUS, they were categorized under the result least likely to be interpreted as benign.
Records were reviewed to determine surgical decisions in women identified as BRCA VUS carriers. Surgeries were considered risk reducing if they were described as prophylactic or risk reducing in the surgical or clinical records. Surgeries were not considered cancer risk reducing if they were performed for treatment of cancer at that site, at another site (e.g., oophorectomy for estrogen/progesterone-positive breast cancer), or for unrelated benign indications. Each breast was considered as an independent entity, whereas both ovaries were considered as a single entity. For example, a woman whose breast cancer treatment entailed a unilateral mastectomy for breast cancer could have a cancer risk-reducing mastectomy (RRM) on the unaffected side and cancer risk-reducing salpingo-oophorectomy (RRO) to decrease the risk of ovarian cancer, whereas a woman with bilateral mastectomies for bilateral cancer could not have a RRM but could still have a RRO. Women were not recontacted for the purpose of determining whether they pursued risk-reducing surgery at an outside facility and only surgeries reported to a provider within UWMC were captured in this retrospective chart review.
This study is not designed to assess psychological impact of a VUS result; however, surgery decisions, especially those soon after results disclosure, may reflect patient result interpretation and associated anxiety. This project was ruled exempt from the University of Washington Institutional Review Board approval as it was initiated as a quality assurance measure.
RESULTS
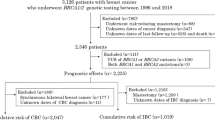
Between 1998 and 2009, approximately 1375 genetic tests for BRCA1 and BRCA2 had been ordered through the UWMC Medical Genetics Clinic. Utilization of genetic testing for breast and ovarian cancers has increased over the past 10 years, with five BRCA1 and BRCA2 tests ordered by the clinic staff in 1998 and 189 ordered in 2009. A total of 145 individuals were identified as having one or more VUS in BRCA1 or BRCA2 (Fig. 1), of which 132 records were sufficiently detailed for analysis. Reasons for referral are summarize in Table 2.
After exclusion of men and women who were tested for a known family variant or who had a known deleterious mutation, 107 female patients with a median age of 45 years (26–84) received a BRCA VUS test result. Ancestries as reported by the patients are as follows: 68.2% white, 8.4% Ashkenazi (at least one grandparent), Asian 7.5%, African descent 5.6%, native American 2.8%, African and Native American descent 0.9%, and unspecified 6.5%. Sixty-one women (57%) were counseled solely by genetic counselors, 42 (39.3%) were counseled by a medical geneticist and genetic counselor, and four (3.7%) were counseled solely by a medical geneticist. Cancer risk assessment and candidacy for genetic testing were typically based on clinical judgment, which permitted consideration of incomplete or complex family information, and family history of other associated cancers, such as melanoma or pancreatic cancer. Documentation of use of tools such as BRCAPro and Myriad prevalence tables was inconsistent and insufficient for meaningful analysis. Only nine women with VUS results reported no family history of breast and/or ovarian cancer. Eight of these women were referred for premenopausal breast cancer and one for ovarian and postmenopausal breast cancer. There was no follow-up for two women, including the one with ovarian cancer. One woman with breast cancer treated with lumpectomy and no reported family history went on to have bilateral RRM. Another woman with a result of “suspected deleterious” had a unilateral mastectomy for breast cancer treatment and went on to have risk-reducing bilateral salpingo-oophorectomy. The total number of women with no family history of cancer is insufficient to compare the likelihood of pursuing risk-reducing surgeries for women with and without family history of breast and/or ovarian cancer. The 13 unaffected women with a VUS result who were referred solely due to family history typically had a first-degree relative with ovarian cancer or premenopausal breast cancer who was unavailable or uninterested in testing or multiple generations of postmenopausal breast cancers with or without ovarian cancer.
