Abstract
Purpose
Standardized and accurate variant assessment is essential for effective medical care. To that end, Clinical Genome (ClinGen) Resource clinical domain working groups (CDWGs) are systematically reviewing disease-associated genes for sufficient evidence to support disease causality and creating disease-specific specifications of American College of Medical Genetics and Genomics–Association for Molecular Pathology (ACMG-AMP) guidelines for consistent and accurate variant classification.
Methods
The ClinGen RASopathy CDWG established an expert panel to curate gene information and generate gene- and disease-specific specifications to ACMG-AMP variant classification framework. These specifications were tested by classifying 37 exemplar pathogenic variants plus an additional 66 variants in ClinVar distributed across nine RASopathy genes.
Results
RASopathy-related specifications were applied to 16 ACMG-AMP criteria, with 5 also having adjustable strength with availability of additional evidence. Another 5 criteria were deemed not applicable. Key adjustments to minor allele frequency thresholds, multiple de novo occurrence events and/or segregation, and strength adjustments impacted 60% of variant classifications. Unpublished case-level data from participating laboratories impacted 45% of classifications supporting the need for data sharing.
Conclusion
RAS-specific ACMG-AMP specifications optimized the utility of available clinical evidence and Ras/MAPK pathway–specific characteristics to consistently classify RASopathy-associated variants. These specifications highlight how grouping genes by shared features promotes rapid multigenic variant assessment without sacrificing specificity and accuracy.
Similar content being viewed by others
Introduction
With recent advances in sequencing technologies, generating genetic data is rapidly becoming cheaper, faster, and utilized across both clinical and research laboratories; however, clinical interpretation of variation remains subjective and complex, limiting accuracy and consistency. Interpretations can differ based on interlaboratory classification rules, access to unique case-level data, and other evidence.1,2 Funded by the National Institutes of Health, the Clinical Genome Resource (ClinGen; http://www.clinicalgenome.org) aims to elucidate, standardize, and archive clinical genetic knowledge and relevance of genetic variation for public use. A major standardization effort was the joint release of variant interpretation guidelines by the American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology (AMP) in 2015 (ref.3). These ACMG-AMP guidelines outline an evidence-based, quantitative framework to inform variant classification, but evaluation of its across-user reliability highlights the need for guidance and expert judgment in its application.2 More recently, clinical laboratories resolving variant discrepancies estimated ~13% of variant classification differences remained discordant due to differing use of these guidelines.1 In addition, differing allele frequency thresholds, which inform benign classifications, impact 9% of initial discrepancies. Thus, additional guideline specificity remains essential to providing accurate and consistent variant interpretations necessary for effective medical care. To improve specificity, ClinGen disease-specific working groups are systematically reviewing disease-associated genes for key evidence that supports disease causality and then creating disease-specific specifications of ACMG-AMP guidelines for variant classification.4
The ClinGen RASopathies Expert Panel (RAS EP) focuses on providing disease-specific recommendations for the genetically heterogeneous disorders caused by pathogenic variants in genes within the Ras/mitogen-activated protein kinase (Ras/MAPK) pathway. These phenotypically related disorders, collectively termed RASopathies, include Noonan syndrome (NS), Noonan syndrome with multiple lentigines (formerly known as LEOPARD syndrome), Costello syndrome, cardiofaciocutaneous syndrome, and Noonan-like syndromes resulting from pathogenic variants in BRAF, CBL, HRAS, KRAS, LZTR1, NF1, NRAS, MAP2K1, MAP2K2, PTPN11, RAF1, RIT1, SHOC2, SOS1, SOS2, and others.5,6,7,8,9 Most pathogenic variants produce an abnormal gain-of-function (GOF) effect that dysregulates Ras/MAPK pathway signaling and are inherited in an autosomal dominant manner with complete penetrance and variable expressivity; however, some genes (e.g., NF1, LZTR1) have been associated with loss-of-function (LOF)10,11 and/or autosomal recessive inheritance (unpublished data). NS, the most common of the RASopathies, is estimated to affect 1:1,000 to 1:2,500 individuals and has multisystem involvement with principal features including characteristic facial anomalies with hypertelorism and downslanted palpebral fissures, variable intellectual disabilities, skeletal involvement (e.g., pectus deformity and short stature), and cardiovascular abnormalities.12 Cardiovascular defects, observed in roughly 50–80% of NS individuals, include pulmonary valve stenosis, hypertrophic cardiomyopathy, and other congenital heart defects usually presenting early in life.13 Neurodevelopment varies substantially from normal to ~25% of affected individuals having learning disabilities.14 NS affects the ectodermal, hematopoietic, lymphatic, gastrointestinal, and genitourinary systems, and entails a predisposition to certain malignancies. Other RASopathies share these overlapping phenotypical features with varying severity and expressivity.
