Abstract
Purpose
Mutations in POLG, the most common single-gene cause of inherited mitochondrial disease, are diagnostically challenging owing to clinical heterogeneity and overlap between syndromes. We aimed to improve the clinical recognition of POLG-related disorders in the pediatric population.
Methods
We performed a multinational, phenotype: genotype study using patients from three centers, two Norwegian and one from the United Kingdom. Patients with age at onset <12 years and confirmed pathogenic biallelic POLG mutations were considered eligible.
Results
A total of 27 patients were identified with a median age at onset of 11 months (range 0.6–80.4). The majority presented with global developmental delay (n=24/24, 100%), hypotonia (n=22/23, 96%) and faltering growth (n=24/27, 89%). Epilepsy was common, but notably absent in patients with the myocerebrohepatopathy spectrum phenotype. We identified two novel POLG gene mutations.
Conclusion
Our data suggest that POLG-related disease should be suspected in any child presenting with diffuse neurological symptoms. Full POLG sequencing is recommended since targeted screening may miss mutations. Finally, we simplify the classification of POLG-related disease in children using epilepsy as the crucial defining element; we show that Alpers and myocerebrohepatopathy spectrum follow different outcomes and that they manifest different degrees of respiratory chain dysfunction.
Similar content being viewed by others
INTRODUCTION
POLG (OMIM *174763) encodes the catalytic subunit of DNA polymerase gamma, the enzyme responsible for mitochondrial DNA replication and repair.1 Mutations in POLG result in mitochondrial DNA depletion and/or multiple deletions and are considered the most common cause of inherited mitochondrial disorders.2, 3
The first pathogenic POLG mutation was identified in families with autosomal dominant progressive external ophthalmoplegia.4 Subsequently, POLG mutations have been associated with a wide range of overlapping clinical phenotypes, including (i) Alpers syndrome; (ii) myocerebrohepatopathy spectrum (MCHS); (iii) myoclonic epilepsy, myopathy, sensory ataxia—including disorders previously described as spinocerebellar ataxia with epilepsy; (iv) ataxia neuropathy spectrum, including phenotypes previously described as sensory ataxia, neuropathy, dysarthria, and ophthalmoplegia and mitochondrial recessive ataxia syndrome; (v) autosomal dominant progressive external ophthalmoplegia; and (vi) autosomal recessive progressive external ophthalmoplegia.5, 6 Rare phenotypes include mitochondrial neurogastrointestinal encephalopathy (MNGIE)-like phenotype,7 mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes (MELAS)-like phenotype,8 premature ovarian failure,9 Parkinsonism, psychiatric disorders, cataract,10 sensorineural hearing loss, diabetes, and cardiomyopathy.11
Alpers syndrome and MCHS are the two phenotypes most commonly reported with POLG mutations in the pediatric population.12 The neuropathology of Alpers syndrome (OMIM 203700) was first described in 1931,13 but it was not until the 1980s that the link to mitochondrial dysfunction was made.14 Pathogenic POLG mutations causing Alpers syndrome were first reported in 2004.15 This syndrome is almost universally fatal in childhood, making it one of the most severe forms in the spectrum of POLG-related disease. Alpers syndrome is characterized by progressive encephalopathy with psychomotor regression, refractory epilepsy, and characteristic liver disease,16 presenting most frequently during infancy after an initial period of normal development.5, 6 The most common early seizure types are focal and focal evolving to bilateral convulsive seizures, with predominance of epileptiform discharges over occipital regions.17 The seizure semiology may evolve with time to more complex forms including epilepsia partialis continua, myoclonic epilepsy, and status epilepticus.17, 18, 19