The types of results disclosed included six (5.6%) initially classified as “suspect deleterious” and six (5.6%) initially classified as “favor polymorphism.” Forty-eight (44.9%) patients later received amended reports due to variant reclassification; among the amended reports, three (6.3%) VUS were reclassified as deleterious, three (6.3%) as “suspect deleterious,” three (6.3%) as “favor polymorphism,” and 39 (81.3%) as benign (Table 3). This classification reflects the test interpretation or amended reports issued by Myriad Genetics Laboratories.24 Years to reclassification ranged from 0 to 9; 5 of 22 (22.7%) female index cases followed for 8 or more years still had a result classified as a VUS (Fig. 2, A and B). As of June 1, 2010, 47 female patients (44% of the VUS population) tested at the UWMC Medical Genetics Clinic still had a result classified as a VUS; the median period of follow was 4 years (6 months to 11 years).
A, Current classification of initial VUS result. Length of available follow-up depends on year the woman was tested and her health status and cessation of ongoing care within our institute. Total bar height represents total number of women with follow-up for a given time period, and subgroups indicate current classification of initial VUS result. B, Time from identification of initial VUS result to reclassification. Time to reclassification of initial VUS result varied. Total bar height represents total number of VUS results reclassified at the designated time period, and subgroups indicate how VUS was reclassified.
Where available, pre- and posttest genetic counseling records documented the genetic counselor and/or geneticist gathered and provided information in accordance with the NSGC recommendations. On VUS result disclosure, the genetic counselors consistently relayed additional data provided by Myriad, including the number of times the result had been detected in index families in the Myriad Genetics database, the cosegregation with cancer in families, and the co-occurrence with deleterious mutations.
Women receiving a VUS result were advised to recontact the Medical Genetics clinic in 1–3 years for an update of the variant status and availability of additional testing; however, they were not seen routinely except as clinically indicated, such as when new personal, family, or variant information became available. Women for whom follow-up information is available typically received ongoing care at our affiliated multidisciplinary cancer care center; accordingly, follow-up intervals and duration were highly variable and dependent on the woman's health status. The pre- and posttest cancer diagnoses and surgical decisions of patients who received a BRCA VUS result are presented in Table 3. Post-VUS disclosure, 14 RRMs were performed in 11 women (7.5% unilateral and 2.8% bilateral); four were unilateral and performed at the time of contralateral therapeutic mastectomy, four were unilateral in a woman with a history of contralateral therapeutic mastectomy, two were bilateral in a woman who previously had unilateral breast conserving therapy (BCT), and four were bilateral in women with no personal history of cancer but who were assessed to be at high risk based on family history of breast cancer. At the time of this study, 7 of the 11 women who underwent RRM had results that remained classified as a VUS, 2 of 11 women had results that remained classified as a “suspect deleterious,” one woman had a result reclassified as deleterious, and one woman had a result reclassified as benign. Post-VUS disclosure, RROs were performed in 22 women (20.5%); 20 occurred in women with a personal history of breast cancer and two occurred in women with a family history of breast and/or ovarian cancer. Of the women pursuing postdisclosure RRO, 17 were treated by the same surgeon affiliated with UWMC, three by unidentified unaffiliated surgeons, and two by a separate affiliated surgeon. At the time of this study, 18 of 22 (81.8%) women pursing RRO post-VUS disclosure retained their originally classified results (15 VUS, three “suspect deleterious”); two (9.1%) women had a result reclassified as benign, one (4.5%) woman had a result reclassified as “suspect deleterious,” and one (4.5%) woman had a result reclassified as deleterious.
Motivations for risk-reducing surgery post-VUS disclosure cannot be fully ascertained from this retrospective chart review. Two women with no personal cancer history pursued bilateral RRM after BRCA VUS disclosure with the primary documented factor being strong family history of breast cancer. Factors documented in the other woman pursuing bilateral RRM after BRCA VUS disclosure included personal history of breast cancer successfully treated with lumpectomy and VUS results. Multiple factors in RRO surgical decision making were considered in 18 of 22 (81.8%) cases; of those, factors documented included uncertainty of genetic testing (61.1%), family history of breast and/or ovarian cancer (94.4%), and personal history including menopausal status and cancer history (83.3%). Two cases (9.1%) cited the VUS as the sole purpose for pursuing RRO; both were initially classified as “suspected deleterious” and both women had a history of breast cancer. Two cases (9.1%) were performed by unaffiliated surgeons, and records were not available for review.
