Abstract
Purpose
Pompe disease results from lysosomal acid α-glucosidase (GAA) deficiency and its associated glycogen accumulation and muscle damage. Alglucosidase alfa (recombinant human GAA (rhGAA)) received approval in 2006 as a treatment for Pompe disease at the 160 L production scale. In 2010, larger-scale rhGAA was approved for patients up to 8 years old without cardiomyopathy. NCT01526785 evaluated 4,000 L rhGAA efficacy/safety in US infantile- or late-onset Pompe disease (IOPD, LOPD) patients up to 1 year old transitioned from 160 L rhGAA.
Methods
A total of 113 patients (87 with IOPD; 26 with LOPD) received 4,000 L rhGAA for 52 weeks dosed the same as previous 160 L rhGAA. Efficacy was calculated as the percentage of patients stable/improved at week 52 (without death, new requirement for invasive ventilation, left ventricular mass z-score increase >1 if baseline was >2, upright forced vital capacity decrease ≥15% predicted, or Gross Motor Function Measure–88 decrease ≥8 percentage points). Safety evaluation included an extension ≤20 months.
Results
Week 52 data was available for 104 patients, 100 of whom entered the extension. At week 52, 87/104 (83.7%) were stable/improved. Overall survival was 98.1% overall, 97.6% IOPD, 100% LOPD; 92.4% remained invasive ventilator–free (93.4% IOPD, 88.7% LOPD). Thirty-five patients had infusion-associated reactions. Eight IOPD patients died of drug-unrelated causes.
Conclusions
Most Pompe disease patients were clinically stable/improved after transitioning to 4,000 L rhGAA. Safety profiles of both rhGAA forms were consistent.
Similar content being viewed by others
Introduction
Pompe disease (OMIM 232300) is an autosomal recessive lysosomal disorder caused by a deficiency of acid α-glucosidase (GAA)1 in which glycogen accumulation progressively damages skeletal, respiratory, and cardiac muscle.2 Classic infantile-onset Pompe disease (IOPD) is defined as symptom onset at ≤1 year of age with cardiomyopathy,3 late-onset Pompe disease (LOPD) as symptom onset at >1 year of age (irrespective of cardiac involvement) or ≤1 year without cardiomyopathy.3 Cardiac involvement defines classic IOPD3 but affects some patients with LOPD.4 Intermediate phenotypes occur occasionally4 (e.g., infant-onset cardiomyopathy with slower progression than that of classic IOPD5).
In 2006, the US Food and Drug Administration (FDA) approved Myozyme® (alglucosidase alfa (recombinant human GAA, rhGAA), Sanofi Genzyme, Cambridge, MA) produced at the 160 L pilot scale (160 L rhGAA) to treat all Pompe disease patients, based on IOPD studies.6,7 rhGAA manufactured at a larger scale subsequently received US approval in 2010, based on the Late Onset Treatment Study (LOTS, NCT00158600);8 however, owing to differing product attributes between 160 L and larger-scale rhGAA, the FDA required a separate Biologics License Application filing for the larger scale (Lumizyme®; Sanofi Genzyme, Cambridge, MA). The initially approved US indication of larger-scale rhGAA was limited to Pompe patients ≥8 years old without cardiomyopathy.9 Outside the United States, larger-scale rhGAA was approved for all Pompe disease patients.
To extend evidence for larger-scale rhGAA throughout the Pompe disease population, ADVANCE, a phase IV, open-label, 52-week study (NCT01526785), prospectively evaluated the safety and efficacy of 4,000 L rhGAA in previously 160 L rhGAA–treated US patients with Pompe disease aged ≥1 year, irrespective of cardiac involvement. ADVANCE data supported Lumizyme US label expansion to all patients with Pompe disease in 2014.
ADVANCE evaluated the comparability of larger-scale rhGAA in patients who had previously received 160 L rhGAA. The primary efficacy outcome was the percentage of patients clinically stable or improved at week 52: without death; new dependence on invasive ventilation; or worsened cardiac, respiratory, or motor status. Secondary objectives involved the evaluation of overall and invasive ventilator–free survival, changes from baseline in each primary end-point component, safety profile, and immunogenicity.
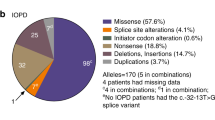
Genotypes and baseline phenotypes of participants will be detailed elsewhere (manuscript in preparation).
Materials and methods
ADVANCE was conducted at 52 US centers between 9 March 2012 and 29 December 2014. The Western Institutional Review Board (IRB; Puyallup, WA) or local IRBs approved the protocol/amendment and informed consent materials. ADVANCE complied with Good Clinical Practice and the Declaration of Helsinki. Parents/guardians of minors signed informed consent (as did any participants who were 18 years old or older); when possible, minors assented. An Independent Data and Safety Monitoring Board was consulted ad hoc. Centers, investigators, and IRBs are listed in Supplementary Appendix 1 online.
