Abstract
Purpose: Coverage policies for genetic services for hereditary cancers are of interest because the services influence cancer risk reduction for both persons with cancer and their family members. We compared coverage policies for BRCA genetic testing and genetic counseling among selected payers in the United States to illuminate eligibility criteria variation that may explain differential access by insurance type. We compared these policies with policies for breast cancer screening with magnetic resonance imaging to consider whether payers apply a unique policy approach to genetic services.
Methods: We conducted a case study of large private and public payers selected on number of covered lives. We examined coverage policies for BRCA genetic testing, genetic counseling, and screening with magnetic resonance imaging and the eligibility criteria for each. We compared eligibility criteria against National Comprehensive Cancer Network guidelines.
Results: Eligibility criteria for BRCA testing were related to personal history and family history of cancer. Although private payers covered BRCA testing for persons with and without cancer, the local Medicare carrier in our study only covered testing for persons with cancer. In contrast, Arizona's Medicaid program did not cover BRCA testing. Few payers had detailed eligibility criteria for genetic counseling. Private payers have more detailed coverage policies for both genetic services and screening with magnetic resonance imaging in comparison with public payers.
Conclusion: Despite clinical guidelines establishing standards for BRCA testing, we found differences in coverage policies particularly between private and public payers. Future research and policy discussions can consider how differences in private and public payer policies influence access to genetic technologies and health outcomes.
Similar content being viewed by others
Main
BRCA testing is one of the first genetic tests to move from bench to bedside. Several professional associations have included BRCA testing in clinical guidelines to identify patients at high risk for hereditary breast and ovarian cancer.1–5 Guidelines from the US Preventive Services Task Force (USPSTF) recommend genetic counseling and BRCA testing for “… women whose family history is associated with an increased risk for deleterious mutations in BRCA1 or BRCA2 genes.”2 In addition, the National Comprehensive Cancer Network (NCCN) lays out in detail a clinical pathway to help providers identify persons with hereditary breast and ovarian cancer.4 NCCN has also incorporated into its guidelines American Cancer Society recommendations for breast cancer screening using magnetic resonance imaging (MRI) for persons at high risk for breast cancer6 (Table 1).
Access to BRCA testing and related services often depends on cost and coverage of services by payers.7–9 To leverage value of technologies and services, payers define scope of healthcare benefits based on eligibility criteria. Previous researchers have discussed coverage policy development and have even discussed policy formulation and considerations for genetic testing specifically.10–15 Although researchers have described policy development processes, few studies have examined the coverage policies themselves. Recently, Latchaw et al.16 reviewed policies of 10 private payers in Illinois and observed wide variability in coverage.
Coverage policies “… influence[s] the types of medical care Americans receive, because health insurance coverage is the gateway to the availability of medical innovations.”17 Policies contribute to setting thresholds of whom to test, then which screening and prevention services to offer and when. Without an understanding of the composition and content of the policies, we cannot begin to hypothesize how criteria within the policies may affect access by covered populations or differences in access between payers. Coverage policies for genetic services for hereditary cancers are of particular interest because the services influence cancer risk reduction for both persons with cancer and their family members.
We build on prior research by studying several national and local coverage policies for public and private payers to determine and compare the criteria included in coverage policies for BRCA genetic testing and genetic counseling. We also assess policies for a comparison service, breast cancer screening with MRI, to consider whether payers apply a unique policy approach to genetic testing and genetic counseling in relationship to other services. This article (1) describes the eligibility criteria for cancer risk genetic counseling, BRCA testing, and breast cancer screening with MRI; (2) compares eligibility criteria between payers and between services; and (3) discusses implications of these policies for covered persons.
MATERIALS AND METHODS
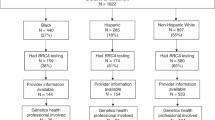
We conducted a case study of selected private and public payers. We chose payers and states with the largest number of covered lives because coverage policies would potentially have an impact on a large number of people. Number of covered lives is estimated by the Health Care Delivery Policy Program at Harvard University and the Kaiser Family Foundation.18–20 We selected states with a higher than average number of beneficiaries in 2007 (Medicaid) and 2010 (Medicare). In total, we reviewed policies from eight private payers and 17 states.