Use of chemoprevention, such as tamoxifen, as an alternative or supplemental breast cancer risk-reducing option was not consistently documented.
DISCUSSION
In women referred for genetic counseling due to concern for being at increased risk of breast and/or ovarian cancer, identifying a VUS in BRCA1 or BRCA2 increases the complexity of genetic counseling and medical decision making. Irreversible treatment decisions may be made without knowing whether or when the VUS will be reclassified. Certainly, several other factors may impact a patient's clinical decision-making process.25,26 In women considered at high risk for breast and/or ovarian cancer, personal and family experience of cancer is likely to influence surgical decisions, as observed in our experience and elsewhere.27,28 Also, the available data, such as characteristics of the genetic alteration, results of functional assays, or observed cosegregation of VUS with disease, may give clues as to the direction the variant may be reclassified, and communication of this data may influence a patient's perception of a VUS. Other important factors, such as marital/partner status, ethnicity, parity, employment status, education, and insurance status may influence a patient's decision to undergo certain surveillance or risk-reducing procedures, although the first three factors were not observed to correlate with surgical decisions in a previous study.27 We did not evaluate these data for our study population due to inconsistent documentation.
Previous studies of women with pathogenic BRCA mutations are widely variable, showing 0-54% pursue RRM27,29–36 and 12–74% pursue RRO27,29–37 (Table 4). Comparatively, women tested for but not found to have BRCA pathogenic mutations pursued RRM and RRO, at estimated rates of 2–24% and 2–23%, respectively.27,32,38,39 In our study population of women receiving BRCA VUS results, 11 of 107 women (10.3%) pursued uni- or bilateral RRM and 22 of 107 women (20.6%) pursued RRO. This observed uptake rate overlaps those reported for women both with and without clearly pathogenic mutations. Surgical decision making in our population was highly contextual, and in only two cases, the VUS was the sole attributed reason for surgery (RRO); both cases were classified as “suspected deleterious” in women with a history of breast cancer. Two women with VUS later classified as benign pursued RRO, raising concern that surgery may have been performed in women not at increased risk of ovarian cancer. Although the risks of postmenopausal oophorectomy are largely limited to procedural risks, premenopausal women pursuing RRO assume additional risks due to loss of normal ovarian hormone secretion, including osteoporosis and sexual dysfunction.
In our study population, reclassification occurred up to 9 years after initial testing, and 22.7% of women followed up for 8 or more years after initial testing had results that remained classified as a VUS. To facilitate communication in the event of reclassification, it is important for clinics offering genetic counseling and testing to maintain a reliable system for contacting patients who have received a VUS result. As it may be unrealistic to expect clinics to assume the responsibility of maintaining current contact information for all patients who received a VUS result, it is important to emphasize the patient's role in alerting medical providers to changes in address and to periodically request updates on the status of VUS reclassification. In addition, it may be advisable to discuss with the patient how and whether to communicate reclassification information to their family in the event of their death as reclassification could be informative for medical decision making in family members. Recontact for updated information or at the time of reclassification also presents an opportunity to invite patients or family members for further genetic counseling and consideration of genetic testing that may not have been previously available. As recontact by the provider may be unexpected, our common practice has been to mail a brief letter informing the patient or family that updated information on the genetic variant is available and requesting them to call the clinic for further information. This allows the individual to initiate the conversation at a time and in a setting they feel appropriate.