Inclusion and exclusion criteria
US patients ≥1 year old with a genetically and/or biochemically confirmed diagnosis of Pompe disease and who had previously received 160 L rhGAA were eligible. Enrollment in other studies, investigational treatments within the previous 3 months, clinical instability (unlikely to survive 52 weeks), or inability to comply were exclusionary. Female adolescents had to test negative for pregnancy.
Study periods
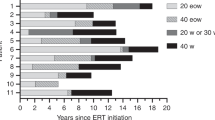
The efficacy phase was 52 weeks, followed by a safety extension continuing until label expansion (Figure 1A).
(a) Study period timeline. (b) Dosing regimens of 4,000 L rhGAA at week 52. (c) CONSORT diagram of patient flow. The full analysis set (N = 113) comprised all patients receiving at least one dose of 4,000 L rhGAA. A total of 104 patients had week 52 primary outcome data (including two patients who died on-study before week 52 and two patients who withdrew before week 52 and then died) and were the denominator for that end point. rhGAA, recombinant human alpha-glucosidase (alglucosidase alfa).
Treatment
Patients received intravenous 4,000 L rhGAA at the same dose as their prestudy 160 L rhGAA, generally 20 mg/kg body weight every other week (71.7% (81/113) of treated patients and 68.0% (68/100) of week 52 survivors; Figure 1B) for 52 weeks followed by an extension of ≤20 months.
Efficacy assessments
The primary efficacy outcome was the proportion of patients who at week 52 were stable or improved without any clinical worsening events: death, new invasive-ventilator dependency, increase in left ventricular mass (LVM) z-score >1 over a baseline z-score >2, total % Gross Motor Function–88 (GMFM-88) decrease of ≥8 percentage points from baseline (parallel to the validation population10), or seated % predicted forced vital capacity (FVC) decrease of ≥15 percentage points from baseline.
Secondary efficacy outcomes at week 52 were Kaplan–Meier estimates of overall and invasive ventilator–free survival and changes from baseline in LVM z-score, total GMFM-88 % score, and % predicted upright FVC.
Cardiac assessments
Echocardiographic LVM z-scores were determined11 at baseline and weeks 26 and 52, interpreted locally with masked central review. z-scoring avoided assumptions about the relationship of cardiac size and structure to children’s body surface areas.12
Respiratory assessments
Upright FVC was determined per guidelines13 in invasive ventilator–free patients deemed reliably testable.14 Ventilator use (invasive15 or noninvasive) was documented at each visit. Invasive-ventilator dependence was defined as initiation of invasive ventilation persisting for ≥14 days thereafter.
Motor assessments
Motor function levels, jointly categorizing children aged ≤2 and >2 years, were assessed at baseline only, classifying patients as walkers, supported walkers, supported standers, sitters, or those with restricted antigravity movement. Motor-decline history (within 2 months before enrollment) was collected.
GMFM-8816 was assessed at baseline and weeks 26 and 52. Originally a scale for cerebral palsy,17,18 GMFM-88 has been used in LOPD to develop the Quick Motor Function Test19 and in a previous clinical trial.20
Safety profile and immunogenicity
Adverse events (AEs) were monitored continuously in the efficacy and extension phases. Treatment-emergent AEs (TEAEs) occurred on treatment whether or not related to the treatment. Infusion-associated reactions (IARs) were related (or possibly related) TEAEs during infusion, ≤24 hours afterward, or delayed reactions thereafter. Vital signs, weight, and concomitant therapies were monitored at infusion visits. Physical examinations and 12-lead electrocardiograms (ECG) were conducted at baseline and weeks 26 and 52. Anti-rhGAA immunoglobulin (Ig) G titers were determined at enrollment, baseline, and every 4 weeks. High-sustained antibody titers (HSAT) were predefined as peak titers ≥25,600 that had not declined ≥2 dilution levels at final testing. IgE was tested only in patients with potential hypersensitivity. Extension assessments (physical examination, echocardiography, ECG, pulmonary function tests, hematology/blood chemistry/urinalysis, total and inhibitory IgG, height, and ventilator use) were performed every 6 months.
Statistical methods
Sample size included any confirmed US Pompe disease patients meeting inclusion/exclusion criteria. The safety/full analysis set included all patients receiving any 4,000 L rhGAA. The per-protocol population included patients with baseline and week 52 data, excluding those who discontinued, died, or received 160 L rhGAA during the study before week 52. No formal hypothesis testing was planned. Descriptive statistics with 95% confidence intervals (CI) were reported. Subgroup analyses (for five or more patients) included sex, invasive-ventilation status, 160 L treatment duration, age at 160 L initiation, baseline LVM z-score and motor-function levels, and peak IgG quartiles. IOPD and LOPD groups and age strata at prestudy 160 L initiation were analyzed descriptively post hoc. TEAEs were categorized by system, severity, and seriousness.
Results
Patient disposition and characteristics
Patient disposition is shown in Figure 1C. One hundred thirteen patients ≥1–18 years of age received ≥1 4,000 L rhGAA infusion. One hundred patients participated through week 52. Efficacy was evaluated in 104 patients with data for any primary end-point component (including death: before week 52, 2 patients died and 2 others withdrew and then died). At baseline, 43 patients were ventilated—32 invasively and 11 noninvasively—and 75 had any history of pneumonia. Median total treatment duration was 929 days (range 41–985 days). Table 1 summarizes the patient characteristics.