Hepatic involvement may progress rapidly to end-stage liver failure, and may be triggered by valproic acid,20, 21 but is not universal; affected children with biallelic POLG mutations with encephalopathy without liver failure are well recognized.11, 19 Diagnostic criteria for Alpers syndrome include characteristic liver histopathological changes, namely two of the following: microvesicular steatosis, bile ductular proliferation, hepatocyte dropout, bridging fibrosis or cirrhosis, collapse of liver cell plates, parenchymal lobular architecture, regenerative nodules and oncocytic changes in scattered hepatocytes not affected by steatosis.12
MCHS is also severe and fatal, but less frequently reported than Alpers syndrome. MCHS most frequently presents between the neonatal period and three years and is characterized by a triad of myopathy or hypotonia, developmental delay or encephalopathy, and liver dysfunction.12 Diagnostic criteria for MCHS include absence of hepatic histopathological features of classical Alpers and at least two of the following: neuropathy; seizures; elevated blood or cerebrospinal fluid lactate; dicarboxylic aciduria; renal tubular dysfunction with aminoaciduria, glycosuria, or bicarbonaturia; hearing loss; abnormal magnetic resonance image (MRI), with either cerebral volume loss, delayed myelination, or white matter disease; and either isolated deficiency of complex IV (cytochrome c oxidase) or a combined defect of two or more oxidative phosphorylation complexes in skeletal muscle or liver biopsy.5, 6, 19, 22, 23
MNGIE is a rare autosomal recessive mitochondrial disorder usually caused by mutations in TYMP encoding thymidine phosphorylase, an enzyme involved in nucleoside salvage. MNGIE usually presents between the first and third decades with severe gastrointestinal dysmotility, failure to thrive, vomiting, abdominal pain, cachexia, and neurological symptoms including encephalopathy, ptosis, ophthalmoplegia, peripheral neuropathy, and muscle weakness.24, 25 POLG mutations have been previously reported in four patients (aged 15–50 years) with a MNGIE-like phenotype.7, 26
In this study we aimed to improve clinical recognition of the extremely heterogeneous and overlapping pediatric POLG phenotypes by carefully documenting and analyzing the natural history of early-onset POLG-related disorders in a large multinational pediatric cohort.
MATERIALS AND METHODS
Study design and population
We conducted a multicenter, retrospective study including collaborating centers from Norway (Haukeland University Hospital, Bergen and University Hospital North of Norway, Tromsø) and the United Kingdom (Great Ormond Street Hospital, London). All subjects with age at onset <12 years and biallelic pathogenic POLG variants were considered eligible. Patients who died before the POLG gene was identified were included if subsequent analysis of stored samples revealed two pathogenic POLG mutations. Deceased patients were included if an affected sibling had genetically confirmed POLG-related disease and a similar clinical course. This study includes detailed clinical data of 13 patients (cases 1, 2, 3, 4, 9, 15, 16, 17, 18, 19, 20, 22, and 24; Supplementary File 1 online) whose POLG mutations had been reported previously.27, 28 Data collection was completed in July 2016.
Patients were phenotypically classified into three groups: Alpers spectrum, MCHS, and MNGIE phenotypes, based on previously described criteria.12, 23, 24, 25 In view of the rarity of MCHS, and to provide a better understanding of this particular phenotype, a systematic literature review (using the search terms “POLG,” “mitochondria,” “Alpers,” “infantile hepatocerebral syndromes,” “mitochondrial DNA depletion,” and “myocerebrohepatopathy syndrome” in PubMed, June 2016) was used to identify previously published cases. Cases with age at onset less than 12 years fulfilling the criteria for MCHS and confirmed bialleleic POLG mutations were included. These additional MCHS cases were not included in the natural history analysis.
Data collection
Patient data (demographic information, clinical features, biochemical data, muscle biopsy, neurophysiological, neuroimaging and genetic findings, and medical treatment including response to antiepileptic drugs) were collected using a structured electronic case report form that was developed and tested by a pilot study of 10 patients conducted in Haukeland University Hospital, Bergen, Norway.