The example of BRCA1 and BRCA2 VUSs reflects emerging issues in clinical application of genetic technologies. As uptake of genetic services and utilization of sequencing increase, the frequency of VUS detection will also increase. Recently discovered genes are likely to have even more complexity in prediction of risk because of limited data on the effects of variants.40
The ambiguities that accompany VUSs detected by the well-established BRCA genetic tests speak to the importance of administering genetic tests in a clinical setting accompanied by genetic counseling and the need for accurate and efficient classification tools, such as functional assays or statistical models. Providers of genetic services and patients who receive VUS results should discuss a plan for recontact in the event that new information become available. Moreover, because patients with VUS results may undergo irreversible interventions with associated risks and unclear benefits, periodic communication may help ensure patient understanding of this type of result and its conferred disease risk. An ongoing dialog about the most current understanding of a VUS will minimize the likelihood of surgical decisions based on misunderstood genetic information.
There are several limitations to this study. This report is based on retrospective chart review, and it is possible the nuances of the counseling session are not exhaustively documented in available records. Because we have not interviewed these patients nor are they research participants, we can only make assumptions about patient's subjective interpretation of VUS result and the role this type of result played in subsequent decisions to undergo cancer risk-reducing surgeries. As the majority the women who pursued RRO were treated by the same surgeon, we cannot evaluate the impact of the surgeon on patient decision making. Similarly, this report is limited to the experience of a single center and includes primarily non-Ashkenazi whites; it is possible that the findings do not generalize to all populations. Finally, post-VUS disclosure medical records are unavailable for 27.1% of our study population, likely because many were referred from unaffiliated providers to whom they returned for subsequent care. Despite these limitations, the available data offer insight into surgical outcomes in BRCA VUS carriers receiving clinical care at our institute over the first 11 years of BRCA clinical availability.
There are several areas for future research addressing patient understanding and use of genetic information postdisclosure of a VUS result. Qualitative studies with women receiving VUS results may offer insight into their experiences and concerns and suggest methods to improve the counseling process. Analysis of patient characteristics, such as demographics, personal medical history, and family history, may reveal factors associated with pursuit of cancer risk-reducing surgeries after VUS disclosure to ensure appropriate follow-up and additional counseling if necessary. Although the median age of the women in our study was 45, many of the women were of reproductive age; women with a VUS may alter reproductive decision making based on genetic testing. In addition, our findings reflect the practices of a single tertiary care academic center; it would be useful to characterize the experience of several sites, including a diversity of practice settings. Finally, it will be useful to investigate patient decision making after VUS disclosure in other highly penetrant cancer predisposition syndrome genes for which cancer risk-reducing surgeries are typically offered, such as the genes associated with Lynch syndrome or RET-associated familial medullary thyroid carcinoma.
As genetic testing for cancer susceptibility is offered to more moderate or low-risk women, the potential harm from risk-reducing surgeries for women identified with a VUS may be greater. For example, a VUS identified in a woman with a first-degree relative with postmenopausal breast cancer would have a low a priori risk of developing breast or ovarian cancer or of testing BRCA mutation positive. This compares with ovarian cancer where 10–15% may be attributable to BRCA1 and BRCA2 mutations,41,42 thus a woman with a VUS with a first-degree relative with ovarian cancer may be more likely to be counseled to consider bilateral salpingo-oophorectomy. Interestingly, our study sample had no women referred for family history of ovarian cancer alone, but this is becoming a much more common referral.
In conclusion, variants of unknown significance will continue to present both patients and providers with an uncertain measure of disease risk, thereby complicating decisions regarding cancer surveillance and prevention. Our experience described in this study shows that women who received BRCA1 or BRCA2 VUS results in the context of practices concordant with NSGC guidelines pursued cancer risk-reducing surgeries at rates overlapping reported uptake rates both in women with and without clearly pathogenic mutations. In addition, on the basis of the observation that VUS reclassification may occur at 9 or more years after testing, we endorse all providers offering genetic testing to establish a reliable tracking system and discuss with the patient a plan to communicate reclassification information to them or their family members in the event of their death. Challenges in medical decision making after identification of a genetic VUS are not unique to BRCA testing, and further research both in BRCA VUS disclosure and in other highly penetrant cancer predisposition genes will be helpful to guide future genetic counseling practices.