Eighty-seven treated patients had IOPD. Seventeen of these, despite symptom onset at <1 year of age and cardiac involvement,3 had started prestudy 160 L rhGAA at >1 year of age (see Table 1 footnotes); three had been diagnosed late (at ages 2.7 years, ~13 months, and ~14 months) and the others were diagnosed at <12 months of age. They may have atypical IOPD or an intermediate slower-progressing infantile cardiomyopathic phenotype.5 Twenty-six treated patients had LOPD: 6 with and 20 without cardiac involvement.
Efficacy
Primary outcome
At week 52, 87/104 (83.7%) patients were stable or improved (Table 2; IOPD: 69/82 (84.1%; 95% CI 74.4–91.3%); LOPD: 18/22 (81.8%; 95% CI 59.7–94.8%); per-protocol population: 86/98 (87.8%; 95% CI: 79.6–93.5%)).
Seventeen patients clinically worsened from baseline to week 52 (Table 2; baseline severities in Supplementary Appendix 2), including 2 on-study deaths before week 52 (2 others—both IOPD—who died after withdrawing before week 52 were not counted in the composite end point), 5 newly invasive ventilator–dependent (3 IOPD and 2 LOPD: 1 with and 1 without cardiac involvement), and 10 ventilator-free with a decline in GMFM-88 and/or FVC. Of the newly ventilator-dependent, 2 also had GMFM-88 decline. The LOPD patient who became ventilator-dependent at day 114, at age 2.84 years, thus failing the primary end point, nevertheless showed GMFM-88 improvement (77% baseline score +8.1 percentage points at week 52). Eight patients showed a decline in GMFM-88 alone at week 52; 2 a decline in both GMFM-88 and FVC.
No patient with complete LVM data exhibited clinical LVM z-score deterioration at week 52, although 2/52 (3.8%), both IOPD, had transient increases at week 26 (Table 2).
Twelve patients showed a decline of ≥8 GMFM-88 percentage points at week 52. At baseline, 1 of these had walked independently, 4 walked with assistance, 6 stood assisted, and 1 sat; 5 of the 12 had had prestudy motor decline.
Sensitivity analyses
These analyses examined lesser degrees of decline than those defined for the primary outcome measure. While 108 patients had baseline GMFM-88 data, only 90 also had week 52 data. Twelve of the 90 declined by ≥8 percentage points; 5 additional patients declined by ≥4 percentage points. Of 22 patients with week 52 FVC data, 2 declined by ≥15 percentage points; 1 more by >10, and 3 more by >5.
Subgroup analyses
More girls (44/48, 91.7%) than boys (43/56, 76.8%) were stable/improved at week 52. Baseline independent walkers (18/19, 94.7%), sitters (18/19, 94.7%), or restricted-mobility patients (22/26, 84.6%) had higher stable/improved proportions than supported walkers (18/23, 78.3%) or supported standers (9/15, 60.0%). Twenty-eight of 32 (87.5%) patients invasively ventilated at baseline and 59/72 (81.9%) ventilator-free patients were stable/improved at week 52. Only 2/6 (33.3%) patients with baseline LVM z-scores >5 were stable/improved at week 52, compared with 5/6 (83.3%) with an LVM z-score of 2–5 and 38/47 (80.9%) with an LVM z-score of –2 to 2.
Higher anti-rhGAA IgG titer quartiles had fewer stable/improved patients than lower quartiles: titer 0–400, 21/22 patients (95.5%); titer 800, 10/11 patients (90.9%); titer 1,600–3,200, 26/33 patients (78.8%); and titer 6,400–102,400, 14/19 patients (73.7%). Three of five patients who became invasive ventilator–dependent had peak IgG titers of 102,400, although only two of these had HSAT; the third had a persistent elevated titer below protocol-defined HSAT (final titer of 25,600 at week 117; minimum 6,400 [week 36]; peak 102,400 [week 30]). The other two newly ventilator-dependent patients had peak and last titers of 3,200 at day 28/1,600 at week 20 and 800 at day 450/400 at week 117.
Secondary outcomes
Secondary outcomes are shown in Figure 2. Kaplan-Meier curves indicated 98.1% overall survival at week 52 (95% CI 92.7–99.5%) overall, 97.6% (95% CI 90.7–99.4%) for IOPD, and 100.0% (95% CI 84.6–100.0%) for LOPD. Invasive ventilator–free survival was 92.4% (95% CI 83.9–96.5%) overall, 93.4% (95% CI 83.5–97.5%) for IOPD, and 88.7% (95% CI 61.4–97.1%) for LOPD. Two LOPD patients became invasive ventilator–dependent: one with and one without cardiac involvement.