Preterm birth was defined as birth before a gestational age of 37 completed weeks. Microcephaly was defined as head circumference more than two standard deviations below the mean for age and sex. Renal tubulopathy was defined by the presence of at least three of the following: tubular acidosis with generalized aminoaciduria, tubular proteinuria, glycosuria, Fanconi syndrome, or increase in urinary N-acetyl-beta-D-glucosaminidase/creatinine ratio. Liver involvement was defined by the presence of two or more of the following in at least two different time points: elevated aspartate aminotransferase, gamma-glutamyltransferase, bilirubin or ammonia, low serum albumin, or pathological histological findings on liver biopsy. Hearing impairment was defined as abnormal auditory evoked response test. Neuroimaging was reviewed by two independent investigators. Therapy-resistant epilepsy was defined using the International League Against Epilepsy definition.29
Statistical analysis
Descriptive data analysis was performed using statistic software package SPSS version 23.0. End of follow-up was defined as the patient’s last visit to the hospital or death. Univariate survival analysis was performed using log-rank test to compare differences in survival time between categories.
All genetic studies were performed with informed consent. Ethical approval for the study was obtained from the Regional Committee for Medical and Health Research Ethics, Western Norway (REK 2014/1783-4). The study was registered as an audit at Great Ormond Street Hospital, London, United Kingdom.
RESULTS
Demography
Twenty-seven patients (15 male, 12 female) from 22 pedigrees (including two patients from consanguineous families) with genetically confirmed POLG mutations were identified. Nineteen were diagnosed in the United Kingdom and eight in Norway. The majority of patients were Northern European (n=23), with two patients from Cyprus, one from United Arab Emirates, and one of Pakistani background (Supplementary File 1).
Major clinical features
Median age at onset of symptoms requiring medical evaluation for the group as a whole was 11.2 months (range 0.6 to 80.4). The majority of cases were born at term with uneventful pregnancy and delivery (n=26); three cases were small for gestational age and one had microcephaly. Neonatal problems occurred in 11/27 (41%) of cases, including feeding difficulties (n=9/25, 36%), vomiting (n=7/21, 33%), hypotonia (n=4/23, 17%), and hypoglycemia (n=2/20, 10%). None had neonatal seizures. Disease onset was apparently spontaneous in 15/26 (58%) and followed an infectious illness in 11 cases (42%).
The predominant clinical features (Table 1) were faltering growth (n=24/27, 89%), global developmental delay (n=24/24, 100%), hypotonia (n=22/23, 96%), seizures (n=19/26, 73%), and vomiting (n=22/26, 85%). Focal evolving to bilateral convulsive seizures (Table 1) were the most common seizure type (n=14/19, 74%). Infantile spasms were observed in one case (patient 23). Electroencephalogram (EEG) was pathological in 19 of 22 patients (Table 1) with epileptiform activities predominantly over occipital regions (Figure 1).
EEG, MRI and histopathological findings in POLG disease. Upper panel: EEG traces and MRI scans recorded during the same period of hospitalization in two patients with Alpers syndrome caused by POLG mutations. (a) (case 2): EEG tracing displayed at 30 mm/cm, 150 μV/cm, 0.01–30 Hz. EEG shows high-voltage polyspike-slow and sharp-slow wave around 1–2 Hz frequency in the right occipitotemporal channels. Axial T2-weighted MRI shows bilateral high T2 signal consistent with cortical edema, in the occipitotemporal regions. (b) (case 4): EEG tracing displayed at 30 mm/cm, 500 μV/cm, and 0.01–30 Hz. Periodic polyspike-slow waves localized at the left occipitotemporal area. Axial T2-weighted MRI shows bilateral cortical edema, in the occipitotemporal regions. Lower panel: muscle histochemistry from three cases shows occasional fibers with dense mitochondrial accumulations on the Gömöri trichrome stain (A, case 17; B, case 18; and C, case 4). In a few fibers, these formed subsarcolemmal accumulations that indented the sarcoplasm on at least two sides as seen typically in ragged red fibers (a and b). EEG, electroencephalogram; MRI, magnetic resonance image.