To date, more than 35 clinical laboratories across many countries offer multigene, next-generation sequencing–based genetic testing panels for the RASopathies (www.genetests.org; www.ncbi.nlm.nih.gov/gtr/). Some genes have established hotspots (e.g., missense defects altering Asn308 in PTPN11 or Ser257 in RAF1); however, many NS-causing variants have limited observations in affected individuals. Although these genes are highly evolutionarily conserved, missense variants are observed in general population cohorts (e.g., (ExAC; http://exac.broadinstitute.org/)).15 Most observed variation in these cohorts is benign as the frequencies are higher than the general population prevalence of NS; however, observations of ultrarare missense variation remains confounded as affected individuals with milder phenotypes and unaware of an existing genetic condition may be included.
Familial testing is informative for classification when a variant is inherited from a well-phenotyped unaffected parent, segregates with disease in affected family members, or occurs de novo in sporadic cases, which is estimated to occur in ~50% of NS cases.12 The predicted effect of a novel variant on protein function influences the likelihood that an ultrarare variant is disease causing. Missense variants underlying NS have GOF (i.e., hypermorphic or neomorphic) effects on Ras/MAPK signaling, and thus can be assessed through functional analysis of the Ras pathway using activation/inactivation mechanisms and/or catalytic functions.5 On the other hand, in silico informatic approaches predicting tolerance of amino acid substitutions depend highly on evolutionary conservation and, given Ras pathway proteins are highly conserved, most variation is deemed not tolerated, thus limiting the specificity of those algorithms for the RASopathies.
Here, we report the RAS EP’s results in curating gene and Ras/MAPK pathway–specific information and generating ACMG-AMP disease-specific guidelines for assessing variation associated with GOF effects in RASopathy genes.
Materials and methods
ClinGen RASopathy Expert Panel
The RAS EP membership represents a diverse range of expertise and qualifications including medical geneticists, research scientists, and clinical laboratory diagnosticians. Additionally, representatives from clinical diagnostic laboratories contribute to curating case-level data, variant classifications, and other RAS EP projects. Members divided into smaller teams to support gene groups with similar structure and/or function. The EP members and support team span national and international institutions in three countries (the United States, France, and Germany) and welcome public participation. All RAS EP members were subjected to disclosure of potential conflicts of interest and are required to maintain disclosure with ClinGen.
Data sources for variant classification
Genes and variants were curated using publicly available data sources and in silico prediction algorithms listed in Supplementary Table S1 online. Variants were prioritized for classification due to well-established pathogenic classifications or presence in ClinVar (https://www.ncbi.nlm.nih.gov/clinvar/). A variant’s filtering allele frequency, representing its statistically corrected population frequency, was obtained from ExAC.15,16 The National Heart, Lung, and Blood Institute’s Exome Sequencing Project Exome Variant Server was used rarely for frequencies of insertion/deletion variants.17 Clinical and research laboratories submitted internal data for review during variant interpretations or their data was extrapolated from ClinVar. Published data were obtained from relevant manuscripts.
Gene parameters
RASopathy-associated genes and conditions in the literature are listed in Supplementary Table S2 online.5,6,7,8,9 RAS EP gene-specific teams focused on defining parameters beneficial to variant classification of GOF effects for BRAF, HRAS, KRAS, MAP2K1, MAP2K2, PTPN11, RAF1, SHOC2, and SOS1. Assessed parameters include approved HUGO Gene Nomenclature Committee symbol, primary clinically relevant transcript, and associated RASopathy conditions. Dosage sensitivity available from the ClinGen Dosage Sensitivity Map was reviewed and accepted by the RAS EP. Additional curated information included identification of key functional domains, functional assays, and animal models. Gene parameters are shown in Supplementary Table S6 online. Application of ClinGen’s gene–disease validity framework18 to define the strength of evidence for the association between each RASopathy gene and condition, in which at least one claim was made, is in progress.