Solid lines indicate survival or invasive ventilator–free survival percentages; dotted lines indicate 95% CIs. (a) Kaplan–Meier curve for overall survival. Solid lines indicate survival percentages; dotted lines indicate 95% CIs. (b) Kaplan–Meier curve for invasive ventilator–free survival. Solid lines indicate invasive ventilator–free survival percentages; dotted lines indicate 95% CI. (c) Mean and 95% CI GMFM-88 total % score per visit. (d) Mean and 95% CI change from baseline in GMFM-88 total % score. (e) Mean and 95% CI LVM z-score per visit. (f) Mean and 95% CI change from baseline in LVM z-score. (g) Mean and 95% CI % predicted seated FVC per visit. (h) Mean and 95% CI change from baseline in FVC. CI, confidence interval; FVC, forced vital capacity; GMFM-88, Gross Motor Function–88; IOPD, infantile-onset Pompe disease; LOPD, late-onset Pompe disease; LVM, left ventricular mass.
Sixty-seven patients had M-mode echocardiographic data at baseline and week 52. Mean LVM z-score was stable throughout (baseline mean ± SD −0.1 ± 2.63 vs. week 52 −1.0 ± 1.68) with a mean change of −0.5 ± 1.71 (IOPD: 0.4 ± 2.80 at baseline (n = 64), −0.8 ± 1.65 at week 52 (n = 50), mean change, −0.8 ± 1.83, and LOPD: –1.5 ± 1.42 at baseline (n = 22), –1.5 ± 1.73 at week 52 (n = 17), mean change 0.1 ± 1.13). Medians and ranges at baseline were −0.6 (−4.0 to 10.3) overall, −0.6 (−3.8 to 10.3) for IOPD, and −1.4 (−4.0 to 1.0) for LOPD, and at week 52 −1.0 (−4.7, 5.7) overall, −1.1 (−4.7 to 5.7) for IOPD, and −0.9 (−4.7 to 1.8) for LOPD. Median (range) changes at week 52 were −0.4 (−8.1 to 3.4) overall, −0.4 (−8.1 to 3.4) for IOPD, and −0.3 (−1.8 to 1.9) for LOPD. For patients with missing LVM z-score data, there were echocardiographic data-acquisition challenges due to Pompe-related remodeled cardiomyopathy.
Mean ± SD total GMFM-88 percent score improved significantly, from 46.3 ± 32.97% at baseline to 50.8% ± 35.99% at week 52, with a mean absolute change of 3.7 percentage points (95% CI 0.1–7.4 percentage points). Median (range) total GMFM-88% score at baseline was 47.9% (0.0–100.0%) overall, 38.9% (0.0–99.7%) for IOPD, and 70.9% (0.0–100.0%) for LOPD, and at week 52 55.7% (0.0–100.0%) overall, 45.3% (0.0–100.0%) for IOPD, and 85.9% (69.8%) for LOPD. Median (range) change at week 52 was 0.3 (−53.1 to 89.3) percentage points overall, 0.3 (−53.1 to 89.3) percentage points for IOPD, and 0.2 (−20.3 to 28.2) percentage points for LOPD.
Mean seated (upright) % predicted FVC was 66.6 ± 29.6% at baseline (n = 24), 73.3 ± 30.8% at week 26 (n = 23), and 71.1 ± 31.3% at week 52 (n = 22). Mean changes were 4.8 ± 11.5% (range −12.0% to 30.0%; 95% CI −0.2 to 9.8%) at week 26 and 2.3 ± 11.80% (range −17.4 to 36.0; 95% CI −3.0–7.5) at week 52. Medians and ranges were 64.5% (22.0–116.0%) at baseline and 74.5% (20.0–123.0%) at week 52, and the median (range) change was 1.0 (−17.4 to 36.0) percentage points.
One of 32 invasively and 2 of 11 noninvasively ventilated patients were ventilator-free at weeks 26 and 52. One patient required invasive and noninvasive ventilation at week 26 (and at final visit, week 28).
In post hoc evaluation of improvement using clinically important difference thresholds of the same magnitude as for decline (GMFM-88 increase ≥8 percentage points, LVM z-score decrease of 1 from a baseline of >2, or % predicted FVC increase of 15 percentage points), 22 patients were improved at week 52. Six patients without extension data were improved at week 52: 3 in GMFM-88 alone, 2 in LVM z-score alone (decrease of ≥1 from a baseline >2), and 1 in both GMFM-88 and LVM z-score. Twelve patients with extension data were improved in GMFM-88 alone at week 52 and further improved during the extension. In 2 patients with LVM z-score and GMFM improvements at week 52, GMFM further improved on the extension but extension LVM z-score data were unavailable. One patient was improved in % predicted FVC and total GMFM-88 score at week 52 and showed continued improvement in GMFM-88 on the extension without FVC data. One patient was improved in % predicted FVC at week 52 and in % predicted FVC and GMFM-88 on the extension.
Safety profile
Adverse events (efficacy plus extension periods) are summarized in Table 3. No patient left the study owing to an AE other than death. In TEAEs by systems, 97.4% of patients experienced infections, 75.2% general disorders/administration-site conditions, 74.3% gastrointestinal disorders, 74.3% respiratory/chest disorders, 53.1% skin conditions, 41.6% musculoskeletal and connective tissue disorders, 30.1% cardiac disorders, and 30.9% nervous system disorders.