We searched several online databases in May 2011 to identify BRCA genetic testing and genetic counseling coverage policies among the selected payers. These included private payer websites, state Medicaid sites, the Medicare coverage policy database, and other electronic databases such as PubMed, Lexis Nexis legal, and Google.21–28
We identified BRCA testing and genetic counseling coverage policies for four private payers (Aetna, Cigna, Humana, and UnitedHealthcare) representing more than 50 million covered lives. We identified one local Medicare carrier (Washington State) with a policy addressing BRCA testing. We also found statements from four Medicaid programs (AZ, CA, IL, and NY)29–39 (Table 2). We then identified coverage policies for breast cancer screening with MRI among these payers.40–43
We used the NCCN clinical guidelines as a framework for examining eligibility criteria. We categorized criteria based on personal history of breast or ovarian cancer; family history of breast or ovarian cancer; race/ethnicity; age at diagnosis; BRCA mutation carrier status, family member carries a BRCA mutation, and/or other criteria.
RESULTS
Genetic testing
Personal history of cancer is a primary criterion for coverage among both private and public payers. Private payers, the local Medicare carrier, and California Medicaid combine this criterion with additional secondary criteria such as young age at diagnosis, family history, family history of BRCA carriers, or ethnicity (e.g., founder populations of Ashkenazi Jewish, Icelandic, Swedish, Hungarian, or other). Two private payers include clauses related to limited family structure or adoption of children.
Family history of breast and ovarian cancer is a primary criterion for coverage eligibility but only among private payers and California Medicaid. In contrast, Washington State's local Medicare coverage determination indicates that family history without a personal history of cancer is not adequate for Medicare coverage. The policy states, “Screening services, such as presymptomatic genetic tests and services, are those used to detect an undiagnosed disease or disease predisposition, and as such are not a Medicare benefit and not covered by Medicare. Similarly, Medicare may not reimburse the costs of tests/examinations that assess the risk for and/or of a condition unless the risk assessment clearly and directly effects the management of the patient …”37
Finally, documents from state Medicaid programs range from decisions of noncoverage to policies without eligibility criteria. Arizona's policy states that “Genetic testing is not covered to determine whether a member carries a hereditary predisposition to cancer or other diseases. Genetic testing is also not covered for members diagnosed with cancer to determine whether their particular cancer is due to a hereditary genetic mutation known to increase the risks of developing that cancer.”31 Memos, policy manuals, and fee schedules indicate that Illinois and New York Medicaid programs cover BRCA testing, but we did not identify any specific eligibility criteria from these payers.
Genetic counseling
Private payers have coverage policies for genetic counseling but do not outline in depth the eligibility criteria for receiving this service. All four private payers refer to genetic counseling services in relationship to receiving genetic testing or guiding treatment. Medicare in Washington also covers counseling before and after genetic testing. We did not identify policies for genetic counseling for the Medicaid programs in this study (Table 3).
Breast cancer screening with MRI
Private payers cover breast cancer screening with MRI for persons at high risk for hereditary breast and ovarian cancer. The eligibility criteria within private payer policies largely reflect NCCN guidelines (Table 4). Although we identified no policies specific to breast cancer screening with MRI for the public payers, Illinois and New York have considered legislation mandating coverage of screening by all insurers within the state.44,45
DISCUSSION
Our example of BRCA testing and genetic counseling highlights differences in coverage policies between four private and five public payers that may affect access and outcomes, particularly among enrollees with public insurance.