Specification of ACMG-AMP criteria
Each ACMG-AMP criterion3 was addressed for potential disease- or gene-specific specifications based on RAS EP expertise in evaluating variants in these genes and relative to the pathogenicity, incidence, and GOF disease mechanism of the RASopathies. NS was utilized as the representative disorder given it is the most common and well-studied disorder. Criteria specifications included gene- or disease-specific specifications, strength adjustments for surplus evidence, and judgment of criteria not applicable to the RASopathies (summarized in Table 1). Remaining criteria were used as recommended.
The RAS EP collaboratively engaged with ClinGen initiatives and working groups, including the Sequence Variant Interpretation Working Group and the Cardiomyopathy Working Group, to share and review specifications to maintain consistency and integrity of ACMG-AMP criteria application.
Specification validation and variant classification
The EP performed retrospective analysis of 37 exemplar pathogenic variants distributed across the aforementioned genes to highlight evidence requirements supporting pathogenicity. Classification of an additional 66 ClinVar variants validated final ACMG-AMP specifications.
Minor allele frequency (MAF) thresholds were calculated as described in the Results section (see Supplementary Table S3 online) and validated by evaluating the general population frequency of common pathogenic variants and/or hotspot positions. Briefly, over 5,000 diagnostic cases with reported pathogenic variants in the GeneDx (Gaithersburg, MD) internal database were compiled, and variants were grouped by the codon they altered (data not shown). The top three codons with pathogenic variation in each gene were evaluated for allele frequencies in three large population cohorts—ExAC, Exome Sequencing Project Exome Variant Server, and 1000 Genomes15,17,19—in order to confirm that benign allele frequency thresholds were not attained.
The RAS EP classified variants grouped into three categories: (i) well-established pathogenic variants (n = 37), (ii) variants with consistent (concordant) classifications in ClinVar across clinical laboratories (n = 28), and (iii) variants with inconsistent (discrepant) classifications in ClinVar (n = 38). First, each gene-specific team reviewed well-established pathogenic variants, typically with excessive functional and/or case-level data to determine criteria with abundant evidence supporting pathogenicity. Variants were re-reviewed using criteria strength specifications to ensure pathogenicity was retained in the absence of standard strong criteria. Any issues with criteria application or ambiguous data were reviewed by the RAS EP to improve specificity. Next, group 2 and 3 variants were used to validate proposed specifications. Final minor criteria adjustments occurred as needed based on expertise judgment of potentially unexpected classifications. The resultant approved specifications are reported herein.
For each variant, publicly available information and case-level data were collected through clinical and research laboratory contributions. Laboratories were encouraged to provide preliminary criteria assessments based on their available information. Gene-specific teams reviewed the cumulative data and relevant application of the modified ACMG-AMP criteria for accuracy. If the team unanimously approved of criteria usage, then criteria were combined per ACMG-AMP rules for final variant class. If criteria application was unclear or contested, the team presented evidence to the RAS EP for review. If needed, official polling of criteria application or variant classification was completed. Final applied criteria and approved classifications required complete consensus by gene-specific teams or an 80% quorum vote by the RAS EP. If these conditions were not met, the RAS EP deferred assignment of an official classification.
Results and discussion
ACMG-AMP criteria were established as general guidelines for interpreting variants for Mendelian disorders, so these broad and highly conservative criteria inevitably created disparities in their application. Reviewing ACMG-AMP guidelines in the context of a specific group of genes like those involved in the RASopathies revealed two distinct approaches for solving potentially ambiguous usage. First, initial specifications established a basic infrastructure for criteria specification relative to any related or unrelated genes that share the same inheritance pattern (e.g., autosomal dominant), general prevalence (e.g., rare), and disease mechanism (e.g., GOF). This approach provided significant utility in binning groups of genes sharing common underlying genetic characteristics for rapid variant classification in large data sets. Second, unique specifications including additional disease- and/or gene-specific assessments further refined classification precision when genes share similar features like overlapping functionality within a cellular process, signaling pathway, or protein structure. Utilizing either or both of these approaches can rapidly streamline interpretation workflows when genes, such as those involved in the RASopathies, are analyzed together in a clinical setting.