References
Chen S, Parmigiani G Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol 2007 25: 1329–1333
Antoniou A, Pharoah PD, Narod S, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet 2003 72: 1117–1130
Brose MS, Rebbeck TR, Calzone KA, Stopfer JE, Nathanson KL, Weber BL Cancer risk estimates for BRCA1 mutation carriers identified in a risk evaluation program. J Natl Cancer Inst 2002 94: 1365–1372
American College of Medical Genetics (ACMG). Genetic susceptibility to breast and ovarian cancer: assessment, counseling and testing guidelines, 2005. Available at: http://www.health.state.ny.us/nysdoh/cancer/obcancer/contents.htm. Accessed August 21, 2010.
American Society of Clinical Oncology (ASCO) American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol 2003 21: 2397–2406
United States Preventive Services Task Force (USPTSF) Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Ann Intern Med 2005 143: 355–361
Frank TS, Deffenbaugh AM, Reid JE, et al. Clinical characteristics of individuals with germline mutations in BRCA1 and BRCA2: analysis of 10,000 individuals. J Clin Oncol 2002 20: 1480–1490
Weitzel JN, Lagos V, Blazer KR, et al. Prevalence of BRCA mutations and founder effect in high-risk Hispanic families. Cancer Epidemiol Biomarkers Prev 2005 14: 1666–1671
Nanda R, Schumm LP, Cummings S, et al. Genetic testing in an ethnically diverse cohort of high-risk women: a comparative analysis of BRCA1 and BRCA2 mutations in American families of European and African ancestry. JAMA 2005 294: 1925–1933
Saam J, Burbidge LA, Bowles K, et al. Decline in rate of BRCA1/2 variants of uncertain significance: 2002–2008. Poster presented at the 27th Annual Education Conference of the National Society of Genetic Counselors, Los Angeles, CA, October 2008.
Berliner JL, Fay AM Risk assessment and genetic counseling for hereditary breast and ovarian cancer: recommendations of the National Society of Genetic Counselors. J Genet Couns 2007 16: 241–260
Gomez Garcia EB, Oosterwijk JC, Timmermans M, et al. A method to assess the clinical significance of unclassified variants in the BRCA1 and BRCA2 genes based on cancer family history. Breast Cancer Res 2009 11: R8
Spearman AD, Sweet K, Zhou XP, McLennan J, Couch FJ, Toland AE Clinically applicable models to characterize BRCA1 and BRCA2 variants of uncertain significance. J Clin Oncol 2008 26: 5393–5400
National Cancer Insitute (NCI). BRCA1 and BRCA2: cancer risk and genetic testing, 2009. Available at: http://www.cancer.gov/cancertopics/factsheet/Risk/BRCA. Accessed August 21, 2010.