Renal tubular dysfunction was observed in three cases, and one child had hypothyroidism. Ophthalmological involvement occurred in 12 patients, including optic atrophy in two cases (patients 13 and 16) and cataract in another two cases (patients 19 and 20). Two children (patients 1 and 21) had hearing impairment.
Biochemical, neurophysiological and muscle biopsy findings
Laboratory investigations at presentation revealed increased lactate in blood in 60% (n=12/20) and in cerebrospinal fluid in 40% (n=2/5). Hepatic aminotransferases were increased in 13/20 cases (Table 1). Electromyogram and nerve conduction studies were performed on six cases and were abnormal in only one case, who had neuropathic and axonal changes. Visual evoked response was abnormal in 5 of 10 cases.
Muscle biopsy was performed in 14 cases, and was abnormal in 10 (Table 1): three had ragged red fibers (Figure 1) and four COX-negative fibers; excessive lipid accumulation was observed in 7 cases and abnormal respiratory chain activities in 9 cases (Supplementary File 2). Interestingly, most Alpers patients had normal respiratory chain enzyme activities or isolated deficiency of a single enzyme complex, whilst those with MCHS had multiple respiratory chain complex deficiencies (Supplementary File 2).
Neuroimaging
MRIs were available for 17 cases. The majority (n=14/17, 82%) showed abnormality at disease onset. The most common MRI finding was cortical focal lesions manifesting as T2/FLAIR hyperintensities involving cortical and subcortical areas, predominantly affecting the occipital lobes (Figure 1). Less frequently, T2-hyperintense thalamic lesions (n=3/17, 18%) and cerebellar atrophy (n=1/17, 6%) were observed (Table 1).
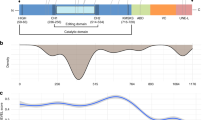
Genetic findings
All cases had two confirmed pathogenic POLG variants identified either by targeted mutation analysis for specific common mutations (c.1399G>C, p.Ala467Thr and c.2243G>C, p.Trp748Ser) or by sequence analysis of all coding regions of POLG. Two novel POLG gene mutations (c.1493A>C, p.Lys498Thr, and c.1862 G>A, p.Gly621Asp) were identified (patients 23 and 26). The c.2492A>G, p.Tyr831Cys change has a relatively high population frequency (0.006277; Exome Aggregation Consortium (ExAC), Cambridge, MA),30 but when it occurs in trans with a severe mutation such as c.3401A>G, p.His1134Arg it is clearly pathogenic. All POLG mutations and associated phenotypes identified in this study are illustrated in Figure 2.
Schematic diagram of the POLG gene illustrating mutations identified in this study. Mutations associated with the Alpers and MCHS phenotypes are located throughout the gene, i.e., in the exonuclease, linker, and polymerase domains. The mutations in the patient with a MNGIE-like phenotype were also present in patients with Alpers and MCHS. MCHS, myocerebrohepatopathy spectrum; MNGIE, mitochondrial neurogastrointestinal encephalopathy.
Phenotype spectrum
Six patients fulfilled diagnostic criteria for MCHS, 19 for Alpers, and one for a MNGIE-like phenotype. One patient was unclassified owing to insufficient data. The median age at onset for the MCHS group was 4.7 months (range 0.9–7 months) compared to 12.4 months (range 0.9–80.4 months) for the Alpers group. All patients with MCHS had liver pathology, hypotonia, and failure to thrive. None had seizures (Table 2). Five additional patients from the literature review fulfilling diagnostic criteria for MCHS19, 22, 31 had similar clinical features and also did not have seizures (Table 2). The common founder mutations c.1399G>C, p.Ala467Thr and c.2243G>C, p.Trp748Ser were present in one MCHS case in our cohort (case 16) and one case in the literature. All cases in our cohort fulfilling diagnostic criteria for Alpers syndrome had epilepsy (19/19). One patient was classified as having a MNGIE-like phenotype (case 27). This is a 7-year-old boy, who presented at the age of 3 months with failure to thrive, progressive gastrointestinal dysmotility, vomiting, and gradually became dependent on total parental nutrition. He has muscle weakness, absent lower limb reflexes, and is wheelchair dependent. He is developmentally delayed and has learning difficulties. He has no liver pathology, seizures, or leukoencephalopathy.