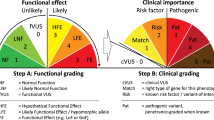
The RAS EP reviewed each ACMG-AMP criteria for its applicability to the RASopathies. Specifications (or lack thereof) were categorized into five major areas: (i) not applicable criteria, (ii) no changes, (iii) disease-specific, (iv) gene-specific, and (v) strength adjustable with extra evidence. Disease-specific ACMG-AMP specifications were adjusted relative to inheritance, prevalence, and GOF disease mechanism, while other criteria were deemed not applicable to the RASopathies. Gene-specific specifications highlighted criteria that uniquely apply based on the Ras/MAPK pathway and protein characteristics. For strength, the RAS EP recognized that certain criteria such as de novo occurrences in affected individuals were crucial evidence supporting pathogenicity, and, as these events accumulated, the likelihood a variant was pathogenic increased. Summarized RAS EP ACMG-AMP pathogenic and benign criteria specifications are listed in Table 1.
ACMG-AMP specifications and gene curation
Gene curation produced key information relevant to ACMG-AMP specifications and variant classification. All curated information discussed henceforth is summarized within Supplementary Table S6 online.
Based on the GOF disease mechanism and highly conserved nature of these genes, some disease- and gene-specific adjustments were assessed quickly. Supporting criterion PP2 (genes with a low rate of benign missense variation) was considered applicable to all genes. Supporting benign criterion BP1 (missense variant in a gene where only LOF cause disease) is not applicable given GOF variants are typically missense; however, in keeping with its rationale, we redefined BP1 to LOF variants in a gene where only GOF cause disease. The BP7 definition related to synonymous variants was expanded to include noncanonical intronic and regulatory variants, which are similarly correlated in likelihood of disease causality.
Other criteria were deemed not applicable. PM3 and PP4 are not applicable due to the RASopathies being a genetically heterogeneous group of autosomal dominant disorders. Additionally, a reputable database of RASopathy variant interpretations without supporting evidence does not exist; therefore, criteria PP5 and BP6 are not applicable.
Upon reviewing dosage sensitivity data, PVS1 (related to LOF variants) was also judged not applicable when assessing pathogenicity for RASopathies due to GOF effects. PTPN11 was the only gene with sufficient evidence supporting haploinsufficiency; however, this is associated with autosomal dominant metachondromatosis. Predicted LOF or null alleles in PTPN11 should be assessed using unmodified ACMG-AMP criteria. No gene had sufficient evidence supporting triplosensitivity, so criteria were not adjusted for this mechanism.
Gene-specific specifications were based on five subgroups sharing similar function and/or structure: (i) PTPN11, (ii) BRAF/RAF1, (iii) HRAS/KRAS/NRAS, (iv) MAP2K1/MAP2K2, and (v) SOS1/SOS2. Genes within these groups often share analogous residues, thus a known functional residue in one gene is equivalent in function to other genes within that subgroup. Using this logic, any pathogenic variant in one gene should have analogous pathogenic residues in other subgroup genes. ACMG-AMP criteria utilizing this logic are PS1 and PM5. Additionally, PM1 usage (i.e., mutational hotspots and/or critical and well-established functional domains) was explicitly defined for each gene and/or subgroup.
Appropriate functional assays for assessing pathogenicity primarily measured Ras/MAPK pathway dysregulation through increased phosphorylation of ERK or MEK. Most approved animal models exhibited dysmorphic or craniofacial anomalies and a cardiac phenotype. Detailed guidance for approved functional assays for application of PS3 is described in Supplementary Table S6 online.