Schwartz GF, Hughes KS, Lynch HT, et al. Proceedings of the international consensus conference on breast cancer risk, genetics, & risk management, April, 2007. Breast J 2009 15: 4–16
Weitzel JN, McCaffrey SM, Nedelcu R, MacDonald DJ, Blazer KR, Cullinane CA Effect of genetic cancer risk assessment on surgical decisions at breast cancer diagnosis. Arch Surg 2003 138: 1323–1329
van Dijk S, Otten W, Timmermans DR, et al. What's the message? Interpretation of an uninformative BRCA1/2 test result for women at risk of familial breast cancer. Genet Med 2005 7: 239–245
Dorval M, Gauthier G, Maunsell E, et al. No evidence of false reassurance among women with an inconclusive BRCA1/2 genetic test result. Cancer Epidemiol Biomarkers Prev 2005 14: 2862–2867
van Dijk S, Timmermans DR, Meijers-Heijboer H, Tibben A, van Asperen CJ, Otten W Clinical characteristics affect the impact of an uninformative DNA test result: the course of worry and distress experienced by women who apply for genetic testing for breast cancer. J Clin Oncol 2006 24: 3672–3677
O'Neill SC, Rini C, Goldsmith RE, Valdimarsdottir H, Cohen LH, Schwartz MD Distress among women receiving uninformative BRCA1/2 results: 12-month outcomes. Psychooncology 2009 18: 1088–1096
Hallowell N, Foster C, Ardern-Jones A, Eeles R, Murday V, Watson M Genetic testing for women previously diagnosed with breast/ovarian cancer: examining the impact of BRCA1 and BRCA2 mutation searching. Genet Test 2002 6: 79–87
Loader S, Shields CG, Rowley PT Impact of genetic testing for breast-ovarian cancer susceptibility. Genet Test 2004 8: 1–12
Vos J, Otten W, van Asperen C, Jansen A, Menko F, Tibben A The counsellees' view of an unclassified variant in BRCA1/2: recall, interpretation, and impact on life. Psychooncology 2008 17: 822–830
Myriad Genetic Laboratories. BRACAnalysis® technical specifications, 2008. Available at: http://www.myriadtests.com/provider/doc/BRACAnalysis-Technical-Specifications.pdf. Accessed August 21, 2010.
De Leeuw JR, van Vliet MJ, Ausems MG Predictors of choosing life-long screening or prophylactic surgery in women at high and moderate risk for breast and ovarian cancer. Fam Cancer 2008 7: 347–359
Ray JA, Loescher LJ, Brewer M Risk-reduction surgery decisions in high-risk women seen for genetic counseling. J Genet Couns 2005 14: 473–484
Uyei A, Peterson SK, Erlichman J, et al. Association between clinical characteristics and risk-reduction interventions in women who underwent BRCA1 and BRCA2 testing: a single-institution study. Cancer 2006 107: 2745–2751
McCullum M, Bottorff JL, Kelly M, Kieffer SA, Balneaves LG Time to decide about risk-reducing mastectomy: a case series of BRCA1/2 gene mutation carriers. BMC Womens Health 2007 7: 3
Skytte AB, Gerdes AM, Andersen MK, et al. Risk-reducing mastectomy and salpingo-oophorectomy in unaffected BRCA mutation carriers: uptake and timing. Clin Genet 2010 77: 342–349
Evans DG, Lalloo F, Ashcroft L, et al. Uptake of risk-reducing surgery in unaffected women at high risk of breast and ovarian cancer is risk, age, and time dependent. Cancer Epidemiol Biomarkers Prev 2009 18: 2318–2324
Beattie MS, Crawford B, Lin F, Vittinghoff E, Ziegler J Uptake, time course, and predictors of risk-reducing surgeries in BRCA carriers. Genet Test Mol Biomarkers 2009 13: 51–56
Morgan D, Sylvester H, Lucas FL, Miesfeldt S Cancer prevention and screening practices among women at risk for hereditary breast and ovarian cancer after genetic counseling in the community setting. Fam Cancer 2009 8: 277–287
Metcalfe KA, Foulkes WD, Kim-Sing C, et al. Family history as a predictor of uptake of cancer preventive procedures by women with a BRCA1 or BRCA2 mutation. Clin Genet 2008 73: 474–479
Meijers-Heijboer H, Brekelmans CT, Menke-Pluymers M, et al. Use of genetic testing and prophylactic mastectomy and oophorectomy in women with breast or ovarian cancer from families with a BRCA1 or BRCA2 mutation. J Clin Oncol 2003 21: 1675–1681