Survival analysis
Of 27 patients, four were alive at the time of data analysis, and one had been lost to follow-up. Median age at death was 15.8 months (range 1.0 to 184.6 months), whereas median time from disease onset to death was 4.9 months (range 0.5 to 181.2 months). The main causes of death were liver failure (13/22), sepsis (5/22), and status epilepticus (4/22). Median survival time of patients with disease onset ≤12 months was 3.6 months ( range 0.5–181) compared to 10 months (range 1.4–82) for those with disease onset >12 months. Further analysis showed that median survival time of patients with epilepsy was 4 months (range 0.5–181), compared to 5 months (range 0.5–91) for those without epilepsy. Survival analysis by phenotype showed that the median survival time for patients with MCHS was 5 months (range 0.6–22) and 4 months (range 0.5–181) for Alpers.
DISCUSSION
Diagnosis of mitochondrial disorders is still a major challenge, particularly in the pediatric population. POLG mutations are associated with a wide and overlapping spectrum of phenotypes and while several major clinical entities are now recognized, it is likely that neither the full spectrum nor the extent to which the phenotypes overlap is yet known.5, 6 Reports in adults of minor phenotypes such as MELAS-like, MNGIE-like, optic atrophy, diabetes, and hearing loss7, 8, 10, 11 have added to the confusion. The cornerstone of clinical diagnosis is a relevant phenotypic classification that physicians in everyday clinical practice can use. We have therefore analyzed the largest pediatric cohort to date to provide a comprehensive clinical description of pediatric patients with POLG-related disease.
We found that the majority of patients had relatively diffuse clinical features with hypotonia, developmental delay, failure to thrive, and seizures. These nonspecific clinical features overlap with the manifestations of other mitochondrial disorders presenting during early childhood, including Alpers syndrome caused by defects in other genes (e.g., TWNK, FARS2, NARS2, and PARS2),32, 33, 34, 35, 36 and causes of Leigh syndrome such as SURF1 deficiency.37, 38, 39 Consequently, identifying which individuals to screen for POLG mutations in the neonatal period and early childhood is challenging. Further, our study showed that early-onset POLG-related disorders are associated with high mortality (n=22/26, 85%). The elapsed median time from disease onset to death was 5 months, highlighting the rapid disease progression. As a result, early clinical recognition and diagnosis is particularly urgent, especially in families seeking prenatal diagnosis.
Epilepsy was one of the major clinical features, and was present in 89% (n=17/19) at disease onset. Seizure semiology was similar to that reported in adult-onset POLG-related disorders17, 39 with predominance of focal and focal evolving to bilateral convulsive seizures and epileptiform discharges over occipital regions. Ataxia, movement disorders, and stroke-like episodes were less frequent compared to adults with POLG mutations. Cataract and retinopathy have been reported in adults,10, 18 but we now describe two pediatric patients with cataract and two with optic atrophy. Diabetes and cardiomyopathy were not present in our pediatric cohort. Despite the overlapping features between early- and later-onset POLG-related disorders, it is clear from our study, and our literature review, that these two groups are not identical and we feel they should be considered as two separate entities.