Disease-specific and strength specifications of ACMG-AMP classification criteria
Assessments of allele frequencies (BA1, BS1, and PM2)
The standard ACMG-AMP threshold for applying BA1 was set at a highly conservative value of 5%. BS1 has a standard definition that the MAF is greater than expected for the disorder; however, defining expected remains subjective when factoring in genetic and allelic heterogeneity, penetrance, and other contributions. We established BA1, BS1, and PM2 by evaluating the generally accepted 1:1,000 to 1:2,500 prevalence range of NS12 and validated these thresholds by retrospective review of MAFs of known pathogenic variants. This prevalence range is an estimate of the true prevalence and observed prevalence, respectively, where true prevalence reflects the assumption that NS is often considered underdiagnosed or unascertained in the general population. To address this potential ascertainment bias, MAFs were assessed over varying values of bias (Supplementary Tables S3A,B online). Ultimately, the estimated true prevalence of 1:1,000 at full ascertainment was equivalent to 40% ascertainment bias in the observed prevalence of 1:2,500. The RAS EP agreed that the likelihood of 60% of unascertained affected individuals in the population was dubious. Thus, the extremely conservative prevalence of 1:1,000 at 100% ascertainment was approved to calculate the stand-alone MAF (BA1) as 0.0005 for these autosomal dominant, fully penetrant disorders.
The genetic and allelic heterogeneity of NS afforded additional means to adjust MAF thresholds for BS1. We refined BS1 MAF by incorporating gene contributions to NS. Pathogenic variants in PTPN11 were estimated as the highest contributor to NS causing ~50% of all cases; thus, at a prevalence of 1:1000 with full ascertainment, the MAF of all PTPN11 pathogenic alleles is estimated to be 0.00025. Given this extremely low threshold, it is neither beneficial nor necessary to further refine individual or allelic contribution values for each gene. Therefore, 0.00025 was established as BS1 MAF threshold for all genes.
To validate MAFs, the RAS EP retrospective reviewed the prevalence of the most common pathogenic variants observed in clinical testing (Supplementary Table S5 online). Given that there are known hotspot codons, the EP evaluated the combined MAF at a given codon versus independent allelic substitutions to ensure thresholds were conservative. At most one pathogenic allele at a given codon was observed in any population cohort with a minimum of 1,000 individuals,15,17,19 thus validating these MAF thresholds while recognizing that an occasional individual could be undiagnosed in the general population. Furthermore, a variant, PTPN11 p.Arg265Gln, presenting in patients with likely unrecognized mild phenotypic features20 also fell below these conservative thresholds. These assessments concluded that a variant should be completely absent from large population cohorts for PM2 usage.
Observation of multiple cases of de novo events (PS2 and PM6)
Strength of de novo case evidence corresponds to whether parentage is confirmed (PS2) or presumed (PM6). Knowing >50% of NS cases are sporadic, multiple cases may be observed, some with and some without parental confirmation, making it difficult to navigate when to apply PS2 and/or PM6. Therefore, we developed a series of criteria across PS2 and PM6 to denote various combinations of independent de novo occurrences, with and without parental data, guiding how to modulate the strength of evidence. For example, documentation of three affected individuals with presumed de novo events (PM6) should equal strong criteria, as it is highly unlikely that all cases have misattributed parentage. Very strong evidence of pathogenicity is supported with at least two confirmed cases or having one confirmed case in conjunction with two presumed. Dual application of both unmodified PS2 and PM6 is only acceptable with a singleton occurrence in each category.
Increased prevalence of variant in probands versus controls (PS4)
Criteria PS4 designates that variants with significantly higher prevalence in cases versus controls is strong evidence. Due to a potential lack of historical case-control studies, an added caveat allows for application of moderate evidence in instances where very rare variants were observed in multiple unrelated individuals with the same phenotype but absent from large population cohorts such as ExAC. Following the spirit of this caveat and given the inability to use PP4 due to genetic heterogeneity, the EP defined PS4 as an observation of at least five unrelated probands with similar phenotype as sufficient. Moderate and supporting criteria usage was defined as three to four and one to two unrelated probands, respectively. Every effort should be made to ensure that probands assessed from the literature are unique cases with a valid and relevant phenotype and no other reportable or potentially pathogenic variants are observed.