Laboratory values unrelated to Pompe disease changed little from baseline to week 52. No urinalysis results required notification.
Thirty-five patients (31.0%) had 149 IARs (Supplementary Table S1); all were mild or moderate in intensity, and most were nonserious. Eight patients had IARs suggesting hypersensitivity; all tested negative for anti-rhGAA IgE antibodies. IARs by anti-rhGAA IgG titer quartiles of seropositive patients were as follows: 0–400, 9 events in 5/24 patients (21%); 800, 17 events in 2/13 patients (15%); 1,600–3,200, 34 events in 10/33 patients (30%); and 6,400–102,400, 75 events in 11/19 patients (58%).
Forty-four patients had 124 severe AEs, whether or not related to treatment. Severe AEs occurring in 5% or more of the safety population were pneumonia (11%), respiratory distress (8%), or respiratory failure (6%). Two patients had had 5–10 episodes each of pneumonia during the prestudy year; during the study one of these patients had one episode and the other had three episodes.
Seventy-three patients had 287 serious AEs (SAEs) whether or not related to treatment, most frequently pneumonia, respiratory distress, pyrexia, and device-related infection (e.g., associated with the infusion port). Eight patients had drug-related SAEs (serious IARs in six patients: one had abdominal pain, diarrhea, and pyrexia; one had vomiting; one had self-injurious ideation; one had pyrexia and chills (twice each), rhonchi, and tremor; one had peripheral edema; and one had chills, pyrexia, and nausea). Non-IAR drug-related SAEs were left ventricular hypertrophy, assessed as decreased treatment response (one patient) and gross motor delay (twice in one patient).
Eight patients with IOPD died of causes reflecting Pompe disease progression. Two died during the study before week 52, two after leaving the study before week 52, and four during the extension. Supplementary Table S2 lists causes, ages, IgG titer trajectories, and timing of deaths. Two patients who died had been diagnosed at ~2 months of age and had cardiac involvement at, respectively, ~2 months and 35 days of age but started 160 L rhGAA at, respectively, 7.9 and ~11 years of age. No deaths were deemed drug-related.
Immunogenicity
Seventy-seven of 113 (68.1%) patients were IgG anti-rhGAA–seropositive at baseline. Of those who were seronegative at baseline, 24 remained so after 52 weeks and 12 seroconverted at 148 ± 174 days (median 113 days, range 21–643 days; seroconverters’ median initial titer 100, range 100–1,600). Median peak anti-rhGAA IgG titer was 1,600 (n = 89, range 0–102,400) for patients who were seropositive at any point. Seven of these ever-seropositive patients (6.2%) tolerized during the study; 27 (23.9%) showed titer decreases of more than twofold; only five had HSAT.
No enzyme-inhibitory IgG antibodies were noted; one IOPD patient had uptake-inhibitory IgG antibodies. (This patient became invasive ventilator–dependent at day 289, at 4.3 years of age, and had a baseline GMFM-88 of 45.8%, declining by 4.5 percentage points at week 26 and 20.3 percentage points at week 52. The patient experienced five SAEs: two episodes of unspecified pneumonia and one each of parainfluenza pneumonia, sepsis, and device-related infection.)
Five patients had HSAT. Three of these had IOPD; two were genotypically predicted to be cross-reactive immunologic material (CRIM)-negative and one CRIM-positive or unclear. Of the two LOPD HSAT patients, one had cardiac involvement, the other did not (Supplementary Table S3 shows details, IgG trajectories, and outcomes). Three patients with peak titers of 102,400 (two HSAT and one with a sustained intermediate titer descending to 25,600 by week 52) became invasive ventilator–dependent.
Ten patients received concomitant immunomodulation (detailed in Supplementary Table S4); six were genotype-predicted as CRIM-negative, three were CRIM-positive, and one lacked genotype data. Four immunomodulated patients were ventilated at baseline (three invasively, one noninvasively). Three received intravenous immunoglobulin alone to prevent infections after pre-ADVANCE immunomodulation, not to reduce IgG during the study. One additional IOPD patient (HSAT patient 3 in Table S3) had received prophylactic immune-tolerance induction during a previous 160 L rhGAA study. Other patients may have received immunomodulation during prestudy clinical 160 L rhGAA treatment; this was not captured in our data.
Discussion
ADVANCE is the largest single-study cohort to date of treated US children aged 1 year and over with Pompe disease. Most (83.7%) who transitioned from 160 L to 4,000 L rhGAA remained clinically stable or showed improvement at week 52. Of the 16.3% not meeting the composite end point, a GMFM-88 total % score decline of ≥8 percentage points was the most common reason (12/90 evaluable patients (13.3%)). No one with LVM z-score data met the cardiac-decline criterion at week 52, and only 2/22 (9.1%) with FVC data met the respiratory-decline criterion.