Regarding phenotypic classification, our data reinforced the current understanding of Alpers and MCHS as two separate entities with different age at onset and survival. We found, however, significant overlap in clinical features between the Alpers and MCHS subgroups and application of the previously described criteria for diagnosis12, 23 was challenging. Using the characteristic liver pathological findings to differentiate, as previously suggested,12 was not possible as liver biopsy was only performed in three of our cases. This likely reflects clinical practice where liver biopsy is rarely performed in the neonatal and pediatric setting, because of the attendant risks of morbidity and mortality. Moreover, not all patients with the Alpers phenotype even show liver enzyme abnormalities. By comparing our cohort of patients with Alpers and those with MCHS, we found, however, that epilepsy was exclusively associated with the Alpers phenotype (Table 3). To confirm this, we conducted a systematic literature review to identify previously published MCHS cases (Table 2), and found too that none of these had epilepsy. Further, the most severe respiratory chain defects were observed in the MCHS group, supporting the view that these patients are more severely affected and potentially die before the onset of seizures. Discordance observed in one sibling pair (cases 15 and 16) provides further evidence for this hypothesis. Case 15 died at 9 months with intractable seizures whereas his sister case 16 died at 5 months and never developed seizures. Based on our findings, we suggest that instead of using complicated clinical and histopathological criteria to differentiate between Alpers and MCHS phenotypes, the classification of early-onset POLG-related disorders can be simplified into those with or without epilepsy.
Our cohort also includes a patient with an early-onset MNGIE-like phenotype without leukoencephalopathy (patient 27). This expands the phenotypic spectrum in this age group and demonstrates the importance of considering POLG-related disorders in children with severe gastrointestinal dysmotility even in the absence of liver pathology, seizures, or characteristic neuroradiological findings for POLG disease.
Previous reports have recommended screening for the common founder POLG mutations in children younger than 12 years with unexplained encephalopathy, or multisystem neurological disorders.11, 40 Since these mutations (c.1399G>A, p.Ala467Thr and c.2243G>C, p.Trp748Ser) were identified only once in in our MCHS cohort (patient 16) and one previously published MCHS case,31 there is a high risk of missing the diagnosis in these patients, demonstrating clearly the limited value of screening only for common POLG mutations in this age group.
In conclusion, while early-onset POLG-related disease is associated with complex overlapping phenotypes, we suggest classification can be simplified according to the presence or absence of epilepsy. We provide a detailed description of the natural history of early-onset POLG-related disorders, and a simplified classification to facilitate clinical recognition of these disorders by neonatologists and pediatricians. Furthermore, we demonstrate the need to perform full sequence analysis of the entire POLG gene rather than targeting common POLG mutations in patients with unexplained encephalopathy and multisystem disorders with or without epilepsy, both in the neonatal period and during childhood.
Change history
12 October 2018
Since the online publication of the article, the authors have noted errors with Table 2. Patient 8 in Table 2 should be replaced by patient 16, patient 9 should be patient 17, patient 10 should be patient 18, patient 11 should be patient 19, patient 12 should be patient 20 and patient 15 should be patient 22, to correspond to the patient numbers in the full patient table with mutation data in Supplementary file 1 online. Also in Table 2, the correct reference for patients D and E is 31, not 30 as stated. The authors apologize for any inconvenience caused by these errors.
References
Copeland WC, Longley MJ . DNA polymerase gamma in mitochondrial DNA replication and repair. Sci World J 2003;3:34–44.
Chinnery PF, Zeviani M . 155th ENMC workshop: polymerase gamma and disorders of mitochondrial DNA synthesis, 21–23 September 2007, Naarden, The Netherlands. Neuromuscul Disord 2008;18:259–267.
Spinazzola A, Zeviani M . Disorders from perturbations of nuclear-mitochondrial intergenomic cross-talk. J Intern Med 2009;265:174–192.
Van Goethem G, Dermaut B, Lofgren A et al. Mutation of POLG is associated with progressive external ophthalmoplegia characterized by mtDNA deletions. Nat Genet 2001;28:211–212.
Cohen BH, Chinnery PF, Copeland WC . POLG-related disorders. In: Pagon RA, Adam MP, Ardinger HH et al, (eds). GeneReviews. University of Washington: Seattle, WA, 1993.
Saneto RP, Naviaux RK . Polymerase gamma disease through the ages. Dev Disabil Res Rev 2010;16:163–174.
Tang S, Dimberg EL, Milone M et al. Mitochondrial neurogastrointestinal encephalomyopathy (MNGIE)-like phenotype: an expanded clinical spectrum of POLG1 mutations. J Neurol 2012;259:862–868.