Observation of multiple segregations of phenotype in affected family members (PP1)
Criterion PP1 allocates supporting evidence when a variant cosegregates with disease and allows increasing strength with increasing cosegregations. The RAS EP emulated the statistical approach of the ClinGen cardiomyopathy MYH7 EP,21 which specified three levels of evidence using autosomal dominant likelihood ratios of 10 (3 meioses, logarithm of the odds 0.9), 30 (5 meioses, logarithm of the odds 1.5), and 100 (7 meioses, logarithm of the odds 2.1) to count as supporting, moderate, and strong evidence, respectively. For application, the variant must be absent from large populations (i.e., meet PM2 requirements). The EP recommends segregation observations in at least two separate families to decrease the likelihood that the identified variant is in linkage disequilibrium with an unidentified, truly causative variant, or have additional evidence supporting the variant as being causative (e.g., de novo occurrences or functional studies) and not the locus. This issue is being further defined by the ClinGen Sequence Variant Interpretation Working Group.
Performance of the RAS EP ACMG-AMP specifications in variant classification
Over 100 variants were classified using the modified RAS EP ACMG-AMP criteria presented here. These variants fell into three categories: (i) well-established pathogenic variants (n = 37), (ii) variants with consistent (concordant) classifications in ClinVar by clinical laboratories (n = 28), and (iii) variants with inconsistent (discrepant) classifications in ClinVar (n = 38).
Well-established pathogenic variants (group 1) achieved a pathogenic classification without using modified criteria; however, additional evidence available for modified criteria usage was noted and compared. The typical evidence supporting pathogenicity included PS2 (35%), and PS3 (81%), PM1 (76%), PM2 (97%), and PM6 (70%). Other criteria applied include PS1 (3%) and PP1 (14%). Given that PVS1 is not applicable to these genes, one strong criterion is required to classify a variant as pathogenic. Thus, if functional studies were unavailable, 54% (20/37) of these well-established pathogenic variants would not reach a pathogenic classification using standard ACMG-AMP criteria; however, use of strength specifications would recoup pathogenicity for 45% (9/20). This reinforced our strength specifications with additional criteria evidence.
ClinVar variants with concordant (n = 28) or discordant (n = 38) calls were compared relative to use of specified or unspecified criteria. Adjustment of MAF thresholds automatically classified 41% (27/66) of variants into the benign spectrum (Figure 1). These thresholds impact resolution of 37% (14/38) of discrepant ClinVar variants. No variant meeting BA1 or BS1 had conflicting evidence supporting pathogenicity. PM1 for curated functional domains and hotspots applied to 15% of variants. Multiple variants had additional evidence to support usage of strength-modified ACMG-AMP criteria (Figure 2). PS2 and PM6 for de novo occurrences and PS4 for probands were the most frequent criteria with additional evidence, and this underscores the importance of case-level data in variant classification. Approximately 27% of variants had multiple cases presumed de novo (PM6) and 23% had at least three probands (PS4). Interestingly, almost 60% (39/66) of variants had unique case-level data contributed by clinical or research laboratories not reported in the literature (data not shown), supporting the crucial need for public data sharing in databases such as ClinVar.
Variants with either concordant or discrepant classifications were assessed for their frequency in the general population. An additional 32% of variants met the RAS Expert Panel (EP) adjusted frequency threshold for BA1 versus the standard American College of Medical Genetics and Genomics–Association for Molecular Pathology (ACMG-AMP) BA1 threshold. One variant met the RAS EP adjusted frequency for BS1. Data points are colored by the ClinVar classification or discrepancy category of the variant. (Ben, benign; LBen, likely benign; LPath, likely pathogenic; Path, pathogenic; VUS, variant of uncertain significance).
Typically, most variants had additional evidence to achieve higher strength specifications beyond the standard ACMG-AMP definitions. Note that all modified criteria increase in strength with additional evidence except PS4 (*) given it begins at the strong category. No variant met the PS4 threshold of at least five occurrences due to the requirement of extensive phenotypic data.