Overall and ventilator-free survival figures for the full analysis set and IOPD and LOPD subgroups exceeded those from a previous 160 L rhGAA study involving 16 ventilator-free IOPD patients aged 6–36 months (week 52: survival 76.2%; invasive ventilator–free survival 62.5%).7 That study’s patients, unlike ours, were treatment-naive; prestudy untreated disease progression may have limited their overall and ventilator-free survival. ADVANCE’s IOPD patients included many long-term survivors on prestudy 160 L rhGAA. Of the 17 atypical IOPD patients who had survived to postinfancy 160 L rhGAA initiation, 14 survived throughout ADVANCE, possibly reflecting a “healthy survivor” effect.
Geographically diverse newborn-screening studies indicate that starting rhGAA even a few days earlier may lead to better outcomes.21 Delayed prestudy 160 L rhGAA initiation may have affected response if irreversible damage had already occurred before treatment.
ADVANCE’s LOPD patients were younger and more heterogeneous than those in LOTS8 and previously treated, whereas LOTS patients were alglucosidase alfa–naive. Still, LOTS patients, like ADVANCE patients, showed clinical improvement or stability: over 78 weeks of rhGAA treatment, the mean 6-minute-walk distance improved significantly and mean % predicted FVC was statistically stable (Supplementary Table S5). Participants in the 3-year MiniLOTS study of rhGAA in juvenile LOPD were 5.9–15.5 years old, ambulatory, able to perform FVC tests, and free of cardiac involvement.22 Their posttreatment motor and respiratory functioning exceeded those of ADVANCE patients (Supplementary Table S5).
In ADVANCE, mean standing and walking/running/jumping GMFM-88 dimensions (for patients having those skills) showed larger significant improvements from baseline compared with lying/rolling, sitting, and crawling/kneeling, suggesting that 4,000 L rhGAA ameliorated the characteristic lower-limb weight-bearing impairment of Pompe disease and enabled higher levels of motor-skill acquisition than are achievable in untreated disease.23 However, the more mobile patients contributed most to group changes in GMFM-88, whereas those who were nonambulatory at baseline remained so.
Supported walkers or supported standers at baseline were less often stable/improved than independent walkers, sitters, or minimally mobile patients. Sitters and minimally mobile patients had less baseline mobility to lose than supported walkers and supported standers; conversely, independent walkers may be less susceptible to motor decline than those more impaired. For patients with GMFM-88 baseline scores <8%, a floor effect precluded the decline criterion of ≥8 percentage points.
Proportionately more girls than boys were stable or improved. In previous studies24 male LOPD patients were more prevalent,25 had more respiratory impairment,26 and were more likely than females to have shoulder-girdle or bulbar-muscle weakness.26
Two of five HSAT patients became invasive ventilator-dependent during the study, as did another patient with sustained intermediate titer (peak 102,400 and final 25,600), thus failing the composite end point. In the higher IgG quartiles, there were more IARs and fewer stable or improved patients. Conversely, patients who started as seronegative and seroconverted during the study had lower initial titers (median 100 and maximum 1,600) than those starting as anti-160L rhGAA-seropositive. As for 160 L rhGAA in IOPD27 and LOPD,28 immune response affected the efficacy of 4,000 L rhGAA; both duration and intensity may affect clinical status.
Twenty-two patients showed potentially clinically important improvements from baseline to week 52, predominantly in GMFM-88, where those with extension data showed continuing improvement. High responders had a wide range of starting GMFM-88% scores, indicating that 4,000 L rhGAA enabled continued motor development at diverse starting functional levels. Five IOPD patients beginning ADVANCE with persistent cardiomegaly were substantially improved in LVM z-score at week 52. FVC improved in two IOPD patients, in contrast to adult LOPD, in which FVC generally stabilizes.
Pneumonia frequency in ADVANCE reflects age-related susceptibility (overall incidence in hospitalized children has been reported as 15.7/10,000 and as 62/10,000 in those under 2 years old29); the effects of Pompe disease on respiratory-muscle function, cough, and pulmonary hygiene;30 and the vulnerability of invasively ventilated patients to infection. In the Pompe Registry (Sanofi Genzyme, data on file), 109 IOPD patients (58.6% of those with data) and 312 LOPD patients (29.3% of those with data) have ever had pneumonia.
Study limitations include a single-arm design not directly comparing clinical effects between the two manufacturing scales of rhGAA. However, clinical stability or improvement of 83.4% of transitioned patients for at least 52 weeks in a progressive disease supports comparability. Not all patients could be assessed in all composite end-point components, limiting comparability of primary outcomes. FVC was evaluable only in invasive ventilator–independent, testable patients. LVM z-score was evaluable only in patients with echocardiographic data and a baseline LVM z-score >2. Eight patients with only postbaseline FVC testing and any others potentially becoming testable during the study were excluded from the respiratory component, which required baseline and week 52 FVC data. Of 87 stable/improved patients, 15 had data for all five primary end-point components, 28 for four, 23 for three, 18 for two, and 3 for one.