Deschauer M, Tennant S, Rokicka A et al. MELAS associated with mutations in the POLG1 gene. Neurology 2007;68:1741–1742.
Pagnamenta AT, Taanman JW, Wilson CJ et al. Dominant inheritance of premature ovarian failure associated with mutant mitochondrial DNA polymerase gamma. Hum Reprod 2006;21:2467–2473.
Luoma P, Melberg A, Rinne JO et al. Parkinsonism, premature menopause, and mitochondrial DNA polymerase gamma mutations: clinical and molecular genetic study. Lancet 2004;364:875–882.
Horvath R, Hudson G, Ferrari G et al. Phenotypic spectrum associated with mutations of the mitochondrial polymerase gamma gene. Brain 2006;129 (Pt 7):1674–1684.
Nguyen KV, Sharief FS, Chan SS et al. Molecular diagnosis of Alpers syndrome. J Hepatol 2006;45:108–116.
Alpers BJ . Diffuse progressive degeneration of the gray matter of the cerebrum. Arch Neurol Psychiatry 1931;25:469–505.
Gabreels FJ, Prick MJ, Trijbels JM et al. Defects in citric acid cycle and the electron transport chain in progressive poliodystrophy. Acta Neurol Scand 1984;70:145–154.
Naviaux RK, Nguyen KV . POLG mutations associated with Alpers' syndrome and mitochondrial DNA depletion. Ann Neurol 2004;55:706–712.
Harding BN . Progressive neuronal degeneration of childhood with liver disease (Alpers-Huttenlocher syndrome): a personal review. J Child Neurol 1990;5:273–287.
Engelsen BA, Tzoulis C, Karlsen B et al. POLG1 mutations cause a syndromic epilepsy with occipital lobe predilection. Brain 2008;131 (Pt 3): 818–828.
Hakonen AH, Heiskanen S, Juvonen V et al. Mitochondrial DNA polymerase W748S mutation: a common cause of autosomal recessive ataxia with ancient European origin. Am J Hum Genet 2005;77:430–441.
de Vries MC, Rodenburg RJ, Morava E et al. Multiple oxidative phosphorylation deficiencies in severe childhood multi-system disorders due to polymerase gamma (POLG1) mutations. Eur J Pediatr 2007;166:229–234.
Saneto RP, Lee IC, Koenig MK et al. POLG DNA testing as an emerging standard of care before instituting valproic acid therapy for pediatric seizure disorders. Seizure 2010;19:140–146.
Tzoulis C, Engelsen BA, Telstad W et al. The spectrum of clinical disease caused by the A467T and W748S POLG mutations: a study of 26 cases. Brain 2006;129 (Pt 7):1685–1692.
Ferrari G, Lamantea E, Donati A et al. Infantile hepatocerebral syndromes associated with mutations in the mitochondrial DNA polymerase-gammaA. Brain 2005;128 (Pt 4):723–731.
Wong LJ, Naviaux RK, Brunetti-Pierri N et al. Molecular and clinical genetics of mitochondrial diseases due to POLG mutations. Hum Mutat 2008;29:E150–E172.
Nishino I, Spinazzola A, Papadimitriou A et al. Mitochondrial neurogastrointestinal encephalomyopathy: an autosomal recessive disorder due to thymidine phosphorylase mutations. Ann Neurol 2000;47:792–800.
D'Angelo R, Rinaldi R, Carelli V et al. ITA-MNGIE: an Italian regional and national survey for mitochondrial neuro-gastro-intestinal encephalomyopathy. Neurol Sci 2016;37:1149–1151.
Van Goethem G, Schwartz M, Lofgren A et al. Novel POLG mutations in progressive external ophthalmoplegia mimicking mitochondrial neurogastrointestinal encephalomyopathy. Eur J Hum Genet 2003;11:547–549.
Taanman JW, Rahman S, Pagnamenta AT et al. Analysis of mutant DNA polymerase gamma in patients with mitochondrial DNA depletion. Hum Mutat 2009;30:248–254.