Figure 3 compares original ClinVar classifications grouped by concordant tiers (Path/LPath, uncertain significance (VUS), Likely Benign (LBen)/Benign (Ben)) or discordant tiers (Path/LPath versus VUS, LBen/Ben versus VUS) to final RAS EP classifications. Of the final Path/LPath calls, 6/21 (~29%) of discordant or VUS ClinVar classifications upgraded to Path/LPath. Five variants specifically relied on strength-modified pathogenic criteria use for upgrading from VUS > LPath (n = 1) or LPath > PATH (n = 4). On the benign spectrum, 22/66 (~33%) of discordant or VUS classifications were deemed Ben/LBen. Interestingly, 73% (27/37) of benign spectrum variants met modified BA1 or BS1 MAF thresholds. The EP deemed that ~8% (5/66) of variants with either pathogenic or benign spectrum classifications in ClinVar lacked sufficient evidence for classification.
Prior to determining concordance, ClinVar classes were grouped into three categories: (i) pathogenic (Path) and likely pathogenic (LPath), (ii) benign (Ben) and likely benign (LBen), and (iii) variant of uncertain significance (VUS). Variant classifications were considered discordant if clinical laboratory submissions did not group into the same category. These grouped ClinVar classifications were compared with the classifications determined by using the RAS EP–specific ACMG-AMP specifications.
Limitations
The RAS EP acknowledges that these criteria are generally conservative to minimize false positive interpretations and further refinement over time may be necessary. Proband counts and (non-) segregations rely on well-phenotyped individuals; clinical labs must rely on notes by clinical providers to use these rules. Often clinical notes are lacking, and phenotypes provided on requisition forms may be inaccurate; therefore, the proband and segregation counts recommended here are also conservative. These specifications do not explicitly address small in-frame deletions or insertions due to exonic (or rarely intronic) variations that may have GOF effects. The PM4 criterion as written supplies moderate evidence for these variants.
Conclusion
The RAS EP presents a model of ACMG-AMP adaptation that can serve as a common framework for rare, autosomal dominant disorders. These RAS EP specifications highlight how grouping genes under a common phenotype, disease mechanism, and gene functionality allow for rapid multigenic variant assessment without sacrificing specificity and accuracy. Despite a highly conservative approach, MAF assessments had the greatest impact by instantly classifying over 40% of variants to likely benign or benign. Combining similar gene group approaches, as typically seen in clinical testing panels, and available incidence values from the literature or other reporting sources, such as Orphanet (www.orpha.net), would provide the necessary information for automating next-generation sequencing pipelines to rapidly classify variants with MAF <5% in global populations. Harmonizing ACMG-AMP criteria usage across disease groupings will increase consistency and accuracy of variant interpretations, thus improving clinical utility and management of patient care. In the future, the RAS EP will evaluate variants in ClinVar and their evidence to refine classifications of variants, especially those with uncertain significance, or resolve variants with discrepant classifications. Additionally, the RAS EP will assess validity of new disease-causing genes and provide expertise to improve the understanding of the Ras/MAPK genes and their related RASopathy conditions.
References
Harrison SM, Dolinsky JS, Knight Johnson AE et al. Clinical laboratories collaborate to resolve differences in variant interpretations submitted to ClinVar. Genet Med 2017;19:1096–1104.
Amendola LM, Jarvik GP, Leo MC et al. Performance of ACMG-AMP variant-interpretation guidelines among nine laboratories in the Clinical Sequencing Exploratory Research Consortium. Am J Hum Genet 2016;98:1067–1076.
Richards S, Aziz N, Bale S et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 2015;17:405–424.
Rehm HL, Berg JS, Brooks LD et al. ClinGen—the Clinical Genome Resource. N Engl J Med 2015;372:2235–2242.
Rauen KA. The RASopathies. Annu Rev Genomics Hum Genet 2013;14:355–369.
Tidyman WE & Rauen KA. Expansion of the RASopathies. Curr Genet Med Rep 2016;4:57–64.
Tidyman WE & Rauen KA. Pathogenetics of the RASopathies. Hum Mol Genet 2016;25:R123–R132.