Private payers' policies are similar in content and include coverage for those with a personal history of cancer or a family history of cancer. In the absence of coverage for genetic counseling, primary care or other providers may have responsibility for taking and documenting family history. This may affect eligibility for coverage of testing as medical providers do not always take reliable family histories.46–51 Requirements for documentation of family history may also have an impact on access among persons who cannot obtain family history due to blocked family communications, dispersed families, or differing concepts of cancer and family relations.52–54
The local Medicare policy (first implemented in 2007) that we reviewed covers only persons with a personal history of cancer despite USPSTF recommendations to test women with a family history of cancer.2,55 Future studies can document whether BRCA testing coverage changes among public payers in response to passage of the Patient Protection and Affordable Care Act. This new law eliminates cost sharing for preventive services recommended by the USPSTF.56
Several Medicaid programs in our study have policies with no eligibility criteria or consider BRCA testing a noncovered service. It is unclear what lack of defined criteria may mean for persons seeking BRCA testing or genetic counseling in a public payer setting. One possibility is inconsistent coverage determinations that occur on a case-by-case basis. Alternatively, lack of defined criteria may result in a lower threshold that must be met before receiving coverage. These differences may have implications for access among low-income persons and for regional variations in utilization.
We compared policies for BRCA testing with policies for screening with MRI. Private payers included detailed eligibility criteria for both BRCA testing and MRI, whereas coverage policies from public payers were largely absent. This suggests that private payers may communicate policies and eligibility criteria more explicitly than public payers, and private payers' open approach may not be unique to genetic testing.
The scope of this assessment is limited to only a convenience sample of payers and policies. The large plans in this analysis may have a more developed system for reviewing evidence and updating coverage policies compared with smaller plans. These large payers, however, may act as trendsetters with smaller payers adopting similar policies based on the large payers' evidence reviews and policies. Although we include a limited number of plans, they cover approximately 50 million privately insured lives, 1.5 million lives under a local Medicare carrier, and 18.7 million lives under four state Medicaid programs. This research represents the state of coverage in 2011, but policies change over time. As a result, the policies that we identify may not be those used by the payers to determine coverage. Also, importantly, a lack of policy does not equal lack of coverage; furthermore, the presence of a policy is not synonymous with coverage.57
This analysis highlights how even an established genetic technology for a hereditary condition continues to manifest in differential coverage policies. Importantly, we suggest open discussions between policy makers, patients, advocates, and researchers regarding the coverage of genetic technologies among public payers in particular. Within a context of severe state budget constraints, we must continue to evaluate the need for genetic testing in tandem with coverage priorities for other important preventive health services that extend access to a broader segment of the population.
In summary, coverage policies among private and public payers vary despite professional guidelines that establish BRCA testing as standard of care. Policies range from BRCA testing as a noncovered service to policies with detailed eligibility criteria emphasizing personal history and family history of cancer. Future research and policy discussions can consider how policies affect access and utilization of services among privately insured compared with publicly insured populations. In the future, the Patient Protection and Affordable Care Act may affect coverage policies for BRCA testing and genetic counseling among public payers.
References
Berliner JL, Fay AM Risk assessment and genetic counseling for hereditary breast and ovarian cancer: recommendations of the National Society of Genetic Counselors. J Genet Couns 2007 16: 241–260
U.S. Preventive Services Task Force Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Ann Intern Med 2005 143: 355–361
Robson ME, Storm CD, Weitzel J, Wollins DS, Offit K American Society of Clinical Oncology policy statement update: genetic and genomic testing for cancer susceptibility. J Clin Oncol 2010 28: 893–901
National Comprehensive Cancer Network. Genetic/familial high-risk assessment: breast and ovarian, version 1, 2011. Practice guidelines. Available at: http://www.nccn.org. Accessed May 12, 2011.
American College of Medical Genetics Foundation. Genetic susceptibility to breast and ovarian cancer: assessment, counseling, and testing guidelines, 1998. Available at: www.health.state.ny.us/nysdoh/cancer/obcancer/contents.htm. Accessed July 15, 2011.
National Comprehensive Cancer Network. Breast cancer screening and diagnosis, version 1, 2011. Practice guidelines. Available at: http://www.nccn.org. Accessed May 12, 2011.