Tzoulis C, Neckelmann G, Mork SJ et al. Localized cerebral energy failure in DNA polymerase gamma-associated encephalopathy syndromes. Brain 2010;133 (Pt 5):1428–1437.
Kwan P, Arzimanoglou A, Berg AT et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 2010;51:1069–1077.
Lek M, Karczewski KJ, Minikel EV et al. Analysis of protein-coding genetic variation in 60706 humans. Nature 2016;536:285–291.
Tang S, Wang J, Lee NC et al. Mitochondrial DNA polymerase gamma mutations: an ever expanding molecular and clinical spectrum. J Med Genet 2011;48:669–681.
Rotig A, Poulton J . Genetic causes of mitochondrial DNA depletion in humans. Biochim Biophys Acta 2009;1792:1103–1108.
Nikali K, Lonnqvist T. Infantile-onset spinocerebellar ataxia. In: Pagon RA, Adam MP, Ardinger HH et al, (eds). GeneReviews. University of Washington: Seattle, WA, 1993.
Elo JM, Yadavalli SS, Euro L et al. Mitochondrial phenylalanyl-tRNA synthetase mutations underlie fatal infantile Alpers encephalopathy. Hum Mol Genet 2012;21:4521–4529.
Sofou K, Kollberg G, Holmstrom M et al. Whole exome sequencing reveals mutations in NARS2 and PARS2, encoding the mitochondrial asparaginyl-tRNA synthetase and prolyl-tRNA synthetase, in patients with Alpers syndrome. Mol Genet Genomic Med 2015;3:59–68.
Vanlander AV, Menten B, Smet J et al. Two siblings with homozygous pathogenic splice-site variant in mitochondrial asparaginyl-tRNA synthetase (NARS2). Hum Mutat 2015;36:222–231.
Sofou K, De Coo IF, Isohanni P et al. A multicenter study on Leigh syndrome: disease course and predictors of survival. Orphanet J Rare Dis 2014;9:52.
Wedatilake Y, Brown RM, McFarland R et al. SURF1 deficiency: a multi-centre natural history study. Orphanet J Rare Dis 2013;8:96.
Wolf NI, Rahman S, Schmitt B et al. Status epilepticus in children with Alpers' disease caused by POLG1 mutations: EEG and MRI features. Epilepsia 2009;50:1596–1607.
Hakonen AH, Davidzon G, Salemi R et al. Abundance of the POLG disease mutations in Europe, Australia, New Zealand, and the United States explained by single ancient European founders. Eur J Hum Genet 2007;15:779–783.
Acknowledgements
This project was supported by grants from the Western Norway Regional Health Authority (grant 911944), the Lily Foundation, and Great Ormond Street Hospital Children’s Charity. S.R. is supported by a Great Ormond Street Hospital Children's Charity Research Leadership Award (V1260) and her group currently receives research grant funding from the Lily Foundation and the National Institute for Health Research Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. We thank the NHS England Rare Mitochondrial Disease Service laboratories in London and Newcastle for performing respiratory chain enzyme assays and Tom Eichele, Neurophysiology Department, Haukeland University Hospital, Bergen-Norway for help in reviewing EEG findings.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary material is linked to the online version of the paper at
Supplementary information
Rights and permissions
About this article
Cite this article
Hikmat, O., Tzoulis, C., Chong, W. et al. The clinical spectrum and natural history of early-onset diseases due to DNA polymerase gamma mutations. Genet Med 19, 1217–1225 (2017). https://doi.org/10.1038/gim.2017.35
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2017.35
Keywords
This article is cited by
-
A Review of Brain and Pituitary Gland MRI Findings in Patients with Ataxia and Hypogonadism
The Cerebellum (2023)
-
POLG-related disorders and their neurological manifestations
Nature Reviews Neurology (2019)
-
Spectrum of movement disorders and neurotransmitter abnormalities in paediatric POLG disease
Journal of Inherited Metabolic Disease (2018)