Aoki Y, Niihori T, Banjo T et al. Gain-of-function mutations in RIT1 cause Noonan syndrome, a RAS/MAPK pathway syndrome. Am J Hum Genet 2013;93:173–180.
Koenighofer M, Hung CY, McCauley JL et al. Mutations in RIT1 cause Noonan syndrome—additional functional evidence and expanding the clinical phenotype. Clin Genet 2016;89:359–366.
Zenker M. Clinical manifestations of mutations in RAS and related intracellular signal transduction factors. Curr Opin Pediatr 2011;23:443–451.
Rojnueangnit K, Xie J, Gomes A et al. High incidence of Noonan syndrome features including short stature and pulmonic stenosis in patients carrying NF1 missense mutations affecting p.Arg1809: genotype-phenotype correlation. Hum Mutat 2015;36:1052–1063.
Allanson JE & Roberts AENoonan syndrome. In: Pagon RA, Adam MP, Ardinger HH et al (eds). GeneReviews. University of Washington: Seattle, WA, 1993–2017.
Roberts AE, Allanson JE, Tartaglia M & Gelb BD. Noonan syndrome. Lancet 2013;381:333–342.
Lee DA, Portnoy S, Hill P, Gillberg C & Patton MA. Psychological profile of children with Noonan syndrome. Dev Med Child Neurol 2005;47:35–38.
Lek M, Karczewski KJ, Minikel EV et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 2016;536:285–291.
Whiffin N, Minikel E, Walsh R et al. Using high-resolution variant frequencies to empower clinical genome interpretation. Genet Med 2017;19:1151–1158.
National Heart, Lung, and Blood Institute. GO Exome Sequencing Project (ESP), Seattle, WA. Exome Variant Server. http://evs.gs.washington.edu/EVS/. Accessed August 2017.
Strande NT, Riggs ER, Buchanan AH et al. Evaluating the clinical validity of gene-disease associations: an evidence-based framework developed by the Clinical Genome Resource. Am J Hum Genet 2017;100:895–906.
1000 Genomes Project Consortium1000 Genomes Project ConsortiumAuton A 1000 Genomes Project ConsortiumBrooks LD et al. A global reference for human genetic variation. Nature 2015;526:68–74.
Pannone L, Bocchinfuso G, Flex E et al. Structural, functional, and clinical characterization of a novel PTPN11 mutation cluster underlying Noonan syndrome. Hum Mutat 2017;38:451–459.
Kelly MA, Caleshu C, Morales A et al. Adaptation and validation of the ACMG/AMP variant classification framework for MYH7-associated inherited cardiomyopathies: recommendations by ClinGen's Inherited Cardiomyopathy Expert Panel. Genet Med; doi: 10.1038/gim.2017.218 [e-pub ahead of print, 4 January 2018].
Acknowledgments
Funding in part for work in this publication was supported by the National Human Genome Research Institute in conjunction with the Eunice Kennedy Shriver National Institute of Child Health and Human Development under award U41HG006834 (Rehm). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank other ClinGen representatives Steven Harrison, Danielle Azzariti, and Heidi Rehm for their suggestions. We also thank Amber Love and Leora Witkowski for collating variant information and ClinVar submissions. M.Z. was supported by grants from the German Ministry for Education and Research: NSEuroNet (FKZ 01GM1602A) and GeNeRARe (FKZ 01GM1519A).
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Gelb, B.D., Cavé, H., Dillon, M.W. et al. ClinGen’s RASopathy Expert Panel consensus methods for variant interpretation. Genet Med 20, 1334–1345 (2018). https://doi.org/10.1038/gim.2018.3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2018.3
Keywords
This article is cited by
-
A new genomic framework to categorize pediatric acute myeloid leukemia
Nature Genetics (2024)
-
Genomic testing for germline predisposition to hematologic malignancies
Blood Research (2024)
-
Prospective prenatal cell-free DNA screening for genetic conditions of heterogenous etiologies
Nature Medicine (2024)
-
Quantitative thresholds for variant enrichment in 13,845 cases: improving pathogenicity classification in genetic hearing loss
Genome Medicine (2023)
-
Cancer in Costello syndrome: a systematic review and meta-analysis
British Journal of Cancer (2023)