ADVANCE enrolled a large, clinically naturalistic set of 113 treated US Pompe patients ≥1 to 18 years of age; its strength is in including a classic IOPD subset within a broadly representative, geographically diverse real-world cohort. Inherent heterogeneity (in age, severity, phenotype, and prior treatment experience) limits the interpretability of overall group mean changes to indicate treatment response.
Conclusions
ADVANCE efficacy results showed that treatment with 4,000 L rhGAA for 52 weeks maintained clinical stability in most patients with Pompe disease who transitioned from 160 L rhGAA. Safety-profile observations were consistent with prior rhGAA experience; median anti-rhGAA titers remained low. No patients left the study because of AEs other than death, and all deaths were deemed related to Pompe disease rather than to rhGAA.
References
Kishnani PS, Beckemeyer AA. New therapeutic approaches for Pompe disease: enzyme replacement therapy and beyond. Pediatr Endocrinol Rev 2014;12(suppl 1):114–124.
Lim JA, Li L, Raben N. Pompe disease: from pathophysiology to therapy and back again. Front Aging Neurosci 2014;6:177.
Kishnani PS, Amartino HM, Lindberg C, Miller TM, Wilson A, Keutzer J. Timing of diagnosis of patients with Pompe disease: data from the Pompe registry. Am J Med Genet A 2013;161A:2431–2443.
Chien YH, Hwu WL, Lee NC. Pompe disease: early diagnosis and early treatment make a difference. Pediatr Neonatol 2013;54:219–227.
Lee DH, Qiu WJ, Lee J, Chien YH, Hwu WL. Hypertrophic cardiomyopathy in Pompe disease is not limited to the classic infantile-onset phenotype. JIMD Rep 2014;17:71–75.
Kishnani PS, Corzo D, Nicolino M et al. Recombinant human acid [alpha]-glucosidase: major clinical benefits in infantile-onset Pompe disease. Neurology 2007;68:99–109.
Nicolino M, Byrne B, Wraith JE et al. Clinical outcomes after long-term treatment with alglucosidase alfa in infants and children with advanced Pompe disease. Genet Med 2009;11:210–219.
van der Ploeg AT, Clemens PR, Corzo D et al. A randomized study of alglucosidase alfa in late-onset Pompe’s disease. N Engl J Med 2010;362:1396–1406.
Guo J, Kelton CM, Guo JJ. Recent developments, utilization, and spending trends for Pompe disease therapies. Am Health Drug Benefits 2012;5:182–189.
Russell DJ, Rosenbaum PL, Avery LM, Lane M. Gross Motor Function Measure (GMFM-66, GMFM-88) User’s Manual. Mac Keith Press: London, 2002.
Gottdiener JS, Bednarz J, Devereux R et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr 2004;17:1086–1119.
Lopez L, Colan SD, Frommelt PC et al. Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 2010;23:465–495; quiz 576–577.
American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 2002;166:518–624.
Beydon N, Davis SD, Lombardi E et al. An official American Thoracic Society/European Respiratory Society statement: pulmonary function testing in preschool children. Am J Respir Crit Care Med 2007;175:1304–1345.
Organized jointly by the American Thoracic Society, the European Respiratory Society, the European Society of Intensive Care Medicine, and the Société de Réanimation de Langue Française, and approved by ATS Board of Directors, December 2000. International Consensus Conferences in Intensive Care Medicine: noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med 2001;163:283–291.
Russell DJ, Rosenbaum PL, Cadman DT, Gowland C, Hardy S, Jarvis S. The gross motor function measure: a means to evaluate the effects of physical therapy. Dev Med Child Neurol 1989;31:341–352.
Russell DJ, Avery LM, Rosenbaum PL, Raina PS, Walter SD, Palisano RJ. Improved scaling of the gross motor function measure for children with cerebral palsy: evidence of reliability and validity. Phys Ther 2000;80:873–885.
Hanna SE, Bartlett DJ, Rivard LM, Russell DJ. Reference curves for the Gross Motor Function Measure: percentiles for clinical description and tracking over time among children with cerebral palsy. Phys Ther 2008;88:596–607.
van Capelle CI, van der Beek NA, de Vries JM et al. The quick motor function test: a new tool to rate clinical severity and motor function in Pompe patients. J Inherit Metab Dis 2012;35:317–323.
Winkel LP, Van den Hout JM, Kamphoven JH et al. Enzyme replacement therapy in late-onset Pompe’s disease: a three-year follow-up. Ann Neurol 2004;55:495–502.
Yang CF, Yang CC, Liao HC et al. Very early treatment for infantile-onset Pompe disease contributes to better outcomes. J Pediatr 2016;169:174–180.
van Capelle CI, van der Beek NA, Hagemans ML et al. Effect of enzyme therapy in juvenile patients with Pompe disease: a three-year open-label study. Neuromuscul Disord 2010;20:775–782.
van den Hout HM, Hop W, van Diggelen OP et al. The natural course of infantile Pompe’s disease: 20 original cases compared with 133 cases from the literature. Pediatrics 2003;112:332–340.
van Capelle CI. Children With Pompe Disease: Clinical Characteristics, Peculiar Features and Effects of Enzyme Replacement Therapy. Erasmus University: Rotterdam, The Netherlands, 2014: 300.