Kieran S, Loescher LJ, Lim KH The role of financial factors in acceptance of clinical BRCA genetic testing. Genet Test 2007 11: 101–110
Lee SC, Bernhardt BA, Helzlsouer KJ Utilization of BRCA1/2 genetic testing in the clinical setting: report from a single institution. Cancer 2002 94: 1876–1885
Velicer CM, Taplin S Genetic testing for breast cancer: where are health care providers in the decision process?. Genet Med 2001 3: 112–119
Burken MI, Wilson KS, Heller K, Pratt VM, Schoonmaker MM, Seifter E The interface of medicare coverage decision-making and emerging molecular-based laboratory testing. Genet Med 2009 11: 225–231
Giacomini M, Miller F, O'Brien BJ Economic considerations for health insurance coverage of emerging genetic tests. Community Genet 2003 6: 61–73
Logue LJ Genetic testing coverage and reimbursement: a provider's dilemma. Clin Leadersh Manag Rev 2003 17: 346–350
Ramsey SD, Veenstra DL, Garrison LP Jr, et al. Toward evidence-based assessment for coverage and reimbursement of laboratory-based diagnostic and genetic tests. Am J Manag Care 2006 12: 197–202
Schoonmaker M, Bernhardt B, Holtzman NA Coverage of new genetic technologies: what matters to insurers?. Am J Hum Genet 1996 59: A3
Schoonmaker MM, Bernhardt BA, Holtzman NA Factors influencing health insurers' decisions to cover new genetic technologies. Int J Technol Assess Health Care Winter 2000; 16: 178–189
Latchaw M, Ormond K, Smith M, Richardson J, Wicklund C Health insurance coverage of genetic services in Illinois. Genet Med 2010 12: 525–531
Garber AM Cost-effectiveness and evidence evaluation as criteria for coverage policy. Health Aff (Millwood) 2004; suppl web exclusives:W4– 284–296.
Helfner C Covered lives. The numbers, 2007. Available at: http://www.hks.harvard.edu/m-rcbg/hcdp/numbers.htm. Accessed May 15, 2010.
Kaiser Family Foundation. Total number of medicare beneficiaries, 2008. Available at: http://www.statehealthfacts.org/comparetable.jsp?typ=1&ind=290&cat=6&sub=74&sortc=1&o=a. Accessed May 15, 2010.
Kaiser Family Foundation. Total medicaid enrollment, FY2007, 2006. Available at: http://www.statehealthfacts.org/comparetable.jsp?typ=1&ind=198&cat=4&sub=52&sortc=1&o=a. Accessed May 15, 2010.
Aetna. Medical clinical policy bulletins. Available at: http://www.aetna.com/healthcare-professionals/policies-guidelines/medical_clinical_policy_bulletins.html. Accessed May 12, 2011.
Centers for Medicaid and Medicare Services. Medicare coverage database. Available at: http://www.cms.gov/mcd/search.asp?from2=search.asp&. Accessed May 12, 2011.
Cigna. Coverage policies/criteria medical & pharmacy index. Available at: http://www.cigna.com/customer_care/healthcare_professional/coverage_positions/index.html. Accessed May 12, 2011.
Humana. Medical coverage policies. Available at: http://apps.humana.com/tad/tad_new/home.aspx?type=provider. Accessed May 12, 2011.
State of California Department of Health Care Services. Provider manuals. Available at: http://files.medi-cal.ca.gov/pubsdoco/manuals_menu.asp. Accessed May 12, 2011.
UnitedHealthcare. Medical & drug policies and coverage determination guidelines. Available at: https://www.unitedhealthcareonline.com/b2c/CmaAction.do?channelId=016228193392b010VgnVCM100000c520720a____. Accessed May 12, 2011.
Arizona Health Care Cost Containment System (AHCCCS). AHCCCS medical policy manual (AMPM). Available at: http://www.azahcccs.gov/shared/MedicalPolicyManual/MedicalPolicyManual.aspx. Accessed May 12, 2011.
New York State Department of Health. Provider manuals. Available at: http://www.emedny.org/providermanuals/index.html. Accessed May 12, 2011.
Aetna. BRCA testing, prophylactic mastectomy, and prophylactic oophorectomy. Clinical policy bulletin, 2010. Available at: http://www.aetna.com/cpb/medical/data/200_299/0227.html. Accessed May 12, 2011.