Wainberg S, Husted J Utilization of screening and preventive surgery among unaffected carriers of a BRCA1 or BRCA2 gene mutation. Cancer Epidemiol Biomarkers Prev 2004 13: 1989–1995
Lerman C, Hughes C, Croyle RT, et al. Prophylactic surgery decisions and surveillance practices one year following BRCA1/2 testing. Prev Med 2000 31: 75–80
Bradbury AR, Ibe CN, Dignam JJ, et al. Uptake and timing of bilateral prophylactic salpingo-oophorectomy among BRCA1 and BRCA2 mutations carriers. Genet Med 2008 10: 161–166
Schwartz MD, Kaufman E, Peshkin BN, et al. Bilateral prophylactic oophorectomy and ovarian cancer screening following BRCA1/BRCA2 mutation testing. J Clin Oncol 2003 21: 4034–4041
Schwartz MD, Lerman C, Brogan B, et al. Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. J Clin Oncol 2004 22: 1823–1829
Stuckey A, Dizon D, Scalia Wilbur J, et al. Clinical characteristics and choices regarding risk-reducing surgery in BRCA mutation carriers. Gynecol Obstet Invest 2010 69: 270–273
Botkin JR, Smith KR, Croyle RT, et al. Genetic testing for a BRCA1 mutation: prophylactic surgery and screening behavior in women 2 years post testing. Am J Med Genet A 2003 118A: 201–209
Lodder LN, Frets PG, Trijsburg RW, et al. One year follow-up of women opting for presymptomatic testing for BRCA1 and BRCA2: emotional impact of the test outcome and decisions on risk management (surveillance or prophylactic surgery). Breast Cancer Res Treat 2002 73: 97–112
Scheuer L, Kauff N, Robson M, et al. Outcome of preventive surgery and screening for breast and ovarian cancer in BRCA mutation carriers. J Clin Oncol 2002 20: 1260–1268
Sluiter M, Mew S, van Rensberg EJ PALB2 sequence variants in young South African breast cancer patients. Fam Cancer 2009 8: 347–353
Brozek I, Ochman K, Debniak J, et al. High frequency of BRCA1/2 germline mutations in consecutive ovarian cancer patients in Poland. Gynecol Oncol 2008 108: 433–437
Chetrit A, Hirsch-Yechezkel G, Ben-David Y, Lubin F, Friedman E, Sadetzki S Effect of BRCA 1/2 mutations on long-term survival of patients with invasive ovarian cancer; the national Israeli study of ovarian cancer. J Clin Oncol 2008 26: 20–25
Acknowledgements
This work was supported by the University of Washington Northwest Institute of Genetic Medicine from Washington State Life Sciences Discovery funds (Grant 265508) and by the National Institutes of Health T32 GM007454-32 (M.L.M.) for which G.P.J. is the principle investigator. The authors acknowledge Debbie Olson for her invaluable administrative support and the medical geneticists and genetic counselors who counseled these families.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Murray, M., Cerrato, F., Bennett, R. et al. Follow-up of carriers of BRCA1 and BRCA2 variants of unknown significance: Variant reclassification and surgical decisions. Genet Med 13, 998–1005 (2011). https://doi.org/10.1097/GIM.0b013e318226fc15
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e318226fc15
Keywords
This article is cited by
-
BRCA1 Norway: comparison of classification for BRCA1 germline variants detected in families with suspected hereditary breast and ovarian cancer between different laboratories
Familial Cancer (2022)
-
Whole genome sequencing for the investigation of canine mammary tumor inheritance - an initial assessment of high-risk breast cancer genes reveal BRCA2 and STK11 variants potentially associated with risk in purebred dogs
Canine Medicine and Genetics (2020)
-
Points to consider: is there evidence to support BRCA1/2 and other inherited breast cancer genetic testing for all breast cancer patients? A statement of the American College of Medical Genetics and Genomics (ACMG)
Genetics in Medicine (2020)
-
A comparison of cosegregation analysis methods for the clinical setting
Familial Cancer (2018)
-
Recontacting or not recontacting? A survey of current practices in clinical genetics centres in Europe
European Journal of Human Genetics (2018)