Winkel LP, Hagemans ML, van Doorn PA et al. The natural course of non-classic Pompe’s disease; a review of 225 published cases. J Neurol 2005;252:875–884.
van der Beek NA, Hagemans ML, Reuser AJ et al. Rate of disease progression during long-term follow-up of patients with late-onset Pompe disease. Neuromuscul Disord 2009;19:113–117.
Kishnani PS, Goldenberg PC, DeArmey SL et al. Cross-reactive immunologic material status affects treatment outcomes in Pompe disease infants. Mol Genet Metab 2010;99:26–33.
Patel TT, Banugaria SG, Case LE, Wenninger S, Schoser B, Kishnani PS. The impact of antibodies in late-onset Pompe disease: a case series and literature review. Mol Genet Metab 2012;106:301–309.
Jain S, Williams DJ, Arnold SR et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med 2015;372:835–845.
Bembi B, Cerini E, Danesino C et al. Management and treatment of glycogenosis type II. Neurology 2008;71:S12–36.
Author contributions
Dr. Hahn acted as the coordinating investigator and site principal investigator (PI) at Seattle Children’s Hospital; Dr. Kishnani participated in study design, data collection and interpretation as original site PI and later co-investigator at Duke University. Drs. Kronn, Leslie, Pena, Tanpaiboon, Gambello, Gibson, Hillman, Stockton, Day, and Wang were site PIs collecting and interpreting data at their institutions. Sanofi Genzyme-employed authors participated in study design, data collection, analysis and interpretation, manuscript revision, and the decision to submit: Dr. An Haack was the clinical study director, Dr Shafi collected and interpreted safety data; Dr. Sparks interpreted data as a medical director; Dr. Wilson contributed to the design, analysis, and interpretation of motor evaluations; Dr. Zhao contributed to design and data analysis as study statistician. All authors contributed important intellectual revisions to the manuscript, approved the final version for submission, and take full responsibility for the contents.
Acknowledgments
This study was supported by Sanofi Genzyme. The authors exerted sole scientific control of manuscript development and acknowledge writing assistance from Kim Coleman Healy and editing and data graphing assistance from Jane M. Gilbert of Envision Medical Affairs, contracted by Sanofi Genzyme to provide publication support services. Robert Pomponio and Catherine Wilson of Sanofi Genzyme contributed to study design and analysis of respective genetic and motor data. Jennifer Goldstein of Duke University Medical Center analyzed CRIM statuses of genotypes. The ADVANCE sites, contributing investigators, and ethics approvers are listed in the Supplementary Appendix 1.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Disclosure
Dr. Hahn reports honoraria and travel support from Sanofi Genzyme for participation in the ADVANCE investigators’ meeting and personal fees from Seattle Children’s Hospital outside the submitted work. Dr. Kronn discloses research funding from Sanofi Genzyme and New York Medical College during the conduct of the study. Dr. Leslie reports personal fees (honoraria for advisory board activities) and non-financial support (professional writing support) from Sanofi Genzyme during the conduct of the study and personal fees (honoraria) and non-financial support (professional writing support) from Sanofi Genzyme, outside the submitted work. Dr. Pena discloses Sanofi Genzyme advisory board membership for Pompe and Gaucher diseases and speakers’ bureau membership for Gaucher disease. Dr. Tanpaiboon discloses receipt of honoraria and travel support as a principal investigator in clinical trials from Sanofi Genzyme and Biomarin. Dr. Gambello declares that he has nothing to disclose. Dr. Gibson discloses research support and speakers’ bureau membership for Sanofi Genzyme. Dr. Hillman declares that he has nothing to disclose. Dr. Stockton is a member of the Sanofi Genzyme Pompe Registry Advisory Board and discloses research support, honoraria and speakers’ bureau membership from Sanofi Genzyme. Dr. Day declares that he has nothing to disclose. Dr. Wang discloses a speaking stipend and travel support for a Sanofi Genzyme-sponsored Pompe Registry meeting in 2014. Drs. An Haack and Sparks disclose being employees of Sanofi Genzyme; Drs. Shafi and Zhao disclose having been employed and Dr. Wilson having been contracted by Sanofi Genzyme when the study was conducted. Dr. Kishnani discloses research support and honoraria from Sanofi Genzyme and membership of the Sanofi Genzyme Pompe and Gaucher Disease Registry Advisory Boards; she also discloses grants from Roche, Shire Pharmaceuticals, Valerion; personal fees from Alexion Pharmaceuticals, Inc., Amicus Therapeutics, Shire Pharmaceuticals, and Uniqure; and advisory board membership for Baebies, Inc.
Rights and permissions
Open Access This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Hahn, S., Kronn, D., Leslie, N.D. et al. Efficacy, safety profile, and immunogenicity of alglucosidase alfa produced at the 4,000-liter scale in US children and adolescents with Pompe disease: ADVANCE, a phase IV, open-label, prospective study. Genet Med 20, 1284–1294 (2018). https://doi.org/10.1038/gim.2018.2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2018.2