Aetna. Genetic counseling. Clinical policy bulletin, 2010. Available at: http://www.aetna.com/cpb/medical/data/100_199/0189.html. Accessed May 11, 2011.
Arizona Health Care Cost Containment System (AHCCCS). Chapter 300: medical policy for AHCCCS covered services. Available at: http://www.azahcccs.gov/shared/Downloads/MedicalPolicyManual/Chap300.pdf. Accessed May 12, 2011.
Cigna. Genetic testing for susceptibility to breast and ovarian cancer (e.g., BRCA1 & BRCA2). Cigna medical coverage policy, 2010. Available at: http://www.cigna.com/customer_care/healthcare_professional/coverage_positions/medical/mm_0001_coveragepositioncriteria_genetic_testing_for_breast_and_ovarian_cancer.pdf. Accessed May 12, 2011.
Cigna. Genetic counseling. Cigna medical coverage policy, 2011. Available at: http://www.cigna.com/customer_care/healthcare_professional/coverage_positions/medical/mm_0297_coveragepositioncriteria_genetic_counseling.pdf. Accessed May 12, 2011.
Humana. Genetic testing and counseling for hereditary cancer syndromes. Medical coverage policy, 2011. Available at: http://apps.humana.com/tad/tad_new/Search.aspx?criteria=genetic&searchtype=freetext. Accessed May 12, 2011.
Illinois Department of Healthcare and Family Services. Reimbursement for genetic counseling services rendered by genetic counselors. Informational notice, 2008. Available at: http://www.hfs.illinois.gov/html/101408genetic.html. Accessed May 12, 2011.
New York State Department of Health. Fee schedule. Laboratory manual, 2010. Available at: http://www.emedny.org/ProviderManuals/Laboratory/index.html. Accessed May 12, 2011.
Noridian Administrative Services. Genetic testing. Local coverage determination, 2010. Available at: http://www.cms.gov/medicare-coverage-database/details/lcd-details.aspx?LCDId=23664&ContrId=35&ver=29&ContrVer=1&SearchType=Advanced&CoverageSelection=Local&PolicyType=Both&s=56&KeyWord=genetic&KeyWordLookUp=Doc&KeyWordSearchType=Exact&kq=true&bc=IAAAABAAAAAA&. Accessed May 12, 2011.
State of California Department of Health Care Services. Pathology: billing and modifiers. Provider manuals, 2011. Available at: http://files.medi-cal.ca.gov/pubsdoco/manuals_menu.asp. Accessed May 12, 2011.
UnitedHealthcare. Genetic testing for hereditary breast and/or ovarian cancer syndrome (HBOC). Medical policy, 2010. Available at: https://www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/Tools%20and%20Resources/Policies%20and%20Protocols/Medical%20Policies/Medical%20Policies/Genetic_Testing_HBOC_Syndrome.pdf. Accessed May 12, 2011.
Aetna. Magnetic resonance imaging (MRI) of the breast. Clinical policy bulletin, 2011. Available at: http://www.aetna.com/cpb/medical/data/100_199/0105.html. Accessed May 12, 2011.
Cigna. Magnetic resonance imaging (MRI) of the breast, 2010. Available at: http://www.cigna.com/customer_care/healthcare_professional/coverage_positions/medical/mm_0155_coveragepositioncriteria_mri_of_the_breast.pdf. Accessed May 12, 2011.
Humana. Breast magnetic resonance imaging (MRI). Medical coverage policy, 2010. Available at: http://apps.humana.com/tad/tad_new/Search.aspx?criteria=MRI&searchtype=freetext. Accessed May 12, 2011.
UnitedHealthcare. Physician guidelines: current, evidence-based recommendations regarding imaging, 2010. Available at: https://www.unitedhealthcareonline.com/ccmcontent/ProviderII/UHC/en-US/Assets/ProviderStaticFiles/ProviderStaticFilesPdf/Clinician%20Resources/Radiology%20Notification%20Program/Radiology%20Notification%20docs/Evidence_based_Clinical_Guidelines_Imaging.pdf. Accessed May 12, 2011.
Illinois General Assembly. Bill status of SB1464, 94th general assembly. Available at: http://www.ilga.gov/legislation/billstatus.asp?DocNum=1464&GAID=8&GA=94&DocTypeID=SB&LegID=18737&SessionID=50. Accessed May 12, 2011.
New York State Assembly. A01431 summary. Available at: http://assembly.state.ny.us/leg/?default_fld=&bn=A01431&Summary=Y&Actions=Y&Votes=Y&Memo=Y&Text=Y. Accessed May 12, 2011.
Tyler CV Jr, Snyder CW Cancer risk assessment: examining the family physician's role. J Am Board Fam Med 2006 19: 468–477
Sifri RD, Wender R, Paynter N Cancer risk assessment from family history: gaps in primary care practice. J Fam Pract 2002 51: 856
Rich EC, Burke W, Heaton CJ, et al. Reconsidering the family history in primary care. J Gen Intern Med 2004 19: 273–280
Wilson BJ, Qureshi N, Santaguida P, et al. Systematic review: family history in risk assessment for common diseases. Ann Intern Med 2009 151: 878–885
Berg AO, Baird MA, Botkin JR, et al. National Institutes of Health state-of-the-science conference statement: family history and improving health. Ann Intern Med 2009 151: 872–877
Burke W, Culver J, Pinsky L, et al. Genetic assessment of breast cancer risk in primary care practice. Am J Med Genet A 2009 149A: 349–356
Chivers Seymour K, Addington-Hall J, Lucassen AM, Foster CL What facilitates or impedes family communication following genetic testing for cancer risk? A systematic review and meta-synthesis of primary qualitative research. J Genet Couns 2010 19: 330–342
McGrath BB, Edwards KL When family means more (or less) than genetics: the intersection of culture, family and genomics. J Transcult Nurs 2009 20: 270–277
Orom H, Cote ML, Gonzalez HM, Underwood W 3rd, Schwartz AG Family history of cancer: is it an accurate indicator of cancer risk in the immigrant population?. Cancer 2008 112: 399–406
Lesser LI, Krist AH, Kamerow DB, Bazemore AW Comparison between US Preventive Services Task Force recommendations and Medicare coverage. Ann Fam Med 2011 9: 44–49
Henry J Kaiser Family Foundation. Focus on health reform, 2010. Available at: http://www.kff.org/healthreform/upload/8061.pdf. Accessed May 12, 2011.
Huang AJ, Gemperli MP, Bergthold L, Singer SS, Garber A Health plans' coverage determinations for technology-based interventions: the case of electrical bone growth stimulation. Am J Manag Care 2004 10: 957–962
Acknowledgements
This project was supported, in part, by the National Cancer Institute (no. P01CA130818); the Avon Foundation and the Bay Area Breast SPORE (NIH 2P50 CA058207); and the UCSF Helen Diller Family Comprehensive Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, G., Beattie, M., Ponce, N. et al. Eligibility criteria in private and public coverage policies for BRCA genetic testing and genetic counseling. Genet Med 13, 1045–1050 (2011). https://doi.org/10.1097/GIM.0b013e31822a8113
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31822a8113
Keywords
This article is cited by
-
Cancer Genetic Counseling and Testing: Perspectives of Epithelial Ovarian Cancer Patients and Gynecologic Oncology Healthcare Providers
Journal of Genetic Counseling (2018)
-
Development of a Streamlined Work Flow for Handling Patients’ Genetic Testing Insurance Authorizations
Journal of Genetic Counseling (2017)
-
Availability and payer coverage of BRCA1/2 tests and gene panels
Nature Biotechnology (2015)
-
Factors associated with genetic counseling and BRCA testing in a population-based sample of young Black women with breast cancer
Breast Cancer Research and Treatment (2015)
-
Exploring Barriers to Payer Utilization of Genetic Counselors
Journal of Genetic Counseling (2015)